Abstract
Purpose: Trichodysplasia spinulosa (TS) is a rare, disfiguring skin condition which presents with widespread asymptomatic or pruritic, skin-colored papules with white protruding keratin spiculations in immunocompromised individuals. Due to its rarity, there is little data to guide treatment decisions. The purpose of this article is to report a case of TS that completely resolved after treatment with topical cidofovir.Materials and methods: A 19-year-old immunosuppressed female presented with widespread painful, itchy bumps on the nose and face. Upon examination, there were erythematous papules with hyperkeratinized spicules affecting the central face. Biopsy of the lesions was consistent with TS which was confirmed via PCR analysis. The tenderness of this patient’s eruption was highly atypical for TS. Once daily topical application of compounded 1% cidofovir cream was prescribed.Results: The patient’s symptoms resolved completely after 4 weeks of therapy with topical cidofovir 1% cream, without reduction of immunosuppression.Conclusions: Topical cidofovir 1% cream may be a valuable treatment for this rare disease.
Introduction
TS is a rare, disfiguring skin condition with fewer than 40 reported cases. It usually presents as widespread, asymptomatic or pruritic, skin-colored, folliculocentric papules with white protruding keratin spiculations, affecting the central face and ears more commonly than the extremities, trunk, and scalp. There is no standard treatment regimen. It is caused by TSPyV, an opportunistic pathogen, and exclusively affects immunocompromised individuals (Citation1). This case describes the successful use of topical cidofovir to treat a particularly rare presentation of painful TS.
Case description
A 19-year-old female with a history of depression, anxiety, and acute systolic heart failure status post orthotopic heart transplant 8 months prior presented to the dermatology clinic with a three-month history of painful, itchy bumps affecting the face. She reported that the pain was exacerbated by manipulating the lesions. She had been prescribed oral isotretinoin for concurrent acne vulgaris but had discontinued the medication one month prior due to concerns of transplant rejection. Upon examination, there were widespread erythematous papules with hyperkeratinized spicules affecting the nose and central face (). She denied bleeding and discharge from the lesions, and reported no recent fevers, chills, or malaise. The patient’s medications included prednisone, tacrolimus, and mycophenolate mofetil.
Figure 1. Trichodysplasia spinulosa. (A) Widespread erythematous papules with hyperkeratinized spicules distributed on the nose and central face, with concurrent acne vulgaris. (B) Resolution of TS-associated rash following four weeks of topical 1% cidofovir therapy.

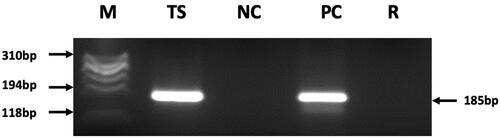
Histopathological examination of a representative lesion revealed a hyperkeratotic plug with bacterial colonies, as well as root sheath epithelial hyperplasia with eosinophilic inclusions, consistent with trichodysplasia spinulosa. PCR analysis confirmed the presence of TSPyV DNA (). The TSPyV copy number was determined via real time PCR method and found to be 4.84 × 105 copies per cell. Therapy was initiated with topical tazarotene 0.05% and imiquimod 3.75% with no noticeable improvement after four weeks. With the help of a local compounding pharmacy, the patient was provided an affordable prescription for topical cidofovir 1% cream, to be applied once daily to affected areas. Significant improvement was noted soon after initiation. Complete resolution was achieved after four weeks of therapy (). Notably, the patient’s immunosuppressive regimen was not interrupted.
Figure 2. PCR detection from a DNA sample obtained from a TS lesion.
Legend: M: molecular weight marker fx174 DNA/Hae III, TS: patient DNA sample is positive for TSPyV, producing expected 185bp PCR product, NC: negative control DNA, PC: positive control DNA (cloned recombinant TSPyV DNA), R: reagent control.
Discussion
The incidence of TS is the same in children, adolescents, and adults and appears to affect both genders equally, though more data are needed to thoroughly characterize its epidemiology (Citation2). It is frequently mistaken for acne when appearing in younger patients, or reported concurrently with it, as in the case of our patient (Citation2, Citation3). TS is almost always reported as asymptomatic or slightly pruritic; to the authors’ knowledge, only one other case of painful TS has been reported, in an otherwise immunocompetent patient being treated with vismodegib (Citation4). Our case of a classic TS patient (a solid organ graft recipient on immunosuppressive regimen) developing tender TS lesions highlights an atypical presentation of an already rare disease.
In the last decade, TSPyV, a small double-stranded DNA virus, has been identified as clonally integrated in trichodysplasia spinulosa-affected cells, with anti-TSPyV immunostaining localizing expression to TS-affected follicular keratinocytes (Citation2, Citation5). A proposed mechanism of action involves dysregulation of MEK, ERK, and MNK1 by interacting with protein phosphatase 2 A (Citation6). Diagnosis of trichodysplasia spinulosa is largely clinical, with skin biopsy performed for confirmation. Histopathologic examination classically reveals dilated and distorted hair follicles, disorganized inner root sheath cell hyperproliferation with abnormally large trichohyalin granules, and gray-blue cytoplasmic material occupying most of the follicular epithelium (Citation1).
TSPyV transmission and pathogenesis are not well-understood; however, viral detection in nasopharyngeal and fecal sampling implies respiratory and/or fecal-oral routes (Citation6). Additionally, while polyomaviruses are thought to manifest upon viral reactivation during immunosuppression, anti-TSPyV antibodies are only detected following clinical evidence of TS, suggesting that the disease state in TS may be caused by primary infection rather than reactivation (Citation7). Although TS is seen in immunocompromised individuals, it has not been reported in the elderly, an observation that further supports primary infection rather than reactivation as cause for TS presentation (Citation2).
Various treatments have been attempted, including manual extraction of keratin projections, oral valganciclovir, oral leflunomide, and reduction of immunosuppressive agents; spontaneous resolution has also been reported (Citation6, Citation8, Citation9). Topical keratolytics, oral minocycline, and topical and oral retinoids have been trialed with limited success (Citation10). Cidofovir is a selective viral DNA polymerase inhibitor indicated for the treatment of cytomegalovirus retinitis in AIDS patients (Citation11). While it is manufactured for intravenous administration, several small studies have reported off-label use of compounded topical cidofovir to treat viral skin disease, including TS. These cases have generally shown modest improvement with different concentrations of topical cidofovir (Citation3, Citation12). The present case demonstrates the exciting result of complete resolution of TS with a relatively low concentration at 1%.
This case is one of extremely few reported instances of painful TS. This and other reports of TS improvement with topical cidofovir hint that clinical trials further evaluating the efficacy of this therapy in larger cohorts of patients are warranted. TS should be considered whenever an immunocompromised patient presents with a hyperkeratotic spicular rash affecting the face. Conversely, a characteristic spiny rash affecting the nose and central face in an otherwise healthy patient should raise suspicion for occult immunosuppressive disease.
Patient consent
The patient discussed in this manuscript has given their written permission for the use of their images and health information.
Data sharing statement
Data sharing is not applicable for this manuscript as no new data were created or generated by this study.
Disclosure statement
The authors have no relevant conflicts of interest to disclose.
Additional information
Funding
References
- DeCrescenzo AJ, Philips RC, Wilkerson MG. Trichodysplasia spinulosa: a rare complication of immunosuppression. JAAD Case Rep. 2016;2(4):1–3. doi: 10.1016/j.jdcr.2016.07.002.
- Rouanet J, Aubin F, Gaboriaud P, et al. Trichodysplasia spinulosa: a polyomavirus infection specifically targeting follicular keratinocytes in immunocompromised patients. Br J Dermatol. 2016;174(3):629–632. doi: 10.1111/bjd.14346.
- Leitenberger JJ, Abdelmalek M, Wang RC, et al. Two cases of trichodysplasia spinulosa responsive to compounded topical cidofovir 3% cream. JAAD Case Rep. 2015;1(6):S33–S5. doi: 10.1016/j.jdcr.2015.09.019.
- Richey JD, Graham TA, Katona T, et al. Development of trichodysplasia spinulosa: case report of a patient with gorlin syndrome treated with vismodegib. JAMA Dermatol. 2014;150(9):1016–1018. Sep doi: 10.1001/jamadermatol.2013.9322.
- Sheu JC, Tran J, Rady PL, et al. Polyomaviruses of the skin: integrating molecular and clinical advances in an emerging class of viruses. Br J Dermatol. 2019;180(6):1302–1311. doi: 10.1111/bjd.17592.
- Wu JH, Narayanan D, Simonette RA, et al. Dysregulation of the MEK/ERK/MNK1 signalling cascade by middle T antigen of the trichoydsplasia spinulosa polyomavirus. J Eur Acad Dermatol Venereol. 2017;31(8):1338–1341. doi: 10.1111/jdv.14326.
- van der Meijden E, Horváth B, Nijland M, et al. Primary polyomavirus infection, not reactivation, as the cause of trichodysplasia spinulosa in immunocompromised patients. J Infect Dis. 2017;215(7):1080–1084.
- Wu JH, Nguyen HP, Rady PL, et al. Molecular insight into the viral biology and clinical features of trichodysplasia spinulosa. Br J Dermatol. 2016;174(3):490–498. doi: 10.1111/bjd.14239.
- Aleissa M, Konstantinou MP, Samimi M, et al. Trichodysplasia spinulosa associated with HIV infection: clinical response to acitretin and valganciclovir. Clin Exp Dermatol. 2018;43(2):231–233. doi: 10.1111/ced.13286.
- Lee JS, Frederiksen P, Kossard S. Progressive trichodysplasia spinulosa in a patient with chronic lymphocytic leukaemia in remission. Australas J Dermatol. 2008;49(1):57–60. doi: 10.1111/j.1440-0960.2007.00422.x.
- Food and Drug Administration. FDA approves cidofovir for treatment of CMV retinitis. J Int Assoc Physicians AIDS Care. 1996;2(8):30. PMID: 11363758.
- Santesteban R, Feito M, Mayor A, et al. Trichodysplasia spinulosa in a 20-month-old girl with a good response to topical cidofovir 1%. Pediatrics. 2015;136(6):e1646-9–e1649. doi: 10.1542/peds.2015-0953.

