ABSTRACT
Objective
To systematically review the literature on hypertensive disorders of pregnancy (HDP) after multifetal pregnancy reduction (MFPR).
Methods
A comprehensive search in PubMed, Embase, Web of Science, and Scopus was performed. Prospective or retrospective studies reporting on MFPR from triplet or higher-order to twin compared to ongoing (i.e., non-reduced) triplets and/or twins were included. A meta-analysis of the primary outcome HDP was carried out using a random-effects model. Subgroup analyses of gestational hypertension (GH) and preeclampsia (PE) were performed. Risk of bias was assessed using the Newcastle-Ottawa Quality Assessment Scale.
Results
Thirty studies with a total of 9,811 women were included. MFPR from triplet to twin was associated with a lower risk for HDP compared to ongoing triplets (OR 0.55, 95% CI, 0.37–0.83; p = 0.004). In a subgroup analysis, the decreased risk of HDP was driven by GH, and PE was no longer significant (OR 0.34, 95% CI, 0.17–0.70; p = 0.004 and OR 0.64, 95% CI, 0.38–1.09; p = 0.10, respectively). HDP was also significantly lower after MFPR from all higher-order (including triplets) to twin compared to ongoing triplets (OR 0.55, 95% CI, 0.38–0.79; p = 0.001). In a subgroup analysis, the decreased risk of HDP was driven by PE, and GH was no longer significant (OR 0.55, 95% CI 0.32–0.92; p = 0.02 and OR 0.55, 95% CI 0.28–1.06; p = 0.08, respectively). No significant differences in HDP were found in MFPR from triplet or higher-order to twin versus ongoing twins.
Conclusions
MFPR in women with triplet and higher-order multifetal pregnancies decreases the risk of HDP. Twelve women should undergo MFPR to prevent one event of HDP. These data can be used in the decision-making process of MFPR, in which the individual risk factors of HDP can be taken into account.
Introduction
Multifetal pregnancies are associated with an increased risk of maternal and perinatal morbidity and mortality compared to singleton pregnancies (Citation1–4). When comparing higher-order multifetal pregnancies (i.e., with three or more fetuses) to twin pregnancies, rates of pregnancy complications are even higher (Citation2,Citation3,Citation5). Maternal risks of multifetal pregnancies include hypertensive disorders of pregnancy (HDP, including gestational hypertension (GH) and preeclampsia (PE)), gestational diabetes , cesarean delivery, and postpartum hemorrhage (Citation6). HDP are described to develop at an earlier gestational age and with higher maternal morbidity comparing multifetal pregnancies with singleton pregnancies (Citation5). Furthermore, HDP are still the leading cause of maternal mortality worldwide, responsible for over 27,800 maternal deaths every year (Citation7). Perinatal risks of multifetal pregnancies are often directly related to perinatal complications including preterm birth and/or very low birth weight (Citation8), with its consequences for the neonate and later in life in terms of neurodevelopmental disorders (Citation9).
The incidence of multifetal pregnancies (twins, triplets, and higher-order pregnancies) has risen remarkably since the 1980s and 1990s, caused by the use of fertility treatments and a higher average maternal age at conception (Citation10,Citation11). Due to primary prevention strategies (Citation12), the incidence of multifetal pregnancies has declined and has now stabilized around 34 per 1,000 live births in the United States (Citation13). In 2020, the triplet and higher-order multifetal birth rate was 79.9 per 100,000 births (Citation14).
When a triplet or higher-order multifetal pregnancy occurs, multifetal pregnancy reduction (MFPR) can be considered to reduce the total number of fetuses by one or more, carried out in the first or early-second trimester (Citation15,Citation16). In the counseling for MFPR, the risk of the procedure (i.e., a chance in loss of the entire pregnancy (Citation17,Citation18)) has to be weighed against the possible maternal and perinatal complications associated with a multifetal pregnancy.
Most studies on MFPR show an increase in gestational age at delivery after MFPR compared to ongoing multifetal pregnancies (Citation19–22). Van de Mheen et al. found that MFPR in women with a trichorionic triplet pregnancy is associated with a decreased risk of preterm birth <32 weeks, while risks for pregnancy loss after reduction or preterm birth <24 weeks in ongoing triplet pregnancies are similar (Citation19).
The effect of MFPR on maternal morbidity is not evident. In order to counsel women with multifetal pregnancies on MFPR appropriately, it is important to have a more extensive knowledge on the development of maternal complications during and after pregnancy. Based on recent literature, MFPR from a twin to a singleton pregnancies to improve pregnancy outcomes should not be advised, due to an increased risk of preterm delivery and pregnancy loss (Citation23). Therefore, the objective of this study was to systematically review the literature on HDP and other maternal outcomes after MFPR in women with triplet and higher-order multifetal pregnancies.
Material and methods
Protocol and registration
This systematic review was reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement (Citation24). The study protocol was registered with the PROSPERO register prior to its commencement (registration number: 344839).
Search strategy
A comprehensive search was performed in the bibliographic databases PubMed, Embase, Web of Science and Scopus from inception to July 6th 2022, in collaboration with a medical librarian (LS). Search terms included controlled terms (MeSH in PubMed and Emtree in Embase) as well as free-text terms. The following terms were used as index terms or free-text words, including synonyms and closely related words: “multiple pregnancies” and “reduction”. The search was performed without date or language restrictions. Duplicate articles were excluded by a medical information specialist (LS) using Endnote X20.0.1 (Clarivatetm), following the Amsterdam Efficient Deduplication (AED)-method (Citation25) and the Bramer-method (Citation26). The full search strategies for all databases can be found in the Supplementary Information (Table S1).
Selection process
Two reviewers (PB and JW) independently screened all potentially relevant titles and abstracts for eligibility using Rayyan (Citation27). Studies were included if they met the following criteria: (i) prospective or retrospective studies; (ii) reporting on MFPR from triplets to twins or MFPR from higher-order multifetal pregnancy to twins compared to ongoing (i.e., non-reduced) triplets and/or twins; (ii) featuring HDP (including GH and PE) as an outcome measure. The exclusion criteria were as follows: (i) review articles, case reports, congress abstracts, and letters; (ii) MFPR to singletons; (iii) studies comparing different types of reduction techniques; (iv) studies comparing early versus late reduction; (v) more than 20% of case group (after MFPR) consisting of spontaneous reduction or selective reduction (i.e., reduction for fetal anomaly or complications related to a monochorionic pregnancy (e.g., twin to twin transfusion syndrome (TTTS), twin anemia polycythemia Sequence (TAPS), selective intra uterine growth restriction (sIUGR)); (vi) outcome data published in other language than English. No restrictions regarding chorionicity were made since chorionicity does not appear to substantially influence maternal outcomes (Citation28), except for those with complications related to monochorionic pregnancies. Full texts were obtained if studies appeared to meet the inclusion criteria or in case of uncertainty. All reasons for exclusion were recorded. Reviewing authors were not blinded to the journal titles, study authors, or institutions. Reference and citation lists of the included studies were scanned to ensure literature saturation. Disagreements regarding study selection were resolved by consulting a third author (MB).
Risk of bias in individual studies
Two reviewers (PM and MB) independently assessed the risk of bias using the Newcastle-Ottawa Quality Assessment Scale (NOS) for non-randomized studies (Citation29). Following the manuals of the tools, studies were scored as either having a “low,” “medium,” “high,” or “unclear” risk of bias.
Outcomes
The primary outcome was HDP, including 1) GH, 2) PE, or 3) both (GH and PE or described as HDP). Secondary outcomes included other maternal outcomes (gestational diabetes (GDM); anemia in pregnancy; cesarean delivery (CD); postpartum hemorrhage (PPH); placental abruption; uterine rupture; HELLP (hemolysis, elevated liver enzymes, and low platelets) syndrome; eclampsia; amniotic fluid embolism; pulmonary embolism; maternal intensive care unit admission; maternal death). Definitions of the outcome measures can be found in .
Table 1. Definitions.
Data collection process and data items
Data from the included studies were extracted by one author (PB) and checked by another (MB). The following baseline data items were collected for all included studies: country; year of publication; study design; study period; sample sizes; reduction approach (transabdominal/transvaginal); reduction technique (KCL injection/aspiration); gestational age at reduction (weeks); type of HDP (GH/PE/HDP); definition of HDP (if reported). Authors of the accepted studies were contacted for important missing data on baseline characteristics. The following demographic data of all included women were collected if available: maternal age at delivery (years); conception (spontaneous/ovulation induction (OI)/assisted reproductive technology (ART)); parity (nulliparous).
The following primary outcome data were collected for all studies: number and/or proportions of GH/PE/HDP. The following secondary outcome data were extracted and when available the number and/or proportions of the outcome measure were also registered: GDM, anemia, CD, PPH, placental abruption, uterine rupture, HELLP syndrome, eclampsia, amniotic fluid embolism, pulmonary embolism, maternal intensive care unit admission, and maternal death.
Synthesis of results
Outcomes were divided into four groups based on the type of case and control groups of the individual studies: 1) MFPR from triplet to twin pregnancy versus ongoing triplet pregnancies, 2) MFPR from all higher-order (including triplets) to twin pregnancy versus ongoing triplet pregnancies, 3) MFPR from triplet to twin pregnancy versus ongoing twin pregnancies, and 4) MFPR from all higher-order (including triplets) to twin pregnancy versus ongoing twin pregnancies. In the individual studies, the primary outcome HDP were reported as GH, PE, or both (GH and PE or described as HDP). For the primary outcome, we presented outcome data of these HDP subgroups narratively and in summary tables with measures of statistical significance if applicable. Furthermore, a pooled data analysis of the main outcome (HDP) was performed using the Cochrane’s Review Manager software Version 5.4 (Citation39). Pooled odds ratios for dichotomous outcomes were calculated using a random-effects model. I2 test was performed to assess heterogeneity, and a value of less than 50% was considered to represent low heterogeneity. Subgroup analyses were performed based on HDP subgroups (GH, PE, and HDP) as well as types of higher-order multifetal pregnancy in the analyses of MFPR from all higher-order (including triplets) to twin pregnancies compared to triplets and twins (analyses 2 and 4, respectively). For secondary outcome, findings were presented narratively and in summary tables with measures of statistical significance, if applicable, in order to prevent selection bias.
Results
Study selection
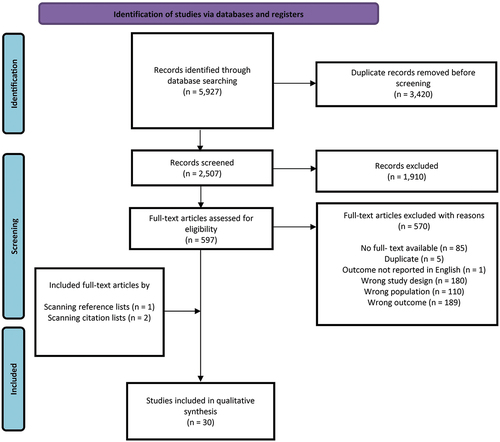
The literature search generated a total of 5,927 records: 1,421 in PubMed, 1,802 in Embase, 1,315 in Web of Science, and 1,389 in Scopus. shows the selection progress and an overview of the reasons for exclusion. After removing duplicates, 2,507 studies remained. Of them, 598 studies were found to be relevant for full-text assessment. After a full-text assessment, 565 studies were excluded, leaving 27 studies that met the eligibility criteria for this systematic review. One study (Citation40) analyzed early transvaginal MFPR (group 1) and late transabdominal MFPR (group 2) and compared the outcomes of both groups to ongoing twin pregnancies (group 3) separately, rather than a comparison of early versus late reduction. Therefore, we did not exclude this article. In addition, three studies were identified by scanning reference and citation lists, resulting in a total of 30 studies evaluating HDP after MFPR from triplet or higher-order multifetal pregnancy to a twin pregnancy compared to ongoing triplets or twins (Citation40–69).
Study characteristics
Baseline characteristics of all included studies can be found in . Eleven studies (Citation44,Citation47,Citation50–52,Citation54,Citation55,Citation58–60,Citation66) reported on HDP after MFPR from triplet to twin pregnancy compared to ongoing triplet pregnancies, and three studies (Citation42,Citation61,Citation67) from higher-order multifetal pregnancy to twin pregnancy compared to ongoing triplet pregnancies. Eight studies (Citation45–47,Citation49,Citation53,Citation55,Citation58,Citation62) reported on HDP after MFPR from triplet to twin pregnancy compared to ongoing twin pregnancies, and 16 studies (Citation40–43,Citation45,Citation46,Citation48,Citation56,Citation57,Citation61–65,Citation67–69) from higher-order multifetal pregnancy to twin pregnancy compared to ongoing twin pregnancies. The 30 studies included a total of 9,811 women who met the inclusion criteria: 1,124 (12%) with MFPR from triplet to twin pregnancy and 1,006 (10%) with MFPR from triplet or higher-order multifetal pregnancy to twin pregnancy. Furthermore, there were 877 (9%) women with an ongoing triplet pregnancy and 6,804 (69%) women with an ongoing twin pregnancy in the comparison groups. In 21 (70%) studies, the procedure of MFPR was performed with a transabdominal approach using potassium chloride (KCL), eight (27%) studies used other methods (), or a combination of transabdominal KCL injection and other methods depending on the gestational age at reduction. In one study (3%), the method of reduction was not reported. Six (20%) studies described their definition of diagnosis of either GH, PE, or HDP.
Table 2. Baseline characteristics of the included studies.
Baseline characteristics of included women
Demographic baseline characteristics are presented in . Of all studies, 24 (80%) reported on maternal age of the included women, 28 (93%) on conception methods, and 22 (73%) on the amount of nulliparous women. No differences in maternal age were seen in women with MFPR from triplet or higher-order multifetal pregnancy to twins compared to women with ongoing triplets. In six studies (Citation43,Citation46,Citation47,Citation65,Citation69) a significant higher maternal age was found in women with MFPR from triplet or higher-order multifetal pregnancy to twins compared to women with ongoing twins. In general, women in the MFPR groups were substantially more likely to have used OI or ART than women with ongoing triplet or twin pregnancies. No substantial trend was seen in the amount of nulliparous women within groups.
Table 3. Demographic baseline characteristics of all the included studies.
Risk of bias within studies
The results of our risk of bias assessment using the Newcastle-Ottawa Quality Assessment Scale (NOS) for cohort studies and case–control studies can be found in Table S2. The risk of bias was “low” in four studies and “moderate” in the remaining 27 studies.
Results of individual studies
HDP after MFPR from triplet and higher-order multifetal pregnancy to twin pregnancy versus ongoing triplet pregnancies
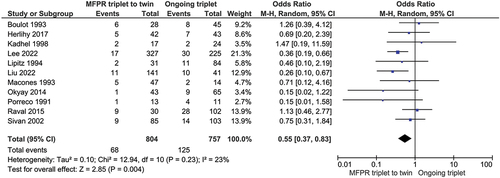
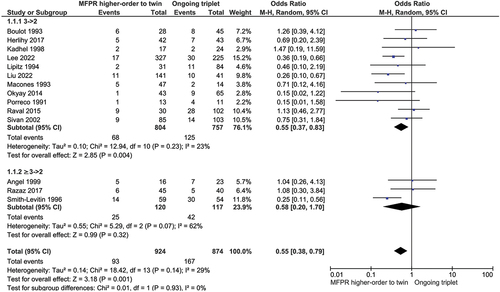
Results of individual studies comparing GH, PE, or HDP after MFPR from triplet or higher-order to twin pregnancy versus ongoing triplet pregnancies can be found in Table S3. MFPR from triplet to twin pregnancy was associated with a lower risk for HDP compared to ongoing triplet pregnancies (), with a corresponding odds ratio (OR) of 0.55 (95% confidence interval (CI), 0.37–0.83; p = 0.004; I2 = 23%). In a subgroup analysis of PE, the difference was no longer significant (Figure S1, OR 0.64, 95% CI, 0.38–1.09; p = 0.10; I2 = 39%), while GH remained significant lower in MFPR from triplet to twin compared to ongoing triplets (Figure S1, OR 0.34,95% CI, 0.17–0.70; p = 0.004; I2 = 0%). HDP was also significantly lower after MFPR from all higher-order (including triplets) to twin pregnancy compared to ongoing triplet pregnancies (, OR 0.55, 95% CI, 0.38–0.79; p = 0.001; I2 = 29%). In a subgroup analysis of HDP after MFPR from all higher-order to twin pregnancy compared to ongoing triplets, without studies including MFPR from triplet to twin only, the difference in HDP was no longer significant (, OR 0.58, 95% CI, 0.20–1.70; p = 0.32; I2 = 62%). Also, in a subgroup analysis of GH, the difference was no longer significant (Figure S2, OR 0.55, 95% CI, 0.28–1.06; p = 0.08; I2 = 21%). The subgroup analysis of PE was consistent with the main analysis (Figure S2) since PE was significantly decreased in women after MFPR from all higher-order to twin pregnancy versus ongoing triplet pregnancies (Figure S2, OR 0.55, 95% CI, 0.32–0.92; p = 0.02; I2 = 50%).
HDP after MFPR from triplet and higher-order multifetal pregnancy to twin pregnancy versus ongoing twin pregnancies
Results of individual studies comparing GH, PE, or HDP after MFPR from triplet or higher-order to twin pregnancy versus ongoing twin pregnancies can be found in Table S4. There were no significant differences in HDP when comparing MFPR from triplet to twin pregnancy and ongoing twin pregnancies (Figure S3, OR 1.28, 95% CI, 0.79–2.07; p = 0.32; I2 = 23%). Also, no significant differences in HDP were found after MFPR from all higher-order to twin pregnancy (including triplets) versus ongoing twin pregnancies (Figure S4, OR 1.06, 95% CI, 0.85–1.33; p = 0.59; I2 = 0%). For the comparison of MFPR from triplet to twin versus ongoing twin pregnancies, the analyses of subgroups of HDP (GH, PE, and HDP) were consistent with the main analysis (Figure S5). In a subgroup analysis, GH was significantly higher in women with twins after MFPR from triplet or higher-order multifetal pregnancies compared to women with ongoing twins (Figure S6, OR 1.67, 95% CI, 1.08–2.57; p = 0.02; I2 = 0%).
Other maternal outcomes
provides detailed information with regard to other maternal outcomes. Of all studies, 21 (70%) reported on gestational diabetes (GDM), 17 (57%) on cesarean delivery (CD), 4 (13%) on postpartum hemorrhage (PPH), and 7 (23%) on placental abruption. Most studies did not find a significant difference in GDM in women after MFPR from triplet or higher-order pregnancy to twin pregnancy compared to women with either ongoing triplet or twin pregnancies (Citation42,Citation43,Citation45–47,Citation49,Citation51,Citation55,Citation57,Citation58,Citation67,Citation68). One study (Citation63) showed a significantly higher risk for GDM in women after MFPR from triplet to twin pregnancy versus ongoing twin pregnancies (p = 0.022). Two studies (Citation60,Citation66) reported a significant decrease in risk for GDM after MFPR from triplet to twin versus ongoing triplet pregnancies. Kim et al. (Citation40) reported that women with twin pregnancies after MFPR from higher-order pregnancy (with early transvaginal method) have lower risk for GDM compared to women with ongoing twin pregnancies (OR 2.33, 95% CI, 1.06–5.10; p = 0.034).
Table 4. Other maternal outcomes.
A lower incidence of CD in women with twin pregnancies after MFPR from triplet or higher-order pregnancy compared to women with ongoing triplet pregnancies was found in most studies (Citation44,Citation47,Citation50,Citation52,Citation58,Citation59,Citation61,Citation66), however only three studies (Citation50,Citation52,Citation66) reported a significant difference. Two studies (Citation58,Citation62) found a significantly higher incidence of CD among women with a twin pregnancy after MFPR compared to women with ongoing twin pregnancies. Of the three studies reporting on PPH (Citation47,Citation51,Citation62), none showed a significant difference in PPH in women after MFPR versus women with ongoing twin or triplet pregnancies. In the studies reporting on placental abruption (Citation43,Citation56,Citation58–60,Citation62,Citation64), no significant differences were found within the groups. A limited number of studies focused on HELLP syndrome (Citation44,Citation69) or pulmonary embolism (Citation44), and none of these reported significant differences in outcome within the groups. No studies have been reported on anemia, uterine rupture, eclampsia, amniotic fluid embolism, maternal intensive care unit admission, or maternal death.
Discussion
The results of this systematic review and meta-analysis indicate that women after MFPR from a triplet or higher-order multifetal pregnancy to a twin pregnancy have a significantly lower risk for HDP compared to women with ongoing triplet pregnancies. For MFPR from triplet to twin, this result is driven by GH. For MFPR from higher-order to twin, this result is driven by PE. Furthermore, this meta-analysis found that women with twins after MFPR (from triplet or higher-order pregnancy) have a similar risk for HDP compared to women with ongoing twin pregnancies. Based on these results, MFPR in women with triplet and higher-order multifetal pregnancies can be considered, and might result in a decrease in the occurrence of HDP, with potentially important consequences for other pregnancy complications such as (iatrogenic) preterm birth. To our knowledge, this is the first systematic review to focus exclusively on HDP after MFPR, providing an evaluation of all evidence currently available.
In terms of other maternal outcomes, this systematic review found that MFPR from triplet or higher-order multifetal pregnancy to a twin pregnancy compared to ongoing triplet or twin pregnancies does not seem to be associated with altered risk for GDM, PPH, HELLP syndrome, and pulmonary embolism. As expected, incidence of CD is lower in women after MFPR from triplet or higher-order multifetal pregnancy to a twin pregnancy compared to ongoing triplet pregnancies.
Two previously published systematic reviews are also reported on HDP after MFPR. In line with the results of our study, Zipori et al. (Citation22) found no significant differences in their meta-analysis of HDP in women after reduced triplet pregnancies compared to non-reduced twin pregnancies (OR 1.23, 95% CI, 0.82–1.84; p = 0.33; I2 = 16%). However, in contrast to our meta-analysis, a control group of ongoing triplet pregnancies was not included. Raffé-Devine et al. (Citation70) reported on maternal, fetal, and neonatal outcomes after MFPR from twin to singleton, triplet to twin or singleton and quadruplets to twins with different types of control groups without strict exclusion criteria (for example, no exclusion of selective reduction and MFPR from triplet to singleton). No significant trends with respect to HDP were reported, but no meta-analysis was performed.
The lower risk of HDP in women with twins after MFPR from a triplet or higher-order multifetal pregnancy compared to women with ongoing triplet pregnancies found in our study is in line with the latest evidence on the pathophysiology of HDP. The higher risk of HDP in women with multifetal compared to singleton pregnancies might be explained by a greater placental mass in which angiogenetic factors derived from abnormal placental tissue cause more severe endothelial dysfunction in the maternal cardiovascular system (Citation71–73). By performing MFPR and reducing the number of fetuses in women with triplets and higher-order multifetal pregnancies, the enlargement of the harmful placental tissue may also reduce, possibly resulting in less endothelial dysfunction and lower risk of HDP. On the other hand, we found that women with twins after MFPR from all higher-order multifetal pregnancies have a significantly higher risk of developing GH compared to women with ongoing twins (Figure S6). We expect that this increased risk might be caused by a difference in the preexistent maternal cardiovascular health state of these women, with a higher maternal age at conception and more need for fertility treatments. Further research is still needed to explain the exact pathophysiology of HDP in women with multifetal pregnancies.
The results of this systematic review should be viewed in light of the following limitations. Only a small number of studies had a prospective design, so the conclusions of this review are based exclusively on retrospective data with its inherent shortcomings in terms of selection bias. For example, most individual studies included in this meta-analysis did not adjust appropriately for possible confounders of HDP such as maternal age, smoking status, obesity, or other preexisting diseases increasing risks for HDP. Furthermore, it is important to take into account that all included women in the MFPR groups were more likely to have used OI or ART (), possibly overestimating the incidence of HDP in individual studies. Nevertheless, when adjustment for these fertility treatments would take place, then the lower risk for HDP in women after MFPR from triplet or higher-order to twin pregnancy compared to women with ongoing triplets would only become more clear. Following the insufficient adjustment of possible confounders, in most studies a moderate risk of bias was found. A second cause of the moderate risk of bias found in most studies was the lack of documentation on the presence of preexisting hypertension of the included women, and, if data on preexisting hypertension were documented, women with such a history were not excluded from data analysis. Furthermore, the robustness of the results presented in this review is limited, as inaccurate or unprovided definition of HDP, GH, and PE might have biased our reported outcomes.
Remarkably, while MFPR decreased the occurrence of HDP in our two main comparisons, in the subgroup analyses, this result is driven by GH in one group (i.e., for MFPR triplet to twin versus ongoing triplet) and by PE in the other group (i.e., for MFPR higher-order to twin versus ongoing triplet). A post-hoc analysis showed that the main analyses (i.e., HDP as an outcome) were sufficiently powered, while the subgroup analyses for GH and PE were underpowered. For example, comparing the occurrence of PE in MFPR triplet to twin versus ongoing triplets in 555 versus 583 women achieved 73% power at a significance level of 0.05. In this specific comparison, to achieve a power of 80% each group would have to include 676 women. Therefore, the results of all these subgroup analyses should be interpreted with caution. Based on our results, when comparing MFPR triplet to twin versus ongoing triplets, 12 women should undergo MFPR to prevent one event of HDP.
In conclusion, this meta-analysis suggests that MFPR in women with triplet and higher-order multifetal pregnancies decreases the risk of HDP compared to women with ongoing triplet pregnancies. For MFPR from triplet to twin versus ongoing triplets this is driven by GH and for MFPR from higher-order to twin versus ongoing triplets this is driven by PE. These data can be used in the decision-making process of MFPR, in which the individual risk factors of HDP can be taken into account. To gain more insight into the effect of MFPR on HDP and to counsel women with multifetal pregnancies appropriately, future studies should investigate meaningful parameters such as gestational age at onset, need for antihypertensive drug treatment and severity of manifestation of the disorder, with accurate use of diagnosis of HDP according to the most recent ISSHP classification (Citation30).
Author contributions
PB, CG, and MB conceived and designed the study. PB and LS performed the literature search. PB, JW, and EH screened articles for inclusion. PB and MB extracted data and appraised the risk of bias of the identified articles. PB and MB analyzed the data. PB, JW, LM, EP, CG, and MB interpreted the results and revised and contributed to the intellectual content of the manuscript. All authors approved the final version of the manuscript.
Supplemental Material
Download MS Word (834.1 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/10641955.2023.2225597
Additional information
Funding
References
- Workshop Group TEC Multiple gestation pregnancy. The ESHRE Capri workshop group. Hum Reprod. 2000 Aug;15(8):1856–15. doi: 10.1093/humrep/15.8.1856
- Luke B, Brown MB. Maternal morbidity and infant death in twin vs triplet and quadruplet pregnancies. Am J Obstet Gynecol. 2008; Apr;198(4):401 e1–10. doi: 10.1016/j.ajog.2007.10.785
- Wen SW, Demissie K, Yang Q, et al. Maternal morbidity and obstetric complications in triplet pregnancies and quadruplet and higher-order multiple pregnancies. Am J Obstet Gynecol. 2004 Jul;191(1):254–258.
- American College of O, Gynecologists’ Committee on Obstetric P, Committee on G. Committee opinion No 671: perinatal risks associated with assisted reproductive technology. Obstet Gynecol. 2016 Sep;128(3):e61–8. doi: 10.1097/AOG.0000000000001643
- Devine PC, Malone FD. Maternal complications associated with multiple pregnancy. Clin Obstet Gynecol. 2004; Mar;47(1):227–236. doi: 10.1097/00003081-200403000-00023
- Luke B, Brown MB. Contemporary risks of maternal morbidity and adverse outcomes with increasing maternal age and plurality. Fertil Steril. 2007 Aug;88(2):283–293. doi: 10.1016/j.fertnstert.2006.11.008
- Wang W, Xie X, Yuan T, et al. Epidemiological trends of maternal hypertensive disorders of pregnancy at the global, regional, and national levels: a population-based study. BMC Pregnancy Childbirth. 2021 May 8;21(1):364. doi: 10.1186/s12884-021-03809-2
- Tucker J, McGuire W. Epidemiology of preterm birth. BMJ. 2004 Sep 18;329(7467):675–678. doi:10.1136/bmj.329.7467.675.
- Schieve LA, Tian LH, Rankin K, et al. Population impact of preterm birth and low birth weight on developmental disabilities in US children. Ann Epidemiol. 2016 Apr;26(4):267–274.
- and ACoO, Gynecologists, Society for Maternal-Fetal M. ACOG Practice Bulletin No. 144: multifetal gestations: twin, triplet, and higher-order multifetal pregnancies. Obstet Gynecol. 2014 May;123(5):1118–1132. doi: 10.1097/01.AOG.0000446856.51061.3e
- Practice Committee of American Society for Reproductive M. Multiple gestation associated with infertility therapy: an American Society for Reproductive Medicine Practice Committee opinion. Fertil Steril. 2012 Apr;97(4):825–834. doi: 10.1016/j.fertnstert.2011.11.048
- Practice Committee of the American Society for Reproductive M, Practice Committee of the Society for Assisted Reproductive T. Guidelines on number of embryos transferred. Fertil Steril. 2009 Nov;92(5):1518–1519. doi: 10.1016/j.fertnstert.2009.08.059
- Martin JA, Hamilton BE, Osterman MJK, et al. Births: final Data for 2017. Natl Vital Stat Rep. 2018 Nov;67(8):1–50.
- Osterman M, Hamilton B, Martin JA, et al. Births: final Data for 2020. Natl Vital Stat Rep. 2021 Feb;70(17):1–50.
- Berkowitz RL, Lynch L, Chitkara U, et al. Selective reduction of multifetal pregnancies in the first trimester. N Engl J Med. 1988 Apr 21;318(16):1043–1047. doi: 10.1056/NEJM198804213181607
- Evans MI, Fletcher JC, Zador IE, et al. Selective first-trimester termination in octuplet and quadruplet pregnancies: clinical and ethical issues. Obstet Gynecol. 1988 Mar;71(3 Pt 1):289–296.
- Berkowitz RL, Lynch L, Stone J, et al. The current status of multifetal pregnancy reduction. Am J Obstet Gynecol. 1996 Apr;174(4):1265–1272.
- Chaveeva P, Kosinski P, Puglia D, et al. Trichorionic and dichorionic triplet pregnancies at 10-14 weeks: outcome after embryo reduction compared to expectant management. Fetal Diagn Ther. 2013;34(4):199–205. doi: 10.1159/000356170
- van de Mheen L, Everwijn SM, Knapen MF, et al. The effectiveness of multifetal pregnancy reduction in trichorionic triplet gestation. Am J Obstet Gynecol. 2014 Nov;211(5):536 e1–6.
- Dodd JM, Crowther CA. Reduction of the number of fetuses for women with triplet and higher order multiple pregnancies. Cochrane Database Syst Rev. 2003;2:1–14. CD003932.
- Evans MI, Britt DW. Fetal reduction 2008. Curr Opin Obstet Gynecol. 2008; Aug;20(4):386–393. doi: 10.1097/GCO.0b013e3283079b93
- Zipori Y, Haas J, Berger H, et al. Multifetal pregnancy reduction of triplets to twins compared with non-reduced triplets: a meta-analysis. Reprod Biomed Online. 2017 Sep;35(3):296–304.
- van de Mheen L, Everwijn SM, Knapen MF, et al. Pregnancy outcome after fetal reduction in women with a dichorionic twin pregnancy. Hum Reprod. 2015 Aug;30(8):1807–1812.
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021 Mar 29;372:n71. doi: 10.1136/bmj.n71
- Otten. Amsterdam Efficient Deduplication (AED) method. 2019.
- Bramer WM, Giustini D, de Jonge GB, et al. De-duplication of database search results for systematic reviews in EndNote. J Med Libr Assoc. 2016 Jul;104(3):240–243.
- Ouzzani M, Hammady H, Fedorowicz Z, et al. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016 Dec 5;5(1):210. doi: 10.1186/s13643-016-0384-4
- Maxwell CV, Lieberman E, Norton M, et al. Relationship of twin zygosity and risk of preeclampsia. Am J Obstet Gynecol. 2001 Oct;185(4):819–821.
- Wells G. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2000.
- Brown MA, Magee LA, Kenny LC, et al. Hypertensive disorders of pregnancy: iSSHP classification, diagnosis, and management recommendations for International Practice. Hypertension. 2018 Jul;72(1):24–43.
- Quintanilla Rodriguez BS, Mahdy H. Gestational diabetes. StatPearls. Treasure Island (FL): StatPearls publishing copyright © 2023. Tampa, FL, USA: StatPearls Publishing LLC; 2023.
- James AH. Iron deficiency anemia in pregnancy. Obstet Gynecol. 2021 Oct 1;138(4):663–674. doi:10.1097/AOG.0000000000004559.
- Practice Bulletin No. 183: postpartum Hemorrhage. Obstet Gynecol. 2017 Oct;130(4):e168–e186. doi: 10.1097/AOG.0000000000002351
- Schmidt P, Skelly CL, Raines DA. Placental abruption. StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © 2023. Tampa, FL, USA: StatPearls Publishing LLC; 2023.
- Togioka BM, Tonismae T. Uterine Rupture. StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © 2023. Tampa, FL, USA: StatPearls Publishing LLC; 2023.
- Kirkpatrick CA. The HELLP syndrome. Acta Clin Belg. 2010; Mar;65(2):91–97. doi: 10.1179/acb.2010.020
- Magley M, Hinson MR, Eclampsia. StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © 2023. Tampa, FL, USA: StatPearls Publishing LLC; 2023.
- Haftel A, Chowdhury YS. Amniotic Fluid Embolism. StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © 2023. Tampa, FL, USA: StatPearls Publishing LLC; 2023.
- Review Manager (RevMan) 5.4. The Cochrane Collaboration; 2020.
- Kim MS, Kang S, Na ED, et al. Obstetrical outcomes of embryo reduction and fetal reduction compared to non-reduced twin pregnancies. Arch Gynecol Obstet. 2019 Apr;299(4):953–960.
- Alexander JM, Hammond KR, Steinkampf MP. Multifetal reduction of high-order multiple pregnancy: comparison of obstetrical outcome with nonreduced twin gestations. Fertil Steril. 1995; Dec;64(6):1201–1203. doi: 10.1016/S0015-0282(16)57985-0
- Angel JL, Kalter CS, Morales WJ, et al. Aggressive perinatal care for high-order multiple gestations: does good perinatal outcome justify aggressive assisted reproductive techniques? Am J Obstet Gynecol. 1999 Aug;181(2):253–259.
- Belogolovkin V, Ferrara L, Moshier E, et al. Differences in fetal growth, discordancy, and placental pathology in reduced versus nonreduced twins. Am J Perinatol. 2007 Nov;24(10):575–579.
- Boulot P, Hedon B, Pelliccia G, et al. Effects of selective reduction in triplet gestation: a comparative study of 80 cases managed with or without this procedure. Fertil Sterility. 1993 1993 Sep 1;60(3):497–503. doi:10.1016/s0015-0282(16)56167-6.
- Groutz A, Yovel I, Amit A, et al. Pregnancy outcome after multifetal pregnancy reduction to twins compared with spontaneously conceived twins. Hum Reprod. 1996 Jun;11(6):1334–1336.
- Haas J, Hourvitz A, Dor J, et al. Perinatal outcome of twin pregnancies after early transvaginal multifetal pregnancy reduction. Fertil Steril. 2014 May;101(5):1344–1348.
- Herlihy N, Naqvi M, Romero J, et al. Multifetal Pregnancy reduction of trichorionic triplet gestations: what is the benefit? Am J Perinatol. 2017 Dec;34(14):1417–1423.
- Hwang JL, Pan HS, Huang LW, et al. Comparison of the outcomes of primary twin pregnancies and twin pregnancies following fetal reduction. Arch Gynecol Obstet. 2002 Dec;267(2):60–63.
- Jiang J-J, Han T, Zhu Y-H. The early second-trimester multifetal pregnancy reduction improves pregnancy outcome. CEOG. 2021 2021 Feb 15;48(1):164–167.
- Kadhel P, Olivennes F, Fernandez H, et al. Are there still obstetric and perinatal benefits for selective embryo reduction of triplet pregnancies? Hum Reprod. 1998 Dec;13(12):3555–3559.
- Lee JY, Lee SM, Jeong M, et al. Short-term and long-term outcomes of trichorionic triplet pregnancies with expectant management. Acta Obstet Gynecol Scand. 2022 Jan;101(1):111–118.
- Lipitz S, Reichman B, Uval J, et al. A prospective comparison of the outcome of triplet pregnancies managed expectantly or by multifetal reduction to twins. Am J Obstet Gynecol. 1994 Mar;170(3):874–879.
- Lipitz S, Uval J, Achiron R, et al. Outcome of twin pregnancies reduced from triplets compared with nonreduced twin gestations. Obstet Gynecol. 1996 Apr;87(4):511–514.
- Liu S, Li G, Wang C, et al. Pregnancy and obstetric outcomes of dichorionic and trichorionic triamniotic triplet pregnancy with multifetal pregnancy reduction: a retrospective analysis study. BMC Pregnancy Childbirth. 2022 Apr 5;22(1):280. doi: 10.1186/s12884-022-04617-y
- Macones GA, Schemmer G, Pritts E, et al. Multifetal reduction of triplets to twins improves perinatal outcome. Am J Obstet Gynecol. 1993 Oct;169(4):982–986.
- Mostajeran F, Gharavi H, Ahmadi SM. Comparison of twin pregnancy outcome after assisted reproductive technology with and without embryo reduction [Original Article]. Int J Reprod BioMed. 2006;4(2):69–72.
- Nevo O, Avisar E, Tamir A, et al. Neonatal course and outcome of twins from reduced multifetal pregnancy versus non-reduced twins. Isr Med Assoc J. 2003 Apr;5(4):245–248.
- Okyay E, Altunyurt S, Soysal D, et al. A comparative study of obstetric outcomes in electively or spontaneously reduced triplet pregnancies. Arch Gynecol Obstet. 2014 Jul;290(1):177–184.
- Porreco RP, Burke MS, Hendrix ML. Multifetal reduction of triplets and pregnancy outcome. Obstet Gynecol. 1991 Sep;78(3 Pt 1):335–339.
- Raval DB, Naglak M, Iqbal SN, et al. Outcomes of Triplets reduced to Twins versus non-reduced Triplet Pregnancies. J Clin Gynecol Obstet. 2015;4(1):160–163. doi: 10.14740/jcgo322w
- Razaz N, Avitan T, Ting J, et al. Perinatal outcomes in multifetal pregnancy following fetal reduction. CMAJ. 2017 May 8;189(18):E652–E658. doi: 10.1503/cmaj.160722
- Selam B, Lembet A, Stone J, et al. Pregnancy complications and neonatal outcomes in multifetal pregnancies reduced to twins compared with nonreduced twin pregnancies. Am J Perinatol. 1999;16(2):65–71. doi: 10.1055/s-2007-993838
- Seo SS, Jo MY, Kim MR, et al. Outcome of twin pregnancies after selective fetal reduction. Korean J Fertil Sterility. 2003;30(1):85–94.
- Silver RK, Helfand BT, Russell TL, et al. Multifetal reduction increases the risk of preterm delivery and fetal growth restriction in twins: a case-control study. Fertil Steril. 1997 Jan;67(1):30–33.
- Singh C, Thakur S, Shahnaz G, et al. Clinical outcomes in higher-order multiples reduced to dichorionic diamniotic (DCDA) twins compared with primary twins and singletons: a prospective observational study. Int J Gynaecol Obstet. 2022 Jun;157(3):671–676.
- Sivan E, Maman E, Homko CJ, et al. Impact of fetal reduction on the incidence of gestational diabetes. Obstet Gynecol. 2002 Jan;99(1):91–94.
- Smith-Levitin M, Kowalik A, Birnholz J, et al. Selective reduction of multifetal pregnancies to twins improves outcome over nonreduced triplet gestations. Am J Obstet Gynecol. 1996 Oct;175(4 Pt 1):878–882.
- Wang Y. Study on fetal reduction in multiple births. Int J Clin Exp Med. 2016;91:6846–6849.
- Yuce T. Reduction of multifetal gestation to twins: is it always possible to attain natural outcomes? Cukurova Med J. 2016;41(3): 485–490.
- Raffé-Devine J, Somerset DA, Metcalfe A, et al. Maternal, fetal, and neonatal outcomes of elective fetal reduction among multiple gestation pregnancies: a systematic review. J Obstet Gynaecology Canada. 2021;44(1):60–70.e12. doi: 10.1016/j.jogc.2021.07.020
- Bdolah Y, Lam C, Rajakumar A, et al. Twin pregnancy and the risk of preeclampsia: bigger placenta or relative ischemia? Am J Obstet Gynecol. 2008 Apr;198(4):428 e1–6.
- Aviram A, Giltvedt MK, Sherman C, et al. The role of placental malperfusion in the pathogenesis of preeclampsia in dichorionic twin and singleton pregnancies. Placenta. 2018 Oct;70:41–49.
- Weiner E, Feldstein O, Schreiber L, et al. Placental component and pregnancy outcome in singleton versus twin pregnancies complicated by Preeclampsia. Fetal Diagn Ther. 2018;44(2):142–148. doi: 10.1159/000479737
- ACOG practice bulletin. Diagnosis and management of preeclampsia and eclampsia. Number 33, January 2002. American College of Obstetricians and Gynecologists. Int J Gynaecol Obstet. 2002 Apr;77(1):67–75.
- Brown MA, Lindheimer MD, de Swiet M, et al. The classification and diagnosis of the hypertensive disorders of pregnancy: statement from the International Society for the Study of Hypertension in Pregnancy (ISSHP). Hypertens Pregnancy. 2001;20(1):IX–XIV. doi: 10.3109/10641950109152635