Abstract
Context
Chinese medicine injections (CMIs) are widely used as adjuvant therapy for cervical cancer in China. However, the effectiveness of different types of CMIs remains uncertain.
Objective
To assess the effectiveness and safety of CMIs when used in conjunction with radiotherapy (RT) or concurrent chemoradiotherapy (CCRT), particularly in combination with cisplatin (DDP), docetaxel plus cisplatin (DP), and paclitaxel plus cisplatin (TP).
Materials and methods
Randomized controlled trials (RCTs) were searched in databases including CNKI, WanFang, VIP, SinoMed, PubMed, Cochrane Library, Embase, and Web of Science from inception to September 2023. We calculated the risk ratio with a 95% confidence interval and the surface under the cumulative ranking area curve (SUCRA) for the clinical efficacy rate (CER), the efficacy rate by Karnofsky Performance Status (KPS), and the rates of leukopenia reduction (LRR) and gastrointestinal reactions (GRR).
Results
Forty-seven RCTs were included, including nine CMI types: Aidi, Fufangkushen, Huangqi, Kangai (KA), Kanglaite (KLT), Renshenduotang, Shenqifuzheng (SQFZ), Shenmai (SM), and Yadanzi. KLT and KA were likely optimal choices with radiotherapy for CER and KPS, respectively. KA and KLT were optimal choices with RT + DDP for CER and GRR, respectively. KLT was the likely optimal choice with RT + DP for CER and KA for both KPS and GRR. SM and SQFZ were the likely optimal choices with RT + TP for CER and LRR, respectively.
Conclusions
The optimal recommendation depends on whether CMIs are used with radiotherapy or concurrent chemoradiotherapy. More high-quality RCTs are needed to confirm further and update the existing evidence.
Introduction
Globally, cervical cancer is the fourth most common female malignant tumor in both incidence and mortality, ranking only after breast cancer, colorectal cancer, and lung cancer, which is centrally caused by persistent human papillomavirus (HPV) infections, with HPV strains 16 and 18 causing the vast majority of cases (Sung et al. Citation2021). Due to the existence of a transparent socioeconomic gradient in cervical cancer, the incidence is three times higher in countries with a low Human Development Index (HDI) compared to countries with a very high HDI. At the same time, the mortality is six times higher in low HDI countries than in countries with very high HDI (Singh et al. Citation2023). As the most populous country, China is suffering from a high burden of cervical cancer; the trend in incidence of cervical cancer increased from 1990 to 2019, particularly in younger age, while the trend in mortality declined in older age (Shen et al. Citation2022).
Chronic infection by high-risk HPV oncogenic subtypes causes almost all cases of cervical cancer. Therefore, effective primary prevention of cervical cancer depends on HPV detection and vaccination (Johnson et al. Citation2019). Meanwhile, secondary prevention and treatment depend on the extent of the disease at diagnosis and locally available resources and may involve radical hysterectomy, chemoradiation, or a combination of both (Cohen et al. Citation2019). Radiotherapy (RT), especially brachytherapy, is the primary treatment in the management of cervical cancer for early-stage tumors with local risk factors. At the same time, concurrent chemoradiotherapy (CCRT) is the standard treatment for advanced local tumors (Chargari et al. Citation2022). Various combinations of cisplatin, paclitaxel, bevacizumab, carboplatin, topotecan, and gemcitabine are recommended as first-line therapies (Koh et al. Citation2015). Meanwhile, a recent meta-analysis reported that cisplatin-based CCRT, especially paclitaxel plus cisplatin (TP), could be the best choice for cervical cancer in efficacy and safety (Fu et al. Citation2017; Li Citation2022).
Traditional Chinese medicine (TCM), recognized as a complementary and alternative medical system, is among the oldest healthcare systems globally. Chinese medicine injections (CMIs), notably, representative anticancer CMIs within Chinese patent medicines, have found extensive use in the clinical management of cervical cancer in China over many years. However, the effectiveness of specific types of CMIs, particularly in combination with RT or CCRT for cervical cancer, remains uncertain. The current study conducted a network meta-analysis to comprehensively evaluate the efficacy and safety of CMIs as adjuvant treatments in conjunction with RT or cisplatin-based CCRT for managing cervical cancer. This evaluation was compared to conventional treatment alone to provide evidence and guidance for clinical medication strategies.
Materials and methods
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Page et al. Citation2021), and this study was registered with PROSPERO (CRD42022361708).
Search strategy
We searched the literature in four Chinese databases (CNKI, WanFang, VIP, and SinoMed), and four English databases (PubMed, Cochrane Library, Embase, and Web of Science), from inception to September 2023. The search strategy employed encompassed the terms "cervical cancer", "radiotherapy", and "chemoradiotherapy" along with their respective abbreviations and all synonymous variations tailored for each specific database.
Eligibility criteria
Inclusion criteria
Type of population: patients diagnosed with cervical cancer.
Type of intervention: combined with CMIs.
Type of comparison: RT or cisplatin-based CCRT, such as cisplatin (DDP), docetaxel plus cisplatin (DP), and TP.
Type of outcomes: efficacy evaluation indicators were the clinical efficacy rate (CER) and efficacy rate according to the Karnofsky performance status (KPS). Safety evaluation indicators were the leukopenia reduction rate (LRR) and gastrointestinal reaction rate (GRR). CER was evaluated using the Response Evaluation Criteria in Solid Tumors (RECIST) (Therasse et al. Citation2000). KPS was examined according to the Karnofsky performance scale score, in which an increase of ≥ 10 after treatment is considered an improvement, a decrease of ≥10 is regarded as a decrease, and stability is considered between the two (Yates et al. Citation1980). LRR and GRR were evaluated for incidence and severity using the Common Terminology Criteria for Adverse Events (CTCAE) (Trotti et al. Citation2003). These outcomes were calculated using the following formula: CER = number of complete and partial response patients/total number of patients × 100%; KPS = number of patients who responded to improvement by the KPS score/total number of patients × 100%; LRR = (number of patients with leukopenia reduction adverse events/total number of patients) × 100%; GRR = (number of patients with gastrointestinal adverse events/total number of patients) × 100%.
Type of study design: randomized controlled trials (RCTs).
Exclusion criteria
Duplicates.
Non-clinical trial study.
Non-randomized controlled study.
The control group or treatment group combined traditional Chinese medicine therapies such as footbath, acupuncture catgut embedding, acupoint application, and others.
Literature screening and data extraction
After removing duplicates of retrieved studies, the two screening phases were conducted by two independent reviewers (F Ma and Q Wang): (1) titles and abstracts were screened according to the eligible criteria; (2) full texts of initial studies were further screened for the final inclusion. The following information were extracted: study characteristics (authors, publication year, country), patient characteristics (age, tumor stage), interventions (drug, treatment duration), comparisons and outcomes. Any disagreements were solved by the third author (H Xie).
Assessment of methodological quality
The methodological quality assessment was conducted by two independent reviewers (D Zhang or ZH Wang) using the Cochrane Bias Risk Assessment Tool, which was composed of randomization, protocol concealment, allocation concealment, measurement blinding, completeness of outcome data, selective outcome reporting, and other biases (Higgins et al. Citation2011). To evaluate the risk of bias of studies, each item was rated as low risk, high risk, or unclear risk. Any disagreements were solved by the third author (H Xie).
Statistical analysis
The frequentist random-effect model with STATA 15.0 software was adopted to perform the network meta-analysis (Chaimani et al. Citation2013; Chaimani and Salanti Citation2015). The risk ratio (RR) with a 95% confidence interval (95% CI) was calculated for binary data. The surface under the cumulative ranking area curve (SUCRA) was calculated to rank multiple interventions. SUCRA values of 100% and 0% were assigned as the best and worst treatments for efficacy and safety, respectively. A sensitivity analysis was conducted to assess the reliability. Finally, a comparison-adjusted funnel plot was created to evaluate the publication bias and the effect of small studies (Wang and Sun Citation2020).
Results
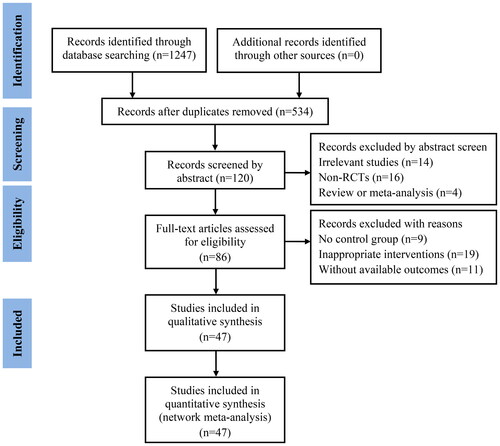
Selection of the included studies
According to the search strategy, 47 eligible studies (Cao and Wen Citation2005; Liu Citation2009; Hu and Lei Citation2011; Lu et al. Citation2011; Wang et al. Citation2011; Yin et al. Citation2011; Zhou et al. Citation2011; Chen and Liu Citation2012; Chen and Zhang Citation2012; Wen et al. Citation2012; Chen Citation2013; Wu et al. Citation2013; Chen et al. Citation2014; Deng and Cai Citation2014; Deng and Chen Citation2014; Huang et al. Citation2014; Li et al. Citation2014; Zhong et al. Citation2014; Li et al. Citation2015; Liu et al. Citation2015; Deng et al. Citation2015a, Citation2015b; Jiang et al. Citation2016; Li et al. Citation2016; Mu Citation2016; Qin et al. Citation2016; Xiong and Zhou Citation2016; Gao et al. Citation2017; Li Citation2017; Zhang Citation2017; Li et al. Citation2018; Li and Wu Citation2018; Ma et al. Citation2018; Shao Citation2018; Wang et al. Citation2018; Yan et al. Citation2018; Cao Citation2019; Tian et al. Citation2019; Zhang Citation2019; Dong et al. Citation2020; Li et al. Citation2020; Liu et al. Citation2020; Li and Xi Citation2020; Song et al. Citation2020; Wang Citation2021; Ge et al. Citation2022; Peng and Li Citation2022) were included, involving 4138 cases, 4 types of comparisons (RT, RT + DDP, RT + DP, RT + TP) and 9 types of CMIs, such as Aidi (AD), Fufangkushen (FFKS), Huangqi (HQ), Kangai (KA), Kanglaite (KLT), Renshenduotang (RSDT), Shenqifuzheng (SQFZ), Shenmai (SM), and Yadanzi (YDZ). The study selection is shown in .
Characteristics of the included studies
All 47 studies were single-center trials conducted in China and published from 2005 to 2022. Among these CMIs, AD was mentioned in 3 studies, FFKS in 15 studies, HQ in 2 studies, KA in 8 studies, KLT in 5 studies, RSDT in 1 study, SQFZ in 2 studies, SM in 2 studies, and YDZ in 9 studies. Among these comparisons and interventions, RT was mentioned in 17 studies while RT + AD in 1 study, RT + FFKS in 5 studies, RT + KA in 2 studies, RT + KLT in 1 study, RT + YDZ in 8 studies; RT + DDP in 8 studies while RT + DDP + AD in 2 studies, RT + DDP + KA in 2 studies, RT + DDP + KLT in 2 studies, RT + DDP + FFKS in 2 studies; RT + DP in 10 studies while RT + DP + KA in 3 studies, RT + DP + KLT in 2 studies, RT + DP + FFKS in 4 studies, and RT + DP + RSDT in 1 study. RT + TP was mentioned in 11 studies while RT + TP + FFKS in 4 studies, RT + TP + HQ in 2 studies, RT + TP + KA in 1 study, RT + TP + SM in 2 studies, RT + TP + SQFZ in 1 study, and RT + TP + YDZ in 1 study. The treatment duration for all studies ranged from 2 to 28 weeks ().
Table 1. The main characteristics of the included randomized controlled trials.
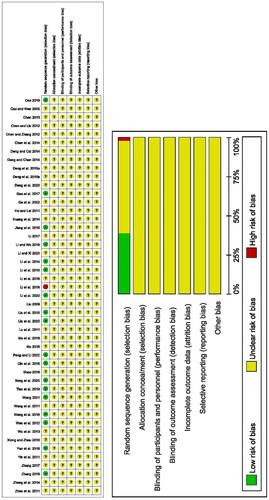
Quality assessment of the included studies
Among the 47 studies included, only 18 studies provided details about the randomization method. Of these, 17 studies were evaluated as low-risk, and 1 as high-risk. The remaining studies did not provide specific information on the details of the randomization. None of the studies mentioned protocol concealment, allocation concealment, measurement blinding, completeness of outcome data, selective outcome reporting, or other biases. As a result, all of these aspects were rated as unclear risk ()
Network meta-analysis
Clinical efficacy rate (CER)
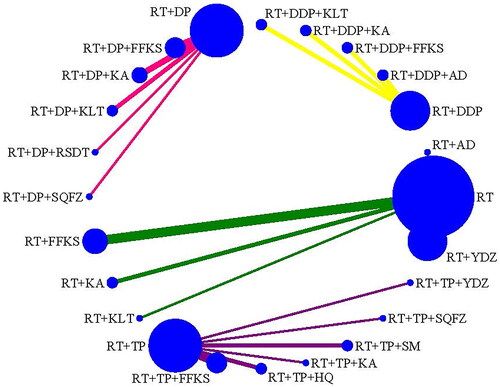
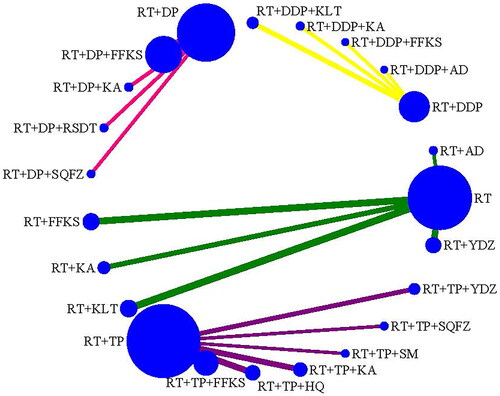
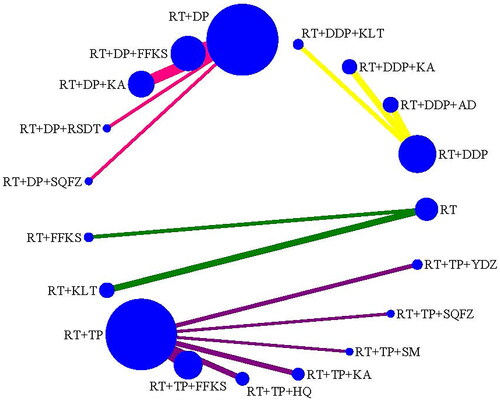
CER was reported in 43 studies (Cao and Wen Citation2005); Liu Citation2009; Hu and Lei Citation2011; Lu et al. Citation2011; Wang et al. Citation2011; Yin et al. Citation2011; Zhou et al. Citation2011; Chen and Liu Citation2012; Chen and Zhang Citation2012; Wen et al. Citation2012; Chen Citation2013; Wu et al. Citation2013; Chen et al. Citation2014; Deng and Cai Citation2014; Deng and Chen Citation2014; Huang et al. Citation2014; Li et al. Citation2014; Zhong et al. Citation2014; Li et al. Citation2015; Deng et al. Citation2015b; Jiang et al. Citation2016; Li et al. Citation2016; Mu Citation2016; Qin et al. Citation2016; Xiong and Zhou Citation2016; Gao et al. Citation2017; Li Citation2017; Zhang Citation2017; Li et al. Citation2018; Li and Wu Citation2018; Shao Citation2018; Wang et al. Citation2018; Yan et al. Citation2018; Cao Citation2019; Tian et al. Citation2019; Zhang Citation2019; Dong et al. Citation2020; Li et al. Citation2020; Liu et al. Citation2020; Song et al. Citation2020; Wang Citation2021; Ge et al. Citation2022; Peng and Li Citation2022), with 3847 cases, including 4 types of comparisons (RT, RT + DDP, RT + DP, RT + TP) and 5 types of CMIs combined with RT, 4 types of CMIs combined with RT + DDP, 4 types of CMIs combined with RT + DP, 6 types of CMIs combined with RT + TP ().
The pooled results indicated that RT + AD, RT + FFKS, RT + KA, and RT + KLT were associated with a significant increase in CER compared to RT alone. Furthermore, RT + DDP + KA and RT + DDP + KLT significantly increased the CER compared to RT + DDP. In the case of RT + DP, RT + DP + FFKS, RT + DP + KA, and RT + DP + KLT, the CER significantly increased compared to RT + DP. For RT + TP, both RT + TP + FFKS and RT + TP + SM significantly increased CER compared to RT + TP. However, RT + TP + HQ was associated with a significant decrease in CER compared to RT + TP + FFKS, and RT + TP + SM was found to substantially increase CER compared to RT + TP + HQ ().
Table 2. Network meta-analysis for the efficacy of CMIs combined with RT or CCRT for cervical cancer.
Based on the SUCRA values for CER, KLT was identified as the most probable to be the best combination with RT. For RT + DDP, KA emerged as the most likely to be the best combination. In the case of RT + DP, KLT was deemed the most probable to be the best combination. Last, for RT + TP, SM was identified as the most likely to be the best combination. The ranking of CMI interventions was as follows: RT + KLT (92.1%) > RT + KA (63.7%) > RT + AD (54.5%) > RT + FFKS (47.9%) > RT + YDZ (39.4%) > RT (2.4%); RT + DDP + KA (83.9%) > RT + DDP + KLT (72.2%) > RT + DDP + AD (47.5%) > RT + DDP + FFKS (38.2%) > RT + DDP (8.2%); RT + DP + KLT (95.7%) > RT + DP + KA (59.7%) > RT + DP + RSDT (47.9%) > RT + DP + FFKS (45.4%) > RT + DP (1.3%); and RT + TP + SM (80.7%) > RT + TP + KA (67.9%) > RT + TP + FFKS (64.1%) > RT + TP + SQFZ (53.7%) > RT + TP + YDZ (50.7%) > RT + TP + HQ (16.9%) > RT + TP (15.9%) ().
Table 4. Rank of SUCRA for the efficacy and safety of CMIs combined with RT or CCRT for cervical cancer.
Efficacy rate by Karnofsky Performance Status (KPS)
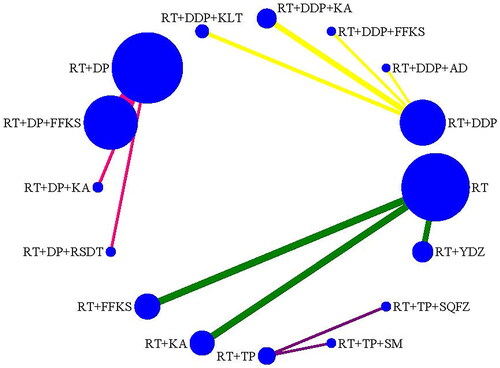
KPS was reported in 24 studies (Cao and Wen Citation2005; Liu Citation2009; Hu and Lei Citation2011; Lu et al. Citation2011; Wang et al. Citation2011; Yin et al. Citation2011; Zhou et al. Citation2011; Chen and Liu Citation2012; Chen and Zhang Citation2012; Wen et al. Citation2012; Chen Citation2013; Huang et al. Citation2014; Li et al. Citation2014; Zhong et al. Citation2014; Liu et al. Citation2015; Jiang et al. Citation2016; Mu Citation2016; Qin et al. Citation2016; Li et al. Citation2018; Yan et al. Citation2018; Tian et al. Citation2019; Liu et al. Citation2020; Li and Xi Citation2020; Wang Citation2021) with 1646 cases, including 4 types of comparisons (RT, RT + DDP, RT + DP, RT + TP) and 5 types of CMIs combination with RT, 4 types of CMIs combination with RT + DDP, 4 types of CMIs combination with RT + DP, and 6 types of CMIs combination with RT + TP ().
The pooled results indicated that RT + KA significantly improved KPS compared to RT alone. Additionally, RT + DP + FFKS and RT + DP + KA were associated with a significant increase in KPS compared to RT + DP. In contrast, RT + DP + RSDT decreased the KPS significantly compared to RT + DP + KA ().
According to the SUCRA values for KPS, KA was the most likely to be the best combination with RT. FFKS was the most likely to be the best combination with RT + DDP. KA was the most likely to be the best combination with RT + DP, and SM was the most likely to be the best combination with RT + TP. The ranking of CMI interventions was as follows: RT + KA (86.7%) > RT + FFKS (59.2%) > RT + AD (50.1%) > RT + YDZ (37.1%) > RT (17%); RT + DDP + FFKS (71.2%) > RT + DDP + KLT (54.8%) > RT + DDP + AD (51.8%) > RT + DDP + KA (50.8%) > RT + DDP (21.3%); RT + DP + KA (97.6%) > RT + DP + FFKS (66.6%) > RT + DP + RSDT (24.4%) > RT + DP (11.5%); RT + TP + SM (63.3%) > RT + TP + SQFZ (62.9%) > RT + TP (23.8%) ().
Rate of leukopenia reduction (LRR)
LRR was reported in 25 studies (Cao and Wen Citation2005 Hu and Lei Citation2011; Yin et al. Citation2011; Zhou et al. Citation2011; Chen and Liu Citation2012; Chen and Zhang Citation2012; Wen et al. Citation2012; Chen Citation2013; Chen et al. Citation2014; Deng and Cai Citation2014; Huang et al. Citation2014; Zhong et al. Citation2014; Deng et al. Citation2015a; Jiang et al. Citation2016; Mu Citation2016; Qin et al. Citation2016; Li Citation2017; Zhang Citation2017; Ma et al. Citation2018; Shao Citation2018; Yan et al. Citation2018; Cao Citation2019; Tian et al. Citation2019; Li et al. Citation2020; Wang Citation2021; Peng and Li Citation2022) with 2063 cases, including 4 types of comparisons (RT, RT + DDP, RT + DP, RT + TP) and 5 types of CMIs combination with RT, 4 types of CMIs combination with RT + DDP, 4 types of CMIs combination with RT + DP, and 6 types of CMIs combination with RT + TP ().
The pooled results indicate that combinations such as RT + TP + HQ, RT + TP + SM, and RT + TP + SQFZ significantly reduced LRR compared to RT + TP. Furthermore, RT + TP + SM and RT + TP + SQFZ substantially decreased LRR compared to RT + TP + FFKS. RT + TP + SQFZ significantly reduced LRR compared to RT + TP + KA ().
Table 3. Network meta-analysis for the safety of CMIs combined with RT or CCRT for cervical cancer.
According to the SUCRA values for LRR, YDZ was the most likely to be the best combination with RT. KLT was most likely to be the best combination with RT + DDP. KLT was the most likely to be the best combination with RT + DP, and SQFZ was the most likely to be the best combination with RT + TP. The ranking of CMIs interventions was as follows: RT + YDZ (94.8%) > RT + FFKS (71.3%) > RT + KLT (51.7%) > RT + KA (38.8%) > RT + AD (28.2%) > RT (15.2%); RT + DDP + KLT (58.1%) > RT + DDP + FFKS (53.9%) > RT + DDP + AD (49.5%) > RT + DDP + KA (48.7%) > RT + DDP (39.9%); RT + DP + KLT (78.5%) > RT + DP + RSDT (53.7%) > RT + DP + KA (53.6%) > RT + DP + FFKS (34.9%) > RT + DP (29.2%); RT + TP + SQFZ (82.1%) > RT + TP + SM (78.0%) > RT + TP + HQ (68.8%) > RT + TP + YDZ (63.9%) > RT + TP (24.5%) > RT + TP + KA (19.9%) > RT + TP + FFKS (12.9%) ().
Rate of gastrointestinal reactions (GRR)
GRR was reported in 25 studies (Yin et al. Citation2011; Zhou et al. Citation2011; Chen and Liu Citation2012; Chen and Zhang Citation2012; Wen et al. Citation2012; Chen Citation2013; Huang et al. Citation2014; Li et al. Citation2014; Zhong et al. Citation2014; Jiang et al. Citation2016; Mu Citation2016; Li Citation2017; Zhang Citation2017; Ma et al. Citation2018; Shao Citation2018; Wang et al. Citation2018; Cao Citation2019; Tian et al. Citation2019; Dong et al. Citation2020; Li et al. Citation2020; Liu et al. Citation2020; Song et al. Citation2020; Wang Citation2021; Ge et al. Citation2022; Peng and Li Citation2022) with 2171 cases, including 4 types of comparison (RT, RT + DDP, RT + DP, RT + TP) and 5 types of CMIs combination with RT, 4 types of CMIs combination with RT + DDP, 4 types of CMIs combination with RT + DP, and 6 types of CMIs combination with RT + TP ().
The pooled results indicate that using RT + DDP + AD, RT + DDP + KA, and RT + DDP + KLT significantly reduced the GRR compared to RT + DDP. Similarly, RT + DP + FFKS and RT + DP + KA demonstrated a significant decrease in GRR compared to RT + DP ().
According to the SUCRA values for GRR, KLT was the most likely to be the best combination with RT. KLT was the most likely to be the best combination with RT + DDP. RSDT was the most likely to be the best combination with RT + DP, and KA was the most likely to be the best combination with RT + TP. The ranking of CMI interventions was as follows: RT + KLT (72.1%) > RT (51.7%) > RT + FFKS (26.2%); RT + DDP + KLT (90.9%) > RT + DDP + AD (62.1%) > RT + DDP + KA (46.6%) > RT + DDP (0.4%); RT + DP + KA (88.0%) > RT + DP + RSDT (64.9%) > RT + DP + KLT (46.9%) > RT + DP + FFKS (45.9%) > RT + DP (4.3%); and RT + TP + KA (58.6%) > RT + TP + SQFZ (57.7%) > RT + TP + SM (55.8%) > RT + TP + YDZ (52.5%) > RT + TP + FFKS (49.6%) >RT + TP + HQ (41.9%) > RT + TP (33.9%) ().
Sensitivity analysis
A sensitivity analysis was performed to assess the impact of each study on the overall summary estimate, achieved by systematically omitting one study at a time. The findings indicate that excluding any single study did not significantly influence the outcomes (CER, KPS, LRR, GRR). This suggests that the results are statistically robust and reliable.
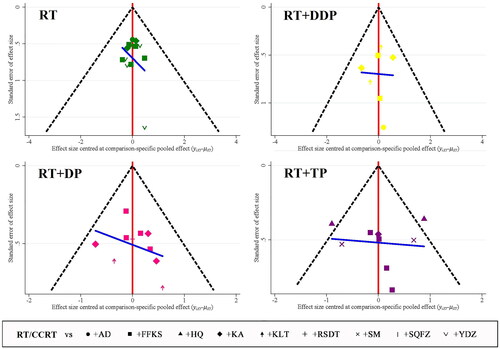
Publication bias
Comparison-adjusted funnel plots were generated for each outcome. Egger and Begg’s tests were conducted to assess the symmetry of the distributions. The results indicate some asymmetry in the CER funnel plots (Egger: p > 0.05, Begg’s: p > 0.05; Egger: p > 0.05, Begg’s: p > 0.05; Egger: p < 0.05, Begg’s: p < 0.05; Egger: p > 0.005, Begg’s: p > 0.05) as illustrated in .
Discussion
Cervical cancer poses a significant global public health challenge, with a particularly pronounced burden in many countries. In the management of cervical cancer, radiotherapy, especially brachytherapy, is the primary treatment for early-stage tumors with local risk factors. Additionally, cisplatin-based concurrent chemoradiotherapy is optimal for both efficacy and safety. TCM is crucial in China’s national work-related injury and maternity medical insurance, acting as a supplement or alternative to Western medicine. Chinese patent medicines play a vital supplementary role in cervical cancer treatment. A 2019 meta-analysis revealed that the combination of Kangai injection with cisplatin-based concurrent chemoradiotherapy exhibited higher efficacy (CER and KPS) and a lower incidence of side effects (LRR and GRR) compared to concurrent chemoradiotherapy alone (Cui et al. Citation2019).
Furthermore, a 2023 network meta-analysis demonstrated that Fufangkushen injection combined with paclitaxel plus cisplatin improved short-term efficacy and mitigated toxicity in cervical cancer treatment compared to paclitaxel plus cisplatin alone (Liu and Wang Citation2023). These published studies have strengthened the confidence of Chinese clinicians in using CMIs in conjunction with radiotherapy or cisplatin-based concurrent chemoradiotherapy for cervical cancer treatment. However, the optimal choice among CMIs combined with radiotherapy or cisplatin-based concurrent chemoradiotherapy for cervical cancer remains uncertain. Therefore, this network meta-analysis was undertaken to address this issue.
A total of 47 eligible studies comprising 4138 cases were included in this research, covering four types of comparison (RT, RT + DDP, RT + DP, RT + TP) and nine types of Chinese medicine injections (AD, FFKS, HQ, KA, KLT, RSDT, SQFZ, SM, YDZ). Based on the RR with a 95% CI and the SUCRA value, Kanglaite and Kangai are likely the optimal choices with radiotherapy for CER and KPS, respectively. Furthermore, Kangai and Kanglaite were likely optimal with radiotherapy and cisplatin for CER and GRR, respectively. Kanglaite was identified as the likely optimal choice with radiotherapy and docetaxel plus cisplatin for CER and Kangai for both KPS and GRR. Last, Shenmai and Shenqifuzheng were suggested as optimal choices with radiotherapy and paclitaxel plus cisplatin for CER and LRR, respectively. In summary, the optimal recommendation to combine Chinese medicine injections with radiotherapy or concurrent chemoradiotherapy depends on the specific conventional treatment used.
TCM, including Chinese medicine injections, exerts antitumor effects through two main aspects: health-strengthening (Fu-Zheng) and pathogen-eliminating (Qu-Xie). The key mechanism involves the regulation of the immune system in cancer patients (Wang et al. 2020; Citation2020). Kanglaite demonstrates inhibitory effects on various tumor cells, promoting tumor cell apoptosis by influencing related genes. For instance, it exhibits anti-triple-negative breast cancer effects by arresting the cell cycle and inhibiting cyclin-dependent kinase 1 (CDK1) dephosphorylation (Lu et al. Citation2008; Zhao et al. Citation2023). Kangai, on the other hand, exerts an antiproliferative function by inhibiting the interleukin (IL)-6/signal transducer and activator of transcription (STAT) 3 signaling pathway, subsequently inducing G1 phase arrest in gastric cancer cells (Zheng et al. Citation2022). Shenmai plays a role in remodeling the homeostasis of pro- and anti-angiogenic factors, promoting tumor vessel normalization, and enhancing drug delivery and antitumor effects. This insight into the pharmacological mechanisms of Shenmai in tumors is viewed from the perspective of vascular regulation (Cheng e al. Citation2021). When combined with chemotherapy, Shenqifuzheng exhibits better therapeutic efficacy than conventional chemotherapy alone, primarily through immunoregulation (Yang et al. Citation2017). Furthermore, animal research has indicated that Shenqifuzheng can alleviate fatigue symptoms in tumor-bearing mice by inhibiting pro-inflammatory cytokines produced by peripheral immune cells (Zhu et al. Citation2019).
However, when considering Chinese medicine injections as adjuvant treatment for cervical cancer, attention should be directed toward two critical aspects: multidrug resistance (MDR) chemotherapy and adverse drug reactions (ADRs) associated with CMIs. TCM is recognized for its crucial role in cancer treatment due to its low toxicity, high efficacy, safety, and potential to reverse MDR (Wei et al. Citation2022). In multidrug resistance, the existing literature suggests that Kanglaite can inhibit the expression of multidrug resistance-associated protein (MRP) 1 by suppressing the expression of PVT1 in gastric cancer (Zhang et al. Citation2017). Similarly, Shenqifuzheng has been reported to significantly enhance the efficacy of cisplatin in reducing tumor mass by regulating the expression of CD206 and CD86 (Yan et al. Citation2023). Regarding ADRs, an analysis of the spontaneous reporting system in Chinese Guangdong Province from 2003 to 2017 revealed that CMIs had a slightly lower percentage of serious ADRs and a notably higher percentage of unknown (new) ADRs compared to non-CMI injections. High-risk ADRs for CMIs included anaphylactic shock and anaphylactoid reactions (Li et al. Citation2019). Another analysis of Chinese Hubei province from 2014 to 2019 indicated that the age groups of children (0-10 years) and adult patients (41-80 years) had the highest rates of reporting ADRs for CMIs. Most ADRs occurred within one week, predominantly on the same day after receiving CMIs. Major concerns included anaphylactic shock, dyspnea, and anaphylactoid reactions, which were identified as the leading causes of death (Huang et al. Citation2021).
This research has several limitations. First, variations in characteristics such as age, disease stage, comparisons, interventions, and treatment courses may contribute to heterogeneity. Second, the absence of reported randomization methods in some literature and a lack of information on other biases could further contribute to increased heterogeneity. Furthermore, the exclusive focus on the literature from China may limit the generalizability and overall quality of the evidence. Last, the small sample size in some RCTs may lead to small study effects, affecting the robustness of the findings.
Conclusions
Our network meta-analysis indicates that the use of Chinese medicine injections as an adjunctive treatment in combination with radiotherapy or concurrent chemoradiotherapy is associated with higher levels of efficacy and/or safety for cervical cancer compared to radiotherapy or concurrent chemoradiotherapy alone. The optimal recommendation for specific CMIs combined with radiotherapy or concurrent chemoradiotherapy varies depending on the conventional treatment scheme, with the guiding principle of maximizing patient benefits. However, it is crucial to acknowledge the poor quality of all included studies. To establish more robust conclusions, additional large-sample, multicenter, double-blind, and high-quality trials are needed to further confirm and update the existing evidence.
Authors’ contributions
Sun SG and Song HY designed the study. Ma F, Wang Q, Zhang D, Wang ZH, and Xie H conducted literature searches, data extraction, and methodological quality evaluation and wrote the manuscript. Sun SG performed the statistical analysis and created the tables and pictures. Liu XH and Zhang HX helped to revise the manuscript. All authors approved the final version of the manuscript.
Acknowledgements
The authors thank the Home for Researchers editorial team (www.home-for-researchers.com) for a language editing service.
Disclosure statement
The authors report there are no competing interests to declare.
Data availability statement
All data generated or analyzed during this study are included in this published article, further inquiries can be made with the corresponding author(s).
Additional information
Funding
References
- Cao H, Wen XR. 2005. Treatment of malignant tumor by Kangai injection and radiotherapy. Zhejiang J Integr Tradit Chin West Med. 15:736–738. Chinese.
- Cao JF. 2019. Clinical observation on the treatment of cervical cancer with compound sophora injection combined with radiochemotherapy. China’s Naturopath. 27:64–65. Chinese.
- Chaimani A, Higgins JPT, Mavridis D, Spyridonos P, Salanti G. 2013. Graphical tools for network meta-analysis in STATA. PLOS One. 8(10):e76654. doi: 10.1371/journal.pone.0076654.
- Chaimani A, Salanti G. 2015. Visualizing assumptions and results in network meta-analysis: the network graphs package. Stata J. 15(4):905–950. doi: 10.1177/1536867X1501500402.
- Chargari C, Peignaux K, Escande A, Renard S, Lafond C, Petit A, Lam Cham Kee D, Durdux C, Haie-Méder C. 2022. Radiotherapy of cervical cancer. Cancer Radiother. 26(1–2):298–308. doi: 10.1016/j.canrad.2021.11.009.
- Chen P, Cao FJ, Li F, Deng SH. 2014. Bruceolic oil emulsion enhances the effect of radiotherapy in patients with cervical carcinoma. J Hubei Univ Med. 31:7–10. Chinese.
- Chen YJ. 2013. Clinical observation on the combination of Fufangkushen injection and radiochemotherapy in the treatment of advanced cervical cancer. Guid J Trad Chin Med Pharm. 19:51–53. Chinese.
- Chen YJ, Liu GS. 2012. Clinical observation on Kangai injection combined with radiochemotherapy in the treatment of advanced cervical cancer. Guid J Trad Chin Med Pharm. 18:33–35. Chinese.
- Chen YJ, Zhang SS. 2012. Clinical observation on the treatment of cervical cancer with Renshenduotang injection combined with synchronous radiochemotherapy. Guid J Trad Chin Med Pharm. 18:35–36. Chinese.
- Cheng L, Liu W, Zhong C, Ni P, Ni S, Wang Q, Zhang Q, Zhang J, Liu J, Xu M, et al. 2021. Remodeling the homeostasis of pro- and anti-angiogenic factors by Shenmai injection to normalize tumor vasculature for enhanced cancer chemotherapy. J Ethnopharmacol. 270:113770. doi: 10.1016/j.jep.2020.113770.
- Cohen PA, Jhingran A, Oaknin A, Denny L. 2019. Cervical cancer. Lancet. 393(10167):169–182. doi: 10.1016/S0140-6736(18)32470-X.
- Cui M, Chi ZH, Yu S. 2019. A meta-analysis of clinical efficacy of Kangai injection with radiotherapy and chemotherapy for advanced cervical cancer. J Guiyang Chin Med. 41:84–89. Chinese.
- Deng SH, Cai XJ. 2014. Clinical observation of bruceae oil emulsion on enhancing the sensitivity of radiotherapy combined with 192Ir afterloading intracavitary brachytherapy in the treatment for carcinoma of uterine cervix. Modern J Integr Tradit Chin West Med. 23:1503–1505. Chinese.
- Deng SH, Chen P. 2014. Clinical observation of bruceae oil emulsion combined with radiotherapy and afterloading intracavitary brachytherapy in patients with cervical cancer. J Mod Oncol. 22:1928–1930. Chinese.
- Deng SH, Duan X, Chen P. 2015a. Clinical observation on enhancing radiotherapy effect of bruceae oil emulsion in patients with cervical cancer. Lishizhen Med Mat Med Res. 26:1940–1942. Chinese.
- Deng SH, Duan X, Chen P. 2015b. Observation of the effect of compound Sophora flavescens Ait injection combined with intensity modulated radiation therapy and intracavitary brachytherapy on cervical carcinoma. Modern J Integr Tradit Chin West Med. 24:2185–2187. Chinese.
- Dong Y, Zhang CL, Xu N, Qiu CY. 2020. Study on the effect of radiochemotherapy combined with compound Sophora injection in the treatment of cervical cancer. Pract Clin J Integr Tradit Chin West Med. 20:93–95. Chinese.
- Fu ZZ, Li K, Peng Y, Zheng Y, Cao LY, Zhang YJ, Sun YM. 2017. Efficacy and toxicity of different concurrent chemoradiotherapy regimens in the treatment of advanced cervical cancer: a network meta-analysis. Medicine . 96(2):e5853. doi: 10.1097/MD.0000000000005853.
- Gao S, Wang HX, Yue CS, Wang P, Yu C. 2017. Efficacy of Shenmai injection in radiotherapy and chemotherapy of cervical cancer. Pract J Cancer. 32:805–807 + 813. Chinese.
- Ge YL, Zhu YP, Jiang J, Zhuang YL. 2022. Effects of concurrent chemoradiotherapy combined with Aidi injection adjuvant therapy on levels of MMP-9 and TIMP-1 and inflammatory factors in patients with cervical cancer. Chin Modern Doctor. 60:9–12 + 16. Chinese.
- Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JAC, . 2011. The cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 343(2):d5928–d5928. doi: 10.1136/bmj.d5928.
- Hu YX, Lei X. 2011. Observation on the therapeutic effect of Aidi injection combined with radiotherapy in the treatment of advanced cervical cancer. Modern J Integr Tradit Chin West Med. 20:4671–4672. Chinese.
- Huang J, Zhang CY, Ding JQ, Wu HX, Yu Y, Liao ZR. 2014. Analysis of the therapeutic effect of Shenqifuzheng injection combined with radiotherapy and chemotherapy in the treatment of advanced cervical cancer. J Gannan Med Univ. 34:885–887. Chinese.
- Huang R, Cai Y, Yang L, Shangguan X, Ghose B, Tang S. 2021. Safety of traditional Chinese medicine injection based on spontaneous reporting system from 2014 to 2019 in Hubei Province, China. Sci Rep. 11(1):8875. doi: 10.1038/s41598-021-88339-9.
- Jiang XF, Lin S, Lu HC, Zhu MH, Wang YP, Sun HY. 2016. Analysis of effects of radiochemotherapy combined with compound sophora injection on cellular immunity in patients with cervical cancer. Chin Hosp Pharm J. 36:119–121. Chinese.
- Johnson CA, James D, Marzan A, Armaos M. 2019. Cervical cancer: an overview of pathophysiology and management. Semin Oncol Nurs. 35(2):166–174. doi: 10.1016/j.soncn.2019.02.003.
- Koh W-J, Greer BE, Abu-Rustum NR, Apte SM, Campos SM, Cho KR, Chu C, Cohn D, Crispens MA, Dorigo O, et al. 2015. Cervical cancer, version 2. 2015. J Natl Compr Canc Netw. 13(4):395–404; quiz 404.,. doi: 10.6004/jnccn.2015.0055.
- Li D, Wen YF, Liu YA. 2015. Kanglaite injection combined radiotherapy and chemotherapy in the treatment of advanced cervical cancer. J Changchun Univ Chin Med. 31:151–153. Chinese.
- Li GL, Li YH, Zhang QZ, Xie JL. 2018. The clinical study on 125I particle implantation combined with java brucea fruit oil artery perfusion in the treatment of recurrent cervical cancer. Guangming J Chin Med. 33:2415–2418. Chinese.
- Li H, Deng J, Deng L, Ren X, Xia J. 2019. Safety profile of traditional Chinese herbal injection: an analysis of a spontaneous reporting system in China. Pharmacoepidemiol Drug Saf. 28(7):1002–1013. doi: 10.1002/pds.4805.
- Li ML, Wu XH. 2018. Clinical effect of Kanglaite injection combined with radiotherapy and chemotherapy for advanced cervical cancer. Drug Evaluat. 15:33–35. Chinese.
- Li MY, Zhu TF, Zhang CN. 2016. Clinical effect of Astragalus polysaccharides on protecting marrow suppression of cervical carcinoma after chemotherapy. Guangzhou Med J. 47:36–38. Chinese.
- Li Q, Xi Y. 2020. Effect of Brucea javanica oil emulsion injection on immune function and quality of life in elderly patients with cervical cancer undergoing postoperative radiotherapy. Modern J Integr Tradit Chin West Med. 29:2603–2606. Chinese.
- Li XY, Xie XM, Zhou C, Liu L. 2014. Clinical observation on treating terminal cervical cancer by radiotherapy with Kang’ai injection plus cisplatin. Clin J Chin Med. 6:9–11. Chinese.
- Li Y. 2017. Clinical efficacy of compound sophora flavescens injection in reducing the toxic side effects of concurrent radiotherapy and chemotherapy for cervical cancer. J North Pharm. 14:15. Chinese.
- Li YC, Shi ZY, Ren DM, Deng XY. 2020. Effects of astragalin on the immune function and adverse reactions in patients with cervical cancer undergoing radiotherapy and chemotherapy. J Xinxiang Med Univ. 37:580–583 + 587. Chinese.
- Li YF. 2022. The application of different drugs in the sensitization of radicalradiotherapy for advanced cervical cancer: a network meta-analysis [Thesis]. Nanchang Univ.
- Liu FQ, Li D, Liu F. 2015. Effect of Brucea javanica oil emulsion injection on cellular immune function in elderly patients with cervical cancer undergoing postoperative radiotherapy. Chin J Gerontol. 35:2429–2431. Chinese.
- Liu T, Wang WP. 2023. Network meta-analysis of Fufangkushen injection combined with TP chemotherapy in lung cancer, ovarian cancer and cervical cancer. J Liaoning Univ Trad Chin Med. 25:144–152. Chinese.
- Liu W, Yang H, Peng HX, Xie XY, Zhang TT. 2020. Effect of Fufangkushen injection combined with chemotherapy and intensity modulated radiation therapy in treatment of advanced cervical cancer. J Xinxiang Med Univ. 37:1156–1160. Chinese.
- Liu XG. 2009. Clinical analysis of the effect of Kangai injection on the quality of life of postoperative cervical cancer patients. Contemp Med. 15:130–131. Chinese.
- Lu Y, Li C-S, Dong Q. 2008. Chinese herb related molecules of cancer-cell-apoptosis: a minireview of progress between Kanglaite injection and related genes. J Exp Clin Cancer Res. 27(1):31. doi: 10.1186/1756-9966-27-31.
- Lu Z, Qi L, Li GX, Ma CG, Liu J, Liu K. 2011. Clinical efficiency of compound Kushen injection combined with radiotherapy in the treatment of patients with cervical cancer. Chin Hosp Pharm J. 31:1114–1117. Chinese.
- Ma YY, Sun YX, Liu H. 2018. Effect of Shenqifuzheng injection on immune function, quality of life, and toxic side effects in postoperative radiochemotherapy patients with cervical cancer. Modern J Integr Tradit Chin West Med. 27:3239–3241. Chinese.
- Mu Y. 2016. Effect of Fufangkushen injection combined with radiochemotherapy on immune function in patients with advanced cervical cancer. J Med Forum. 37:120–121. Chinese.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, et al. 2021. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 372:n71. doi: 10.1136/bmj.n71.
- Peng FH, Li L. 2022. Analysis of the adverse effects of Brucea javanica oil injection in the treatment of cervical cancer. Clin Med J. 20:26–31. Chinese.
- Qin XL, Jia YL, Bao YN. 2016. The clinical effect of Fufangkushen injection combined with chemoradiation on advanced cervical cancer. J Mod Oncol. 24:1959–1961. Chinese.
- Shao Y. 2018. The efficacy of radiotherapy and chemotherapy combined with compound Sophora flavescens injection in the treatment of cervical cancer patients and impact on cellular immune function index levels. Med J Chin People’s Health. 30:39–41. Chinese.
- Shen X, Cheng Y, Ren F, Shi Z. 2022. The burden of cervical cancer in China. Front Oncol. 12:979809. doi: 10.3389/fonc.2022.979809.
- Singh D, Vignat J, Lorenzoni V, Eslahi M, Ginsburg O, Lauby-Secretan B, Arbyn M, Basu P, Bray F, Vaccarella S. 2023. Global estimates of incidence and mortality of cervical cancer in 2020: a baseline analysis of the WHO global cervical cancer elimination initiative. Lancet Glob Health. 11(2):e197–e206. doi: 10.1016/S2214-109X(22)00501-0.
- Song HM, Zhang Y, Yang D. 2020. Effect on kang’ai injection combined with concurrent radiotherapy and chemotherapy in treatment of advanced cervical cancer. Chin Archi Tradit Chin Med. 38:122–125. Chinese.
- Sung H, Ferlay J, Siegel R, Laversanne M, Soerjomataram I, Jemal A, Bray F. 2021. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 71(3):209–249. doi: 10.3322/caac.21660.
- Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, et al. 2000. New guidelines to evaluate the response to treatment in solid tumors. J Natl Cancer Inst. 92(3):205–216. doi: 10.1093/jnci/92.3.205.
- Tian J, Wang L, Luo XH. 2019. Synergistic effect of kanglaite injection on radiotherapy for patients with cervical cancer. Pract J Cancer. 34:1132–1135. Chinese.
- Trotti A, Colevas AD, Setser A, Rusch V, Jaques D, Budach V, Langer C, Murphy B, Cumberlin R, Coleman CN, et al. 2003. CTCAE v3.0: development of a comprehensive grading system for the adverse effects of cancer treatment. Semin Radiat Oncol. 13(3):176–181. doi: 10.1016/S1053-4296(03)00031-6.
- Wang J, Wang YL, Tan HW, Mi Y, Liu D. 2018. Application of Kang’ai injection in concurrent radiochemotherapy of cervical cancer postoperation and serum IGF-2, SCC and IFN levels. Prog Modern BioMed. 18:3510–3513. Chinese.
- Wang Q, Sun SG. 2020. Optimization ratio between Coptis chinensis and Cinnamo of Jiaotai pill plus benzodiazepines for insomnia in China: a network meta-analysis Chin. J Integr Tradit West Med. 40:560–566. Chinese.
- Wang S. 2021. Effect of Kanglaite injection combined with chemotherapy on serum tumor markers, t-lymphocyte subsets, inflammatory factors, and quality of life in elderly cervical cancer patients. Chin J Gerontol. 41:2962–2965.
- Wang S, Long S, Deng Z, Wu W. 2020. Positive role of Chinese herbal medicine in cancer immune regulation. Am J Chin Med. 48(7):1577–1592. doi: 10.1142/S0192415X20500780.
- Wang Y, Zhang Q, Chen Y, Liang C-L, Liu H, Qiu F, Dai Z. 2020. Antitumor effects of immunity-enhancing traditional Chinese medicine. Biomed Pharmacother. 121:109570. doi: 10.1016/j.biopha.2019.109570.
- Wang YB, Lai BS, Luo HH. 2011. Observation on the therapeutic effect of compound Sophora flavescens injection combined with three-dimensional conformal radiotherapy in the treatment of recurrent cervical cancer. Med Inf. 24:4901–4902. Chinese.
- Wei J, Liu Z, He J, Liu Q, Lu Y, He S, Yuan B, Zhang J, Ding Y. 2022. Traditional Chinese medicine reverses cancer multidrug resistance and its mechanism. Clin Transl Oncol. 24(3):471–482. doi: 10.1007/s12094-021-02716-4.
- Wen CH, Feng XQ, Luo RC. 2012. Clinical observation of Shenmai injection combined with TP regimen concurrent radiotherapy in the treatment of moderate and advanced cervical cancer. Chin Pharm. 23:702–704. Chinese.
- Wu HH, Liang H, Li Y. 2013. Treatment of early cervical cancer by intensity modulated radiation therapy combined with Brucea javanica oil emulsion injection. Hebei J Trad Chin Med. 35:236–238. Chinese.
- Xiong G, Zhou J. 2016. Clinical observation of composite radix Sophora flavescentis injection on alleviating toxic reaction in concurrent chemoradiotherapy for cervical cancer. J Mod Oncol. 24:3787–3790. Chinese.
- Yan B, Shi R, Lu YY, Fang DD, Ye MN, Zhou QM. 2023. Shenqi Fuzheng injection reverses M2 macrophage-mediated cisplatin resistance through the PI3K pathway in breast cancer. PLOS One. 18(1):e0279752. doi: 10.1371/journal.pone.0279752.
- Yan MJ, Chen BG, Zhao P. 2018. Effects of compound matrine injection on complications prevention and quality of life in patients with cervical cancer. Modern Hosp. 18:539–542. Chinese.
- Yang Y, Ting W, Xiao L, Shufei F, Wangxiao T, Xiaoying W, Xiumei G, Boli Z. 2017. Immunoregulation of Shenqi Fuzheng injection combined with chemotherapy in cancer patients: a systematic review and meta-analysis. Evid Based Complement Alternat Med. 2017:5121538. doi: 10.1155/2017/5121538.
- Yates JW, Chalmer B, McKegney FP. 1980. Evaluation of patients with advanced cancer using the Karnofsky performance status. Cancer. 45(8):2220–2224. doi: 10.1002/1097-0142(19800415)45:8<2220::AID-CNCR2820450835>3.0.CO;2-Q.
- Yin GL, Wu JJ, Zhu Y, Cai M, Wang WW. 2011. Clinical observation of compound Sophora flavescens injection in the prevention of acute radiation proctitis. Chin Pharm. 22:1090–1094. Chinese.
- Zhang J. 2019. Clinical efficacy and safety analysis of Kanglaite injection combined with radiotherapy and chemotherapy in the treatment of advanced cervical cancer. World Latest Med Inf. 19:183. Chinese.
- Zhang JJ. 2017. Effect of Kangai Injection on reducing the toxic and side effects of synchronous radiochemotherapy in middle and late stage cervical cancer. J Pract Trad Chin Med. 33:437–438. Chinese.
- Zhang XW, Liu L, Zhang XZ, Bo P. 2017. Kanglaite inhibits the expression of drug resistance genes through suppressing PVT1 in cisplatin-resistant gastric cancer cells. Exp Ther Med. 14(2):1789–1794. doi: 10.3892/etm.2017.4650.
- Zhao M, Fu L, Xu P, Wang T, Li P. 2023. Network pharmacology and experimental validation to explore the effect and mechanism of Kanglaite injection against triple-negative breast cancer. Drug Des Devel Ther. 17:901–917. doi: 10.2147/DDDT.S397969.
- Zheng CL, Hou KZ, Wang AQ, Fang WX, Yu ST, Liang JE, Qi HY, Qu XJ, Liu YP, Che XF. 2022. Kangai injection inhibits gastric cancer cells proliferation through IL-6/STAT3 pathway. Chin J Integr Med. 28(6):524–530. doi: 10.1007/s11655-020-3265-6.
- Zhong JP, Huang J, Ding JQ, Wu HX, Yu Y, Shen CM. 2014. Clinical analysis of Kangai injection combined with concurrent chemoradiotherapy in the treatment of advanced cervical cancer. Jiangxi Med J. 49:64–66. Chinese.
- Zhou YQ, Ma XJ, Tan BX, Ren T, Hu J. 2011. Clinical observation on Aidi injection combined with concurrent radiochemotherapy for advanced cervical cancer. Evaluat Analy Drug Use Hosp Chin. 11:363–365. Chinese.
- Zhu G, Zhang B, Jiang F, Zhao L, Liu F. 2019. ShenQi FuZheng injection ameliorates fatigue-like behavior in mouse models of cancer-related fatigue. Biomed Pharmacother. 111:1376–1382. doi: 10.1016/j.biopha.2019.01.042.