Figures & data
Figure 1. A, E: Clinical features of bullous pemphigoid lesions on the skin of a patient upon initial diagnosis (lesions covering over 40% of the body-surface area). B, F: following a two-week therapy regimen involving the administration of Dupilumab in conjunction with low-dose hormones, a notable reduction in the presence of lesions was seen (lesions covering 35% of the body-surface area). C, G: following a 4-week therapy protocol using only upadacitinib, a significant improvement in the condition of the skin lesions was noted (lesions covering 10% of the body-surface area)., with no occurrence of new lesions. D, H: following a sustained 10-week course of upadacitinib treatment, the regression of pre-existing lesions persisted (lesions covering < 5% of the body-surface area), with no new lesions observed.
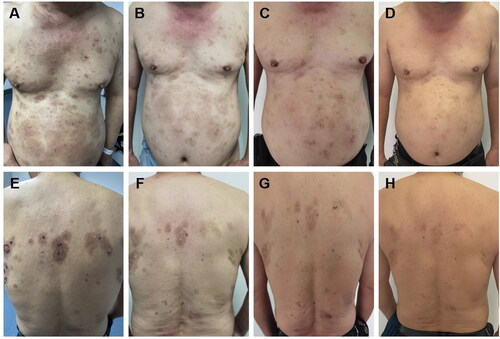
Figure 2. The histopathological findings obtained from this patient. A, B: the vesicular skin lesions exhibited subepidermal blisters containing neutrophils and eosinophils, along with an infiltration of lymphocytes and eosinophils in the superficial dermis (H&E, A: ×200; B: ×400). C, D: the psoriasis lesions are characterized by hyperkeratosis and parakeratosis of the epidermis, clubbing hyperplasia of the epidermis, neutrophil infiltration, thinning of the granular layer, regular thickening of the spinous layer, and a small number of lymphocytes surrounding the blood vessels in the superficial dermis (H&E, C: ×200; D: ×400).
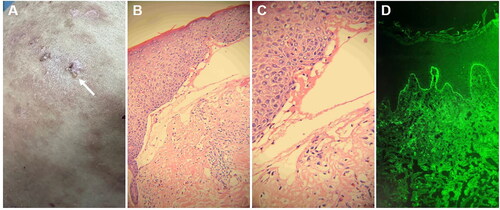
Figure 3. A, E: The occurrence of psoriatic lesions was observed subsequent to the administration of dupilumab for a period of two weeks (PASI = 1.6). B, F: the lesions associated with psoriasis became more severe subsequent to the implementation of a dupilumab treatment regimen lasting six weeks (PASI = 2.4). C, G: following a 4-week course of treatment consisting exclusively of upadacitinib, a significant improvement in cutaneous lesions was observed, with no occurrence of new lesions (PASI = 0.8). D, H: Existing lesions continued to diminish and no new lesions were observed following a sustained 10-week course of upadacitinib treatment (PASI = 0).
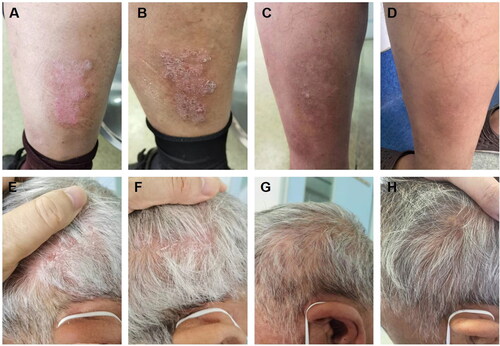
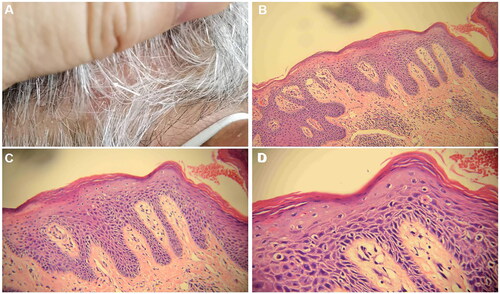
Figure 4. Histopathological findings of scalp psoriasis lesions (hematoxylin-eosin staining was utilized for histopathology). A. The samples were obtained from cutaneous lesions on the scalp that exhibited erythema and scaling. B, C, D: a small number of lymphocytes encircle the blood vessels in the superficial dermis, where hyperkeratosis and parakeratosis of the epidermis are observed, along with clubbing hyperplasia of the epidermis, neutrophil infiltration, thinning of the granular layer, and regular thickening of the spinous layer. The magnification factors for B, C, and D are 10×, 20×, and 40×, respectively.