Abstract
Purpose
Patient-Reported Outcome Measures (PROMs) aim to facilitate patient-centred care by objectively measuring consumer views of their health and well-being in addition to monitoring patient outcomes. This review sought to identify PROMs suitable for adults receiving inpatient rehabilitation to guide clinical practice and consumer engagement in healthcare.
Material and methods
The scoping review methodology was guided by PRISMA-ScR and JBI guidelines. Seven electronic databases (Medline, Embase, CINAHL, PsycInfo, Cochrane CENTRAL, Cochrane Reviews, Scopus) and grey literature were searched from January 2000 to October 2022. Two reviewers independently screened the articles. Data were extracted and summarised thematically to derive clinical implications.
Results
Of 9096 records retrieved, 51 articles were included for analysis. Fifty-nine key PROMs were identified in the rehabilitation literature. The Euro-QOL 5D was reported for more than one-third of the studies. There were numerous condition-specific PROMs pertaining to health conditions such as arthritis, stroke and cardiac failure or symptoms such as pain, depression, fatigue and weakness. Most rehabilitation trials reported using PROMs before therapy and after discharge to monitor within-admission changes.
Conclusions
PROMs are frequently used in rehabilitation research and have the potential to yield helpful data for the evaluation of clinical services.
Introduction
Patient-reported outcome measures (PROMs) are an integral part of evidence-based clinical practice in rehabilitation hospitals worldwide [Citation1–4]. They enable consumers to report their health and wellbeing over time, which fosters patient-centred care and consumer engagement in healthcare delivery [Citation5]. PROMs are also a useful tool for nurses, doctors, allied health professionals and other members of the multidisciplinary team to monitor rehabilitation progress, alongside therapy outcome measures [Citation6] and objective tests of performance [Citation7–9]. PROMS improve safety and quality by incorporating the views of care recipients about which elements of rehabilitation should be prioritised [Citation10,Citation11].
Although PROMs are well embedded in acute hospital settings [Citation12], emergency departments [Citation13] and outpatient settings [Citation14–16], PROMs used for inpatient rehabilitation are less well understood and there is variable implementation into routine care [Citation17]. Many rehabilitation PROMs are available, yet uptake appears fragmented. There are ‘generic’ PROMs which can be used across multiple rehabilitation presentations and can encompass multiple dimensions of health, such as the EuroQOL-5D-5L [Citation18–20] or the Short Form-36 [Citation21,Citation22]. There are also ‘condition specific’ PROMs for consumers that relate to a diagnosis such as arthritis, stroke or Parkinson’s disease or are focused on symptoms such as pain, fatigue, anxiety, depression and disability [Citation23]. There is a growing body of global literature regarding condition-specific PROMs for use in rehabilitation hospitals, especially in relation to PROMs for stroke survivors [Citation24,Citation25], people with hip or knee joint replacements [Citation26–29], Parkinson’s disease [Citation30,Citation31], spinal cord injury [Citation32] or low back pain [Citation33].
Nurses and other health professionals within the multidisciplinary rehabilitation team can use generic and condition-specific PROMs to support shared decision making and to facilitate hospital discharge planning [Citation34–36]. PROMs can also be used to assist patients to reflect on their own health priorities and progress [Citation37–39]. They can facilitate communication between patients and health professionals, and help to identify barriers to good health [Citation9,Citation14]. Philpot et al. (2018) noted that barriers sometimes exist to implementing PROMs in rehabilitation practice [Citation40]. Select PROMs were considered by some people to be time consuming and complex to follow. Health professionals sometimes reported consumer health literacy as a barrier, compounded by presentation of most PROMs in English alone [Citation40]. Facilitators to PROM uptake included the ability to track patient views over time, co-decision making and streamlining of patient consultations when PROMs were shared across the multidisciplinary team [Citation40,Citation41].
For health professionals to be able to select the best tool to use in clinical practice, it is helpful to summarise the main generic and condition-specific PROMs for inpatient rehabilitation hospitals, the clinical populations and symptoms they apply to and how they are scored. The aim of this scoping review is to address these needs. The research questions are: (1) what generic PROMs have been in the scientific literature for inpatient rehabilitation (2) what condition-specific PROMs are typically used for particular diagnoses or symptoms (3) what are the main scale characteristics of inpatient rehabilitation PROMs?
Methods
This review has been co-designed and co-authored with consumer representatives who assisted in the development of the research question, evidence synthesis and manuscript. We used the scoping review methodology to explore the breadth of this topic, map the available literature, identify key concepts in the literature and identify areas of emerging evidence to inform clinical practice [Citation42–46]. Scoping reviews have an a priori protocol, involve extensive database searching, and have documented transparent and reproducible steps [Citation47]. They can also be used to determine whether a systematic review is required or warranted [Citation44–46,Citation48].
Identifying relevant studies
Eligibility criteria were guided by expert opinions, the research team and Joanna Briggs Institute guidelines to develop the population, concept and context for the review [Citation49]. The population of interest was adults (18 years and older) in rehabilitation hospitals. To be included, PROMs had to report patient views of individual health, wellbeing or quality of life, not patient satisfaction or patient experience [Citation50]. PROMs could be completed by the patient independently or with support, but not by proxy. Included journal articles were accessible as full text, peer-reviewed publications and written in English. Only articles that reported primary, quantitative research within inpatient rehabilitation settings were included. Articles were excluded if PROMs were not collected during the reported inpatient rehabilitation trial, except for elective joint arthroplasty surgery patients participating in inpatient rehabilitation for whom PROMs are routinely collected prior to surgery, then three and six months after surgery [Citation51]. Research conducted in non-rehabilitation settings were also excluded, e.g. acute hospitals, community settings, mental health or palliative care.
Search strategy
The search strategy developed for this review was an iterative approach with consultation between the reviewers and a health sciences librarian who executed the searches. The final comprehensive search was conducted across MEDLINE, EMBASE, CINAHL, Cochrane, PsycInfo, Scopus and grey literature including Google Scholar and clinical trial registries. These databases were searched for literature published from 2000 until October 2022, with an example of the search strategy for MEDLINE found in Appendix. Keywords within the search were derived the major categories of ‘patient-reported outcome measure’ and ‘rehabilitation’. Reference lists of the included studies, and of relevant systematic reviews, were examined for relevant additional sources.
Selection of studies
The studies identified in the search were upload to Covidence [Citation52]. Two reviewers independently screened studies by title and abstract, who then independently screened full texts and identified studies meeting the review criteria. At each stage, the reviewers resolved conflicts by discussion to consensus, with consultation by a third reviewer if necessary.
Data charting
Data from eligible studies were independently extracted by two reviewers in a chart designed specifically for this review. This captured key characteristics of studies, including design and methods, population, intervention overview, average inpatient admission length, PROMs utilised and any available detail of the PROM. Where sufficient detail of the PROM properties was not described in the study, this was sought through internet searching. PROM detail included a number of items within the tool, scoring range, direction of scales and interpretation of scores.
Synthesis of Results
The final dataset was synthesised by an iterative process as demonstrated by McKercher (2022) [Citation5], with the focus on accessibility of the data for health professionals seeking to use PROMs in rehabilitation practice. Subsequently, PROMs were separated into generic and condition-specific categories. Data were mapped in tabular and descriptive format, with the number of items within each PROM additionally graphically illustrated. Further detail included study characteristics (e.g. country of origin, year), setting, major domains measured in the PROM (i.e. physical, psychological, social), tool design, number of items and specific domains within the tools [Citation49,Citation53]. A narrative summary of the results was completed in text format including the overall findings and how these results may influence further research or clinical practice [Citation53].
Results
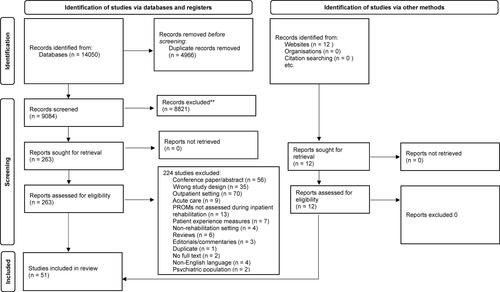
Following the removal of duplicates, 9096 records were retrieved from the seven databases, with an additional 12 from grey literature. illustrates the results of the search strategy within the PRISMA flow diagram [Citation54]. A review of title and abstracts identified 8821 records that did not meet eligibility criteria. A total of 275 full texts were sought for review, with 68 identified as conference abstracts or proceedings. The remaining 207 full texts were assessed for eligibility, with 156 excluded. Often manuscripts were excluded because the study design did not match the research question (n = 35); studies were only in outpatient settings (n = 70); or PROM use did not occur during an inpatient rehabilitation admission (n = 13). The final review included 51 articles.
Supporting Information Table A outlines the characteristics of included rehabilitation studies, such as study design, type of inpatient rehabilitation facility and the country where the study was conducted. Most studies (n = 35, 68.6%) were published within the last five years. The most prominent health condition studied was arthritic diseases [Citation55–63], followed by neurological conditions such as Parkinson’s disease [Citation30,Citation31,Citation64–66], multiple sclerosis [Citation67,Citation68], stroke [Citation24,Citation25,Citation69–75] and spinal cord injury [Citation76–78], then, cardiopulmonary conditions [Citation79–84]. Sample sizes ranged from 10 to 16,966 participants in a three-year, retrospective controlled clinical trial using medical history audits, where collection of a single quality of life PROM, the EQ-5D-5L, was previously embedded in usual care [Citation85]. The average reported inpatient rehabilitation admission length ranged from 14 days in a joint arthroplasty study to 172 days in a spinal cord injury study [Citation76]. Several studies (n = 18, 35.2%) did not report rehabilitation length of stay. Most studies (n = 43, 84.3%) utilised three or less PROMs. The use of six PROMs was the highest reported and occurred in two studies of neurological patients [Citation72,Citation77]. The timepoints of PROM use were most often at baseline and at discharge from inpatient rehabilitation, with 31 studies (60.7%) reporting at least these two timepoints. Use of PROMs between baseline and discharge was reported in two studies [Citation71,Citation79], with daily use of the Multidimensional Mood Questionnaire implemented in a study of stroke patients [Citation71]. Nearly half of the studies (n = 25) included long-term follow-up, ranging from six weeks to 36 months post-discharge.
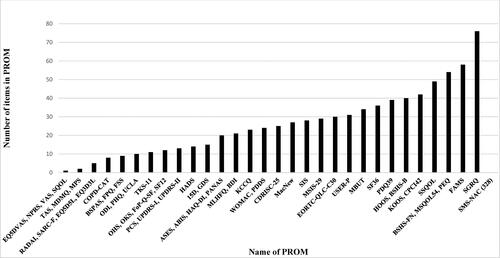
A total of 59 PROMs were identified within these research articles, 32 of which were condition-specific, encompassing musculoskeletal, cardiopulmonary and neurological conditions. An additional 18 PROMs reported specific symptoms, with seven (39%) pertaining to pain and four (22%) to anxiety or depression. The remaining 10 were classified as generic and able to be applied across any person receiving inpatient rehabilitation. illustrates the number of questions within each PROM, ranging from a single question to 328 (average 27 questions/PROM).
summarises the broad constructs measured by the condition-specific PROMs, with the tools encapsulating psychological (anxiety, behaviour, emotions, fatigue, etc.), physical (symptoms, activities of daily living, mobility, gait, hand function, etc.) and social (communication, supports, community links, etc.) aspects of self-reported individual health. The assessment of arthritic diseases (both osteoarthritis and rheumatoid conditions) was addressed by many PROMs, with nine separate tools identified (). Aside from the Arthritis Self Efficacy Scale which addressed psychological issues of arthritis, the other tools were concerned with only physical constructs or falls risk assessment and prevention [Citation94]. This contrasts with the tools specific to neurological conditions such as stroke, Parkinson’s disease and multiple sclerosis, where physical, psychological and social domains were usually examined.
Table 1. Condition-specific patient-reported outcome measures (PROMs) used for inpatient rehabilitation.
Supporting Information Table B details tool structure and scoring interpretation for each condition-specific PROM, in addition to the more detailed domains relevant for the conditions. For example, the Prosthesis Evaluation Questionnaire examines issues of prosthetic use (appearance, sounds, ambulation, etc.), whereas the Burn Specific Health and Anxiety Scales quantify emotional, physical and functional issues related to burn affected skin. This table highlights that most condition-specific PROMS (n = 8, 89%) included examination of physical components of health, such as the impact of pain and joint stiffness on the ability to participate in functional and social or leisure activities.
Also highlighted in Supporting Information Table B is the variability in number of questions within each condition-specific PROM, with numbers ranging from two to 328 (average 38.5/PROM). This average is skewed by the Stoke Mandeville Spinal Needs Assessment Checklist, with 328 questions specific to people receiving rehabilitation for spinal cord injuries [Citation95], with the next highest number of questions found in the St George Respiratory Questionnaire-A being a total of 76 [Citation96]. Whilst most condition-specific PROMs exclusively used Likert-type scales, several tools [Citation76,Citation97–103] used other methods of scoring such as the Multiple Sclerosis Quality of Life questionnaire where a mix of Likert-type scales in addition to yes/no questions generates physical health and mental health summary scores [Citation104].
outlines the symptom-specific PROMs identified within the rehabilitation research literature, with tools concerned with more distinctive domains. Psychological aspects of health including anxiety, depression, self-esteem and mood were addressed in most symptom-specific PROMs (n = 13, 72%), with physical domains of health examined in 11 (61%) tools and social aspects explored in 3 (17%) of tools. The symptom of pain was the focus within the majority of symptom-specific PROMs, with seven (39%) using scales or questionnaires to assess subjective levels of pain that may occur in many conditions.
Table 2. Examples of symptom specific patient-reported outcome measures in the rehabilitation research literature.
Supporting Information Table C details the score ranges and interpretation of each symptom-specific PROM, with all tools utilising Likert-type scales [Citation78,Citation100,Citation109–121] aside from the Geriatric Depression Scale [Citation122] where respondents answer yes/no to questions regarding their mental health. Of note, the Hospital and Anxiety Depression Scale (HADS) [Citation123] was reported in nine of the studies in this review (Supporting Information Table A). This symptom-specific PROM contains 14 questions, with each scaled from absence to extreme presence of psychological symptoms of anxiety and depression. This tool was designed for ease of application and for screening purposes only, and not to be used for definitive diagnoses [Citation123].
The 10 generic PROMs identified within this review covered a broad range of physical, psychological and social constructs (). Evaluation of physical (n = 7, 70%) and/or psychological (n = 8, 80%) domains were included in most generic PROMs. The number of questions within each PROM ranged from 1 to 36, with an average of 14.6 per PROM (see Supporting Information Table D). Aside from the EQ-5D-5L-VAS [Citation126] that utilises a single visual analogue scale to quantify an individuals’ own view of overall health, the other generic PROMs identified in the rehabilitation research literature use Likert-type scales for scoring. The EQ-5D-5L was the most frequently utilised PROM, with over a third of the studies in this review reporting scores (Supporting Information Table A). Score ranges and interpretation for each PROM are summarised in Supporting Information Table D.
Table 3. Generic patient-reported outcome measures used for inpatient rehabilitation.
Discussion
An analysis of the global literature showed the use of PROMs for people participating in inpatient rehabilitation to be variable, despite the availability and usefulness of these tools [Citation17,Citation32,Citation127,Citation128]. In countries such as the United States there is a movement towards adopting value-based payment models that incorporate patient-centred outcomes together with therapy outcome measures, whilst in Australia there is consideration that PROMs may be utilised to optimise care quality, safety and patient satisfaction [Citation6,Citation17]. At the same time, multidisciplinary teams seek clarity on which generic PROMs and condition-specific PROMs are best suited for use in rehabilitation hospitals [Citation32].
This review of papers on rehabilitation research trials found 59 PROMs used with rehabilitation inpatients. The EuroQol-5D-5L and Short Form-36 were the most frequently used generic PROMs for rehabilitation services and programs. According to Groeneveld (2019), the EuroQol-5D-5L is particularly helpful for showing changes in general health and quality of life over the course of rehabilitation [Citation72]. Whether or not the tool is sensitive enough to demonstrate specific changes remains open to question, especially when applied alone. A wide range of condition-specific PROMs were also reported. These varied greatly in length, complexity and suitability for clinical application, especially considering pressures on patient length of stay. Aligned with the International Consortium for Health Outcomes Measurement (ICHOM) recommendations [Citation23], we found that condition-specific PROMs give insights into a patient’s perspective of their physical capabilities, as well as views on changes over the course of rehabilitation in their psychological status and perceived social limitations. This is important to rehabilitation therapists who seek to report outcomes across several functional domains that reflect the patients’ lived experiences.
The review supports the value add of partnering with consumers to measure their perceptions of change over the course of their rehabilitation stay. As noted by Heath et al. (2021) [Citation129], rehabilitation teams can benefit from sharing PROMs data to monitor patient progress. Generic PROMs are particularly helpful in this regard, to monitor changes in cohorts over time. This can be reported at a system level when all patients at a given service complete the same generic PROM. Working as teams, clinicians can select, apply and share the findings of PROMs when collaborating towards common rehabilitation goals. Interdisciplinary rehabilitation approaches can therefore benefit from team decisions incorporating PROMs data across physical, psychological and social domains [Citation128,Citation130]. However, the importance of understanding a patient’s perspective and experience of rehabilitation goes beyond the direct clinical team. As highlighted by Kayes and Papadimitriou (2023) [Citation131], for patient-centred practice to be embedded in health services, key stakeholders at the level of funders, insurers and policymakers need to consider and prioritise patient views, which may be derived in part from the use of PROMs.
There were several limitations of this review. First, the analysis was restricted to what was reported in the published research literature and the review might not have captured every PROM suitable for rehabilitation inpatients. Second, the review only included papers published in English and the findings are not necessarily representative of all global regions, ethnicities or cultures. It was beyond the scope of the current review to evaluate the impact of different cultures, countries and languages on the reliability and validity of the rehabilitation PROMS examined. This is an important consideration for future trials. We did not specifically examine the effects of implementing electronic health record-based PROMs, which has already been examined by Heinemann et al. (2022) [Citation32]. Simple Likert-type scales were used by the vast majority of PROMs and the psychometric properties of rehabilitation PROMs awaits further analysis and verification. As noted by Terwee et al. (2021) [Citation130], there can sometimes be an overlap in PROMs definitions, and wide variation in terminology and scoring differences for rehabilitation PROMs. It would be beneficial to develop a specific inpatient rehabilitation PROM, whereby clinicians can access tools known to be valid for application in the rehabilitation context. Most of the studies analysed in this review were from research trials and there may be a difference between the use of PROM in daily practice as compared to in a research design. There is also potentially a research-practice gap between the findings and recommendations of researchers and the implementation of PROMS into everyday clinical practice.
Conclusion
Rehabilitation PROMs aim to facilitate consumer engagement in the design, delivery and evaluation of services. Although a range of PROMS have been identified for research use, there remains a need for consensus on a minimum set of PROMS to be implemented clinically in rehabilitation hospitals. There is arguably a need to design new rehabilitation PROMS that are both reliable and more patient-centred.
Supplemental Material
Download Zip (161.1 KB)Acknowledgement
Thank you to Elizabeth Lawrence, a research librarian at La Trobe University, for assistance with devising and conducting the literature search.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Licht T, Nickels A, Riedl D, et al. Evaluation of inpatient cancer rehabilitation by routine electronic patient-reported outcome measures (ePROM): improvement of quality of life (QoL) and psychological distress. J Clin Oncol. 2019;37(Suppl 15):e18294–e18294.
- Licht T, Nickels A, Rumpold G, et al. Evaluation by electronic patient-reported outcomes of cancer survivors’ needs and the efficacy of inpatient cancer rehabilitation in different tumor entities. Support Care Cancer. 2021;29(10):5853–5864. doi: 10.1007/s00520-021-06123-x.
- Smit EB, Bouwstra H, van der Wouden JC, et al. Development of a patient-reported outcomes measurement information system (PROMIS®) short form for measuring physical function in geriatric rehabilitation patients. Qual Life Res. 2020;29(9):2563–2572. doi: 10.1007/s11136-020-02506-5.
- Williams K, Sansoni J, Morris D, et al. Patient-reported outcome measures: literature review. Sydney: ACSQHC; 2016.
- McKercher JP, Slade SC, Jazayeri JA, et al. Patient experiences of codesigned rehabilitation interventions in hospitals: a rapid review. BMJ Open. 2022;12(11):e068241. doi: 10.1136/bmjopen-2022-068241.
- Perry A, Morris M, Unsworth C, et al. Therapy outcome measures for allied health practitioners in Australia: the AusTOMs. Int J Qual Health Care. 2004;16(4):285–291. doi: 10.1093/intqhc/mzh059.
- Wade DT. Measurement in neurological rehabilitation. Curr Opin Neurol Neurosurg. 1992;5(5):682–686.
- Wade DT. What is rehabilitation? An empirical investigation leading to an evidence-based description. Clin Rehabil. 2020;34(5):571–583. doi: 10.1177/0269215520905112.
- Greenhalgh J, Gooding K, Gibbons E, et al. How do patient reported outcome measures (PROMs) support clinician-patient communication and patient care? A realist synthesis. J Patient Rep Outcomes. 2018;2(1):42. doi: 10.1186/s41687-018-0061-6.
- Castro EM, Malfait S, Van Regenmortel T, et al. Co-design for implementing patient participation in hospital services: a discussion paper. Patient Educ Couns. 2018;101(7):1302–1305. doi: 10.1016/j.pec.2018.03.019.
- Lim S, Morris H, Pizzirani B, et al. Evaluating hospital tools and services that were co-produced with patients: a rapid review. Int J Qual Health Care. 2020;32(4):231–239. doi: 10.1093/intqhc/mzaa020.
- Myles PS, Myles DB, Galagher W, et al. Minimal clinically important difference for three quality of recovery scales. Anesthesiology. 2016;125(1):39–45. doi: 10.1097/ALN.0000000000001158.
- Vaillancourt S, Cullen JD, Dainty KN, et al. PROM-ED: development and testing of a Patient-Reported outcome measure for emergency department patients who are discharged home. Ann Emerg Med. 2020;76(2):219–229. doi: 10.1016/j.annemergmed.2019.12.023.
- Lapin BR, Honomichl R, Thompson N, et al. Patient-reported experience with patient-reported outcome measures in adult patients seen in rheumatology clinics. Qual Life Res. 2021;30(4):1073–1082. doi: 10.1007/s11136-020-02692-2.
- Farrington C, Noble B. The use and correlation of patient reported outcome measures (PROMs) in a hospital outpatient setting. BMJ Support. 2014;4(Suppl 1):A5–A5.
- Thestrup Hansen S, Kjerholt M, Friis Christensen S, et al. Haematologists’ experiences implementing patient reported outcome measures (PROMs) in an outpatient clinic: a qualitative study for applied practice. J Patient Rep Outcomes. 2019;3(1):74. doi: 10.1186/s41687-019-0166-6.
- Keeney T, Kumar A, Erler KS, et al. Making the case for patient-reported outcome measures in big-data rehabilitation research: implications for optimizing patient-centered care. Arch Phys Med Rehabil. 2022;103(5s):s140–s145. doi: 10.1016/j.apmr.2020.12.028.
- Chen P, Lin K-C, Liing R-J, et al. Validity, responsiveness, and minimal clinically important difference of EQ-5D-5L in stroke patients undergoing rehabilitation. Qual Life Res. 2016;25(6):1585–1596. doi: 10.1007/s11136-015-1196-z.
- Nolan CM, Longworth L, Lord J, et al. The EQ-5D-5L health status questionnaire in COPD: validity, responsiveness and minimum important difference. Thorax. 2016;71(6):493–500. doi: 10.1136/thoraxjnl-2015-207782.
- Koga R, Sasaki T, Ideta R, et al. The EQ-5D-5L in patients admitted to a hospital in Japan with recent spinal cord injury: a descriptive study. Spinal Cord. 2019;57(11):960–965. doi: 10.1038/s41393-019-0306-0.
- Hobart JC, Williams LS, Moran K, et al. Quality of life measurement after stroke: uses and abuses of the SF-36. Stroke. 2002;33(5):1348–1356. doi: 10.1161/01.str.0000015030.59594.b3.
- Haigh R, Tennant A, Biering-Sorensen F, et al. The use of outcome measures in physical medicine and rehabilitation within Europe. J Rehabil Med. 2001;33(6):273–278.
- Measurement ICfHO. Patient centred outcome measures. 2022; Available from: https://www.ichom.org/patient-centered-outcome-measures/
- Tramonti F, Fanciullacci C, Giunti G, et al. Functional status and quality of life of stroke survivors undergoing rehabilitation programmes in a hospital setting. Neurorehabilitation. 2014;35(1):1–7. doi: 10.3233/NRE-141092.
- Vaz LO, Almeida JC, Froes K, et al. Effects of inspiratory muscle training on walking capacity of individuals after stroke: a double-blind randomized trial. Clin Rehabil. 2021;35(9):1247–1256. doi: 10.1177/0269215521999591.
- Hardy A, Courgeon M, Pellei K, et al. Improved clinical outcomes of outpatient enhanced recovery hip and knee replacements in comparison to standard inpatient procedures: a study of patients who experienced both. Orthop Traumatol Surg Res. 2022;108(6):103236. doi: 10.1016/j.otsr.2022.103236.
- Rissman CM, Keeney BJ, Ercolano EM, et al. Predictors of facility discharge, range of motion, and Patient-Reported physical function improvement after primary total knee arthroplasty: a prospective cohort analysis. J Arthroplasty. 2016;31(1):36–41. doi: 10.1016/j.arth.2015.09.002.
- Alviar MJ, Olver J, Brand C, et al. Do patient-reported outcome measures used in assessing outcomes in rehabilitation after hip and knee arthroplasty capture issues relevant to patients? Results of a systematic review and ICF linking process. J Rehabil Med. 2011;43(5):374–381. doi: 10.2340/16501977-0801.
- Roos EM, Toksvig-Larsen S. Knee injury and osteoarthritis outcome score (KOOS) - validation and comparison to the WOMAC in total knee replacement. Health Qual Life Outcomes. 2003;1(1):17. doi: 10.1186/1477-7525-1-17.
- Morris M, Iansek R, Kirkwood B. A randomized controlled trial of movement strategies compared with exercise for people with Parkinson’s disease. Mov Disord. 2009;24(1):64–71. doi: 10.1002/mds.22295.
- Frazzitta G, Maestri R, Bertotti G, et al. Intensive rehabilitation treatment in early Parkinson’s disease: a randomized pilot study with a 2-year follow-up. Neurorehabil Neural Repair. 2015;29(2):123–131. doi: 10.1177/1545968314542981.
- Heinemann AW, Nitsch KP, Gracz K, et al. Implementing patient-reported outcome measures in inpatient rehabilitation: challenges and solutions. Arch Phys Med Rehabil. 2022;103(5S):S67–S77. doi: 10.1016/j.apmr.2021.05.010.
- Zdravkovic A, Grote V, Pirchl M, et al. Comparison of patient- and clinician-reported outcome measures in lower back rehabilitation: introducing a new integrated performance measure (t2D). Qual Life Res. 2022;31(1):303–315. doi: 10.1007/s11136-021-02905-2.
- Briffa N. The employment of patient-reported outcome measures to communicate the likely benefits of surgery. Patient Relat Outcome Meas. 2018;9:263–266. doi: 10.2147/PROM.S132746.
- Bukstein DA, Guerra DG, Huwe T, et al. A review of shared decision-making: a call to arms for health care professionals. Ann Allergy Asthma Immunol. 2020;125(3):273–279. doi: 10.1016/j.anai.2020.06.030.
- Coronado-Vázquez V, Canet-Fajas C, Delgado-Marroquín MT, et al. Interventions to facilitate shared decision-making using decision aids with patients in primary health care: a systematic review. Medicine (Baltimore). 2020;99(32):e21389. doi: 10.1097/MD.0000000000021389.
- Brusco NK, Atkinson V, Woods J, et al. Implementing PROMS for elective surgery patients: feasibility, response rate, degree of recovery and patient acceptability. J Patient Rep Outcomes. 2022;6(1):73. doi: 10.1186/s41687-022-00483-6.
- Morris ME, Atkinson V, Woods J, et al. Patient judgement of change with elective surgery correlates with patient reported outcomes and quality of life. Healthcare (Basel). 2022;10(6):999. doi: 10.3390/healthcare10060999.
- Heng H, Kiegaldie D, Slade SC, et al. Healthcare professional perspectives on barriers and enablers to falls prevention education: a qualitative study. PLoS One. 2022;17(4):e0266797. doi: 10.1371/journal.pone.0266797.
- Philpot LM, Barnes SA, Brown RM, et al. Barriers and benefits to the use of patient-reported outcome measures in routine clinical care: a qualitative study. Am J Med Qual. 2018;33(4):359–364. doi: 10.1177/1062860617745986.
- Boyce MB, Browne JP, Greenhalgh J. The experiences of professionals with using information from patient-reported outcome measures to improve the quality of healthcare: a systematic review of qualitative research. BMJ Qual Saf. 2014;23(6):508–518. doi: 10.1136/bmjqs-2013-002524.
- Tricco AC, Lillie E, Zarin W, et al. A scoping review on the conduct and reporting of scoping reviews. BMC Med Res Methodol. 2016;16(1):15–15. doi: 10.1186/s12874-016-0116-4.
- Colquhoun HL, Levac D, O'Brien KK, et al. Scoping reviews: time for clarity in definition, methods, and reporting. J Clin Epidemiol. 2014;67(12):1291–1294. doi: 10.1016/j.jclinepi.2014.03.013.
- Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. doi: 10.1080/1364557032000119616.
- Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implementation Sci. 2010;5(1):69. doi: 10.1186/1748-5908-5-69.
- Munn Z, Peters MD, Stern C, et al. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):1–7. doi: 10.1186/s12874-018-0611-x.
- Peters MDJ, Marnie C, Tricco AC, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Implement. 2021;19(1):3–10. doi: 10.1097/XEB.0000000000000277.
- Pham MT, Rajić A, Greig JD, et al. A scoping review of scoping reviews: advancing the approach and enhancing the consistency. Res Synth Methods. 2014;5(4):371–385. doi: 10.1002/jrsm.1123.
- Peters MD, Godfrey C, McInerney P, et al. Chapter 11: Scoping reviews. In: Aromataris E, Munn Z, editors. JBI manual for evidence synthesis. Vol. 2020. Adelaide, Australia: JBI; 2020.
- Dawson J, Doll H, Fitzpatrick R, et al. The routine use of patient reported outcome measures in healthcare settings. BMJ. 2010;340(1):c186–c186. doi: 10.1136/bmj.c186.
- Roos EM, Lohmander LS. The knee injury and osteoarthritis outcome score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes. 2003;1(1):64. doi: 10.1186/1477-7525-1-64.
- Covidence Systematic Review Software. 2022. Available from: www.covidence.org
- Moola S, Munn Z, Tufanaru C, et al. Chapter 7: systematic reviews of etiology and risk. In: Aromataris E, Munn Z, editors. JBI manual for evidence synthesis. Adelaide, Australia: JBI; 2020.
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906. doi: 10.1016/j.ijsu.2021.105906.
- Buhagiar MA, Naylor JM, Harris IA, et al. Effect of inpatient rehabilitation vs a monitored Home-Based program on mobility in patients with total knee arthroplasty: the HIHO randomized clinical trial. JAMA. 2017;317(10):1037–1046. doi: 10.1001/jama.2017.1224.
- Bumberger A, Borst K, Willegger M, et al. Specific knowledge and resilience affect short-term outcome in patients following primary total hip arthroplasty. Arch Orthop Trauma Surg. 2022;142(6):1229–1237. doi: 10.1007/s00402-021-03967-0.
- Hutchinson AG, Gooden B, Lyons MC, et al. Inpatient rehabilitation did not positively affect 6-month patient-reported outcomes after hip or knee arthroplasty. ANZ J Surg. 2018;88(10):1056–1060. doi: 10.1111/ans.14814.
- Johns N, Naylor J, McKenzie D, et al. Is inpatient rehabilitation a predictor of a lower incidence of persistent knee pain 3-months following total knee replacement? A retrospective, observational study. BMC Musculoskelet Disord. 2022;23(1):855. doi: 10.1186/s12891-022-05800-0.
- Mahomed N, Davis A, Hawker G, et al. Inpatient compared with Home-Based rehabilitation following primary unilateral total hip or knee replacement: a randomized controlled trial. J Bone Joint Surg Am. 2008;90(8):1673–1680. doi: 10.2106/JBJS.G.01108.
- Naylor JM, Hart A, Harris IA, et al. Variation in rehabilitation setting after uncomplicated total knee or hip arthroplasty: a call for evidence-based guidelines. BMC Musculoskelet Disord. 2019;20(1):214. doi: 10.1186/s12891-019-2570-8.
- Rohringer M, Fink C, Kellerer JD, et al. Longitudinal observational study on health literacy and clinical outcomes in older adults with total knee arthroplasty in the context of inpatient and outpatient rehabilitation. J Orthop Trauma Rehabil. 2022;29(1):221049172210921. doi: 10.1177/22104917221092161.
- Tribe KL, Lapsley HM, Cross MJ, et al. Selection of patients for inpatient rehabilitation or direct home discharge following total joint replacement surgery: a comparison of health status and out-of-pocket expenditure of patients undergoing hip and knee arthroplasty for osteoarthritis. Chronic Illn. 2005;1(4):289–302. doi: 10.1177/17423953050010041101.
- Uhlig T, Bjørneboe O, Krøll F, et al. Involvement of the multidisciplinary team and outcomes in inpatient rehabilitation among patients with inflammatory rheumatic disease. BMC Musculoskelet Disord. 2016;17(1):18. doi: 10.1186/s12891-016-0870-9.
- Monticone M, Ambrosini E, Laurini A, et al. In-patient multidisciplinary rehabilitation for Parkinson’s disease: a randomized controlled trial. Mov Disord. 2015;30(8):1050–1058. doi: 10.1002/mds.26256.
- Miyai I, Fujimoto Y, Yamamoto H, et al. Long-term effect of body weight-supported treadmill training in Parkinson’s disease: a randomized controlled trial. Arch Phys Med Rehabil. 2002;83(10):1370–1373. doi: 10.1053/apmr.2002.34603.
- Kaseda Y, Ikeda J, Sugihara K, et al. Therapeutic effects of intensive inpatient rehabilitation in advanced Parkinson’s disease. Neurol Clin Neurosc. 2017;5(1):18–21. doi: 10.1111/ncn3.12088.
- Boesen F, Nørgaard M, Skjerbæk AG, et al. Can inpatient multidisciplinary rehabilitation improve health-related quality of life in MS patients on the long term - The Danish MS hospitals rehabilitation study. Mult Scler. 2020;26(14):1953–1957. doi: 10.1177/1352458519884244.
- Drulovic J, Bursac LO, Milojkovic D, et al. MSQoL-54 predicts change in fatigue after inpatient rehabilitation for people with multiple sclerosis. Disabil Rehabil. 2013;35(5):362–366. doi: 10.3109/09638288.2012.704122.
- Aydin T, Kesiktaş FN, Oren MM, et al. Sarcopenia in patients following stroke: an overlooked problem. Int J Rehabil Res. 2021;44(3):269–275. doi: 10.1097/MRR.0000000000000487.
- Fernandez Sanchis D, Cuenca Zaldivar JN, Calvo S, et al. Cost-effectiveness of upper extremity dry needling in the rehabilitation of patients with stroke. Acupunct Med. 2022;40(2):160–168. doi: 10.1177/09645284211055750.
- Forster SD, Gauggel S, Loevenich R, et al. A microanalysis of mood and self-reported functionality in stroke patients using ecological momentary assessment. Front Neurol. 2022;13:854777. doi: 10.3389/fneur.2022.854777.
- Groeneveld IF, Goossens PH, van Meijeren-Pont W, et al. Value-Based stroke rehabilitation: feasibility and results of patient-reported outcome measures in the first year after stroke. J Stroke Cerebrovasc Dis. 2019;28(2):499–512. doi: 10.1016/j.jstrokecerebrovasdis.2018.10.033.
- Hartley T, Burger M, Inglis-Jassiem G. Post stroke health-related quality of life, stroke severity and function: a longitudinal cohort study. Afr J Disabil. 2022;11:947.
- Jiang H, Li H, Wang Z, et al. Effect of early cognitive training combined with aerobic exercise on quality of life and cognitive function recovery of patients with poststroke cognitive impairment. J Healthc Eng. 2022;2022:1–7. doi: 10.1155/2022/9891192.
- Wong Y, Li CJ, Ada L, et al. Upper limb training with a dynamic hand orthosis in early subacute stroke: a pilot randomized trial. JRM. 2022;54:jrm00279. doi: 10.2340/jrm.v54.2231.
- Eaton R, Duff J, Wallace M, et al. The value of the whole picture: rehabilitation outcome measurement using patient self-report and clinician-based assessments after spinal cord injury. Spinal Cord. 2022;60(1):71–80. doi: 10.1038/s41393-021-00677-7.
- Finley M, Euiler E, Baehr L, et al. Relationship of psychosocial factors and musculoskeletal pain among individuals with newly acquired spinal cord injury. Spinal Cord Ser Cases. 2021;7(1):61. doi: 10.1038/s41394-021-00415-4.
- Maggio MG, Naro A, De Luca R, et al. Body representation in patients with severe spinal cord injury: a pilot study on the promising role of powered exoskeleton for gait training. JPM. 2022;12(4):619. doi: 10.3390/jpm12040619.
- Benzer W, Platter M, Oldridge NB, et al. Short-term patient-reported outcomes after different exercise-based cardiac rehabilitation programmes. Eur J Cardiovasc Prev Rehabil. 2007;14(3):441–447. doi: 10.1097/HJR.0b013e32802bf7ae.
- Passantino A, Guida P, Rizzo C, et al. Malnutrition in patients admitted to in-hospital cardiac rehabilitation: clinical correlates and association with mortality. Monaldi Arch Chest Dis. 2021;92(2):24. doi: 10.4081/monaldi.2021.1960.
- Péran L, Beaumont M, Le Ber C, et al. Effect of neuromuscular electrical stimulation on exercise capacity in patients with severe chronic obstructive pulmonary disease: a randomised controlled trial. Clin Rehabil. 2022;36(8):1072–1082. doi: 10.1177/02692155221091802.
- Scaglione A, Panzarino C, Modica M, et al. Short- and long-term effects of a cardiac rehabilitation program in patients implanted with a left ventricular assist device. PLoS One. 2021;16(12):e0259927. doi: 10.1371/journal.pone.0259927.
- Weberg M, Hjermstad MJ, Hilmarsen CW, et al. Inpatient cardiac rehabilitation and changes in self-reported health related quality of life–A pilot study. Ann Phys Rehabil Med. 2013;56(5):342–355. doi: 10.1016/j.rehab.2013.03.004.
- Tamulevičiūtė-Prascienė E, Beigienė A, Lukauskaitė U, et al. Effectiveness of additional resistance and balance training and telephone support program in exercise-based cardiac rehabilitation on quality of life and physical activity: randomized control trial. Clin Rehabil. 2022;36(4):511–526. doi: 10.1177/02692155211065632.
- Grote V, Unger A, Bottcher E, et al. General and disease-specific health indicator changes associated with inpatient rehabilitation. J Am Med Dir Assoc. 2020;21(12):2017.e2010–2017.e2027. doi: 10.1016/j.jamda.2020.05.034.
- Zidarov D, Swaine B, Gauthier-Gagnon C. Quality of life of persons with lower-limb amputation during rehabilitation and at 3-month follow-up. Arch Phys Med Rehabil. 2009;90(4):634–645. doi: 10.1016/j.apmr.2008.11.003.
- Seyedoshohadaee M, Ghezeljeh TN, Samimi R, et al. Implementation of a nursing rehabilitation model to improve quality of life of patients with hand burns: a randomized clinical trial. Eur J Transl Myol. 2022;32:10650.
- Froutan R, Saberi A, Ahmadabadi A, et al. The effect of a recreational therapy program on the pain anxiety and quality of life of patients with burn injuries: a randomized clinical trial. J Burn Care Res. 2022;43(2):381–388. doi: 10.1093/jbcr/irab153.
- Zal M, Deldar K, Froutan R, et al. Rehabilitation of burn victims: improving quality of life in victims with face and neck burn through an augmented reality coupled pamphlet. J Burn Care Res. 2022;44:311.
- Do JH, Gelvosa MN, Choi KY, et al. Effects of multimodal inpatient rehabilitation vs conventional pulmonary rehabilitation on physical recovery after esophageal cancer surgery. Arch Phys Med Rehabil. 2022;103(12):2391–2397. doi: 10.1016/j.apmr.2022.05.019.
- Faller H, Hass HG, Engehausen D, et al. Supportive care needs and quality of life in patients with breast and gynecological cancer attending inpatient rehabilitation. A prospective study. Acta Oncol. 2019;58(4):417–424. doi: 10.1080/0284186X.2018.1543947.
- Heß V, Meng K, Schulte T, et al. Decreased mental health, quality of life, and utilization of professional help in cancer patients with unexpressed needs: a longitudinal analysis. Psychooncology. 2022;31(5):725–734. doi: 10.1002/pon.5856.
- Riedl D, Giesinger JM, Wintner LM, et al. Improvement of quality of life and psychological distress after inpatient cancer rehabilitation: results of a longitudinal observational study. Wien Klin Wochenschr. 2017;129(19–20):692–701. doi: 10.1007/s00508-017-1266-z.
- Morris ME, Haines T, Hill AM, et al. Divesting from a scored hospital fall risk assessment tool (FRAT): a cluster randomized non-inferiority trial. J Am Geriatr Soc. 2021;69(9):2598–2604. doi: 10.1111/jgs.17125.
- Kennedy P, Hamilton L. The needs assessment checklist: a clinical approach to measuring outcome. Spinal Cord. 1999;37(2):136–139. doi: 10.1038/sj.sc.3100745.
- Jones PW, Quirk FH, Baveystock CM. The St George’s respiratory questionnaire. Respir Med. 1991;85(Suppl B):25–31; discussion 33–27. doi: 10.1016/s0954-6111(06)80166-6.
- Brady TJ. Measures of self-efficacy: arthritis self-efficacy scale (ASES), arthritis self-efficacy scale-8 item (ASES-8), children’s arthritis self-efficacy scale (CASE), chronic disease self-efficacy scale (CDSES), parent’s arthritis self-efficacy scale (PASE), and rheumatoid arthritis self-efficacy scale (RASE). Arthritis Care Res (Hoboken). 2011;63(Suppl 11):S473–S485.
- Fairbank JC, Pynsent PB. The oswestry disability index. Spine (Phila PA 1976). 2000;25(22):2940–2952; discussion 2952. doi: 10.1097/00007632-200011150-00017.
- Boone DA, Coleman KL. Use of the prosthesis evaluation questionnaire (PEQ). JPO. 2006;18(Proceedings):P68–P79. doi: 10.1097/00008526-200601001-00008.
- Romano J, Jensen M, Turner J. The chronic pain coping inventory-42: reliability and validity. Pain. 2003;104(1–2):65–73. doi: 10.1016/s0304-3959(02)00466-9.
- Jones PW. St. George’s respiratory questionnaire: MCID. COPD. 2005;2(1):75–79. doi: 10.1081/copd-200050513.
- Hambly K. The use of the tegner activity scale for articular cartilage repair of the knee: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2011;19(4):604–614. doi: 10.1007/s00167-010-1301-3.
- Mørup-Petersen A, Skou ST, Holm CE, et al. Measurement properties of UCLA activity scale for hip and knee arthroplasty patients and translation and cultural adaptation into Danish. Acta Orthop. 2021;92(6):681–688. doi: 10.1080/17453674.2021.1977533.
- Preedy VR. Multiple sclerosis quality of life-54 questionnaire. In: Kreutzer JS, DeLuca J, Caplan B, editors. Encyclopedia of clinical neuropsychology. New York (NY): Springer New York; 2011. p. 1684–1685.
- Meyer AM, Bartram MP, Antczak P, et al. A tailored discharge program improves frailty and mood in patients undergoing usual rehabilitative care: a randomized controlled trial. J Am Med Dir Assoc. 2022;23(12):1962.e1–1962.e13. doi: 10.1016/j.jamda.2022.09.003.
- Bremander AB, Holmstrom G, Bergman S. Depression and age as predictors of patient-reported outcome in a multidisciplinary rehabilitation programme for chronic musculoskeletal pain. Musculoskeletal Care. 2011;9(1):41–48. doi: 10.1002/msc.198.
- Khanna M, Sivadas D, Gupta A, et al. Impact of inpatient rehabilitation on quality of life among stroke patients. J Neurosci Rural Pract. 2022;13(4):800–803. doi: 10.25259/JNRP-2022-1-18-R1-(2322).
- Wan CS, Reijnierse EM, Maier AB. Risk factors of readmissions in geriatric rehabilitation patients: RESORT. Arch Phys Med Rehabil. 2021;102(8):1524–1532. doi: 10.1016/j.apmr.2021.01.082.
- Kemmler W, Sieber C, Freiberger E, et al. The SARC-F questionnaire: diagnostic overlap with established sarcopenia definitions in older German men with sarcopenia. Gerontology. 2017;63(5):411–416. doi: 10.1159/000477935.
- Jackson-Koku G. Beck depression inventory. Occup Med (Lond). 2016;66(2):174–175. doi: 10.1093/occmed/kqv087.
- Bjelland I, Dahl AA, Haug TT, et al. The validity of the hospital anxiety and depression scale: an updated literature review. J Psychosom Res. 2002;52(2):69–77. doi: 10.1016/s0022-3999(01)00296-3.
- Connor KM, Davidson JR. Development of a new resilience scale: the Connor‐Davidson resilience scale (CD‐RISC). Depress Anxiety. 2003;18(2):76–82. doi: 10.1002/da.10113.
- Herschbach P, Berg P, Dankert A, et al. Fear of progression in chronic diseases: psychometric properties of the fear of progression questionnaire. J Psychosom Res. 2005;58(6):505–511. doi: 10.1016/j.jpsychores.2005.02.007.
- Fonseca-Pedrero E, Ortuno-Sierra J, Paino M, et al. Screening the risk of bipolar spectrum disorders: validity evidence of the mood disorder questionnaire in adolescents and young adults. Revista de Psiquiatría y Salud Mental (English Edition). 2016;9(1):4–12. doi: 10.1016/j.rpsmen.2016.01.006.
- Gnambs T, Scharl A, Schroeders U. The structure of the rosenberg self-esteem scale. Zeitschrift Für Psychologie. 2018;226(1):14–29. doi: 10.1027/2151-2604/a000317.
- Krupp LB, LaRocca NG, Muir-Nash J, et al. The fatigue severity scale: application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol. 1989;46(10):1121–1123. doi: 10.1001/archneur.1989.00520460115022.
- McNeil DW, Rainwater AJ. Development of the fear of pain questionnaire-III. J Behav Med. 1998;21(4):389–410. doi: 10.1023/a:1018782831217.
- Finley MA, Euiler E. Association of musculoskeletal pain, fear-avoidance factors, and quality of life in active manual wheelchair users with SCI: a pilot study. J Spinal Cord Med. 2020;43(4):497–504. doi: 10.1080/10790268.2019.1565717.
- Kahl C, Cleland JA. Visual analogue scale, numeric pain rating scale and the McGill pain questionnaire: an overview of psychometric properties. Phys Ther Rev. 2005;10(2):123–128. doi: 10.1179/108331905X55776.
- Sullivan MJ, Bishop SR, Pivik J. The pain catastrophizing scale: development and validation. Psychol Assess. 1995;7(4):524–532. doi: 10.1037/1040-3590.7.4.524.
- Altuğ F, Ünal A, Kilavuz G, et al. Investigation of the relationship between kinesiophobia, physical activity level and quality of life in patients with chronic low back pain 1. J Back Musculoskelet Rehabil. 2016;29(3):527–531. doi: 10.3233/BMR-150653.
- Montorio I, Izal M. The geriatric depression scale: a review of its development and utility. Int Psychogeriatr. 1996;8(1):103–112. doi: 10.1017/s1041610296002505.
- Snaith RP. The hospital anxiety and depression scale. Health Qual Life Outcomes. 2003;1(1):29. doi: 10.1186/1477-7525-1-29.
- Oosterveer DM, Wermer MJH, Volker G, et al. Are there differences in Long-Term functioning and recovery between hemorrhagic and ischemic stroke patients receiving rehabilitation? J Stroke Cerebrovasc Dis. 2022;31(3):106294. doi: 10.1016/j.jstrokecerebrovasdis.2021.106294.
- Bordne S, Rietz C, Schulz RJ, et al. Behavioral and emotional quality of life of patients undergoing inpatient geriatric rehabilitation. Rehabil Psychol. 2020;65(3):299–310. doi: 10.1037/rep0000332.
- Feng Y-S, Kohlmann T, Janssen MF, et al. Psychometric properties of the EQ-5D-5L: a systematic review of the literature. Qual Life Res. 2021;30(3):647–673. doi: 10.1007/s11136-020-02688-y.
- Ashford S, Brown S, Turner-Stokes L. Systematic review of patient-reported outcome measures for functional performance in the lower limb. J Rehabil Med. 2015;47(1):9–17. doi: 10.2340/16501977-1889.
- Harris IA, Peng Y, Cashman K, et al. Association between patient factors and hospital completeness of a patient-reported outcome measures program in joint arthroplasty, a cohort study. J Patient Rep Outcomes. 2022;6(1):32. doi: 10.1186/s41687-022-00441-2.
- Heath EL, Ackerman IN, Cashman K, et al. Patient-reported outcomes after hip and knee arthroplasty: results from a large national registry. Bone Jt Open. 2021;2(6):422–432. doi: 10.1302/2633-1462.26.BJO-2021-0053.R1.
- Terwee CB, Zuidgeest M, Vonkeman HE, et al. Common patient-reported outcomes across ICHOM standard sets: the potential contribution of PROMIS®. BMC Med Inform Decis Mak. 2021;21(1):259. doi: 10.1186/s12911-021-01624-5.
- Kayes NM, Papadimitriou C. Reflecting on challenges and opportunities for the practice of person-centred rehabilitation. Clin Rehabil. 2023;37(8):1026–1040. doi: 10.1177/02692155231152970.
Appendix
Database(s): Ovid MEDLINE(R) ALL 1946 to 31 October 2022.