Abstract
Objectives
The risk of falls increases with age and often requires an emergency medical service (EMS) response. We compared the characteristics of patients attended by EMS in response to repeat falls within 30 days and 12 months of their first EMS-attended fall; and explored the number of days between the index fall and the subsequent fall(s).
Methods
This retrospective cohort study included all adults (> =18 years of age) who experienced their first EMS-attended fall between 1 January 2016 and 31 December 2020, followed up until 31 December 2021. Patients who experienced > =1 subsequent fall, following their first recorded fall, were defined as experiencing repeat falls. Multivariable logistic regression was used to identify the factors associated with repeat falls; and Kaplan-Meier analysis was used to estimate the time (in days) between consecutive EMS-attended falls.
Results
A total of 128,588 EMS-attended fall-related incidents occurred involving 77,087 individual patients. Most patients, 54,554 (71%) were attended only once for a fall-related incident (30,280 females; median age 73 years, inter-quartile range (IQR): 55–84). A total of 22,533 (29%) patients experienced repeat EMS-attended falls (13,248 females; median age 83 years, IQR: 74–89, at first call). These 22,533 patients accounted for 58% (74,034 attendances) of all EMS-attendances to fall-related incidents. Time between EMS-attended falls decreased significantly the more falls a patient sustained. Among the 22,533 patients who experienced repeat falls, 13,363 (59%) of repeat falls occurred within 12 months: 3,103 (14%) of patients sustained their second fall within 30 days of their index fall, and 10,260 (46%) between 31 days to 12 months. Patients who were transported to the hospital, via any urgency, at their first EMS-attended fall, had a reduced odds of sustaining a second EMS-attended fall within both 30 days and 31 days to 12 months, compared to non-transported patients.
Conclusion
Nearly 30% of all patients attended by EMS for a fall, sustained repeat falls, which collectively accounted for nearly 60% of all EMS-attendances to fall-related incidents. Further exploration of the role EMS clinicians play in identifying and referring patients who sustain repeat falls into alternative pathways is needed.
Introduction
Emergency Medical Services (EMS) are responding to an increasing number of people who have fallen (Citation1–4). Increasing age is a risk factor associated with falling (Citation5, Citation6). As the proportion of older adults in the population increases globally, an increase in the incidence of falls is growing concurrently (Citation7). Falls at any age have the potential to result in injuries ranging from minor to life threatening or even death (Citation8), and often require prehospital emergency care and transport to the hospital. Moreover, there is a risk of a subsequent fall following an initial fall (Citation2, Citation9, Citation10).
Patients categorized as experiencing ‘repeat falls’ are described as sustaining one or more subsequent falls, following their initially recorded fall (Citation2, Citation9, Citation10). The risk of repeat falls increases with age and immobility (Citation5, Citation9, Citation11–13). Repeat falls are shown to be associated with reduced independence (Citation14), reduced quality of life (Citation14), and with repeat transports to hospital in older adults (Citation5, Citation9, Citation11–13). Multiple EMS systems globally have reported an increase in responses for repeat falls (Citation1–4, Citation11). A study in the USA, showed that among older adults attended by EMS for a fall, nearly 20% experienced one repeat transport within 30 days, and 40% within 6 months (Citation11).
This study aimed to examine EMS-attended adults who sustained repeat falls in Western Australia (WA). The study objectives were to 1) compare the characteristics of patients who sustained one fall compared to those who sustained repeat falls; 2) describe the characteristics of patients attended in response to repeat falls within 30 days and 31 days to 12 months of their first EMS-attended fall; 3) explore the number of days between the index fall and the subsequent fall(s); and 4) compare the mortality in patients who sustained one fall compared to those who sustained repeat falls.
Methods
Study Design and Setting
This retrospective cohort study included all adult patients (≥18 years of age) attended by St. John Western Australia (SJWA) EMS in response to a fall between 1 January 2015 and 31 December 2021. As the sole provider of ground-based EMS in the state of WA, SJWA covers the largest geographical area (2.5 million square kilometers) of any single EMS agency in the world; responding to more than 280,000 calls for EMS assistance each year (Citation15). The SJWA EMS is staffed by paramedics in the metropolitan area, with a mix of paramedic and emergency medical technicians (EMTs) in rural areas (known as volunteer ambulance officer crews in WA) (Citation15). Following an EMS attendance, a patient can be transported to hospital via transport urgency 1 (most urgent) to 5 (least urgent). During the study period no alternative referral pathways to other healthcare providers were available to EMS personnel in WA when managing patients who fell.
Data Collection/Data Source
Data were obtained from SJWA EMS electronic patient care records (ePCR), where paramedics and EMTs (hereafter collectively referred to as EMS clinicians) described each patient’s presentation and clinical management, together with EMS dispatch data. Falls were identified by researchers using data from the Medical Priority Dispatch System (Citation16), and by searching free-text fields within the ePCR fields, using manual screening, machine learning and natural language processing (Citation17). The machine learning model used to identify the cohort presented in this study has been previously described (Citation17). All identified falls from these sources were included after removal of duplicate cases. Falls identified as: suicide, patient not located on scene, motor vehicle incidents, assaults or kicked by an animal were excluded.
Using probabilistic linkage techniques, we linked records in the WA Death Registry (Citation18) with those in the ePCR by surname, given name, date of birth, and residential address. Date of death was extracted for all patients with a death registration. We also linked records in the ePCR associated with the same individual using the same techniques, to identify people who had multiple emergency EMS attendances. For this linkage we used “Fine-grained record linkage software” (Fril, version 2.1.5, Emory University and Center for Diseases Control and Prevention, Atlanta, Georgia, U.S.), supplemented by Python Record Linkage Toolkit (version 0.14.0). Fril has elsewhere been reported to perform well for identifying the same individual, with 99% precision (positive predictive value) and 95% recall (sensitivity) (Citation19). This screening could include false positive links, so it was refined by using machine learning techniques (Citation17). Missing examination texts were exceedingly rare because this field on the ePCR is where the primary EMS clinicians record details of the case.
We defined a patient’s index fall as their first recorded fall in the data set. Therefore, patients who only sustained one single fall during the study period, only sustained their index fall. We defined patients who experienced > =1 subsequent fall, following their index fall, as experiencing repeat falls. For the purpose of this study, and to identify patients who experienced repeat falls, a one-year phase-in period and one-year follow-up period were applied to this data set.
The data extracted were from 1st of January 2015 to the 31st of December 2021. Patients who sustained any EMS-attended fall in 2015 (one-year phase-in period) were excluded, as were any patients who experienced their index fall in 2021 (the one-year follow-up period). This allowed follow-up on all patients who sustained their index fall in 2016 to 2020, as this study focused on subsequent falls that occurred within 30 days and 12 months of a patient’s index fall (Citation2). A 5-year cohort of all EMS-attended adults who sustained their index fall between 1 January 2016 and 31 December 2020 formed the study cohort.
Data Extraction
Patients’ demographic details (age, sex); EMS dispatch priority to the patient [from 1 (highest) to 3 (lowest)]; clinical information (Glasgow coma scale (GCS) score, pain score (0–10), medications administered (time, route of administration)) stratified by sex; other interventions (type, effect) stratified by sex, were extracted from the ePCR and computer aided dispatch system (CAD). Free texts were searched in the event of missing demographic or dispatch priority data. Injury location was extracted and allocated into the following categories: head and neck; hip to foot; trunk, back and pelvis; and shoulder to hand, as described in the ePCR (Citation20). Any reported injury was included in the analysis of results as described in the ePCR, e.g., abrasion, bleeding, dislocation.
Patient disposition (non-transport/transported from the scene to hospital) was extracted. For transported patients, transport urgency level, was determined by the EMS clinicians at the scene. Transport destination level was coded according to the WA trauma service role delineation and trauma service organizational chart (Citation21). A triage revised trauma scores (tRTS) was computed as a surrogate measure for patients’ physiological condition severity level (Citation22). The first measured values of systolic blood pressure (SBP), Glasgow coma scale (GCS), and respiratory rate (RR) recorded on the ePCR were used to calculate the tRTS, from ‘0′ to ‘12′, for each patient. Lower tRTS scores indicated a high injury severity (Citation22).
Measures/Outcomes
We compared the characteristics and outcomes for patients with repeat falls versus a single fall, and explored factors associated with repeat falls. The independent variables explored included: demographic information (age, sex), dispatch priority, observations [SBP, pain, injury status and location (head or neck; hip to foot; shoulder to hand; and trunk, back or pelvis), respiration rate, oxygen, GCS], and patient disposition (transport urgency, non-transport, and transport destination).
Statistical Analysis
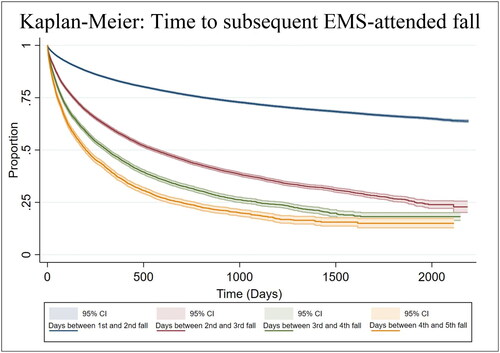
Descriptive statistics were used to summarize the characteristics of all study participants. Kaplan-Meier plots estimating the time (in days) between consecutive EMS-attended falls were generated for the first five patient falls. Patients who only sustained n EMS-attended falls (where n < 5) in the study period, or who were reported to have died after their n-th fall, were censored for their n + 1 fall. The censor date was either the 31 December 2021 or the patient’s date of death, if earlier. Differences in time between consecutive falls were assessed using log-rank tests. Odds ratios (OR) were produced in the multivariable logistic regression allowing for the identification of factors (from the patient’s index fall) that are associated with the likelihood of a repeat fall. The patient data analyzed in the model reflects all patient data collected at their first EMS-attended fall. A Wald test was conducted on all categorical variables to assess their significance as predictors of the dependent variable. Data analysis was performed using STATA statistical software Version 17.0 (College Station, TX, USA).
We could not derive a cox proportional hazards model (proportional hazards assumption) and non-proportional hazards models (Weibull survival distribution: generalized gamma distribution) to determine the association between survival time (time to second EMS-attended fall) of patients because our data violated the model’s assumptions, even after data stratification. Multivariable logistic regression was used to investigate the association between independent variables recorded at a patient’s index fall and the likelihood of experiencing a repeat fall within two-time frames: i) within 30 days, and ii) between 31 and 365 days of the index fall. To ensure all patients were alive and therefore at risk of experiencing a second fall, patients who died within 30 days of their index fall were excluded from the regression model exploring repeat falls within 30 days. Similarly, patients who died within 365 days of their index fall were excluded from the regression model exploring repeat falls between 31 and 365 days of their index fall. All patients who were therefore alive and could potentially have experienced the outcome of interest, namely a second fall, were included in the model.
Ethical Approval
Curtin University Human Research Ethics Committee approval [HR128/2013-85, 09 March 2022] and SJWA Research Governance Committee approval [11 March 2022] was obtained.
Results
Study Cohort
Between 1 January 2016 and 31 December 2020, 77,087 patients sustained their index fall. Following-up until 31 December 2021 (12 month follow up), we included 128,588 EMS-attendances to falls. A total of 54,554 (71%) individual patients only had one EMS-attended fall-related incident. A total of 22,533 (29%) individual patients had more than one EMS-attended fall. These 22,533 patients accounted for 58% (74,034 attendances) of all EMS-attendances to fall-related incidents. graphically presents all EMS-attendances to falls by fall frequency. A total of 177 falls identified as: suicide, patient not located on scene, motor vehicle incidents, assaults or kicked by an animal were excluded.
Figure 1. The total number of subsequent EMS-attended falls for the 77,087 adults who sustained an index EMS-attended fall between 1 January 2016 and 31 December 2020.
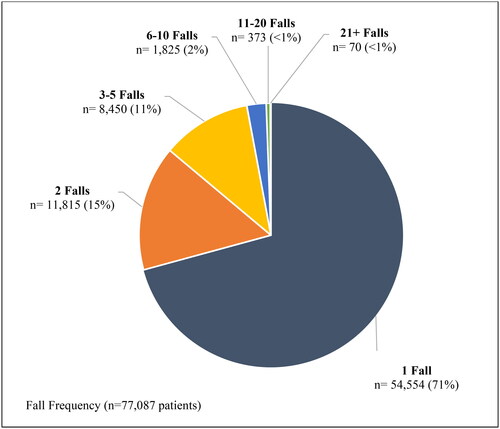
The 22,533 (29%) patients who experienced repeat falls sustained between 2 and 131 EMS attended falls in total (median: 2, interquartile range (IQR): 2–4). Age ranged from 18 to 112 years at the first fall; 19,843 (88%) were aged 65 years or older and 9,261 (41%) were 85 years of age or older. Overall, 13,363 (59%) of repeat falls occurred within 12 months: 3,103 (14%) of patients sustained their second fall within 30 days of their index fall, and 10,260 (46%) between 31 days to 12 months. provides patient and case information. Some patients experienced a high number of repeat falls, with 568 (3%) of patients sustaining 10 or more falls, accounting for 8,264 (11%) of all EMS-attendances to falls. Of these 568 patients, 104 (18%) had their second fall within 30 days of their index fall, 342 (60%) had their second fall within 31 to 365 days of their index fall (total in 12 months, 446, 79%), and 52 (9%) died within 30 days of their last fall.
Table 1. Characteristics of all 77,087 EMS-attended patients who fell.
Injuries, Observations, and Treatments
A total of 10,456 (46%) patients who sustained repeat falls were injured at their first fall (6,371 females, 61%). Within this cohort of patients who sustained repeat falls, females had a higher reported frequency of head and neck (2,650, 59%), trunk, back and pelvis (1,166, 62%), shoulder to hand (2,011, 60%), and hip to foot injuries (2,561, 62%), than males at their first fall. Patients median GCS at their first fall was 15 [IQR 15–15], regardless of sex or whether they sustained repeat falls. For patients who experienced repeat falls, median GCS from their 2nd fall was 15 [IQR 14–15] regardless of sex. Median tRTS for all patients, male or female, was 12 [IQR 12–12]. Males had a median pain score of ‘0′ at their only fall (IQR: 0–4) and at their first of multiple falls (IQR: 0–1). Females had a median pain score of ‘1′ at their only fall (IQR: 0–6) and ‘0′ at their first of multiple falls (IQR: 0–3).
A higher frequency of medication administration is shown in patients who sustained one single fall (19,570, 39%) compared to patients who sustained repeat falls, at their first fall (5,322, 24%). Intravenous cannulation, 3 lead and 12 lead electrocardiogram (ECG) were the most frequently used interventions. Injuries, observations, and treatments/interventions are detailed further in .
Disposition
A total of 66,121 (86%) patients were transported to hospital at their index fall, shown in . Of the 22,533 patients who experienced repeat falls, 18,075 (80%) were transported at their index fall. A total 8,636 (48%) patients experienced a repeat transport (transported at first and second fall) within 12 months: 1,714 within 30 days and 6,922 within 31 days to 12 months of their initial transport. Further details about patient disposition are shown in .
Table 2. Repeat transport to hospital within 30 days and 12 months of index fall in patients who sustained repeat falls.
reports total patient deaths within 30 days, or 365 days of their index and final fall. In patients who sustained one fall, 3,012 (6%) died within 30 days of their fall and 8,604 (16%) within 365 days of their fall. In patients who sustained repeat falls, fewer died within 30 days of their index fall (206, 1%), and within 365 days of their index fall (2,614, 12%) compared to those who sustained one fall.
Kaplan-Meier
Time between calls decreased significantly the more falls a patient sustained (p < 0.001), as shown in . The Kaplan-Meier estimates for median time between the second and third fall was 558 days (18 months) [25%: 135 days; 75%: 1,913 days]. The median time between third and fourth fall was 310 days (10 months) [25%: 76 days; 75%: 1,090 days]. The median time between fourth and fifth fall was 199 days (6 months) [25%: 53 days; 75%: 697 days].
Multivariable Logistic Regression: Likelihood of Experiencing a Repeat Fall
The odds ratios of second EMS-attended fall following an index fall, are shown in . All assessed variables were found to be independently associated with the odds ratio of a patient sustaining a second fall within 30 days or 31 days to 12 months of their index fall.
Table 3. Factors associated with a second EMS-attended fall within 30 days and 31 to 365 days following the index fall: a Multivariable logistic regression model.
Male patients attended by the EMS for an index fall had an increased odds of sustaining a second fall within 30 days and 31 days to 12 months. Older adults (>65 years of age) and patients attended via low dispatch priority (2 vs 1, 3 vs 1) at their index fall had an increased odds of a second EMS-attended fall within 30 days and 31 days to 12 months. Patients with a reported injury at their first fall had a reduced odds of sustaining a second EMS-attended fall within 30 days and 31 days to 12 months. Patients who were transported, via any urgency, at their index EMS-attended fall, had a reduced odds of sustaining a second EMS-attended fall within 30 days and 31 days to 12 months, compared to non-transported patients.
Discussion
Patients who experienced repeat EMS-attended falls accounted for 29% of all patients attended in response to fall-related incidents, and accounted for nearly 60% of all EMS-attendances to fall-related incidents, in the same time period. The results of this study confirm previous findings that a large proportion of EMS workload relating to falls is attending the same patients repeatedly.
There is a growing body of literature indicating that older adults are increasingly using EMS services in response to falls, as they are a vulnerable population at risk of repeat falls (Citation23). Our findings are consistent with a study from the USA that showed nearly one third of older adults who called 911 for a fall, called EMS again for fall assistance (Citation9). Similarly, our results showed that time between subsequent falls decreases, with consecutive falls (Citation9). We found that older, uninjured, non-transported patients had an increased odds of sustaining a second EMS-attended fall within 30 days and 12 months of their initial fall. In our study, 9% of patients who sustained repeat falls, experienced a repeat transport within 30 days of their index fall. Evans et al., (USA) found 18.3% of EMS-attended patients who fell experienced a repeat transport in 30 days, higher than our findings at 30 days (Citation11). This difference may be due to geographical differences in study location, as WA has a much larger area than North Carolina, with North Carolina accounting for only 5% of the square kilometers of WA.
Transport to hospital became progressively less frequent with subsequent EMS responses, which is consistent with findings from Quatman et al. in a study based in the USA (Citation9), which showed a reduction in transport frequency from 75% of first calls to 21% after the fourth call. We found that patients transported (via any urgency) at their first EMS-attended fall, have a reduced odds of a second EMS-attended fall within the subsequent 30 days or 31 day to 12-month period. Tiedemann et al., (Citation23, Citation24) recommended that the identification of individuals in Australia at high risk of future falls, for onward referral to prevention interventions may reduce EMS-attendances for repeat falls. Our findings show that patients transported at their first fall were less likely to sustain repeat falls. This is potentially the result of patients experiencing onward referrals to preventative interventions during emergency departments or hospital admission, although this requires further research (Citation23, Citation24). While some patients who fall and require EMS, do not require transport to the hospital, guidelines for EMS clinicians to identify and target these high-risk patients, and to refer to alternative falls programs, could be beneficial in addressing this growing demand (Citation25–29).
For patients who experienced repeat EMS-attended falls in WA, time between EMS-attendances decreased significantly, the more falls the patient sustained. Given this, the need to identify those patients at risk of sustaining repeat EMS-attended falls is crucial. Our findings show that demographic information can be used to identify patients at risk of repeat EMS-attended falls. Specifically, males have a high risk of sustaining repeat falls, and the older a patient is at their first EMS-attended fall, the more likely they are to sustain repeat EMS-attended falls. Our findings identified that patients who were uninjured and not transported at their first EMS-attended fall, are more likely to sustain repeat falls. Clinical practice guidelines and prehospital personnel training could potentially benefit from including these patient factors to support prehospital personnel in their identification of patients at a high risk of sustaining repeat EMS-attended falls. Our findings reinforce the urgency of developing and implementing onward referrals to prevention interventions from the prehospital setting and identifying high-risk patients in a timely manner (Citation23, Citation24).
The effectiveness of falls prevention programs has been demonstrated globally (Citation9, Citation12, Citation30–32). A systematic review and meta- analysis (Citation32), indicated that RCT’s of falls prevention programs effectively demonstrate a reduction in falls rates by between 9% and 10% in multifactorial interventions (Citation25, Citation26, Citation32, Citation33). The Falls Decision tree with the London Ambulance service (Citation34) and the St John New Zealand’s referral to their falls prevention service (Citation35) are established examples of alternate referral pathways in the prehospital setting. Demand for EMS by older adults who fall, when not addressed with interventions to foster falls prevention, has increased since 2000 (Citation1, Citation2, Citation4, Citation13, Citation25). Research into the implementation of referral pathways by EMS identified facilitators and barriers when implementing prehospital guidelines (Citation25–27). Further exploration of EMS organizational structures that currently work effectively with referral pathways, could assist in diversifying strategies to approach the development of prehospital guidelines for referral to other services (Citation25–27). Despite the evidence supporting the efficacy of falls prevention programs, a communication gap exists between EMS and community-based allied health and alternative health care pathways (Citation9, Citation24, Citation29, Citation32, Citation33).
Future research exploring EMS-attended falls would benefit by identifying repeat falls, to expand on contributing factors to EMS demand. It is important to consider patients attended by EMS repeatedly for falls when addressing prehospital falls management guidelines. Further exploration of the role EMS clinicians play in identifying and referring patients who sustain repeat falls into alternative pathways is needed. This could potentially be supported by the development of specific education, protocols and guidelines for the prehospital management and referral of older adults who fall.
Limitations
There are several limitations of our study. This study only included those falls patients who were attended by EMS and who called ‘000’; patients who experienced falls or repeated falls and were privately transported, did not call EMS, received care or support in residential aged care facilities only are not included. Socioeconomic, disability, comorbidity status and general medication use are not recorded in the ePCR or CAD and therefore, were not included in this study. It is possible that some EMS attended falls were missed. However, we are confident that all efforts have been made to identify all falls through a combination of manual searching by multiple researchers (PMW, HT, PB, DM), machine learning and natural language processing for data identification (Citation17). Machine learning and natural language processing to identify falls in electronic patient care records from EMS-attendances is a strength of this study, as only 60% of falls cases identified through manual review were actually dispatched as ‘falls’. This is particularly novel as several previous studies have identified falls solely on the basis of a ‘falls’ EMS dispatch code (Citation4, Citation36, Citation37). Finally, the results of our study may not be applicable to other EMS with different EMS staffing profiles and policies.
Conclusions
Considering all EMS-attended adults who fell, nearly a third experienced repeat falls. Of these patients, 59% sustained their second EMS-attended fall within 12 months of their first fall. EMS-attended adults sustained falls in a shorter time frame with every additional fall experienced. This reinforces the importance of having specific prehospital clinical practice guidelines to identify high risk patients at risk of sustaining additional falls in the future. The development of alternative referral pathways to refer patients to allied health and falls prevention programs could support prehospital personnel in their management of patients who sustain, or are at risk of, repeat falls.
Disclosure Statement
RB is a current employee of St John WA and DB is a past employee. JF holds an adjunct research professor position with St John WA and receives research funding from St John WA.
Additional information
Funding
References
- Australian Institute of Health and Welfare: Pointer S. Trends in hospitalised injury due to falls in older people 2007–08 to 2016–17. Injury research and statistics series no. 126. Cat. no. INJCAT 206. Canberra: AIHW; 2019. Report No: 978-1-76054-614-4. https://www.aihw.gov.au/reports/injury/trends-in-hospitalised-injury-due-to-falls/contents/table-of-contents.
- Cox S, Roggenkamp R, Bernard S, Smith K. The epidemiology of elderly falls attended by emergency medical services in Victoria, Australia. Injury. 2018;49(9):1712–9. doi:10.1016/j.injury.2018.06.038.
- Faul M, Stevens JA, Sasser SM, Alee L, Deokar AJ, Kuhls DA, Burke PA. Older adult falls seen by emergency medical service providers: a prevention opportunity. Am J Prev Med. 2016;50(6):719–26. doi:10.1016/j.amepre.2015.12.011.
- Simpson P, Bendall J, Patterson J, Tiedemann A, Middleton P, Close J. Epidemiology of ambulance responses to older people who have fallen in New South Wales, Australia: ambulance response to older fallers. Australas J Ageing. 2013;32(3):171–6. doi:10.1111/j.1741-6612.2012.00621.x.
- World Health Organisation. Falls: WHO. 2021 Apr 26 [accessed 2023 May 20]. https://www.who.int/news-room/fact-sheets/detail/falls.
- World Health Organisation. Step Safety: strategies for preventing and managing falls across the life-course. Geneva. 2021 Apr 27 [accessed 2023 Jan 30]. https://www.who.int/publications/i/item/978924002191-4.
- James SL, Lucchesi LR, Bisignano C, Castle CD, Dingels ZV, Fox JT, Hamilton EB, Henry NJ, Krohn KJ, Liu Z, et al. The global burden of falls: global, regional and national estimates of morbidity and mortality from the Global Burden of Disease Study 2017. Inj Prev. 2020;26(Suppl 2):i3–i11. doi:10.1136/injuryprev-2019-043286.
- Crawley MR, Chapman AJ, Koestner A, Pounders S, Krech L, Lypka M, Fisk C, Iskander G. Fall risk identification throughout the continuum of care for elderly trauma patients: an injury prevention initiative. Injury. 2022;53(11):3715–22. doi:10.1016/j.injury.2022.08.066.
- Quatman CE, Anderson JP, Mondor M, Halweg J, Quatman‐Yates C, Switzer JA. Frequent 911 fall calls in older adults: opportunity for injury prevention strategies. J Am Geriatr Soc. 2018;66(9):1737–43. doi:10.1111/jgs.15457.
- Wallace SP. More than half a million older Californians fell repeatedly in the past year. Policy Brief UCLA Cent Health Policy Res. 2014;(Pb2014-8):1–7.
- Evans CS, Platts-Mills TF, Fern Ez AR, Grover JM, Cabanas JG, Patel MD, Vilke GM, Brice JH. Repeated emergency medical services use by older adults: analysis of a comprehensive statewide database. Ann Emerg Med. 2017;70(4):506–15.e3. doi:10.1016/j.annemergmed.2017.03.058.
- Government of Western Australia. Falls prevention and management in WA: department of Health, WA. 2014 [accessed 2023 Dec 19]. https://ww2.health.wa.gov.au/Articles/F_I/Falls-prevention-and-management-in-WA.
- Ballestas T, Xiao J, McEvoy S, Somerford P. The epidemiology of injury in Western Australia, 2000-2008. Western Australia: Department of Health; 2011.
- Pathania A, Haldar P, Kant S, Gupta S, Pandav C, Bachani D. Prevalence of fall, and determinants of repeat incidents of fall in older persons living in old age homes in the National Capital Territory of Delhi, India. Natl Med J India. 2018;31(6):329–33. doi:10.4103/0970-258X.262912.
- St John Western Australia Ambulance Service. Ambulance and health services: emergency ambulance in Western Australia: SJWA. 2023 [accessed 2023 Aug 2]. https://stjohnwa.com.au/ambulance-and-health-services.
- The Medical Priority Dispatch System: International academies of emergency dispatch (IAED), current version MPDS v14.0. 2023 Mar 14 [accessed 2023 May 24]. https://www.emergencydispatch.org/what-we-do/emergency-priority-dispatch-system/medical-protocol.
- Tohira H, Finn J, Ball S, Brink D, Buzzacott P. Machine learning and natural language processing to identify falls in electronic patient care records from ambulance attendances. Inform Health Soc Care. 2022;47(4):403–13. doi:10.1080/17538157.2021.2019038.
- Department of Justice. The Registry of Births, Deaths and Marriages: government of Western Australia. 2024 Jan 4 [accessed 5 Jan 2024]. https://www.wa.gov.au/organisation/department-of-justice/the-registry-of-births-deaths-and-marriages.
- Jurczyk P, Lu JJ, Xiong L, Cragan JD, Correa A. FRIL: a tool for comparative record linkage. AMIA Annu Symp Proc. 2008;2008:440–4.
- Thomas SL, Muscatello DJ, Middleton PM, Zheng W. Characteristics of fall-related injuries attended by an ambulance in Sydney, Australia: a surveillance summary. N S W Public Health Bull. 2011;22(3-4):49–54. doi:10.1071/NB09034.
- Government of Western Australia Department of Health. State trauma organisational 442 structure. Department of Health. 2018 [accessed 2023 Jun 25]. https://ww2.health.wa.gov.au/Articles/S_T/State-trauma-organisational-structure.
- Champion HR, Sacco WJ, Copes WS, Gann DS, Gennarelli TA, Flanagan ME. A revision of the trauma score. J Trauma Acute Care Surg. 1989;29(5):623–9.
- Tiedemann A, Mikolaizak AS, Sherrington C, Segin K, Lord SR, Close JC. Older fallers attended to by an ambulance but not transported to hospital: a vulnerable population at high risk of future falls. Aust N Z J Public Health. 2013;37(2):179–85. doi:10.1111/1753-6405.12037.
- Tiedemann A, Sherrington C, Orr T, Hallen J, Lewis D, Kelly A, Vogler C, Lord SR, Close JCT. Identifying older people at high risk of future falls: development and validation of a screening tool for use in emergency departments. Emerg Med J. 2013;30(11):918–22. doi:10.1136/emermed-2012-201783.
- Thomas G, Sanchez A, Snooks H. 04 Before the fall: a discussion paper on the organisational difficulties of setting up complex randomised control trials in emergency pre-hospital care. Emerg Med J. 2011;28(3):e1. doi:10.1136/emj.2010.108605.4.
- Snooks H, Cheung WY, Close J, Dale J, Gaze S, Humphreys I, Lyons R, Mason S, Merali Y, Peconi J, et al. Support and Assessment for Fall Emergency Referrals (SAFER 1) trial protocol. Computerised on-scene decision support for emergency ambulance staff to assess and plan care for older people who have fallen: evaluation of costs and benefits using a pragmatic cluster randomised trial. BMC Emerg. 2010;10(2):2.
- Snooks H, Anthony R, Chatters R, Cheung W-Y, Dale J, Donohoe R, Gaze S, Halter M, Koniotou M, Logan P, et al. Support and assessment for fall emergency referrals (SAFER 2) research protocol: cluster randomised trial of the clinical and cost effectiveness of new protocols for emergency ambulance paramedics to assess and refer to appropriate community-based care. BMJ Open. 2012;2(6):e002169. doi:10.1136/bmjopen-2012-002169.
- Snooks HAP, Anthony R, Chatters R, Dale JP, Fothergill RTD, Gaze S, Halter MP, Humphreys I, Koniotou M, Logan PP, et al. Paramedic assessment of older adults after falls, including community care referral pathway: cluster randomized trial. Ann Emerg Med. 2017;70(4):495–505.e28. doi:10.1016/j.annemergmed.2017.01.006.
- Mikolaizak AS, Lord SR, Tiedemann A, Simpson P, Caplan GA, Bendall J, Howard K, Webster L, Payne N, Hamilton S, et al. A multidisciplinary intervention to prevent subsequent falls and health service use following fall-related paramedic care: a randomised controlled trial. Age Ageing. 2017;46(2):200–8.
- Sweeney R, Menezes S, Injury Matters: 2022. 2022 Western Australian falls report. Perth, Western Australia: Injury Matters.
- Centers for Disease Control and Prevention. Preventing falls: a guide to implementing effective community-based fall prevention programs. 2015. 2nd ed.
- Choi M, Hector M. Effectiveness of intervention programs in preventing falls: a systematic review of recent 10 years and meta-analysis. J Am Med Dir Assoc. 2012;13(188):e113–e188.
- Neyens JCL, Dijcks BPJ, Twisk J, Schols JMGA, van Haastregt JCM, van den Heuvel WJA, de Witte LP. A multifactorial intervention for the prevention of falls in psychogeriatric nursing home patients, a randomised controlled trial (RCT). Age Ageing. 2009;38(2):194–9. doi:10.1093/ageing/afn297.
- London Ambulance Service. Documents and guidelines. 2009 Dec [accessed 2024 Jan 01]. https://www.londonambulance.nhs.uk/health-professionals/hcp-information/documents-and-guidelines/.
- St John New Zealand Ambulance Service. Clinical procedures and guidelines 2019. 2019 Jun [accessed 2023 May 13]. https://www.stjohn.org.nz/globalassets/documents/health-practitioners/clinical-procedures-and-guidelines–-comprehensive-edition.pdf.
- Cantwell K, Burgess S, Morgans A, Smith K, Livingston M, Dietze P. Temporal trends in falls cases seen by EMS in Melbourne: the effect of residence on time of day and day of week patterns. Injury. 2016;47(1):266–71. doi:10.1016/j.injury.2015.10.073.
- Paul SS, Harvey L, Carroll T, Li Q, Boufous S, Priddis A, Tiedemann A, Clemson L, Lord SR, Muecke S, et al. Trends in fall-related ambulance use and hospitalisation among older adults in NSW, 2006-2013: a retrospective, population-based study. 2017 Oct 11. Report No: 2204-2091 Contract No.: 4.