Abstract
Purpose
Most patients treated in a hospital setting are fully or partially immobilised. The Activity Board (Träningstavlan® Phystec) is a useful tool to enhance mobilisation after major abdominal cancer surgery. Knowledge of patient experiences of the mobilisation tool is crucial in implementing the Activity Board in health care. This study aimed to describe patient experiences of using the Activity Board after surgery for abdominal cancer.
Materials and methods
Semi-structured face-to-face interviews were conducted in 15 patients who underwent abdominal surgery due to colorectal, ovarian or urinary bladder cancer. All 15 patients (mean age 67.7 years, range 40–86) used the Activity Board postoperatively. The interviews were transcribed verbatim and analysed according to inductive content analysis.
Results
The overarching theme that emerged from the interviews was that “enabling participation facilitates empowerment over rehabilitation”. Three categories supported the theme: prerequisites for using the Activity Board, the value of using supportive behavioural techniques, and the possibility to influence the patients’ care.
Conclusions
These findings suggest that the Activity Board could be a viable tool that activates the person-centred postoperative rehabilitation process by cooperating with the medical team at the hospital ward.
Patients who are in hospital due to cancer surgery are often immobilised, which increases the risk of complications.
The Activity Board can stimulate the patients to participate in the rehabilitation process in a more active way.
The Activity Board can be used to improve and clarify the person-centred approach in hospital settings.
Implications for rehabilitation
Introduction
After surgery, early mobilisation (e.g., sitting, standing, or walking) is known to impact postoperative complications [Citation1]. The most common treatment for solid cancer tumours today is surgery, often combined with chemotherapy, radiotherapy, or both [Citation2]. After major abdominal surgery, the frequency of postoperative complications is relatively high. The most common complications are venous thrombosis and pulmonary complications [Citation3,Citation4]. To enhance recovery and minimise complications, programmes for enhanced recovery after surgery (ERAS) have been developed for use after abdominal surgery [Citation5]. The ERAS programmes include early mobilisation, but evaluation of the mobilisation element is scarce. Although mobilisation is generally known to be important after surgery, the research is lacking and the optimal amount of sitting, standing or walking is not yet established [Citation6].
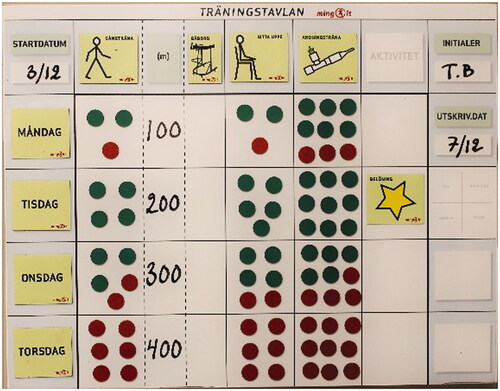
Patients treated in hospital for acute conditions and patients who had elective abdominal surgery spend most of the time immobilised [Citation7,Citation8]. Moreover, there is no difference in immobilisation as a function of age [Citation9]. According to patients, supporting patients’ mobilisation in hospital is essential [Citation10]. The Activity Board (Träningstavlan® Phystec) was developed in Sweden to inform the patient and the medical team about the amount of mobilisation needed after thoracic surgery and is used in several hospitals in Sweden and Denmark. The Activity Board is a whiteboard that hangs in the patient’s room (), and it is used to support the patient’s physical recovery. The board has prefabricated signs for different exercises. It is also equipped with magnets that are red on one side and green on the other to illustrate goals to achieve and goals achieved, respectively. The Activity Board includes techniques that can support or change the patient’s behaviour, such as mobilisation. Examples of behavioural change techniques are goal-setting, self-monitoring and feedback [Citation11,Citation12].
Figure 1. The Activity Board.
In a recent nonrandomised controlled trial (nRCT) we evaluated the Activity Board as a tool to enhance postoperative recovery after abdominal cancer surgery [Citation13]. Our evaluation of the Activity Board resulted in higher mobilisation levels in patients who used the board than in those allocated to usual physiotherapy care. Both groups had individual physiotherapy including mobilisation and breathing exercises. In addition, the patients in the Activity Board group had a shorter time to first flatus and first stool, as well as a briefer length of hospital stay compared to the usual care group. To facilitate the implementation of the Activity Board in health care knowledge of the patients’ thoughts of using the board is important. To be able to conduct a clinically relevant and effective implementation, the patients’ interest in the Activity Board, and potential facilitators or barriers of using the board are important to detect on beforehand. Consequently, this study aimed to describe patients’ experiences of using the Activity Board after surgery for abdominal cancer.
Materials and methods
A qualitative approach was used to describe the patients’ experiences of using the Activity Board. All individual interviews were analysed using inductive content analysis. The reporting of the study follows the SRQR (Standards for Reporting Qualitative Research) checklist [Citation14].
Participants
Participants were recruited from our recently performed nRCT [Citation13]. Patients who were to undergo abdominal surgery due to colorectal cancer, urinary bladder cancer or suspicion of ovarian cancer were asked to participate in the nRCT. Inclusion criteria were expected stay at hospital of at least 3 days, open or robotic-assisted laparoscopic surgery, speak and understand Swedish and the ability to walk. In that study 133 patients, treated at three wards at the hospital, were included. Of these 133 patients, 15 participated in the present study.
The interviews were conducted when the participants were due to be discharged from the hospital within a few days. The participants had given oral and written consent before surgery to be included in the qualitative study when entering the nRCT. Purposive sampling of participants allocated to the Activity Board group and not usual care, was applied to achieve wide variation in sex, age and diagnosis, which could increase the transferability of the results [Citation15,Citation16]. The study was approved by the Regional Ethical Committee of Stockholm (Dnr 2012/2214-31/4, 2016/484-32 and 2017/2349-32).
The Activity Board
When introducing the Activity Board, the physiotherapist and the patient discuss the importance of mobilisation and breathing exercises, and together they set daily goals using red magnets for the different exercises. After the goals are set, the patient has the main responsibility for turning the magnets and achieving the daily goals, with assistance from the medical staff and the physiotherapist. Once an activity, such as walking, sitting or breathing exercises, is completed the patient turns one magnet from red to green. If all goals are achieved for the day, a reward, a golden star, is added to the Activity Board.
Data collection
The individual face-to-face interviews were semi-structured based on an interview guide with open-ended questions, with follow-up questions if needed (Supplementary Appendix 1). The interview guide, following the study’s aim, focused on four main topics: the goal of the Activity Board, the practical usage of the Activity Board, the Activity Board as a motivational tool and the effect of the Activity Board. Three pilot interviews were conducted for the unexperienced interviewer to practice and to improve the interview guide. After the pilot studies, several methodological changes were made. The interview guide was improved, in such way that the follow-up questions were altered so that they would facilitate the patients to give more elaborated stories. “Have other people in your vicinity as relatives or friends supported you and if so, in what way?” followed by “Can you describe what they think and how you have experienced it?” are examples of questions that were added. A complementary follow-up question about future use of the board was also added, “And now that you are about to leave the hospital, is there anything about the Activity Board that you think will be able to help you with your rehabilitation going forward?” In addition, the interview technique was worked on to facilitate more elaborated stories in contrast to clinical anamnesis. The pilot interviews were not included in the data analysis. The interviews, which took place at the hospital ward in the patient’s room, were performed between 2018-03-12 and 2018-04-28 by a physiotherapist (Johanna Eriksson, JE) not involved in the patients’ medical care. The Activity Board, the subject of the interview, was hanging on the wall in the patient’s room during all the interviews. When no new information emerged during the interviews, we terminated the study, with the purpose to receive enough information power to fulfil the aim of the study [Citation16,Citation17]. The interviews lasted 20 to 45 min and were recorded on a digital Dictaphone (Olympus VN-741PC). The transcribed interviews were not returned to the participants for comments.
Researcher characteristics and reflexivity
The researchers responsible for this study were physiotherapists with varied scientific and practical backgrounds, which achieved a broad understanding of the material and helped to ensure dependability [Citation18]. JE, who performed the interviews, has clinical experience working as a physiotherapist in the postoperative setting with this patient group. Andrea Porserud (AP) has experience of working as a physiotherapist with patients having abdominal cancer surgery. Mari Lundberg (ML), Malin Nygren Bonnier (MNB) and Maria Hagströmer (MH) contributed with knowledge within qualitative research, physiotherapy and surgery.
Data analysis
The transcribed interviews were analysed using inductive content analysis, and the conventional inductive approach was used when categories were derived directly from the text [Citation18,Citation19]. According to Graneheim et al. no data related to the purpose should be excluded depending on the existing categories [Citation18]. Consequently, the categories and subcategories were not always based on all the participants’ experiences, since not all the participants had expressed experiences on the subject. A qualitative content analysis according to Graneheim and Lundman can be performed in several steps [Citation18,Citation20]. The analysis aimed at describing what the patients’ experiences were of using the Activity Board (manifest analysis), and to understand how their experiences in using the Activity Board affected them (latent analysis) [Citation18,Citation21,Citation22]. The interviews were coded in the same order as the participants were included in the study. All files were stored according to the ethics approval statement throughout the entire process. AP transcribed three and JE two interviews while a professional transcriber transcribed the 10 remaining interviews. AP and JE read all the interviews to gain a sense of the content and then divided the text into meaning units corresponding to the study's aim. With methodological support from ML, the meaning units were condensed and labelled with a code (examples are given in ). The codes were then organised into categories with subcategories and analysed until an overarching theme was identified. Quotations from the transcriptions are used to illustrate the different categories.
Table 1. Examples of the initial stages of the analysis process.
Techniques to enhance trustworthiness and credibility of data analysis
In order to enhance trustworthiness and credibility of the data analysis, a procedure was agreed beforehand. JE and AP was to analyze all interviews until the coding was done; ML and MNB were to give methodological support during this process. Credibility was enhanced by ML giving methodological support, in selecting the most suitable meaning units as well as checking the coding procedure along the process. Categories and subcategories were created in an iterative process with all co-authors, until consensus was reached. Initially, JE and AP defined preliminary categories and subcategories. These were discussed and if necessary, renamed in collaboration with all the authors. For example, during this process the preliminary subcategory “design” was changed to “design, usability and availability” since the authors found the content of the participants’ experiences also to include experiences of using the board and the location of the board. The category “knowledge gain” was moved and changed to subcategory “confirming knowledge” within the category “the possibility to influence their care” to avoid overlapping. Also, the category “using behavioural supportive techniques” was extended to “the value of using supportive behavioural techniques” since the category included aspects of the experienced value of using the techniques. Several techniques were used to strengthen the credibility of data. Peer debriefing from all authors, and triangulation, in which all authors discussed, analysed and reorganised the categories and subcategories several times until an overarching theme was agreed [Citation15].To further facilitate credibility, quotations are frequently used to support the categories [Citation18]. To minimise the risk of a physiotherapist's potential bias during the interviews the interviewer (JE) described her role as a researcher and not as a physiotherapist [Citation15].
Results
Demographic data on the 15 participants are presented in . The participants stories are summarized into an overarching theme Enabling participation facilitates empowerment over rehabilitation, which builds together the three categories Prerequisites for using the Activity Board, The value of using supportive behavioural techniques, and The possibility to influence their care, and the nine subcategories (). The design of the Activity Board, instructions on how to use it and commitment from the health care staff were parts that facilitated usage of the board. The participants also thought that the supportive behavioural techniques included in the board had an impact on how they could participate in postoperative care. Moreover, the participants expressed that they were strengthened in their care through the Activity Board by knowledge gain, of how to cope with stress and impact physical recovery.
Figure 2. The overarching theme, categories, and subcategories in that order, that was identified in the analysis of patients’ experiences of using the Activity Board after surgery for abdominal cancer.
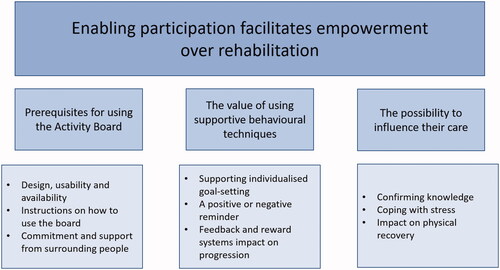
Table 2. Characteristics of the study participants.
Prerequisites for using the Activity Board
This category and its subcategories reflect the participants’ perceptions of the design, usability and availability of the Activity Board. The category also incorporates the necessity of clear and instructive instructions to use the board, as well as support from the medical team and next of kin. (Based on experiences of fifteen participants)
Design, usability and availability
The participants described that the design of the board and its usability were important to support the use. Concerning design, the pictures were perceived as large enough and clearly visible. However, some described the magnets as hard to grip and thus could present a usability problem. The participants also specified the value of the Activity Board’s simplicity. Moreover, the board’s location was found to be significant. To facilitate using the Activity Board, the participants advocated hanging it in a central part of the patient’s room close to the bed. (Based on experiences of fifteen participants)
Naturally, you do have your mobile device at hand, but I can see that you need this simplicity as well– by looking at it, you will see what to do. (P1: woman, 46 y)
The location is important and I would, yes the proximity. Actually. That you really reach it … For me, I do not have a conscience to shout at staff every time you do something there. (P12: man, 75 y)
Instructions on how to use the board
To facilitate the use of the board, the participants mentioned the importance of receiving a clear and instructive introduction of the Activity Board in a non-stressful context. It was clearly described how an unclear introduction could affect compliance negatively. The participants also expressed a need to receive clear information on which activities count and how they should be measured. (Based on experiences of eight participants)
No, but then when the board came up, it was good, clearly. And when she told me what to do, she was very clear too … Yes, how to use it, details and so on. (P1: woman, 46 y)
Then it's a bit diffuse as to what counts. I was showering and washing my hair, brushing my teeth and all that, but I don't know if any of those activities can be counted as board activities. If you were to take it as... and so I stood and showered … and washed my hair. So it took its time, too, but then I do not know if that should be counted as an activity. Maybe one could also get a point for… hi hi… (P3: woman, 71 y)
Commitment and support from surrounding people
Something that further strengthened the use of the board, was if the Activity Board was used as a dialogue tool during routine medical rounds. However, even if the Activity Board raised awareness about mobilisation, the participants were feeble after surgery and needed the physical support from the nursing staff for mobilisation, and also their assistance with catheters and drains. They did not want to add an extra task for the nursing staff by asking for help. The participants’ next of kin were mentioned as a potential resource in assisting with both mobilisation and the Activity Board. Other participants purported that relatives were necessary as the nursing staff did not have the time. (Based on experiences of ten participants)
And so now when the doctor was here and said no but you have to get up now, you have to get up, but then I said yes that but look, I was up one kilometre the other day. (P15: woman, 53 y)
Difficult for the staff also because they have a lot to do already… to take time… and then… because then they still have to sacrifice some time to go with me back and forth. (P3: woman, 71 y)
The value of using supportive behavioural techniques
This category relates to different aspects of the Activity Board that may support the participants take a more active part in postoperative care. The participants described that their activity levels were affected by having clear activity goals, being reminded by the board to be active and receiving continuous feedback. (Based on experiences of twelve participants)
Supporting individualised goal-setting
The participants claimed that the goal-setting of activities was preferably done in partnership between the physiotherapist and the patient. Goal-setting by using the board could be viewed in different ways. On the one hand it could be viewed as something positive that made the goals more easily communicated and visible on the board, making the participants to feel it was easier to take responsibility to achieve the goals. They also stressed that the daily goals were revised and progression was contingent on how the patient is feeling. Consequently, on the other hand goal-setting could be perceived as stressful if the goals were not modified, the participants expressed that they could experience a lack of goal achievement and perhaps even lose interest in the board. The participants also said they feel they would likely fail if the goals were set too high. (Based on experiences of seven participants)
mm . It works great with the hundred meters and planned six, seven times, ah a little like that, you were aware of… then you made it the goal. (P1: woman, 46 y)
And when I started to feel bad and I could not do it during that particular time… when I got almost 39 degrees fever and I felt really bad. Then I just lay and looked at those coloured dots and thought that, that I was a very bad person who could not be out running in the corridor. (P8: woman, 56 y)
A positive or negative reminder
On the one hand, the Activity Board was found to be a positive reminder to perform physical activity. The participants described how the Activity Board emphasised the need for action, as the red magnets was a signal to perform activities, not postpone them. Some of the participants experienced that being reminded helped them self-monitor, i.e., plan, carry out and follow the activities' progression during the day. By almost always being in the participants’ visual field, the Activity Board served as a constant reminder. On the other hand, participants experienced the reminding as a continuing duty to perform and achieve certain physical activities. It was also apparent that the Activity Board was not as useful as a reminder for those with major postoperative complications. (Based on experiences of eleven participants)
You are reminded that no, now you should do because it's a bit of stuff. I'm such that I, I see the board here and I know at about now I know how many rounds, walking rounds I can do. In practice. And then you plan a little bit about what I will do during the day. Because I know that suddenly it will come, you think that now I will do it, now I will just rest for two seconds, and then I will pull myself together and go for a walk and then there will be a visit. (P12: man, 75 y)
Because I … it looks at me a little like this so that, it is, so of course, it has had an impact. That I figured it out myself… “No, I will go now”. (P5: man, 73 y)
No, it has not had, I can tell you, any relevance. Because then I have felt, I have felt so bad, had so much pain that I did not, not even with great effort could I get myself up. No, I don't have the energy to use the board. No, one feels, what should I say. Yes, it does not affect one. You are in so much pain that it does not matter what it says. (P12: man, 75 y)
Feedback and reward systems impact on progression
The participants referred how the Activity Board gave feedback in different ways and how they perceived it. The participants reported that to turn the magnets from red to green often resulted in immediate positive feedback. The participants also expressed that after looking at the Activity Board and seeing what they had achieved, they felt a sense of encouragement or reward. Some participants identified themselves as competitive types and were thereby encouraged by instant feedback and reward, which helped them to perform. However, some participants saw the reward system as a childish activity. Participants also pointed out that recovery progression was clarified when more magnets were turned over time. (Based on experiences of twelve participants)
…there's a good deal of negative emotions… You feel bad and you have cancer and you know… it's not fun at all… hi hi and then you see that… then you see that you have walked a hundred meters… it's good… So it has maintained to a… .it's almost like you get a bouquet of flowers or a bag of sweets… you understand .? (P1: woman, 46 y)
Yes, so I might think that the set-up is a bit infantile in some way with gold stars and coloured dots and things like that. It is not something that's directly me, which I am usually triggered by, and even less so in a context like this. (P8: woman, 56 y)
Yes, but it's the overview here then, that you see, that you see that you make more dots now then than in the beginning when you were more tied to the bed. That you have the strength to walk more as well. (P3: woman, 71y)
The possibility to influence their care
This category involves the participants’ thoughts of how the Activity Board could assist them in their recovery after surgery. They experienced that the Activity Board confirmed and reinforced their previous and new knowledge of mobilisation and breathing exercises, encouraging them to participate in postoperative care. Moreover, they described that the Activity Board helped them gain a sense of control over a stressful and physically difficult situation. (Based on experiences of eleven participants)
Confirming knowledge
The Activity Board confirmed the participants’ previous knowledge and experiences on mobilisation and breathing exercises and illustrated the importance of these activities. The offer from the medical team to use the board was perceived as confirmation and encouragement of the participants’ knowledge, which strengthened them during the postoperative recovery. Moreover, the participants who gained new knowledge on mobilisation and breathing exercises described that the Activity Board clarified their importance. The board worked as a reinforcement of the physiotherapist’s introduction, which included the physiological impact of mobilisation and breathing exercises. They also described that the Activity Board helped in learning about the importance of progression of physical activity. The participants also remarked that it was essential to learn about the evidence of the chosen exercises and the dosage. The participants expressed that the things they learned when using the Activity Board could facilitate active physical activity behaviour after hospital discharge. They described that they would use the knowledge they obtained on measuring physical activity and how to work with goal-setting at home. (Based on experiences of eleven participants)
It's also like… Before I said that I know how important it is to get started, making the work more manageable, you could say. (P13: woman, 70 y)
Mm. To sit up, that it is important to sit up instead of just walking. I did not know that it is very important. (P7: woman, 40 y)
When you are at home… I'll take it easy now. But you could move around in the garden. Overall, I know the number of overall laps taken. Go out and start the tractor sometimes and check things like that. And then you can take notes with one of those. Or, just write in a pad what you are doing. I will certainly do that. That I know what I have done and this depends on the board. So it's just to have a college block, so "Monday" and then what I have done during that time. Yes, yes, sure. You fill it in every time you have been out or what you have eaten and things like that… so I think this. And I will continue to do so! (P5: man, 73 y)
Coping with stress
The participants described that medical care after surgery was stressful and challenging. Hence, they expressed that the Activity Board was something that they could focus on, and it was easy to understand. The board helped the participants to take responsibility for their care. For some participants, stress from the Activity Board was perceived as positive and helped them to avoid being hospitalised. Other participants perceived the Activity Board as burdensome, but it could be positive to focus on the board when their thoughts were occupied on survival or not. In addition, participants expressed that the Activity Board contributed to their engaging in different activities, which helped to reduce feelings of loneliness. (Based on experiences of seven participants)
…that you can tell them that this is something I can really help myself with in order to improve my health. Because the surgeon helps and does the operation and the nurses help with the medicines, the doctors make sure that you get the right help and the assistant nurses make sure you have sheets and that you like . ehe . whatever it is.ehe everything, so there are so many things that they know about me then and this is of help… actually… so I could do something, too. (P1: woman, 46 y)
Impact on physical recovery
The participants recognised that their fitness improved by using the Activity Board. Using the board, they had been more physically active, which they thought would affect their recovery in a positive manner. They also described a feeling of being able to impact the time they spent at the ward and, consequently, on when they could be discharged from hospital. The participants also remarked that the Activity Board should be a routine similar to the other hospital ward routines. (Based on experiences of eight participants)
Yes absolutely. Otherwise, I do not think I would have been as active. I do not think so, but then you have to fight like that. Because you know that it shouts at you and you know that if I'm good, I might get, well that I might be able to come home tomorrow. (P10: man, 65 y)
Well, it was a bit like I said before, I think it would rather be like the hospital management, department head decision, in line with what the employees think, I mean we wash hands before we put on plastic wrap, we do lots of things before we handle a patient. It could be just as obvious then that. As a routine, yes. (P9: man, 71 y)
Discussion
This study indicates that the Activity Board could facilitate patients’ empowerment over rehabilitation after surgery for abdominal cancer by enabling medical care participation. One of the findings is that the participants felt that the board influenced their ability to cope with stress and facilitate physical recovery. Both unifying and differential perceptions among the participants formed the conclusions of the current study.
Many of the participants expressed that they were content with the design of the Activity Board. They were particularly optimistic about the board’s simplicity and that they easily could see and understand the signs of various types of exercises. These findings that the participants valued, a simple and easy to use design with a large display, are in line with previous studies that have evaluated exercise applications in smartphones [Citation23,Citation24]. Another positive attribute of the Activity Board was that it was often in the participants’ visual field. Thus, the board was a constant reminder to the participants to be active. This reminder could be compared with the evaluation of an exercise application in a smartphone in which the icon was set up at the home screen where it was easy to see [Citation24]. Hence, a difference between the Activity Board and the phone is that to use an exercise application in a smartphone, the patient must have the phone nearby and take an active decision to look at the phone.
The analysis showed that the participants discussed the following behaviour change techniques: goal-setting, self-monitoring, feedback and rewards. Changing or supporting a behaviour, in this case mobilisation and breathing exercises, can be difficult. In 2008, Abraham and Michie constructed a taxonomy on behaviour change techniques to use in interventions, and the Activity Board used in our study includes several of these techniques [Citation11]. The participants perceived that goal-setting should be a joint effort by the physiotherapist and patient. This opinion is in accord with research suggesting that person-centred goal-setting should be one part of person-centred care in physiotherapy [Citation25]. The importance of daily goal-setting has also been acknowledged by patients undergoing colorectal surgery [Citation26]. In addition, our analysis showed that the participants perceived that the red and green magnets on the Activity Board gave them an easy way to self-monitor their mobilisation and breathing exercises. Lately, it has been shown that, among behaviour change techniques, self-monitoring was the most commonly used technique associated with increased physical activity [Citation27]. Reward is also a behaviour change technique and, for the Activity Board, the golden star is the most visible reward. Some participants thought the star's simplicity was appealing, whereas others perceived it as somewhat ludicrous. Some participants even saw the star as an insult. Consequently, the way rewards are given in relation to the Activity Board could be further elaborated on, such as in a more person-centred manner.
Moreover, the results showed that participants experienced the Activity Board as a tool that helped them influence their care. Patients willing to participate has been demonstrated in research on patient perceptions of the ERAS concept [Citation26,Citation28]. However, it has also been shown that patients lack knowledge of their care during hospital stay [Citation29]. Understanding and playing an active part in medical care are often challenging for many patients. Therefore, the patient’s autonomy is affected due to the medical care needed [Citation28]. Necessary steps after surgery entail mobilising, regaining autonomy and gaining control over the body [Citation10,Citation30,Citation31]. Perhaps, as a result, the analysis also showed that the Activity Board could assist the participants with stress-coping postoperatively. Such assistance is seen as a much-needed intervention given that patients often suffer from mental stress due to diagnosis, surgery and in-hospital care [Citation32,Citation33]. A review on patient experiences of ERAS indicated a need to help patients feel more secure during the postoperative period [Citation34]. The Activity Board could enable patients to cope with stress and improve their impact on physical recovery. From a patient perspective this study implies that the Activity Board could be implemented in hospital care. With clear instructions to the medical team on how to use the board the barriers that were identified can be handled with extra attention. A daily up-date of patient goals and asking whether patients appreciate the golden star are examples of how person-centred care can be operationalised.
There are limitations to this study, which deserve attention. The researchers responsible for this study are all physiotherapists, which undoubtedly have affected interpretation of findings. Credibilitiy could be affected, leading to results that largely reflect the physiotherapists’ perspective [Citation18]. Some of the participants in the nRCT invited to this study declined participation, but for ethical reasons, we could not register these individuals. Those persons could potentially have had postoperative complications affecting the use of the Activity Board. Lacking these persons' perceptions could also affect the transferability of those who undergo abdominal cancer surgery [Citation18,Citation22,Citation35]. Taken the specific setting and patient groups herein, further research on patients’ perception of the Activity Board should be conducted in other settings and patient groups as well as studies striving to reduce the above limitations. It would be informative to evaluate effects and experiences of the Activity Board at hospital wards for patients with for example cardio-respiratory, neurological, or orthopaedic disorders. To add those results to this study with patients who have had abdominal cancer surgery would increase the knowledge of how to best use the Activity Board in hospital settings. Another area of further research is the medical teams’ perception of working with the Activity Board, which is a crucial part in an implementation process. If the medical team experiences the board more of a barrier than a facilitator in their daily work with patients, improvements of the routines or the Activity Board as such could be of importance. However, if the medical team experiences the board as a positive contribution to their work, and those results are put together with the patients’ perception in this study, a large-scale implementation study of the Activity Board would also be of interest.
In conclusion, the following overarching theme emerged: ‘enabling participation facilitates empowerment over rehabilitation’. The theme suggests that the Activity Board could be a viable tool that activates the person-centred postoperative rehabilitation process by cooperating with the medical team at the hospital ward. The Activity Board has possibilities to facilitate the rehabilitation process for many persons in hospital settings.
Appendix_1_Porserud.docx
Download MS Word (15 KB)Disclosure statement
The authors report no conflicts of interest.
Additional information
Funding
References
- Nicholson A, Lowe MC, Parker J, et al. Systematic review and Meta-analysis of enhanced recovery programmes in surgical patients. Br J Surg. 2014;101(3):172–188.
- Jones LW, Peppercom J, Scott JM, et al. Exercise therapy in the management of solid tumors. Curr Treat Options Oncol. 2010;11(1-2):45–58.
- Kehlet H. The surgical stress response: should it be prevented? Can J Surg. 1991;34(6):565–567.
- Fagarasanu A, Alotaibi GS, Hrimiuc R, et al. Role of extended thromboprophylaxis after abdominal and pelvic surgery in cancer patients: a systematic review and Meta-Analysis. Ann Surg Oncol. 2016;23(5):1422–1430.
- Ljungqvist O, Scott M, Fearon KC. Enhanced recovery after surgery: a review. JAMA Surg. 2017;152(3):292–298.
- Castelino T, Fiore JF, Jr, Niculiseanu P, et al. The effect of early mobilization protocols on postoperative outcomes following abdominal and thoracic surgery: a systematic review. Surgery. 2016;159(4):991–1003.
- Baldwin C, van Kessel G, Phillips A, et al. Accelerometry shows inpatients with acute medical or surgical conditions spend little time upright and are highly sedentary: systematic review. Phys Ther. 2017;97(11):1044–1065.
- Browning L, Denehy L, Scholes RL. The quantity of early upright mobilisation performed following upper abdominal surgery is low: an observational study. Aust J Physiother. 2007;53(1):47–52.
- Mudge AM, McRae P, McHugh K, et al. Poor mobility in hospitalized adults of all ages. J Hosp Med. 2016;11(4):289–291.
- Svensson-Raskh A, Schandl A, Holdar U, et al. "I Have Everything to Win and Nothing to Lose": patient Experiences of Mobilization Out of Bed Immediately After Abdominal Surgery. Phys Ther. 2020;100(12):2079–2089.
- Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychol. 2008;27(3):379–387.
- Michie S, Ashford S, Sniehotta FF, et al. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: the CALO-RE taxonomy. Psychol Health. 2011;26(11):1479–1498.
- Porserud A, Aly M, Nygren-Bonnier M, et al. Objectively measured mobilisation is enhanced by a new behaviour support tool in patients undergoing abdominal cancer surgery. Eur J Surg Oncol. 2019;45(10):1847–1853.
- O'Brien BC, Harris IB, Beckman TJ, et al. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245–1251.
- Patton MQ. Qualitative research & evaluation methods. 4th ed. London: Sage Publication; 2015.
- Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res. 2016;26(13):1753–1760.
- Krippendorff K. Content analysis: an introduction to its methodology. 4th ed. London: Sage Publication; 2018.
- Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105–112.
- Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288.
- Lindgren BM, Lundman B, Graneheim UH. Abstraction and interpretation during the qualitative content analysis process. Int J Nurs Stud. 2020;108:103632.
- Downe-Wamboldt B. Content analysis: method, applications, and issues. Health Care Women Int. 1992;13(3):313–321.
- Graneheim UH, Lindgren BM, Lundman B. Methodological challenges in qualitative content analysis: a discussion paper. Nurse Educ Today. 2017;56:29–34.
- Baretta D, Perski O, Steca P. Exploring users' experiences of the uptake and adoption of physical activity apps: longitudinal qualitative study. JMIR Mhealth Uhealth. 2019;7(2):e11636.
- Casey M, Hayes PS, Glynn F, et al. Patients' experiences of using a smartphone application to increase physical activity: the SMART MOVE qualitative study in primary care. Br J Gen Pract. 2014;64(625):e500–e508.
- Wijma AJ, Bletterman AN, Clark JR, et al. Patient-centeredness in physiotherapy: what does it entail? A systematic review of qualitative studies. Physiother Theory Pract. 2017;33(11):825–840.
- Aasa A, Hovbäck M, Berterö CM. The importance of preoperative information for patient participation in colorectal surgery care. J Clin Nurs. 2013;22(11-12):1604–1612.
- King AC, Whitt-Glover MC, Marquez DX, 2018 Physical Activity Guidelines Advisory Committee, et al. Physical activity promotion: highlights from the 2018 physical activity guidelines advisory committee systematic Review. Med Sci Sports Exerc. 2019;51(6):1340–1353.
- Norlyk A, Harder I. After colonic surgery: the lived experience of participating in a fast-track programme. Int J Qual Stud Health Well-Being. 2009;4:170–180.
- Sommer AE, Golden BP, Peterson J, et al. Hospitalized patients' knowledge of care: a systematic review. J Gen Intern Med. 2018;33(12):2210–2229.
- Jonsson CA, Stenberg A, Frisman GH. The lived experience of the early postoperative period after colorectal cancer surgery. Eur J Cancer Care (Engl)). 2011;20(2):248–256.
- Hughes M, Coolsen MM, Aahlin EK, et al. Attitudes of patients and care providers to enhanced recovery after surgery programs after major abdominal surgery. J Surg Res. 2015;193(1):102–110.
- Abelson JS, Chait A, Shen MJ, et al. Sources of distress among patients undergoing surgery for colorectal cancer: a qualitative study. J Surg Res. 2018;226:140–149.
- Parpa E, Tsilika E, Gennimata V, et al. Elderly cancer patients' psychopathology: a systematic review: aging and mental health. Arch Gerontol Geriatr. 2015;60(1):9–15.
- Sibbern T, Bull Sellevold V, Steindal SA, et al. Patients' experiences of enhanced recovery after surgery: a systematic review of qualitative studies. J Clin Nurs. 2017;26(9-10):1172–1188.
- Polit DF, Beck CT. Generalization in quantitative and qualitative research: myths and strategies. Int J Nurs Stud. 2010;47(11):1451–1458.

