Abstract
Background and Objectives
Benign pigmented lesions and a general uneven tone in people with skin of color are growing issues that have been presented to dermatologists. To the best of our knowledge, this is the first controlled study to examine the efficacy and safety of using the newly introduced 785 nm neodymium-doped yttrium aluminum garnet (Nd:YAG) picosecond laser to treat facial benign pigmented lesions in Asian patients with diffractive lens array.
Materials and Methods
A 785 nm Nd:YAG picosecond laser was used to treat 15 healthy female volunteers older than 18 years who had Fitzpatrick skin types II–IV and facial benign pigmented lesions. Each volunteer received five weekly treatments in dual modes. The clinical improvement was assessed by independent investigators and by objectively measuring the melanin index.
Results
After the treatment, the melanin and erythema indices decreased, and the pigmented lesions showed clinical improvements. No serious adverse effects were observed during the study period.
Conclusions
A 785 nm Nd:YAG picosecond laser may be safe and effective in treating facial benign pigmented lesions in Asian skin.
Keywords:
Introduction
Benign pigmented lesions, or a general uneven tone in people with skin of color, are common and growing concerns that have been presented to dermatologists (Citation1). They are characterized by brown to grayish patches mainly in the periorbital and zygomatic areas on the face (Citation2). They can not only cause significant cosmetic disfigurement but also have a negative emotional impact. This disfiguring hyperpigmentation is one of the most notable manifestations of photoaging caused by chronic exposure to the sun, particularly in Asian skin.
Since the first use of the Q-switched (QS) neodymium-doped yttrium aluminum garnet (Nd:YAG) laser for pigmentation, numerous laser technologies have been used to treat hyperpigmentation in the cosmetic field over the past 25 years (Citation3). Various laser modalities, such as QS Nd:YAG (532 nm), QS alexandrite (755 nm), intense pulsed light, and QS ruby (694 nm) lasers, have been reported to be effective in treating pigmented lesions (Citation4). However, Asians with dark skin are likely to experience postinflammatory hyperpigmentation and/or lesion worsening after receiving laser treatment (Citation5–7).
Picosecond Nd:YAG lasers have recently become commercially available (Citation8). Picosecond lasers can generate high peak powers and high photomechanical effects with low undesirable heat diffusion into neighboring tissues owing to their short pulse duration, which can be as fast as 450 picoseconds in the sub-nanosecond range (Citation9). This advantage makes it possible to minimize the risk of epidermal injury and dyspigmentation (Citation10,Citation11). However, there is a lack of controlled studies regarding the efficacy of picosecond lasers in treating pigmentary disorders, particularly in the Asian population. To the best of our knowledge, this is the first controlled study to examine the efficacy and safety of using the newly introduced 785 nm Nd:YAG picosecond laser to treat facial benign pigmented lesions in Asian patients.
Materials and methods
Participants
This study involved 15 healthy female participants older than 18 years who had Fitzpatrick skin types II–IV and had visited Chung-Ang University Hospital because of facial benign pigmented lesions. This study excluded participants who were photosensitive or receiving medications to induce photosensitivity, participants who had an active sun tan, and participants who had applied a laser procedure, chemical peels, or lightening creams to the treatment area within the past six months. Patients who were either pregnant or lactating were also excluded. All participants voluntarily agreed to participate in this study and provided written informed consent. They were allowed to withdraw from this study at any time.
Treatment protocols
A picosecond Nd:YAG laser with a 785 nm wavelength (600 picoseconds, Helios IV 785™; Laseroptek, Seongnam, Korea) was used in this study. No participant received topical anesthesia. The participants received treatment in dual modes: one pass with a Dia-Fractional 785 nm handpiece that creates a diffractive optical element (DOE)-fractionated microbeam with a fluence of 0.8 J/cm2, a spot size of 5 × 5 mm, and a frequency of 10 Hz on the entire face and another pass with a 785 nm collimator handpiece with a fluence of 0.3–0.4 J/cm2, a spot size of 7 × 7 mm, and a frequency of 10 Hz on the entire face. A cooling mask was applied for 15 min to reduce the feeling of heating sense after laser treatment. Each participant received five weekly treatment sessions in total and was followed up four weeks after the last treatment. Throughout the entire study duration, patients were instructed to refrain from excessive sun or heat exposure, as well as from rubbing or scratching the treated areas. Additionally, they were advised to use hats, parasols, and broad-spectrum sunscreen with SPF 50+.
Assessment
A digital camera was used to obtain standard clinical photographs at the baseline, at each visit before treatment, and four weeks after the end of treatment. Two blinded independent dermatologists assigned scores to the photographs to determine the clinical improvement rates. The scale ranged from one (significantly aggravated) to five (significantly improved) points. Patient satisfaction was assessed after the completion of all sessions (1: very unsatisfied, 2: unsatisfied, 3: neutral, 4: satisfied, and 5: very satisfied). Any adverse reactions were also assessed on each visit.
The photographs of each participant were obtained using a Mark-Vu® skin diagnosis imaging system (PSI PLUS, Suwon, Republic of Korea). The system generated photos under four different lightening conditions: normal light, specular light, polarized light, and ultraviolet light. It also provided the brown and erythema indices, which determined skin color. The melanin index skin parameter was evaluated in vivo using Mexameter MX18® (Courage + Khazaka Electronic GmbH, Köln, Germany).
Statistical analysis
Statistical analyses were performed using GraphPad PRISM® version 8.0.2 (GraphPad Software Inc., San Diego, CA, USA). Repeated measures ANOVA with Bonferroni correction and Friedman’s multiple comparison test were used to assess changes in normally distributed variables and non-normally distributed groups, respectively. A paired t-test and Wilcoxon’s signed-rank test were used to compare outcomes before and after treatments. The data were presented as mean ± standard deviation. Additionally, p-values < 0.05 were considered statistically significant.
Results
We enrolled 15 female Korean participants in this study, and all of them completed the entire protocol without withdrawing. The statistical analysis comprised 15 participants with a mean age of 51.2 ± 9.21 (range: 40–67). Twelve participants had Fitzpatrick skin type III, two participants had type II, and one participant had type IV (). All of the enrolled participants had no other medical history.
Table 1. Demographic characteristics of the participants.
Clinical improvements in pigmentation
The standardized digital clinical photographs revealed clinical improvements in the facial benign pigmented lesions (). In the eighth week, the independent dermatologists assigned an average score of 4.07 ± 0.59, which indicated a moderate to significant improvement in pigmentation. Moreover, 86.7% of the participants reported being extremely satisfied with the result, with an average score of 4.67 ± 0.72 ().
Figure 1. (A, B, C). Clinical photographs of three representative cases showing significant improvements in pigmentary lesions after four treatment sessions with the 785 nm picosecond Nd:YAG laser.
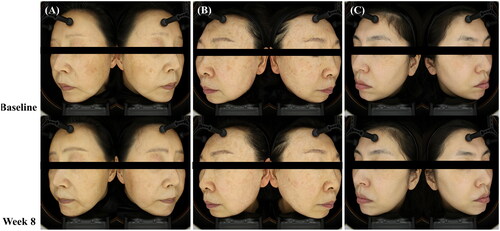
Figure 2. Evaluation of the effects of 785 nm picosecond Nd:YAG laser treatment on the (A) skin melanin index, (B) erythema index, and (C) brown index at weeks 1, 2, 3, 4, and 8 (*p < 0.05, **p < 0.01, and ***p < 0.001 by repeated measures ANOVA and post hoc Bonferroni correction).
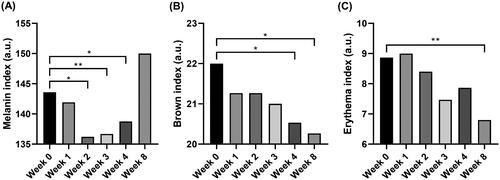
Table 2. Satisfaction of the participants.
Reduction in pigment-related skin parameters
The average melanin index value measured with the Mexameter® was 143.60 ± 31.74 at the baseline, but it decreased to 138.76 ± 32.15 (p = 0.024) at the end of the treatment sessions. The average brown index value measured using Mark-Vu® was 22.00 ± 5.33 at the baseline, but it decreased to 20.27 ± 4.92 after eight weeks (p = 0.029). The average erythema index value measured using Mark-Vu® was 8.87 ± 3.93 at the baseline, but it decreased to 6.80 ± 3.03 on the eighth week (p = 0.005). All skin parameters are shown in .
Safety issues
There were no side effects other than mild pain during the laser treatment and transient erythema immediately following the procedure. All transient erythema and pain resolved after the cooling mask application. Serious adverse effects, such as scarring, secondary infections, or ulceration, were not observed during any treatment sessions or the follow-up period.
Discussion
Picosecond lasers were initially developed to remove tattoos more efficiently than traditional nanosecond domain lasers by breaking nano-sized tattoo ink particles that had aggregated in macrophages and fibroblasts (Citation12). Recently, picosecond lasers with wavelengths of 755 nm, 532 nm, and 1064 nm have proven to be effective in removing benign epidermal and dermal pigmented lesions, such as solar lentigines, freckles, Ota nevus, and melasma, with relatively low risk of side effects (Citation13,Citation14). However, owing to the limited available studies in the literature, further studies are still required to determine the efficacy and safety of picosecond lasers in patients with benign pigmentation.
Picosecond lasers produce fine-tuned and precisely focused energy without inflicting collateral thermal damage to adjacent tissues (Citation9). Picosecond lasers have short recovery times and few adverse effects, such as scarring or burns, because their interaction with tissues is more photomechanical than photothermal (Citation10). However, postinflammatory hyperpigmentation remains a concern when treating pigmented lesions in dark skin, even with a short pulse.
The 785-nm laser beam is characterized by lower absorption by melanin compared to the 532 nm wavelength. However, it is also less absorbed by hemoglobin. This results in a favorable melanosome-to-blood absorption ratio, thereby reducing the risk of microhemorrhages/purpura and post-inflammatory pigmentation (Citation15,Citation16). This is why the 785 nm picosecond laser is recommended for treating lentigines in individuals with darker skin tones (Citation17).
This study re-confirmed that 785 nm picosecond lasers can significantly improve benign pigmentation in Asian skin without causing postinflammatory hyperpigmentation or mottled hypopigmentation.
Both unfractionated and fractionated handpieces were used in this study, as in the previous case series, non-fractionated picosecond lasers generate acoustic shock waves within the target chromophore. The benefit is that the target chromophore is fragmented and removed by macrophages, but thermal damage is minimal in the surrounding tissue. The fractionated laser beam creates numerous microbeams with high peak energy, causing microdamage to the epidermis and dermis. This localized damage is associated with fragmentation of the melanin pigment and remodeling of skin dermal components, and requires less downtime after treatment than conventional lasers (Citation16). Therefore, fractionated picosecond lasers have been reported to be effective in treating melasma (Citation17). The two different beams work by different mechanisms and can have synergistic effects.
In addition, dual mode treatment was performed because the combination of both lasers can lower the peak energy than each laser alone, reducing the possibility of potential side effects (Citation18,Citation19). Cryotherapy can also be considered as an option because it has a synergistic effect with laser in pigmentation treatment, allowing lower laser fluence or greater effect with the same parameter (Citation20). DOEs, which are used to create fractionated arrays, are believed to achieve a more constant delivery of uniformly distributed microbeams than conventional microlens arrays (MLAs). In an ex vivo study on porcine skin, a DOE-assisted 1064 nm fractionated picosecond laser generated more homogeneous microbeams on the surface of the target area and had a higher density of tiny laser-induced vacuoles in the dermis than MLA-assisted irradiation (Citation21). 785 nm picosecond lasers would also induce similar histological changes; however, further ex vivo and in vivo studies are required to confirm this hypothesis.
While the erythema index did not show an increase and even decreased, the underlying mechanism remains unclear. Reports on skin rejuvenation using the 785-nm fractional laser have suggested that this effect might have contributed to the observed outcomes (Citation22).
The limitations of this study are: 1) small sample size, 2) only female patients were included, 3) no comparison to conventional laser, 4) histological changes were not identified, so an accurate diagnosis could not be made, and 5) the study started in the winter and continued through the summer, resulting in increased UV exposure. Limitations 1)-to- 4) are due to the fact that this study was a pilot study and then should be handled in further large sample study. The increase in the melanin index at week 8 is likely due to an error by the examiner in measuring some of the deterioration caused by increased UV exposure. The melanin index measures the pigment in three specific points and calculates the average value, while the brown index measures the average pigment in the entire face. The decrease in the brown index indicates that the overall pigment is not deteriorating. To minimize this error, we should consider increasing the number of points when measuring the melanin index. To the best of our knowledge, this study is the first controlled study to examine the efficacy and safety of the newly introduced 785-nm Nd:YAG fractionated, especially diffuse lens array, and unfractionated picosecond lasers in treating facial benign pigmented lesions in Asian patients. Remarkable improvements in pigmentary lesions and a significant reduction in the melanin index were achieved without any adverse effects. The 785 nm picosecond laser may be a new option for treating patients with melasma, especially those who have not responded to conventional laser therapy. Further prospective and comparative studies should be conducted to provide additional insight into the potential clinical applications of 785 nm picosecond lasers.
Ethical approval
This study’s protocol was approved by the Institutional Review Board of Chung-Ang University Hospital (IRB Approval No. 2112-028-489). All participants signed a photo release consent form authorizing the reproduction and distribution of any images collected during the study.
Disclosure statement
Dr. Kui Young Park works as a consultant and speaker for Laseroptek Inc. The remaining authors have no conflicts of interest to declare.
Data availability statement
The data that support the findings of this study are available from the corresponding author, PKY, upon reasonable request.
Additional information
Funding
References
- Vashi NA, Kundu RV. Facial hyperpigmentation: causes and treatment. Br J Dermatol. 2013; 169 Suppl 3:1–5. doi: 10.1111/bjd.12536.
- Won KH, Lee SH, Lee MH, et al. A prospective, split-face, double-blinded, randomized study of the efficacy and safety of a fractional 1064-nm Q-switched Nd: YAG laser for photoaging-associated mottled pigmentation in Asian skin. J Cosmet Laser Ther. 2016; 18(7):381–386. doi: 10.1080/14764172.2016.1191645.
- Anderson RR, Margolis RJ, Watenabe S, et al. Selective photothermolysis of cutaneous pigmentation by Q-switched Nd: YAG laser pulses at 1064, 532, and 355 nm. J Invest Dermatol. 1989; 93(1):28–32. doi: 10.1111/1523-1747.ep12277339.
- Kung KY, Shek SY, Yeung CK, et al. Evaluation of the safety and efficacy of the dual wavelength picosecond laser for the treatment of benign pigmented lesions in Asians. Lasers Surg Med. 2019; 51(1):14–22. doi: 10.1002/lsm.23028.
- Goldberg DJ. Benign pigmented lesions of the skin. Treatment with the Q-switched ruby laser. J Dermatol Surg Oncol. 1993; 19(4):376–379. doi: 10.1111/j.1524-4725.1993.tb00360.x.
- Murphy MJ, Huang MY. Q-switched ruby laser treatment of benign pigmented lesions in Chinese skin. Ann Acad Med Singap. 1994; 23(1):60–66.
- Wang CC, Sue YM, Yang CH, et al. A comparison of Q-switched alexandrite laser and intense pulsed light for the treatment of freckles and lentigines in Asian persons: a randomized, physician-blinded, split-face comparative trial. J Am Acad Dermatol. 2006;54(5):804–810. doi: 10.1016/j.jaad.2006.01.012.
- Choi YJ, Nam JH, Kim JY, et al. Efficacy and safety of a novel picosecond laser using combination of 1 064 and 595 nm on patients with melasma: a prospective, randomized, multicenter, split-face, 2% hydroquinone cream-controlled clinical trial. Lasers Surg Med. 2017; 49(10):899–907. doi: 10.1002/lsm.22735.
- Kim YJ, Suh HY, Choi ME, et al. Clinical improvement of photoaging-associated facial hyperpigmentation in Korean skin with a picosecond 1064-nm neodymium-doped yttrium aluminum garnet laser. Lasers Med Sci. 2020; 35(7):1599–1606. doi: 10.1007/s10103-020-03008-z.
- Ross V, Naseef G, Lin G, et al. Comparison of responses of tattoos to picosecond and nanosecond Q-switched neodymium: YAG lasers. Arch Dermatol. 1998; 134(2):167–171. doi: 10.1001/archderm.134.2.167.
- Negishi K, Akita H, Matsunaga Y. Prospective study of removing solar lentigines in Asians using a novel dual-wavelength and dual-pulse width picosecond laser. Lasers Surg Med. 2018; 50(8):851–858. doi: 10.1002/lsm.22820.
- Kauvar ANB, Sun R, Bhawan J, et al. Treatment of facial and non-facial lentigines with a 730 nm picosecond titanium: sapphire laser is safe and effective. Lasers Surg Med. 2022; 54(1):89–97. doi: 10.1002/lsm.23450.
- Yu W, Zhu J, Yu W, et al. A split-face, single-blinded, randomized controlled comparison of alexandrite 755-nm picosecond laser versus alexandrite 755-nm nanosecond laser in the treatment of acquired bilateral nevus of ota-like macules. J Am Acad Dermatol. 2018; 79(3):479–486. doi: 10.1016/j.jaad.2017.12.053.
- Alegre-Sanchez A, Jimenez-Gomez N, Moreno-Arrones OM, et al. Treatment of flat and elevated pigmented disorders with a 755-nm alexandrite picosecond laser: clinical and histological evaluation. Lasers Med Sci. 2018; 33(8):1827–1831. doi: 10.1007/s10103-018-2459-z.
- Lee SJ, Han HS, Hong JK, et al. Successful treatment of pigmentary disorders in asians with a novel 730-nm picosecond laser. Lasers Surg Med. 2020; 52(10):923–927. doi: 10.1002/lsm.23261.
- Loh TY, Wu DC. Novel application of the 730 and 785 nm picosecond titanium sapphire lasers for the treatment of nevus of ota. Lasers Surg Med. 2021; 53(9):1141–1145. doi: 10.1002/lsm.23396.
- Murray T, Wu D, Boen M. Algorithmic approach to the treatment of solar lentigines with picosecond lasers. Lasers Surg Med. 2023; 55(8):712–714. doi: 10.1002/lsm.23701.
- Kang H, Kim J, Goo B. The dual toning technique for melasma treatment with the 1064 nm Nd: YAG laser: a preliminary study. Laser Ther. 2011;20(3):189–194. doi: 10.5978/islsm.20.189.
- Choi CP, Yim SM, Seo SH, et al. Retrospective analysis of melasma treatment using a dual mode of low-fluence Q-switched and long-pulse Nd: YAG laser vs. low-fluence Q-switched Nd: YAG laser monotherapy. J Cosmet Laser Ther. 2015; 17(1):2–8. doi: 10.3109/14764172.2014.957217.
- Park JW, Han HS, Koh YG, et al. Split-face comparative trial of 785-nm picosecond neodymium:yttrium-aluminum-garnet laser and precision cryotherapy combination treatment for facial benign pigmented lesions. Dermatol Ther. 2022; 35(2):e15240.
- Kim H, Hwang JK, Jung M, et al. Laser-induced optical breakdown effects of micro-lens arrays and diffractive optical elements on ex vivo porcine skin after 1064 nm picosecond laser irradiation. Biomed Opt Express. 2020; 11(12):7286–7298. doi: 10.1364/BOE.410991.
- Hur H, Choi KH, Hyun DN, et al. The treatment of dilated follicular orifices, depressive acne scars and facial wrinkles using a 785nm picosecond laser. Int J Curr Res Life Sci. 2018;7(02):1139–1143.

