Abstract
Aim
This case study aims to report the efficacy and safety of a Janus kinase (JAK) inhibitor in the treatment of generalized eosinophilic pustular folliculitis (EPF).
Methods
We present a case of a 16-year-old Chinese patient who had been suffering from EPF for two years and had shown no response to both topical and systemic glucocorticoids. The patient was subsequently treated with oral tofacitinib at a dosage of 5mg daily.
Results
Significant remission of eruption and pruritus was observed in the patient upon treatment with tofacitinib. However, a relapse occurred upon dose reduction. Subsequent switch to the highly selective JAK1 inhibitor upadacitinib resulted in complete recovery, with the patient achieving a symptom-free status after six months.
Conclusions
JAK inhibitors show promise as a potential treatment option for EPF patients who do not respond to traditional therapies.
Eosinophilic pustular folliculitis (EPF) is a sterile inflammatory dermatosis characterized by recurrent episodes of pruritic follicular papules and pustules. The present report describes a case of a 16-year-old Chinese patient who suffered from pruritic dermatosis for two years. Previous application of systemic and topical glucocorticoid therapy was ineffective. EPF diagnosis was confirmed by histopathology and successfully treated by using JAK inhibitors. No relapse and disease progression were observed with a follow-up for six months. Thus, JAK inhibitors may be a potential treatment option for EPF.
A 16-year-old Chinese male patient suffered from pruritic dermatosis for two years. The lesion first appeared on the back and then gradually spread to the whole body. A physical examination revealed multiple papules and macules on his face, trunk, and extremities, with most of them breaking and crusting over (). Previous treatment included oral and topical corticosteroids at a local hospital after a diagnosis of eczema, which was effective at first but worsened after stopping the treatment.
Figure 1. (a,c) Clinical manifestation before treatment with tofacitinib. Multiple papules and macules on forechest and left lower limb, with most of them breaking and crusting at the top. (b,d) Clinical manifestation after treatment with upacitinib. The papules have almost faded, leaving significant hyperpigmentation.

The biopsy of the left arm suggested hyperkeratosis, focal parakeratosis, and acanthosis. Follicular epithelium spongiosis and eosinophil infiltration were observed. Perivascular infiltrate by eosinophil and lymphocyte mildly in the superficial and middle dermis (). Alcian blue staining demonstrated some mucin surrounding the follicles. Laboratory examination showed an elevated eosinophil cell count of 0.96 g/L (normal: 0.02–0.52 g/L), and total IgE level of 235 IU/mL (normal: 0–100 IU/mL).
Figure 2. (a,c,d) Histopathology manifestation of the lesion obtained from the left upper arm. Hyperkeratosis, focal parakeratosis, and acanthosis. Follicular epithelium spongiosis and eosinophil infiltration were observed. Perivascular infiltrated by eosinophil and lymphocyte mildly in superficial and middle dermis (hematoxylineosin, scale bars: (a) 200×, (c) 40×, and (d) 200×). (b) Serum levels of eosinophil markers during the treatment course.
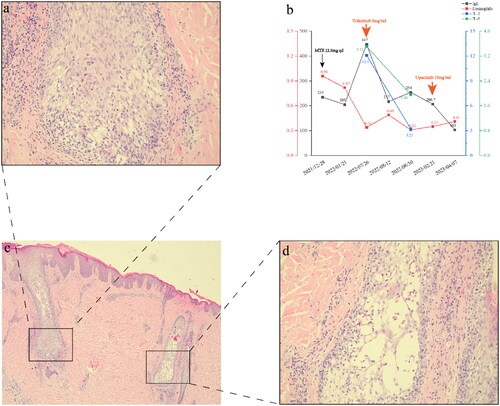
The diagnosis of eosinophilic pustular folliculitis (EPF) was made based on the clinical finding and examination results. Treatment with methotrexate (MTX; 12.5 mg/week) resulted in mild improvement. Itching and new rashes were still reported. Thus, tofacitinib citrate (Qilu Pharmaceutical, Jinan, China) was administered twice a day (5 mg) after excluding the possibility of contraindications and receiving informed consent. The patient’s eruption and pruritus both remitted rapidly, while blood serum IgE level and eosinophil cell count returned to normal limits. Total serum IL-5 level decreased rapidly to 1.96 pg/mL (normal: ≤3.1 pg/mL) and IL-2 to 3.23 pg/mL (normal ≤7.5 pg/mL) after one month of drug administration (). Unfortunately, the disease relapsed during tofacitinib dose reduction, requiring a return to original tofacitinib dosage without improvement. Thus, upacitinib (AbbVie, North Chicago, IL, USA) was prescribed, which is a highly selective JAK1 inhibitor that may be superior to tofacitinib in terms of both safety and efficacy. A complete recovery was achieved within four weeks (). The patient remained symptom-free after a six-month follow-up.
EPF is a sterile inflammatory dermatosis characterized by recurrent episodes of pruritic follicular papules and pustules, mainly affecting the face, upper extremities, and upper back. Classic EPF, immunosuppression-associated EPF, and infancy-associated EPF are the three EPF subtypes (Citation1). Its etiology remains unclear, and histopathology results are eosinophilic infiltration in and around the hair follicles, accompanied by spongiosis and follicle destruction (Citation2). It has also been found that about 50% of facial EPF is associated with follicular mucinosis (Citation3). EPF diagnosis is based on clinical manifestations and histological findings. In the present case, the patient presented with erythema with distinct borders, follicular papules, and macules with surface breaking and crusting, accompanied by significant pruritus. Peripheral blood eosinophil and total IgE levels were elevated. Histopathology showed follicular epithelium spongiosis, eosinophil infiltration, and some mucin surrounding the follicle. Combining these findings with the patient’s age at disease onset and the absence of other co-morbidities, the diagnosis of classic EPF was established.
Systemic or topical indomethacin is considered to be the first treatment choice for classic EPF. Additional alternatives include treatment with ultraviolet light, cyclosporine A, dapsone, tetracyclines, and topical tacrolimus (Citation4). However, patients who are unresponsive and/or intolerant to conventional therapies still urgently need alternative treatment options. Successful treatment with JAK inhibitors has been previously reported in other types of eosinophilic infiltrative diseases, such as Hypereosinophilic Syndrome (Citation5), Chronic eosinophilic pneumonia (Citation6), and Eosinophilic annular erythema (Citation7).
JAK inhibitors cause acneiform eruptions and folliculitis in 1.4%–16.5% of patients receiving oral JAK inhibiters (Citation8). JAK inhibitor-induced acne may arise from a combination of dose-dependent effects, microbial changes, immune responses, and individual patient factors including the use of certain topical treatments (Citation9). However, JAK inhibitor treatment for EPF has an outstanding effect by blocking T helper 2 (Th2) cytokines and inhibiting eosinophil’ maturation and activation. Eosinophils mediate maturation via release of interleukin (IL)-5 from activated Th2 lymphocytes and tissue recruitment, while activation occurs with the help of Th2 cell cytokines, including IL-4, IL-5, IL-10, and IL-13 (Citation10). Thus, Th2 cytokines play a very important role in the production and activation of eosinophils. The JAK1 signaling pathway is essential for Th2 cytokines transcription, and its inhibition allows for the treatment of EPF.
In the present case, the lesions were generalized and long-lasting, and there were new rashes even after topical/systemic glucocorticoid and MTX treatment. Since JAK inhibitors can further interfere with EPF pathogenesis, JAK inhibitors were administered to the patient in addition to the topical corticosteroid. The patient’s pruritus was significantly reduced on the very first day after the application of tofacitinib. The rash completely resolved after four weeks leaving only hyperpigmentation. However, relapse occurred during tofacitinib treatment tapering. Subsequent upadacitinib treatment cleared the rash completely after four weeks.
To the best of our knowledge, this is the first reported case of EPF treated with a JAK inhibitor. JAK inhibitors have a rapid onset of action, relieving patients’ symptoms in a short period of time. In the present case, pruritus symptoms were significantly reduced on the very first day of JAK inhibitor treatment and the rash cleared completely after four weeks of treatment. However, it is worth noting that relapse remains a concern, leading to further considerations of additional options for maintenance therapy and drug tapering in the follow-up period. Besides, screening and monitoring for infectious diseases prior to treatment with JAK inhibitors is critical as JAK inhibitors has been previously reported to be associated with viral infections and reactivations.
Ethics statement
The patient consent was obtained to publication of the case details in this manuscription.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
All data generated or used during the case appear in the submitted manuscription.
Additional information
Funding
References
- Nomura T, Katoh M, Yamamoto Y, et al. Eosinophilic pustular folliculitis: a proposal of diagnostic and therapeutic algorithms. J Dermatol. 2016;43(11):1–4. doi:10.1111/1346-8138.13359.
- Ishiguro N, Shishido E, Okamoto R, et al. Ofuji’s disease: a report on 20 patients with clinical and histopathologic analysis. J Am Acad Dermatol. 2002;46(6):827–833. doi:10.1067/mjd.2002.120533.
- Lee WJ, Won KH, Won CH, et al. Facial and extrafacial eosinophilic pustular folliculitis: a clinical and histopathological comparative study. Br J Dermatol. 2014;170(5):1173–1176. doi:10.1111/bjd.12755.
- Peckruhn M, Elsner P, Tittelbach J. Eosinophilic dermatoses. J Dtsch Dermatol Ges. 2019;17(10):1039–1051. doi:10.1111/ddg.13943.
- King B, Lee AI, Choi J. Treatment of hypereosinophilic syndrome with cutaneous involvement with the JAK inhibitors tofacitinib and ruxolitinib. J Invest Dermatol. 2017;137(4):951–954. doi:10.1016/j.jid.2016.10.044.
- Yamane T, Hashiramoto A. A case of chronic eosinophilic pneumonia associated with rheumatoid arthritis in glucocorticoid-free remission with JAK inhibitor: a case report. Medicine. 2023;102(13):e33396. doi:10.1097/MD.0000000000033396.
- Chastagner M, Shourik J, Jachiet M, et al. Treatment of eosinophilic annular erythema: retrospective multicenter study and literature review. Ann Dermatol Venereol. 2022;149(2):123–127. doi:10.1016/j.annder.2021.07.007.
- Martinez J, Manjaly C, Manjaly P, et al. Janus kinase inhibitors and adverse events of acne: a systematic review and meta-analysis. JAMA Dermatol. 2023;159(12):1339–1345. doi:10.1001/jamadermatol.2023.3830.
- Sun C, Su Z, Zeng Y-P. Association of risk of incident acne and treatment with systemic Janus kinase inhibitors in atopic dermatitis: a systematic review and meta-analysis. Inflamm Res. 2023;72(9):1861–1871. doi:10.1007/s00011-023-01789-x.
- Leiferman KM, Peters MS. Eosinophil-related disease and the skin. J Allergy Clin Immunol Pract. 2018;6(5):1462.e6–1482.e6. doi:10.1016/j.jaip.2018.06.002.

