Abstract
Objective
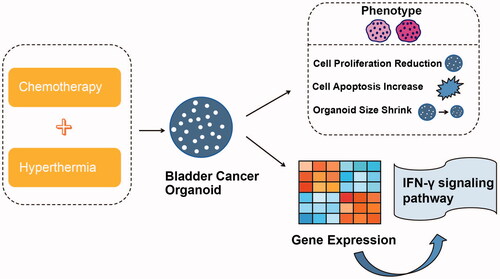
This study aimed to evaluate the combined efficacy of hyperthermia and chemotherapy using a bladder cancer organoid model and to explore hyperthermia-related molecular pathways.
Method
Tumor organoids were generated by embedding RT4 bladder cancer cells into Matrigel. The resulting organoids were treated with pirarubicin or gemcitabine at 37 °C or 42 °C. Proliferation was determined by Ki67 immunofluorescence staining, and apoptosis was assessed using a TdT-mediated dUTP nick end labeling (TUNEL) assay. RNA sequencing was used to identify the differentially expressed genes.
Results
Bladder cancer organoids were successfully established and exhibited robust proliferative abilities. Treatment with gemcitabine or pirarubicin under hyperthermic conditions caused pronounced structural damage to the organoids and increased cell death compared to that in the normothermically treated group. Furthermore, Ki67 labeling and TUNEL assays showed that the hyperthermia chemotherapy group showed a significantly reduced proliferation rate and high level of apoptosis. Finally, RNA sequencing revealed the IFN-γ signaling pathway to be associated with hyperthermia.
Conclusion
Overall, hyperthermia combined with chemotherapy exerted better therapeutic effects than those of normothermic chemotherapy in grade 1-2 non-muscle-invasive bladder cancer, potentially through activation of the IFN-γ-JAK-STAT pathway.
Introduction
Bladder cancer is a prevalent malignant tumor worldwide, and by 2023, the United States was estimated to have 82,290 new cases and 16,710 deaths of bladder cancer [Citation1]. Non-muscle-invasive bladder cancer (NMIBC) is the predominant type, accounting for 75% of all newly diagnosed bladder cancer cases [Citation2]. NMIBC has a high risk of recurrence (60%) and progression. Transurethral resection of bladder tumors (TURBT) is typically performed in patients with NMIBC. Intravesical chemotherapy or immunotherapy is recommended before or after the first-line treatment of TURBT, regardless of the NMIBC risk stratification [Citation3–5]. TURBT aims to completely remove the tumors, whereas intravesical therapy eliminates detached tumor cells and has an ablative effect on residual or unnoticed tumors. Consequently, the recurrence and progression may be reduced [Citation4,Citation6]. Currently, the Bacillus Calmette-Guérin (BCG) vaccine is the most effective intravesical immunotherapy, while mitomycin C, gemcitabine, epirubicin, and pirarubicin have emerged as common intravesical chemotherapy drugs [Citation4]. Despite adjuvant therapies, the recurrence rate of NMIBC remains high (up to 30%) [Citation5]. Further, some patients with bladder cancer do not respond to BCG. Consequently, many opt for radical cystectomy as a salvage treatment in clinical practice. However, this choice may increase the risk of patient mortality and deteriorate the patient’s quality of life post-surgery.
Multimodal combination therapy for bladder preservation has recently attracted significant attention as a research topic. The effectiveness of TURBT combined with radiotherapy and immunotherapy in patients with bladder cancer has been reported [Citation7,Citation8]. Bladder-preserving therapy has demonstrated the ability to maintain bladder function and quality of life while extending patient survival and enhancing overall quality of life [Citation9]. Several strategies have also been reported to improve the efficacy of intravesical chemotherapy, including pH adjustment, instillation duration, drug concentration, and device-assisted intravesical chemotherapy [Citation6]. Among these, hyperthermic intravesical chemotherapy (HIVEC) is promising [Citation10,Citation11], through which the temperature of the intravesical drug solution is set between 41 °C and 44 °C to synergistically maximize the efficacy of hyperthermia and chemotherapy [Citation12]. Some clinical studies were performed to show that HIVEC can reduce the recurrence rate of NMIBC more effectively than chemotherapy alone, without an increase in side effects [Citation5,Citation13], or in the case of BCG-unresponsive NMIBC [Citation14]. However, some studies have shown that HIVEC is not superior to chemotherapy under normothermic conditions [Citation10]. Thus, the additive effects of hyperthermia and chemotherapy remain controversial and need to be verified in greater depth.
Based on these findings, we aimed to investigate whether the combination of intravesical chemotherapy and hyperthermia can enhance the efficacy of bladder cancer treatment after TURBT. We generated bladder cancer organoids from RT4 cells and used these tumor organoids to assess the efficacy of hyperthermia chemotherapy and explore the underlying mechanism. The proposed model may serve as a foundation for patients considering bladder-preserving treatments.
Materials and methods
Cell lines and culture conditions
The human bladder cancer cell line RT4 originated from transitional cell papilloma tissue and was obtained from a grade 1-2 carcinoma of the bladder. RT4 cells were provided by Wuhan Procell Life Technology Co., Ltd. (CL-0431). The cells were cultured as monolayers in T-25 flasks (Corning R, New York, USA) using a specialized RT4 cell-specific medium (CM-0431; Procell, Wuhan, China) in a temperature-controlled environment at 37 °C with 5% carbon dioxide in air.
Formation of bladder cancer organoids
Matrigel (356234, BD Biosciences, NY, USA) was thawed on ice before use, then preheated in an 8-chamber Petri dish (Corning, NY, USA) in an incubator at 37 °C. The cell number was determined using a cell counting plate was and a ratio of 3000 cells per 50 µL of Matrigel was decided. An appropriate volume of the cell suspension was centrifuged at 100 × g for 15 min at 4 °C. The supernatant was removed and the centrifuge tube was placed on ice. The cells were then resuspended in corresponding amount of Matrigel. Next, 50 µL of the cell-Matrigel suspension was added to each well in an 8-chamber dish to create droplets, which was then placed in a 37 °C cell incubator for 30–40 min for Matrigel solidification. Subsequently, complete medium was added for cell culture, and the medium was changed every other day for 12 days.
Drugs and hyperthermia treatment
Cell line-derived organoids were treated with pirarubicin (1 μM and 10 μM) and gemcitabine (1 μM and 10 μM) (MedChemExpress, New Jersey, USA). PBS was used as a control. The RT4 cells were treated with 0.01 μM of pirarubicin and 0.01 μM of gemcitabine (MedChemExpress, New Jersey, USA). In the 37 °C chemotherapy group, the organoids were promptly placed in a 37 °C cell incubator after treatment. For the hyperthermia chemotherapy group, the organoids were exposed to a temperature of 42 °C for 1 h. Following the treatment, the organoids were returned to a temperature of 37 °C and cultured for 72 h. The experiments were repeated thrice for each group.
Morphology analysis
The organoids were imaged using an Observer 5 inverted microscope (Carl Zeiss AG, Germany). All images were analyzed using ImageJ software (National Institutes of Health, Bethesda, Maryland, USA). The diameter and shape parameters were measured using the ImageJ image analysis function.
HE staining and immunofluorescence staining
Organoids were fixed in 10% neutral-buffered formalin, dehydrated, and embedded in paraffin. The paraffin sections were dewaxed, rehydrated, and washed. For immunofluorescence staining, the slides were incubated in boiling citrate buffer for 60 min for antigen retrieval, blocked with 5% BSA in PBS, and incubated with primary and secondary antibodies. To assess the proliferative ability of the organoids, Ki67 antibody (27309-1-AP, Proteintech, Wuhan, China) was used as the primary antibody and Alexa Fluor 594 AffiniPure Goat Anti-Rabbit IgG(H + L) (33112ES60, Wuhan, China) was used as the secondary antibody. Nuclei were stained with 4′, 6′‐diamidino‐2‐phenylindole. A TdT-mediated dUTP nick-end labeling (TUNEL) apoptosis kit (MK1018, Bosterbio, Wuhan, China) was used to evaluate apoptosis.
RNA sequencing (RNA-seq)
RNA-seq analysis of RT4 cells was performed by Wuhan Aiji Baike Biotechnology Co., Ltd. (Wuhan, China). Total RNA was extracted using an miRNeasy Mini Kit (217004; Qiagen, Dusseldorf, Germany). RNA quality was assessed using 1% agarose gel electrophoresis and an RNA Nano 6000 Assay Kit (Agilent, 5067 1511). Genes with p < 0.05 and an absolute fold change of 1.5, were considered differentially expressed genes.
Real-time quantitative polymerase chain reaction (RT-qPCR)
In the control group, RT4 cells were treated with gemcitabine at 37 °C for 72 h. In the experimental group, RT4 cells were first treated with gemcitabine at 42 °C for 1 h and then returned to the 37 °C cell incubator for 71 hs. Total RNA was extracted using a Gene JET RNA Purification Kit (Thermo Scientific, Germany). The quantity and purity of total RNA were verified by spectroscopy (NanoDrop 1000, Thermo Scientific). Total RNA was transcribed into complementary DNA (cDNAs) using the PrimeScript RT reagent kit (11141ES60, Yeasen, Shanghai, China), and the final reaction volume was 20 µL. The cDNA was stored at −80 °C until used for qPCR. The primer sequences are listed in Supplementary Table 1.
Statistical analysis
The results were presented as the mean ± SEM for experiments. Two-tailed t-tests were used for statistical comparisons between two groups, and analysis of variance (ANOVA) followed by Tukey’s or Dunnett’s multiple comparison test was used for statistical comparisons among multiple groups. GraphPad Prism 8.0 (GraphPad Software, San Diego, CA, USA) was used for all data analyses. Statistical significance was set at p < 0.05.
Results
Establishment and characterization of bladder cancer organoids from RT4 cells
To investigate the therapeutic effects of HIVEC, we generated bladder cancer organoids and characterized them. RT4 cells are noninvasive superficial cancer cells, which were used to create organoids. We cultured RT4 cells using the designated protocol and monitored their morphological changes using a bright-field microscope as well as their proliferation status using an immunofluorescence assay (). By day 2, small spheroids were observed in the Matrigel. After a 12-day culture period, the organoids exhibited a rounded morphology and had noticeably grown larger, with diameters ranging approximately between 100–200 μm (). Hematoxylin and eosin (H&E) staining revealed that the organoid cells were arranged in a compact manner with blue nuclei, red cytoplasm, and no obvious necrosis or voids (). Most cells in the organoid were positive for Ki67, suggesting that they were proliferating cells (). Together, these results confirmed the formation of bladder cancer organoids.
Figure 1. Formation of RT4 organoid. (A) a timeline of RT4 organoid-related experiments created using BioRender.com. (B) Representative bright-field images of organoids formed from the RT4 cell line on day 2 and day 12. Scale bar, 100 μm.
(C) Representative H&E staining photomicrograph of RT4 organoids on day 12. Scale bar, 50 μm. (D) Representative immunofluorescence sections of RT4 organoids stained with Ki67 (red). Nuclei were stained with DAPI. Scale bar, 50 μm.

Hyperthermia-based chemotherapy impacts the organoid morphology and dimensions
Gemcitabine () and pirarubicin () are intravesical chemotherapeutic drugs that are commonly used in clinical practice. Therefore, these two chemotherapeutic drugs were used to assess the effects of hyperthermia chemotherapy. The drug concentrations were set at 1 μM and 10 μM, and the cultures were maintained at either 37 °C (control) or 42 °C (hyperthermia). Compared to the blank group, spherical organoids treated with gemcitabine at 37 °C were fragmented (). This effect was more pronounced in the 10 μM group, compared with that in the 1 μM gemcitabine group. Notably, organoids in the hyperthermia group exhibited significantly smaller areas than in the control group at both 1 μM and 10 μM concentrations, as shown by bright-field microscopy (). This suggested that hyperthermia induced apoptosis or necrosis. Similarly, the combination of pirarubicin and hyperthermia exerted a stronger effect on organoid growth than that of pirarubicin alone ().
Figure 2. Hyperthermia chemotherapy influences organoid shape and size. (A, B) Representative bright-field images of RT4 organoids treated with gemcitabine (0-10 μM) and pirarubicin (0-10 μM) at 37 °C and 42 °C. (C) Quantitative analysis of the organoid area in the gemcitabine and the pirarubicin group. The mean ± SEM of 6 organoids per group is shown. Two-way ANOVA analyzed the differences between groups with multiple comparisons. *p < 0.05. (D, E) Representative images with H&E staining of organoids treated with gemcitabine and pirarubicin at 37 °C and 42 °C were shown. Scale bar, 50 μm.

The organoid sections were then stained with H&E. In the control group, organoid cells exhibited a densely packed arrangement featuring blue-stained nuclei, red-stained cytoplasm, and no obvious signs of necrosis or empty spaces. However, in the hyperthermia group, the organoids exhibited shrinking spheres, some of which contained voids at the center (). Notably, hyperthermia combined with 10 μM gemcitabine resulted in significant structural damage to the organoids and substantial cell death (). Similarly, 10 μM pirarubicin combined with hyperthermia showed analogous effects on the organoids (). These results demonstrate that hyperthermia chemotherapy can significantly affect the morphology of organoids and contribute to significant intracellular cell death.
Hyperthermia-based chemotherapy restricts the proliferation of RT4 organoids
To assess organoid viability, we used Ki67, an indicator of cell proliferation. Quantification of Ki67-positive cells revealed a decrease in the proportion of proliferating cells in the organoids treated with gemcitabine (). Furthermore, a significant reduction in cell proliferation was observed after hyperthermia chemotherapy (). Likewise, compared to pirarubicin treatment alone, the combined use of pirarubicin and hyperthermia resulted in reduced Ki67 expression in the organoids (). These results indicate that hyperthermia chemotherapy can effectively inhibit cancer cell proliferation.
Figure 3. Hyperthermia chemotherapy inhibits the proliferation of RT4 organoids. (A, B) Representative immunofluorescence sections of RT4 organoids treated with gemcitabine (0-10 μM) and pirarubicin(0-10 μM) in 37 °C and 42 °C, stained with Ki67 (red). Nuclei were counterstained with DAPI. (C, D) Quantitative analysis of Ki67+ organoids per field and Ki67+ nuclei per organoid in the gemcitabine(0-10 μM) and the pirarubicin (0-10 μM) groups at 37 °C and 42 °C. Differences between groups were analyzed using two-way ANOVA with multiple comparisons. *p < 0.05, **p < 0.01. ***p < 0.001, ****p < 0.0001.

Hyperthermia-based chemotherapy accelerates apoptosis in RT4 organoids
Next, we examined apoptosis in RT4 organoids using a TUNEL assay. TUNEL staining revealed increased apoptosis in organoids treated with gemcitabine (). Notably, a considerably higher proportion of apoptotic cells was observed among organoids subjected to the combined hyperthermia and gemcitabine treatment (). Similarly, when pirarubicin alone was compared with its combination with hyperthermia, the latter showed significantly increased TUNEL-positive results within the organoids (). Taken together, these results indicate that hyperthermia chemotherapy substantially impairs tumor cell growth and promotes cell death.
Figure 4. Hyperthermia chemotherapy accelerates the apoptosis of RT4 organoids. (A, B) Representative images of TUNEL staining (green) of RT4 organoids treated with gemcitabine (0-10 μM) and pirarubicin (0-10 μM) in 37 °C and 42 °C are shown. Nuclei were stained with DAPI. (C, D) Quantitative analysis of TUNEL+ organoids per field and TUNEL+ nuclei per organoid in the gemcitabine (0-10 μM) and the pirarubicin (0-10 μM) group at 37 °C and 42 °C.The differences between groups were analyzed using two-way ANOVA with multiple comparisons. *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001.

RNA sequencing and RT-qPCR analysis of RT4 cells demonstrated differing gene expression patterns between the sets treated with gemcitabine at 37 °C and 42 °C
To reveal the underlying mechanisms of hyperthermia, we performed RNA-seq on RT4 cells in the gemcitabine group (group B) and hyperthermia with gemcitabine (group A) (). Subsequently, heat and volcano maps were drawn to present the differentially expressed genes; the results illustrated that IFNGR2 genes were expressed at low levels (). Next, we conducted gene ontology (GO) enrichment analysis to identify the potential hyperthermia-related pathways (). The analysis revealed the plasma membrane protein complex in the Cellular Component category and the interferon-gamma (IFN-γ)-mediated signaling pathway in the Biological Process category among others (). IFN-γ exhibits pro-tumor effects in diverse cancer types, including breast cancer [Citation15] and glioblastoma [Citation16]. Further, inhibition of the IFNGR-JAK2-STAT1-PARP1 pathway is promotes apoptosis in xenograft viral hepatitis-associated hepatocellular carcinoma [Citation17]. Thus, RT-qPCR was used to authenticate the downregulation of IFN-γ-JAK-STAT pathway-related genes because of hyperthermia. The expression of IFNGR2, IFN-γ, JAK1, JAK2, JAK3, and STAT1 was decreased in the hyperthermia combined with gemcitabine group, which was consistent with our expectations (). Overall, these results suggest a significant downregulation of gene expression in the IFN-γ-JAK-STAT pathway within the hyperthermia group.
Figure 5. RNA sequencing and RT-qPCR analysis of RT4 cell lines revealed differential gene expression between the groups treated with gemcitabine at 37 °C and 42 °C. (A, B) Heatmap and volcano plot illustrating the differentially expressed genes in RT4 cells between the hyperthermia with gemcitabine group (A1, A2, A3) and the gemcitabine group (B1, B2, B3). (C) Gene ontology (GO) enrichment analysis of RT4 cells treated with gemcitabine (0.01 μM) at 37 °C and 42 °C. (D) RT-qPCR assay for IFNGR2, IFN-γ, JAK1, JAK2, JAK3, and STAT1 mRNA levels. The differences between groups were analyzed using an unpaired t-test. ***p < 0.001, ****p < 0.0001.

Discussion
Despite transurethral resection of bladder tumors (TURBT) being a diagnostic and potential therapeutic procedure for NMIBC, its control remains unsatisfactory, with a 1-year recurrence rate ranging from 15–61% and a 5-year recurrence rate ranging from 31–78% [Citation18]. A radical cystectomy may be performed in severe cases [Citation3]. However, this can cause significant inconvenience to the patients. TURBT supplemented with adjuvant therapy, is currently the recommended treatment for NMIBC [Citation19]. Novel strategies, including hyperthermia, are being developed to address the high recurrence and progression rates of NMIBC [Citation20]. Hyperthermia in combination with chemotherapy has been used for many other malignant tumors and has shown synergistic benefits [Citation21]. In particular, the combination of hyperthermia and intravesical chemotherapy has been shown to significantly reduce the risk of NMIBC recurrence in certain studies [Citation5]. For example, a significantly higher 24-month recurrence-free survival (RFS) was observed in patients with intermediate- and high-risk papillary NMIBC treated with hyperthermia with mitomycin C chemotherapy than in patients treated with intravesical BCG [Citation22]. Notably, Guerrero-Ramos et al. found that patients with high-risk NMIBC in the HIVEC group had higher progression-free survival (PFS) at 24 months than that of patients in the intravesical BCG group, but the RFS was not significantly different [Citation23]. Recently, a randomized controlled trial revealed that hyperthermia combined with mitomycin C cannot be recommended over mitomycin C alone for intermediate-risk NMIBC [Citation24]. This controversial finding underscores the urgency to explore and validate the role of hyperthermic chemotherapy in NMIBC.
Validating the synergistic effect of hyperthermia and chemotherapy in NMIBC requires clinical trials as well as in vitro and in vivo animal model experiments, which remain limited. However, several studies have used bladder cancer cell lines to explore the function of hyperthermia chemotherapy and have reported a significantly enhanced cytotoxic effect of hyperthermia when combined with mitomycin-C [Citation25].
Given the limited and controversial research foundation, we used this model to further validate its feasibility and explore its mechanisms. We aimed to provide theoretical support for broader clinical applications of intravesical heat-perfused chemotherapeutic agents.
Organoids are a widely used platform for studying tissue morphogenesis, cancer heterogeneity, and drug screening [Citation26,Citation27]. Cells are typically cultured within special scaffolds to form spherical organoids [Citation28], which are composed of multiple cell types and organ structures, thus recapitulating tumor heterogeneity and the in vitro microenvironment [Citation29]. Organoids have been established from several cancers and characterized [Citation27,Citation30]. Bladder cancer organoids derived from patient tumor tissues or cell lines (RT4, T24, J82, and 5637) have been used in pathophysiological research and drug discovery [Citation28–33]. The RT4 cell line is representative of grade 1-2 NMIBC that is treated with HIVEC, and has a high incidence in clinical cases [Citation34].
In this study, we established bladder cancer organoids using RT4 cells to analyze the effects of hyperthermia chemotherapy. Organoid cultures have been successfully established for various cancers and are used to evaluate drug responses [Citation35,Citation36]. Organoids closely resemble primary tissues genetically and phenotypically, and serve as crucial models for preclinical tumor biology studies. They also have the potential to guide future precision medicine and personalized patient treatment [Citation26,Citation37]. We confirmed the efficacy of hyperthermia chemotherapy using bladder cancer organoids. This model can be repeatedly expanded and demonstrates self-renewal abilities to effectively maintain the tumor structure and microenvironment y [Citation38,Citation39]. A thorough understanding of these mechanisms may facilitate the clinical application of hyperthermia chemotherapy. In general, direct cytotoxic effects boost immune responses, and an increased vascular supply is beneficial for integrating hyperthermia with chemotherapy [Citation21,Citation40]. These cytotoxic effects may be attributed to cell cycle arrest, reduced RNA and DNA synthesis, and DNA repair impairment [Citation40]. Other heat-related stress responses, including heat shock proteins and immune cell activation also play critical roles in antitumor processes [Citation40]. Previous studies have indicated that hyperthermia leads to cell apoptosis and necrosis owing to the direct denaturation of intracellular proteins and immune toxicity induced by the release of heat shock proteins [Citation10,Citation41]. Consistent with these findings, increased levels of apoptosis were observed in organoids treated with both hyperthermia and chemotherapeutic drugs. One explanation for this observation is that hyperthermia can increase drug solubility, cell membrane penetration, and drug absorption [Citation5,Citation12,Citation41,Citation42].
Specifically, the mechanisms of hyperthermia may involve the AKT, ERK, AMPKa, ATM, mTOR, ATF6, and PERK signaling pathways [Citation43–47]. In our study, we discovered that the IFN-γ-JAK-STAT pathway is significantly associated with hyperthermia, enriching its molecular regulatory network.
In conclusion, TURBT supplemented with hyperthermic chemotherapy is feasible for treating grade 1-2 NMIBC, and avoiding the inconvenience caused to patients by radical cystectomy. This study confirmed the effective impact of hyperthermia chemotherapy on grade 1-2 NMIBC using an RT4 organoid model, and identified differentially expressed genes associated with this treatment on the IFN-γ-JAK-STAT pathway. However, we only choose the RT4 cell line to construct the organoid model, which can only indicate hyperthermia chemotherapy efficacy in grade 1-2 NMIBC. For grade 3 NMIBC, we can’t conclude. Overall, this study provides more evidence regarding the mechanism of action of this treatment modality, especially in cases characterized by relatively mild-to-moderate dysplasia. These findings have the potential to offer a clearer therapeutic direction to the medical community and provide robust support for the formulation of personalized treatment plans by healthcare professionals.
Authors contributions
Y.X. and G.S. conceptualized the study. Experiments were conducted by Y.X. and T.Y. Organoid culture technique was guided by H.L. Manuscript drafting was done by G.S. and Y.X. Data analysis was contributed by Y.X. and P.H. Manuscript revision for substantial intellectual content was undertaken by H.Z., C.L. and H.L. All coauthors participated in manuscript editing.
Supplemental Material
Download Zip (3.6 MB)Acknowledgments
We thank Suzhou OptoMedic Technologies Inc. for their equipment support.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
All data presented in this study can be accessed upon inquiry to the corresponding author.
Additional information
Funding
References
- Siegel RL, Miller KD, Wagle NS, et al. Cancer statistics, 2023. CA Cancer J Clin. 2023;73(1):1–10. doi:10.3322/caac.21763.
- Burger M, Catto JWF, Dalbagni G, et al. Epidemiology and risk factors of urothelial bladder cancer. Eur Urol. 2013;63(2):234–241. doi:10.1016/j.eururo.2012.07.033.
- Woldu SL, Bagrodia A, Lotan Y. Guideline of guidelines: non-muscle-invasive bladder cancer. BJU Int. 2017;119(3):371–380. doi:10.1111/bju.13760.
- Lenis AT, Lec PM, Chamie K, et al. Bladder cancer: a review. Jama. 2020;324(19):1980–1991. doi:10.1001/jama.2020.17598.
- Liu K, Zhu J, Song Y-X, et al. Thermal intravesical chemotherapy reduce recurrence rate for non-muscle invasive bladder cancer patients: a meta-analysis. Front Oncol. 2020;10:29. doi:10.3389/fonc.2020.00029.
- Babjuk M, Burger M, Capoun O, et al. European association of urology guidelines on non-muscle-invasive bladder cancer (ta, T1, and carcinoma in situ). Eur Urol. 2022;81(1):75–94. doi:10.1016/j.eururo.2021.08.010.
- Feifer AH, Taylor JM, Tarin TV, et al. Maximizing cure for muscle-invasive bladder cancer: integration of surgery and chemotherapy. Eur Urol. 2011;59(6):978–984. doi:10.1016/j.eururo.2011.01.014.
- Efstathiou JA, Mouw KW, Gibb EA, et al. Impact of immune and stromal infiltration on outcomes following bladder-sparing trimodality therapy for Muscle-Invasive bladder cancer. Eur Urol. 2019;76(1):59–68. doi:10.1016/j.eururo.2019.01.011.
- Ploussard G, Daneshmand S, Efstathiou JA, et al. Critical analysis of bladder sparing with trimodal therapy in muscle-invasive bladder cancer: a systematic review. Eur Urol. 2014;66(1):120–137. doi:10.1016/j.eururo.2014.02.038.
- Angulo JC, Álvarez-Ossorio JL, Domínguez-Escrig JL, et al. Hyperthermic mitomycin C in intermediate-risk non-muscle-invasive bladder cancer: results of the HIVEC-1 trial. Eur Urol Oncol. 2023;6(1):58–66. doi:10.1016/j.euo.2022.10.008.
- Plata A, et al. Long-Term experience with hyperthermic chemotherapy (HIVEC) using mitomycin-C in patients with non-muscle invasive bladder cancer in Spain. J Clin Med. 2021;10(21):5105.
- Lammers RJM, Witjes JA, Inman BA, et al. The role of a combined regimen with intravesical chemotherapy and hyperthermia in the management of non-muscle-invasive bladder cancer: a systematic review. Eur Urol. 2011;60(1):81–93. doi:10.1016/j.eururo.2011.04.023.
- Ruan Q, Ding D, Wang B, et al. A multi-institutional retrospective study of hyperthermic plus intravesical chemotherapy versus intravesical chemotherapy treatment alone in intermediate and high risk nonmuscle-invasive bladder cancer. Cancer Biol Med. 2021;18(1):308–317. doi:10.20892/j.issn.2095-3941.2020.0125.
- Álvarez-Maestro M, Guerrero-Ramos F, Rodríguez-Faba O, et al. Current treatments for BCG failure in non-muscle invasive bladder cancer (NMIBC). Actas Urol Esp (Engl Ed. 2021;45(2):93–102.), doi:10.1016/j.acuroe.2020.08.011.
- Singh S, Kumar S, Srivastava RK, et al. Loss of ELF5-FBXW7 stabilizes IFNGR1 to promote the growth and metastasis of triple-negative breast cancer through interferon-γ signalling. Nat Cell Biol. 2020;22(5):591–602. doi:10.1038/s41556-020-0495-y.
- Khan S, Mahalingam R, Sen S, et al. Intrinsic interferon signaling regulates the cell death and mesenchymal phenotype of glioblastoma stem cells. Cancers (Basel). 2021;13(21):5284. doi:10.3390/cancers13215284.
- Cherng Y-G, Chu YC, Yadav VK, et al. Induced mitochondrial alteration and DNA damage via IFNGR-JAK2-STAT1-PARP1 pathway facilitates viral hepatitis associated hepatocellular carcinoma aggressiveness and stemness. Cancers (Basel). 2021;13(11):2755. doi:10.3390/cancers13112755.
- Teoh JY-C, Kamat AM, Black PC, et al. Recurrence mechanisms of non-muscle-invasive bladder cancer - a clinical perspective. Nat Rev Urol. 2022;19(5):280–294. doi:10.1038/s41585-022-00578-1.
- Zeng N, Xu M-Y, Sun J-X, et al. Hyperthermia intravesical chemotherapy acts as a promising alternative to bacillus Calmette-Guérin instillation in non-muscle-invasive bladder cancer: a network meta-analysis. Front Oncol. 2023;13:1164932. doi:10.3389/fonc.2023.1164932.
- Snider JW, 3rd, Datta NR, Vujaskovic Z. Hyperthermia and radiotherapy in bladder cancer. Int J Hyperthermia. 2016;32(4):398–406. doi:10.3109/02656736.2016.1150524.
- Rao W, Deng ZS, Liu J. A review of hyperthermia combined with radiotherapy/chemotherapy on malignant tumors. Crit Rev Biomed Eng. 2010;38(1):101–116. doi:10.1615/critrevbiomedeng.v38.i1.80.
- Arends TJH, Witjes JA. Results of a randomised controlled trial comparing intravesical chemohyperthermia with mitomycin C versus bacillus Calmette-Guérin for adjuvant treatment of patients with intermediate- and high-risk Non-Muscle-invasive bladder cancer. Eur Urol. 2016;75(2):e26–1052. doi:10.1016/j.eururo.2016.01.006.
- Guerrero-Ramos F, González-Padilla DA, González-Díaz A, et al. Recirculating hyperthermic intravesical chemotherapy with mitomycin C (HIVEC) versus BCG in high-risk non-muscle-invasive bladder cancer: results of the HIVEC-HR randomized clinical trial. World J Urol. 2022;40(4):999–1004. doi:10.1007/s00345-022-03928-1.
- Tan WS, Prendergast A, Ackerman C, et al. Adjuvant intravesical chemohyperthermia versus passive chemotherapy in patients with intermediate-risk non-muscle-invasive bladder cancer (HIVEC-II): a phase 2, open-label, randomised controlled trial. Eur Urol. 2023;83(6):497–504. doi:10.1016/j.eururo.2022.08.003.
- van der Heijden AG, Jansen CFJ, Verhaegh G, et al. The effect of hyperthermia on mitomycin-C induced cytotoxicity in four human bladder cancer cell lines. Eur Urol. 2004;46(5):670–674. doi:10.1016/j.eururo.2004.06.009.
- Medle B, Sjödahl G, Eriksson P, et al. Patient-derived bladder cancer organoid models in tumor biology and drug testing: a systematic review. Cancers (Basel). 2022;14(9):2062. doi:10.3390/cancers14092062.
- Sun G, Ding B, Wan M, et al. Formation and optimization of three-dimensional organoids generated from urine-derived stem cells for renal function in vitro. Stem Cell Res Ther. 2020;11(1):309. doi:10.1186/s13287-020-01822-4.
- Whyard T, Liu J, Darras FS, et al. Organoid model of urothelial cancer: establishment and applications for bladder cancer research. Biotechniques. 2020;69(3):193–199. doi:10.2144/btn-2020-0068.
- Amaral RLF, Miranda M, Marcato PD, et al. Comparative analysis of 3D bladder tumor spheroids obtained by forced floating and hanging drop methods for drug screening. Front Physiol. 2017;8:605. doi:10.3389/fphys.2017.00605.
- Lee SH, Hu W, Matulay JT, et al. Tumor evolution and drug response in patient-derived organoid models of bladder cancer. Cell. 2018;173(2):515–528.e17. doi:10.1016/j.cell.2018.03.017.
- Roelants M, Van Cleynenbreugel B, Van Poppel H, et al. Use of fluorescein isothiocyanate-human serum albumin for the intravesical photodiagnosis of non-muscle-invasive bladder cancer: an in vitro study using multicellular spheroids composed of normal human urothelial and urothelial cell carcinoma cell lines. BJU Int. 2011;108(3):455–459. doi:10.1111/j.1464-410X.2010.09951.x.
- Palmer S, Litvinova K, Dunaev A, et al. Changes in autofluorescence based organoid model of muscle invasive urinary bladder cancer. Biomed Opt Express. 2016;7(4):1193–1200. doi:10.1364/BOE.7.001193.
- Ringuette Goulet C, Bernard G, Chabaud S, et al. Tissue-engineered human 3D model of bladder cancer for invasion study and drug discovery. Biomaterials. 2017;145:233–241. doi:10.1016/j.biomaterials.2017.08.041.
- Ezeabikwa B, Mondal N, Antonopoulos A, et al. Major differences in glycosylation and fucosyltransferase expression in low-grade versus high-grade bladder cancer cell lines. Glycobiology. 2021;31(11):1444–1463. doi:10.1093/glycob/cwab083.
- Dekkers JF, van Vliet EJ, Sachs N, et al. Long-term culture, genetic manipulation and xenotransplantation of human normal and breast cancer organoids. Nat Protoc. 2021;16(4):1936–1965. doi:10.1038/s41596-020-00474-1.
- Ubink I, Bolhaqueiro ACF, Elias SG, et al. Organoids from colorectal peritoneal metastases as a platform for improving hyperthermic intraperitoneal chemotherapy. Br J Surg. 2019;106(10):1404–1414. doi:10.1002/bjs.11206.
- Minoli M, Cantore T, Hanhart D, et al. Bladder cancer organoids as a functional system to model different disease stages and therapy response. Nat Commun. 2023;14(1):2214. doi:10.1038/s41467-023-37696-2.
- Kim YS, Hsieh AC, Lam HM. Bladder cancer patient-derived organoids and avatars for personalized cancer discovery. Eur Urol Focus. 2022;8(3):657–659. doi:10.1016/j.euf.2022.07.006.
- Mullenders J, de Jongh E, Brousali A, et al. Mouse and human urothelial cancer organoids: a tool for bladder cancer research. Proc Natl Acad Sci U S A. 2019;116(10):4567–4574. doi:10.1073/pnas.1803595116.
- Owusu RA, Abern MR, Inman BA. Hyperthermia as adjunct to intravesical chemotherapy for bladder cancer. Biomed Res Int. 2013;2013:262313–262317. doi:10.1155/2013/262313.
- Tan WS, Kelly JD. Intravesical device-assisted therapies for non-muscle-invasive bladder cancer. Nat Rev Urol. 2018;15(11):667–685. doi:10.1038/s41585-018-0092-z.
- Conroy S, Pang K, Jubber I, et al. Hyperthermic intravesical chemotherapy with mitomycin-C for the treatment of high-risk non-muscle-invasive bladder cancer patients. BJUI Compass. 2023;4(3):314–321. doi:10.1002/bco2.203.
- Wan J, Wu W. Hyperthermia induced HIF-1a expression of lung cancer through AKT and ERK signaling pathways. J Exp Clin Cancer Res. 2016;35(1):119. doi:10.1186/s13046-016-0399-7.
- Zhang J-F, Yan X-M, Lan B, et al. Molecular mechanisms of synergistic induction of apoptosis by the combination therapy with hyperthermia and cisplatin in prostate cancer cells. Biochem Biophys Res Commun. 2016;479(2):159–165. doi:10.1016/j.bbrc.2016.08.060.
- Zhao Y-Y, Wu Q, Wu Z-B, et al. Microwave hyperthermia promotes caspase‑3-dependent apoptosis and induces G2/M checkpoint arrest via the ATM pathway in non‑small cell lung cancer cells. Int J Oncol. 2018;53(2):539–550. doi:10.3892/ijo.2018.4439.
- Abolhasani Zadeh F, AkbariRad M, Lian H, et al. Cellular and molecular mechanism of cell proliferation in human gastric cancer drug-Resistant cells after hyperthermia and cisplatin: role of mRNAs and Long-Non-coding RNAs. Turk J Gastroenterol. 2022;33(5):377–386. doi:10.5152/tjg.2022.20845.
- Qin D-Z, Cai H, He C, et al. Melatonin relieves heat-induced spermatocyte apoptosis in mouse testes by inhibition of ATF6 and PERK signaling pathways. Zool Res. 2021;42(4):514–524. doi:10.24272/j.issn.2095-8137.2021.041.