Figures & data
Table 1. Attributes and attribute levels.
Table 2. Characteristics of the study cohort.
Table 3. Patient-reported outcomes.
Figure 1. Preferences for systemic treatment of AD. Relative importance scores (RIS) averaged across the study cohort (a). PWU for type of side effects (b) and application method (c). Bars: means with standard deviations. AD: atopic dermatitis; PWU: Part-Worth Utility; RIS: Relative Importance Scores.
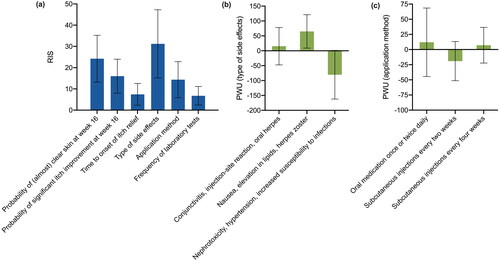
Figure 2. Treatment preferences according to sex, age and psychiatric comorbidity. (a) No significant differences were found with respect to sex. (b) Patients ≤ 40 years of age put more emphasis on the probability of clear skin (p = 0.004) and of itch improvement (p = 0.012) but regarded the type of side effect less relevant (p = 0.002). Older patients had greater concern about “nephrotoxicity, hypertension and increased susceptibility to infections” (p = 0.003) and were more willing to accept “nausea, elevation in lipids and herpes zoster” (p = 0.035). (c) Presence of a psychiatric comorbidity was associated with higher preferences for the probability of clear skin (p = 0.029) and less interest in the type of side effects (p = 0.020). Patients with psychiatric comorbidity were less afraid of “nephrotoxicity, hypertension and increased susceptibility to infections” (p = 0.008) and disliked injections every 4 weeks more (p = 0.033) than other participants. Bars: means with standard deviations. PWU: Part-Worth Utility; RIS: Relative Importance Scores. *p < 0.05, **p < 0.01.
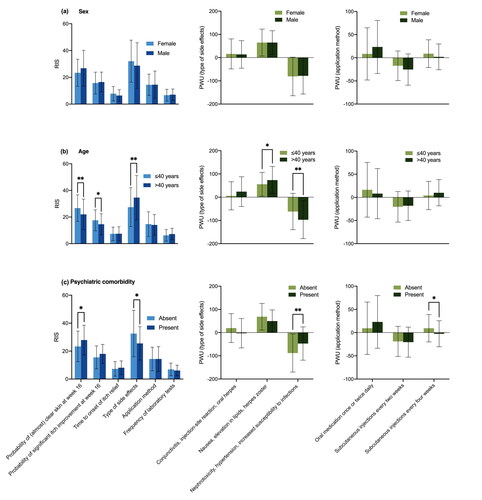
Figure 3. Treatment preferences dependent on current systemic therapy, DLQI and PO-SCORAD. (a) Patients receiving non-biologic drugs placed significantly more value on the time to onset of itch relief than others (p = 0.004 compared to patients on biologics; p = 0.002 compared to those without systemic treatment). Participants treated with biologics were more willing to accept “conjunctivitis, injection-site reaction and oral herpes” (p = 0.001 compared to non-biologic treatment; p = 0.013 compared to participants without systemic treatment). Those receiving non-biologic drugs were less interested in avoidance of “nephrotoxicity, hypertension and increased susceptibility to infections” (p = 0.039 compared to no systemic therapy; p = 0.019 compared to biologics). Compared to those without a systemic therapy, patients treated with biologics were less interested in an oral therapy (p = 0.009) and favored a subcutaneous treatment regimen more (every 2 weeks: p = 0.020; every 4 weeks: p = 0.019). Participants treated with non-biologic agents disliked a subcutaneous medication every other week more than those with biologics (p = 0.042). (b) Health-related quality of life had no significant impact on RIS. However, participants with a DLQI ≤10 attached greater importance to avoidance of “nephrotoxicity, hypertension and increased susceptibility to infections” (p = 0.015) and were more willing to accept “conjunctivitis, injection-site reaction and oral herpes” (p = 0.007). (c) PO-SCORAD >40 was associated with higher preferences for skin clearance (p = 0.015) and itch relief (p = 0.033) and less concern about the type of side effects (p = 0.026). Participants with a PO-SCORAD ≤40 worried more about “nephrotoxicity, hypertension and increased susceptibility to infections” (p = 0.004) and less about “conjunctivitis, injection-site reaction and oral herpes” (p = 0.015). Bars: means with standard deviations. DLQI: Dermatology Life Quality Index; PO-SCORAD: Patient-Oriented SCORing of Atopic Dermatitis; PWU: Part-Worth Utility; RIS: Relative Importance Scores. *p < 0.05, **p < 0.01.
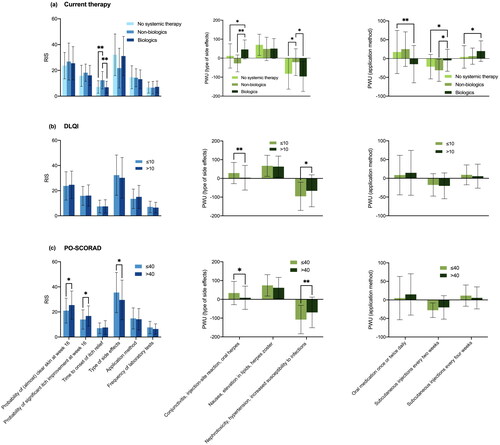
Table 4. Multivariate linear regression models assessing the impact of patient and disease characteristics on RIS of treatment attributes.
Table 5. Multivariate linear regression models assessing the impact of patient and disease characteristics on PWU for levels of the attributes “type of side effects” and “application method”.
Supplemental Material
Download PDF (526 KB)Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request. Additionally, the used model can be provided upon request.
