ABSTRACT
In 2018, the Food and Drug Administration expanded the age of eligibility for the human papillomavirus (HPV) vaccine to 27 to 45 years. However, it is unclear if there are racial/ethnic disparities in HPV vaccine uptake for this age-group following this expanded recommendation. We aimed to identify any disparities in HPV vaccine in 27 to 45 year-olds based on sociodemographic factors. We analyzed nationally representative, cross-sectional data from the 2019 National Health Interview Survey (n = 9440). Logistic regression models estimated the odds of vaccine uptake (receipt of ≥1 vaccine dose) based on sociodemographic factors. Participants were mostly Non-Hispanic Whites (60.7%) and females (50.9%). In adjusted models, females had over three times greater odds of vaccine uptake compared to males (aOR = 3.58; 95% CI 3.03, 4.23). Also, compared to Non-Hispanic Whites, Non-Hispanic Blacks were 36% more likely (aOR = 1.36; 95% CI 1.09, 1.70), and Hispanics were 27% less likely (aOR = 0.73; 95% CI 0.58, 0.92) to receive the vaccine. Additionally, individuals without a usual place of care had lower odds of vaccine uptake (aOR = 0.72; 95% CI 0.57, 0.93), as were those with lower educational levels (aORhigh school = 0.62; 95% CI 0.50, 0.78; aORsome college = 0.83; 95% CI 0.70, 0.98). There are disparities in HPV vaccine uptake among 27 to 45 year-olds, and adult Hispanics have lower odds of receiving the vaccine. Given the vaccine’s importance in cancer prevention, it is critical that these disparities are addressed and mitigated.
Introduction
Human Papillomavirus (HPV) is the leading sexually transmitted infection in the United States,Citation1 and 85% of sexually active individuals will be infected at some point in their lifetime.Citation2 There are over 100 subtypes of HPV, and at least 40 of these can spread through direct contact via vaginal, anal, or oral sex and cause infection.Citation3 Nine out 10 of these infections clear within 2 years, but lingering HPV infections can lead to precancers, anogenital cancers, oropharyngeal cancers, and genital warts.Citation4 At least 44,000 new cases of HPV-associated cancers are diagnosed in the United States each year.Citation5 Furthermore, rates of HPV-associated oropharyngeal cancers have been increasing for the past 40 years,Citation6–8 and currently there are no screening tests for early detection.Citation9,Citation10 Hence, primary prevention through vaccination is critical.Citation10,Citation11
The nonavalent vaccine was initially approved for individuals aged 9–26 years.Citation12 However, in 2018, the Food and Drug Administration (FDA) expanded the age range for eligibility to individuals 27–45 years,Citation13 and the Advisory Committee on Immunization Practices (ACIP) followed in 2019 by recommending the vaccine for this age group based on shared clinical decision-making with a provider.Citation14 Although it is likely that most individuals in this age group have been exposed to some HPV subtypes, many may remain protected against some HPV subtypes covered by the nonavalent vaccine, thereby mitigating risk for developing some HPV-associated malignancies.Citation15,Citation16
As the recommendation to expand the age of eligibility of HPV vaccine to 45 years is relatively recent, there is little data on vaccination among individuals within this age group, and whether these individuals received their vaccination as a result of this latest expanded age of eligibility.Citation17 While new studies have emerged describing HPV vaccine uptake in this age group, is unclear whether, or to what degree disparities are associated with HPV vaccine uptake based on race/ethnicity and other sociodemographic factors. This is important as there are disparities observed in HPV vaccination awareness and uptake among adolescents and young adults.Citation18–20 Very recent evidence indicates that knowledge of HPV, HPV vaccines, and HPV-associated malignancies is significantly lower among Black individuals and other racial minorities.Citation21,Citation22 In addition to disparity in knowledge and awareness, evidence also suggests that rate of HPV vaccine initiation is higher among white adolescents.Citation23,Citation24 However, it is unclear whether the pattern of uptake is similar among adults. Based on already existing disparities in HPV vaccine uptake in general, as well as the shared decision-making model of this expanded recommendation,Citation16 we hypothesized that there are significant disparities in HPV vaccine uptake among racial/ethnic minorities compared to Non-Hispanic White individuals aged 27–45 years, and that racial/ethnic minorities would be disproportionately impacted. We also hypothesized that due to the shared-decision-making model of the expanded age of eligibility, individuals without a regular provider would be less likely to receive the HPV vaccine. To test our hypotheses, we described disparities in HPV vaccine uptake in US adults aged 27–45 years, based on race/ethnicity and other sociodemographic factors.
Methods
National health interview survey data
We analyzed data from the 2019 National Health Interview Survey (NHIS), which was collected starting in 2018 and ending in 2019. This is a cross-sectional survey administered every year by the National Center for Health Statistics (NCHS) to a nationally representative sample of the United States non-institutionalized population.Citation25 Our outcome variable, HPV vaccine uptake, was based on a single questionnaire item: “HPV is the Human Papillomavirus. Have you ever received an HPV shot or vaccine?” Response options were dichotomized to “yes or no.” The independent variables included the respondents’ age (continuous variable), gender (male, female), race and ethnicity (Non-Hispanic White, Non-Hispanic Black, Hispanic, Non-Hispanic Other), marital status (married/partnered, not married), highest level of education (college graduate, some college, high school graduate, less than high school), annual income (<$50K, $50 to < $75K, $75 to < $100K, ≥$100K), insurance status (yes, no), having a usual place for healthcare (yes, no), general health (excellent, very good, good, poor/fair), and geographic region of residence (Northeast, Midwest, West, South). These variables were self-reported.
Sample characteristics and statistical analysis
Our analysis included respondents 27–45 years of age who completed the 2019 NHIS. Gender, marital status, highest level of education, annual income, insurance status, having a usual place for healthcare, general health, smoking behavior, geographic region of residence, and HPV vaccine uptake of the sample were stratified by race and ethnicity using the SURVEYFREQ Procedure in SAS. The Rao-Scott chi-quare test was used to determine significance at α = 0.01. Note that 718 respondents did not answer the question linked to the outcome of interest (“Have you ever received an HPV shot or vaccine?”) and were therefore excluded from the logistic regression analysis. We built crude and adjusted models, and using multivariable logistic regression, we estimated associations between sociodemographic factors and HPV vaccine uptake, obtaining odds ratios at a 95% confidence interval to determine statistical significance.
Results
Sample characteristics
Characteristics of study participants are provided in . The overall sample included 9,440 participants 27–45 years. Of these, about half were female (50.9%), two-thirds married/partnered (68.9%), and one-third had a college degree or more (35.9%), and an annual income of less than $50K (33.5%). Only 15.5% of the study sample had initiated HPV vaccine, highest among Non-Hispanic Black adults (19.4%) and lowest among Hispanics (11.9%) ().
Figure 1. Bar graph showing HPV vaccine status among US adults 27–45 year old, with ≥ 1 dose ever received, by race and ethnicity (p < .05).
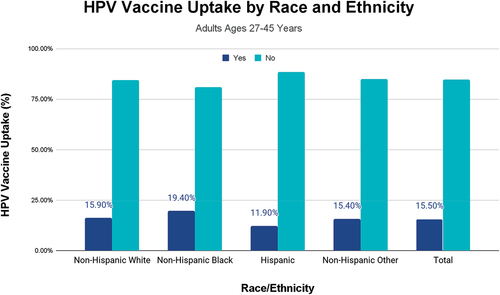
Table 1. Characteristics of study sample.
Estimating the odds of HPV vaccine uptake among adults aged 27–45 years
To understand factors associated with these ethnic/racial disparities in HPV vaccine uptake, we performed individual logistic regression for each independent variable (). In crude analysis, females had over three greater odds of being vaccinated than males (cOR = 3.47; 95% CI 2.97, 4.06). In the fully adjusted model, this strong association between gender and HPV vaccine uptake persisted, with females significantly more likely to receive the vaccine (aOR = 3.58; 95% CI 3.03, 4.23). In both crude and adjusted models, compared to non-Hispanic White adults, non-Hispanic Black adults had greater odds of vaccine uptake (cOR = 1.27; 95% CI 1.03, 1.56; aOR = 1.36; 95% CI 1.09, 1.70), while Hispanic adults had significantly lesser odds of receiving the vaccine (cOR = 0.71; 95% CI 0.58, 0.87; aOR = 0.73; 95% CI 0.58, 0.92). There was also an association between having a usual place of care and receipt of the vaccine, and individuals without a regular place for healthcare were less likely to have been vaccinated against HPV (cOR = 0.67; 95% CI 0.54, 0.82; aOR = 0.72; 95% CI 0.57, 0.92). Odds of receiving the HPV vaccine may be significantly higher in the West compared to the South (cOR = 1.31; 95% CI 1.10, 1.56; aOR = 1.49; 95% CI 1.24, 1.80). In the final adjusted models, there were no associations between HPV vaccination and income, insurance status, and general health. However, for each increasing year of age between 27 and 45 years, individuals had significantly decreased odds of receiving the HPV vaccine (cOR = 0.87; 95% CI 0.85, 0.88; aOR = 0.86; 95% CI 0.84, 0.87). There were also decreased odds of HPV vaccination among less educated individuals compared to individuals who graduated college or more ().
Table 2. Factors associated with uptake of HPV vaccine among 27–45 year olds based on race and ethnicity, and other sociodemographic factors.
Discussion
The primary purpose of this study was to describe vaccination status among US adults 27–45 years of age, based on race/ethnicity, and to identify additional sociodemographic factors associated with HPV vaccination in this age group. To the best of our knowledge, this is the first US-based study to assess racial/ethnic disparities in HPV vaccine uptake among adults 27–45 years of age following the FDA approval to administer the vaccine for this age group in 2018. Understanding racial and ethnic disparities in HPV vaccine uptake has public health implications since vaccination is paramount to primary prevention of HPV-associated cancers.Citation26 Since racial/ethnic inequities in health outcomes exist for many HPV-associated cancers,Citation5,Citation27,Citation28 reducing racial/ethnic disparities in HPV vaccination could contribute long-term to reducing health disparities and inequities that have been historically observed for these cancers.
Our overall finding of low self-reported prevalence of HPV vaccination uptake (15.5% of the study sample) among all adults ages 27–45 years, irrespective of race/ethnicity, is important because it highlights the need for greater public health messaging about the updated FDA age indication and it establishes a baseline from which progress can be tracked. Dissemination and implementation of new guidelines into clinical practice can be slow to occur and a complex process.Citation29,Citation30 Strategies to increase HPV vaccination among adults up to age 45 will require a multifaceted approach that targets health organizations, healthcare providers, and patients to ensure that all stakeholders are aware of the 2018 FDA approval. These strategies will also need to be tailored to different population-groups; therefore, understanding specific racial/ethnic and other demographic disparities in vaccination was the central focus of our study.
We found that even after adjusting for race/ethnicity and other potential confounding factors, women had over three times the odds of vaccine initiation compared to men. This finding is not surprising since women report higher HPV vaccination across the adolescent age spectrum compared to men.Citation31 It is important to note that the HPV vaccine messaging has historically been more female-centric rather than being gender neutral, and the vaccine was approved for young girls for about 5 years before its use in boys were approved.Citation32,Citation33 Unsurprisingly, women have greater knowledge and awareness of the HPV vaccine than men.Citation19,Citation34,Citation35 A previous analysis of national-level data of adults over the age of 18 found that women were 225% more likely to have heard of HPV and 281% more likely to have heard of the HPV vaccine compared to men.Citation19 One study found that adult women in the 27–45 age group may also be more likely to engage with and ask healthcare providers about HPV vaccination; however, when controlling for additional factors, the level of engagement was not found to be statistically significant.Citation18 While the association between HPV infection and cervical cancer is generally well-known among the public, it is important to note that oropharynx cancer is currently the most common HPV-associated cancer type in the United States, and it affects men at a substantially greater rate than women.Citation5,Citation27,Citation28 Therefore, reducing gender disparities in HPV vaccination is also critical for public health, and all proposed strategies for increasing HPV vaccine uptake will need to place an emphasis on eliminating the feminization of HPV vaccines as well as eliminating gender disparities associated with receipt of the vaccine.Citation32,Citation33
With regard to race/ethnicity, we found that compared to Non-Hispanic White adults between 27 and 45 years, Non-Hispanic Black adults were more likely to have been vaccinated against HPV after adjusting for potential confounders, while Hispanic adults were less likely to have been vaccinated. Based on previous literature,Citation19,Citation36,Citation37 we hypothesized that racial/ethnic minorities would fare worse in adult HPV vaccine uptake. Our findings were however different from our hypothesis. A previous study conducted using data prior to the updated 2018 FDA age indication found that Black men in the 27–45 age range had significantly lower odds of HPV vaccination than White men and Black adult women did not differ significantly from white women in their odds of being vaccinated.Citation36 Also, Black adults have been previously shown to be less likely aware of HPV and the HPV vaccine compared to White adults.Citation19 It is important to note that our study used HPV vaccine initiation as the primary outcome rather than completion of the HPV vaccine series. Our results are in contrast with current data which suggests higher HPV vaccine initiation among White adolescents.Citation23,Citation24 However, this differential rate of uptake among adolescents based on race/ethnicity may be a bit more nuanced. For example, a previous study among younger adults (ages 18–26 years) found that while Black individuals were more likely to initiate HPV vaccination compared to White individuals, they were less likely to complete the vaccine series.Citation38 Additionally, our data only includes 1 year post approval of the extended age of eligibility, so more data may be needed to understanding the underlying drivers of our finding, which would also in the future include data on HPV vaccine completion disparities in this adult age group.
Odds of HPV vaccination among adult Hispanic individuals have been mixed. While our study found that Hispanic adults had a lower odds of vaccination compared to Non-Hispanic White adults, a previous study of adult Hispanic men and women conducted prior to the updated expanded age of eligibility in 2018 found no significant difference.Citation36 However, a 2016 study found that Hispanic women ages 18–30 years were less likely to both initiate and complete HPV vaccination compared to White women.Citation37 Nativity and factors associated with acculturation have similarly yielded mixed results; one previous study showing decreased odds of HPV vaccine uptake among foreign-born adults aged 18–26 years,Citation38 while another showed no significant difference for foreign-born adult men and women.Citation39 Latina immigrants have also been shown to be less likely to have general knowledge about the HPV vaccine, how to access the vaccine, or where to obtain more information about the vaccine compared to US-born Latinas.Citation40 Note that the current analysis did not control for nativity or factors related to acculturation, and did not estimate odds of vaccine uptake by sex. Nevertheless, it is important that interventions for preventing HPV-associated cancers through vaccine uptake are targeted toward racial/ethnic minority adults, including individuals who are foreign-born and may have both cultural and linguistic challenges.Citation41 Evidence suggests that among racial/ethnic minorities, those with a preference for, or proficient with English language are more likely to have greater awareness of the HPV vaccine and its effectiveness.Citation41,Citation42 Future studies should focus on understanding the role of language proficiency and acculturation in HPV vaccine uptake among adult racial/ethnic minorities ages 27–45 years, including foreign-born Black and Hispanic individuals in the United States.
Access to care is a hallmark of health promotion and prevention in the United States. It is central to the Department of Health and Human Services’ strategic plan,Citation43 and is a central component of several Healthy People 2030 objectives.Citation44 We confirmed our hypothesis that adults with a regular place of healthcare would have greater odds of receiving the HPV vaccine compared to individuals without one. Having a usual place of care and having regular physician visits have previously been found to be independently associated with adults’ receipt of most common vaccines.Citation45 A lack of recommendation from a healthcare provider has been cited as the most frequent reason for parents not completing the vaccine series.Citation46 Also, among adults ages 27–45 years, healthcare providers have been cited to be the preferred source for receiving information about HPV vaccination.Citation47 This is particularly critical for this recommendation, since the recommendation for the HPV vaccine for this among 27 to 45 year olds includes a caveat that the decision to accept the vaccine should be based on a shared-decision model. Evidently, it may be more difficult to have a shared decision about whether or not to receive the HPV vaccine when an individual does not have a usual place of care or a regular provider to engage in this conversation with. While the current study has not focused on factors driving HPV vaccine hesitancy in adults, evidence from the younger eligible groups suggests that a lack of recommendation, and a lack of knowledge about the HPV vaccine are among two of the most common barriers driving hesitancy to receive the vaccine.Citation48 These are system-level barriers that could be mitigated with regular access to healthcare and physicians engagement with patients to educate on benefits of the HPV vaccine. Taken together, our findings and the findings of previous studies emphasize the important role that regular access to quality healthcare plays in HPV vaccination promotion.
Regarding shared decision-making in vaccinating individuals aged 27–45 years, one important factor, while beyond the scope of the present study, is health literacy, and how race/ethnicity might impact any association between health literacy and HPV vaccine uptake in this age group. Previous evidence suggests a correlation between health literacy and HPV vaccine uptake among individuals between 27 and 45 years.Citation49,Citation50 Given the well-known lack of knowledge of HPV vaccine in the general population, as well as persistent vaccine hesitancy across several subgroups in the United States,Citation19 it is important to further explore the role of health literacy in HPV vaccine uptake in this age group of 27–45 years, based on race/ethnicity, and other sociodemographic factors.
Public health significance
A significant portion of the 27 to 45 year olds in our study were yet to be vaccinated (84.5%). Since most HPV-associated cancers are diagnosed in adults older than 45 years,Citation5 this expanded recommendation to vaccinate individuals up to age 45 years may eventually help prevent more HPV-associated cancers in the future. It is therefore critical to increase awareness and knowledge of HPV/HPV vaccines in this age group. Males are in particular need of increased knowledge of the vaccine, in light of the increasing incidence of both anal and oropharyngeal cancers.Citation6,Citation51,Citation52 For oropharyngeal cancer, about 75% of new cases are in males.Citation6,Citation32 As oral HPV is the primary cause of HPV-associated oropharyngeal cancer, providing the HPV vaccine to middle-aged individuals is undoubtedly an important strategy to decreasing risk of infection, persistence, and eventual HPV-associated oropharyngeal malignancy. While the population benefit of the HPV vaccines in preventing oropharyngeal cancer may not be realized until years later,Citation53 there are ongoing clinical trials to definitely establish that the current vaccines are effective in the prevention of oral HPV infection.
Strengths and limitations
The strengths of our study include our use of a nationally representative sample of adults in the United States. Furthermore, to the best of our knowledge, this is the first study since the FDA’s expanded age of eligibility to exclusively examine differential HPV vaccine uptake in a racial/ethnically diverse sample of 27- to 45-year-old adults. There are important limitations to our study as well. We used self-reported data, which is subject to potential reporting bias that could impact the study results. We also did not have the ability to adjust for a wide range of validated acculturation factors, which could have potentially influenced the association observed between HPV vaccination reported among Hispanic and Asian participants. The latter were grouped under “Other” and due to sample size constraints; we were unable to explore this group further to examine drivers of HPV vaccination among adults. Our outcome of interest was also based on a single-item questionnaire, and we only analyzed data on HPV vaccine initiation and not series completion, and could have resulted in a different pattern of racial/ethnic disparities. More importantly, while individuals in the current study were between 27 and 45 years, they may have received their HPV vaccine at an earlier age,Citation17 and we are unable to establish the exact year of receiving the HPV vaccine among individuals in our study.
Despite these limitations, findings from our nationally representative study provide a strong baseline that can be used to track the effectiveness of HPV vaccine promotion efforts over time, especially based on race/ethnicity. To the best of our knowledge, it is the first to examine the association between race/ethnicity and HPV vaccination uptake among individuals aged 27–45 years. Future studies, including mixed-methodology studies, should explore in-depth HPV vaccine barriers in adults from diverse background, and the role of health literacy in uptake.
Conclusions
Our study found that among adults aged 27–45 years in the United States, there are disparities in HPV vaccine uptake. Adult men, and Hispanics had lower odds of receiving the vaccine, as were individuals without a usual place of care. Given the importance of the HPV vaccine in cancer prevention, it is critical that these disparities are addressed and mitigated.
Disclosure statement
Dr. Osazuwa-Peters is a scientific advisor to Navigating Cancer.
Additional information
Funding
References
- Browne S, Feemster KA. Human papillomavirus: optimizing opportunities for prevention. Curr Opin Pediatr. 2022;34(2):132–8. doi:10.1097/MOP.0000000000001119.
- Chesson HW, Dunne EF, Hariri S, Markowitz LE. The estimated lifetime probability of acquiring human papillomavirus in the United States. Sex Transm Dis. 2014;41(11):660–664. doi:10.1097/OLQ.0000000000000193.
- Markowitz LE, Dunne EF, Saraiya M, Lawson HW, Chesson H, Unger ER. Quadrivalent human papillomavirus vaccine: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2007;56:1–24.
- Pauli S, Kops NL, Bessel M, Lina Villa L, Moreno Alves Souza F, Mendes Pereira GF, Neves Hugo F, Comerlato J, Bandeira I, Fernandes B, et al. Sexual practices and HPV infection in unvaccinated young adults. Sci Rep. 2022;12(1):12385. doi:10.1038/s41598-022-15088-8.
- Osazuwa-Peters N, Simpson MC, Rohde RL, Challapalli SD, Massa ST, Adjei Boakye E. Differences in sociodemographic correlates of human papillomavirus-associated cancer survival in the United States. Cancer Control. 2021;28:10732748211041894. doi:10.1177/10732748211041894.
- Osazuwa-Peters N, Simpson MC, Massa ST, Adjei Boakye E, Antisdel JL, Varvares MA. 40-year incidence trends for oropharyngeal squamous cell carcinoma in the United States. Oral Oncol. 2017;74:90–97. doi:10.1016/j.oraloncology.2017.09.015.
- Chaturvedi AK, Engels EA, Pfeiffer RM, Hernandez BY, Xiao W, Kim E, Jiang B, Goodman MT, Sibug-Saber M, Cozen W, et al. Human papillomavirus and rising oropharyngeal cancer incidence in the United States. J Clin Oncol. 2011;29(32):4294–4301. doi:10.1200/JCO.2011.36.4596.
- Ellington TD, Henley SJ, Senkomago V, O’Neil ME, Wilson RJ, Singh S, Thomas CC, Wu M, Richardson LC. Trends in incidence of cancers of the oral cavity and pharynx—United States 2007–2016. MMWR Morb Mortal Wkly Rep. 2020;69(15):433. doi:10.15585/mmwr.mm6915a1.
- Gillison ML, Chaturvedi AK, Anderson WF, Fakhry C. Epidemiology of human papillomavirus-positive head and neck squamous cell carcinoma. J Clin Oncol. 2015;33(29):3235–42. doi:10.1200/JCO.2015.61.6995.
- Guo T, Eisele DW, Fakhry C. The potential impact of prophylactic human papillomavirus vaccination on oropharyngeal cancer. Cancer. 2016;122(15):2313–2323. doi:10.1002/cncr.29992.
- Osazuwa-Peters N. Human Papillomavirus (HPV), HPV-associated oropharyngeal cancer, and HPV vaccine in the United States–do we need a broader vaccine policy? Vaccine. 2013;31(47):5500–5. doi:10.1016/j.vaccine.2013.09.031.
- Petrosky E, Bocchini JA Jr, Hariri S, Chesson H, Curtis CR, Saraiya M, Unger ER, Markowitz LE. Use of 9-valent Human Papillomavirus (HPV) vaccine: updated HPV vaccination recommendations of the advisory committee on immunization practices. MMWR Morb Mortal Wkly Rep. 2015;64:300–4.
- U.S. Food and Drug Administration (FDA). FDA approves expanded use of Gardasil 9 to include individuals 27 through 45 years old. https://www.fda.gov/news-events/press-announcements/fda-approves-expanded-use-gardasil-9-include-individuals-27-through-45-years-old.
- Meites E, Szilagyi PG, Chesson HW, Unger ER, Romero JR, Markowitz LE. Human papillomavirus vaccination for adults: updated recommendations of the advisory committee on immunization practices. MMWR Morb Mortal Wkly Rep. 2019;68(32):698–702. doi:10.15585/mmwr.mm6832a3.
- Lewis RM, Markowitz LE, Gargano JW, Steinau M, Unger ER. Prevalence of genital human papillomavirus among sexually experienced males and females aged 14–59 years, United States, 2013–2014. J Infect Dis. 2018;217(6):869–77. doi:10.1093/infdis/jix655.
- King LM, Lewnard JA, Niccolai LM. Clinical and public health considerations for HPV vaccination in midadulthood: a narrative review. Open Forum Infect Dis. 2023;10(1). doi:10.1093/ofid/ofad004.
- Suk R, Liao K, Bauer CX, Basil C, Li M. Human papillomavirus vaccine administration trends among commercially insured US adults aged 27-45 years before and After Advisory Committee on Immunization Practices Recommendation Change, 2007–2020. JAMA Health Forum. 2022;3:e224716. doi:10.1001/jamahealthforum.2022.4716.
- Thompson EL, Garg A, Galvin AM, Moore JD, Kasting ML, Wheldon CW. Correlates of HPV vaccination intentions among adults ages 27-45 years old in the U.S. J Commun Health. 2021;46(5):893–902. doi:10.1007/s10900-021-00968-3.
- Adjei Boakye E, Tobo BB, Rojek RP, Mohammed KA, Geneus CJ, Osazuwa-Peters N. Approaching a decade since HPV vaccine licensure: racial and gender disparities in knowledge and awareness of HPV and HPV vaccine. Hum Vaccin Immunother. 2017;13(11):2713–2722. doi:10.1080/21645515.2017.1363133.
- Thompson EL, Wheldon CW, Rosen BL, Maness SB, Kasting ML, Massey PM. Awareness and knowledge of HPV and HPV vaccination among adults ages 27–45 years. Vaccine. 2020;38(15):3143–8. doi:10.1016/j.vaccine.2020.01.053.
- Stephens ES, Dema E, McGee-Avila JK, Shiels MS, Kreimer AR, Shing JZ. Human papillomavirus awareness by educational level and by race and ethnicity. JAMA Netw Open. 2023;6(11):e2343325. doi:10.1001/jamanetworkopen.2023.43325.
- Le D, Kim HJ, Wen KY, Juon HS. Disparities in awareness of the HPV vaccine and HPV-associated cancers among racial/ethnic minority populations: 2018 HINTS. Ethn Health. 2023;28(4):586–600. doi:10.1080/13557858.2022.2116630.
- Abouelella DK, Canick JE, Barnes JM, Rohde RL, Watts TL, Adjei Boakye E, Osazuwa-Peters N. Human papillomavirus vaccine uptake among teens before and during the COVID-19 pandemic in the United States. Hum Vaccines Immunother. 2022;18(7):2148825. doi:10.1080/21645515.2022.2148825.
- Francis JKR, Weerakoon SM, Lucas SL, Mathew MS, Durante JC, Kelly N, Tiro JA. Human papillomavirus vaccination before and during the COVID-19 pandemic. JAMA Netw Open. 2022;5(9):2234000. doi:10.1001/jamanetworkopen.2022.34000.
- Centers for Disease Control and Prevention (CDC). National center for health statistics. National Health Interview Survey; [accessed 2023 Mar 28]. https://www.cdc.gov/nchs/nhis/about_nhis.htm.
- Brotherton JM, Zuber PL, Bloem PJ. Primary prevention of HPV through vaccination: update on the current global status. Curr Obstet Gynecol Rep. 2016;5(3):210–224. doi:10.1007/s13669-016-0165-z.
- Razzaghi H, Saraiya M, Thompson TD, Henley SJ, Viens L, Wilson R. Five-year relative survival for human papillomavirus-associated cancer sites. Cancer. 2018;124(1):203–211. doi:10.1002/cncr.30947.
- Osazuwa-Peters N, Massa ST, Simpson MC, Adjei Boakye E, Varvares MA. Survival of human papillomavirus-associated cancers: filling in the gaps. Cancer. 2018;124(1):18–20. doi:10.1002/cncr.30945.
- Berwick DM. Disseminating innovations in health care. JAMA. 2003;289(15):1969–1975. doi:10.1001/jama.289.15.1969.
- Brownson RC, Fielding JE, Maylahn CM. Evidence-based public health: a fundamental concept for public health practice. Annu Rev Public Health. 2009;30(1):175–201. doi:10.1146/annurev.publhealth.031308.100134.
- Pingali C, Yankey D, Elam-Evans LD, Markowitz LE, Williams CL, Fredua B, McNamara LA, Stokley S, Singleton JA. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years—United States, 2020. MMWR Morb Mortal Wkly Rep. 2021;70(35):1183. doi:10.15585/mmwr.mm7035a1.
- Osazuwa-Peters N, Adjei Boakye E, Mohammed KA, Tobo BB, Geneus CJ, Schootman M. Not just a woman’s business! Understanding men and women’s knowledge of HPV, the HPV vaccine, and HPV-associated cancers. Prev Med. 2017;99:299–304. doi:10.1016/j.ypmed.2017.03.014.
- Daley EM, Vamos CA, Thompson EL, Zimet GD, Rosberger Z, Merrell L, Kline NS. The feminization of HPV: how science, politics, economics and gender norms shaped U.S. HPV vaccine implementation. Papillomavirus Res (Amsterdam, Netherlands). 2017;3:142–8. doi:10.1016/j.pvr.2017.04.004.
- Osazuwa-Peters N, Wang DD, Namin A, John VM, O’Neill M, Patel PV, Varvares MA. Sexual behavior, HPV knowledge, and association with head and neck cancer among a high-risk group. Oral Oncol. 2015;51(5):452–6. doi:10.1016/j.oraloncology.2015.01.011.
- Osazuwa-Peters N, Adjei Boakye E, Chen BY, Clancy J, Vallot PL, Su JL, Beck GE, Varvares MA. Sociodemographic factors associated with knowledge and risk perception of human papillomavirus and human papillomavirus–associated oropharyngeal squamous cell carcinoma among a predominantly Black population. JAMA Otolaryngol Head Neck Surg. 2017;143(2):117–24. doi:10.1001/jamaoto.2016.2784.
- Kasting ML, Giuliano AR, Christy SM, Rouse CE, Robertson SE, Thompson EL. Human papillomavirus vaccination prevalence among adults aged 19–45 years: an analysis of the 2017 national health interview survey. Am J Prev Med. 2020;59(6):837–49. doi:10.1016/j.amepre.2020.05.031.
- Daniel-Ulloa J, Gilbert PA, Parker EA. Human papillomavirus vaccination in the United States: uneven uptake by gender, race/ethnicity, and sexual orientation. Am J Public Health. 2016;106(4):746–747. doi:10.2105/AJPH.2015.303039.
- De P, Budhwani H. Human Papillomavirus (HPV) vaccine initiation in minority Americans. Pub Health. 2017;144:86–91. doi:10.1016/j.puhe.2016.11.005.
- Adjei Boakye E, Zeng W, Governor S, Nagendra S, Tobo BB, Simpson MC, Osazuwa-Peters N. Differences in Human Papillomavirus (HPV) vaccine uptake by nativity status among men aged 18–34 years. Prev Med Rep. 2019;16:101010. doi:10.1016/j.pmedr.2019.101010.
- Ashing KT, Carrington A, Ragin C, Roach V. Examining HPV- and HPV vaccine-related cognitions and acceptability among US-born and immigrant hispanics and US-born and immigrant Non-Hispanic Blacks: a preliminary catchment area study. Cancer Causes Control. 2017;28(11):1341–1347. doi:10.1007/s10552-017-0973-0.
- Lee HY, Luo Y, Neese J, Daniel C, Hahm HC. The role of English proficiency in HPV and HPV vaccine awareness: a cross-sectional study across race/ethnicity. Asian Pac J Cancer Prev. 2021;22(2):349–357. doi:10.31557/APJCP.2021.22.2.349.
- Ashing KT, Chávez NR, Serrano M. HPV vaccine-related knowledge, beliefs, acceptability, and uptake among Latinas who prefer English and those who prefer Spanish. J Health Commun. 2016;21(12):1209–16. doi:10.1080/10810730.2016.1240266.
- US Department of Health and Human Services. Strategic plan FY 2022-2026. Strategic goal 1: protect and strengthen equitable access to high quality and affordable healthcare. https://www.hhs.gov/about/strategic-plan/2022-2026/goal-1/index.html#:~:text=Increasing%20choice%2C%20affordability%20and%20enrollment,safe%20medical%20devices%20and%20drugs.
- U.S. Department of Health and Human Services. Office of disease prevention and health promotion. Healthy People 2030. Objectives. https://health.gov/healthypeople/objectives-and-data/browse-objectives#settings-and-systems.
- Lu PJ, O’Halloran A, Williams WW, Lindley MC, Farrall S, Bridges CB. Racial and ethnic disparities in vaccination coverage among adult populations in the U.S. Am J Prev Med. 2015;49(6 Suppl 4):S412–425. doi:10.1016/j.amepre.2015.03.005.
- Sonawane K, Zhu Y, Montealegre JR, Lairson DR, Bauer C, McGee LU, Giuliano AR, Deshmukh AA. Parental intent to initiate and complete the human papillomavirus vaccine series in the USA: a nationwide, cross-sectional survey. Lancet Public Health. 2020;5(9):484–92. doi:10.1016/S2468-2667(20)30139-0.
- Wheldon CW, Garg A, Galvin AM, Moore JD, Thompson EL. Decision support needs for shared clinical decision-making regarding HPV vaccination among adults 27-45 years of age. Patient Educ Couns. 2021;104(12):3079–85. doi:10.1016/j.pec.2021.04.016.
- Adjei Boakye E, Nair M, Abouelella DK, Joseph CLM, Gerend MA, Subramaniam DS, Osazuwa-Peters N. Trends in reasons for human papillomavirus vaccine hesitancy: 2010–2020. Pediatrics. 2023;151(6). doi:10.1542/peds.2022-060410.
- Galvin AM, Garg A, Griner SB, Moore JD, Thompson EL. Health literacy correlates to HPV vaccination among US adults ages 27-45. J Cancer Educ. 2023;38(1):349–56. doi:10.1007/s13187-021-02123-x.
- Alaraj RA, Brown B, Polonijo AN. “If people were told about the cancer, they’d want to get vaccinated”: knowledge, attitudes, and beliefs about HPV vaccination among mid-adult men. Am J Men’s Health. 2023;17(1):15579883231153310. doi:10.1177/15579883231153310.
- Deshmukh AA, Suk R, Shiels MS, Sonawane K, Nyitray AG, Liu Y, Gaisa MM, Palefsky JM, Sigel K. Recent trends in squamous cell carcinoma of the anus incidence and mortality in the United States, 2001–2015. J Natl Cancer Inst. 2020;112(8):829–38. doi:10.1093/jnci/djz219.
- Liao CI, Francoeur AA, Kapp DS, Caesar MAP, Huh WK, Chan JK. Trends in human papillomavirus-associated cancers, demographic characteristics, and vaccinations in the US, 2001–2017. JAMA Netw Open. 2022;5(3):e222530. doi:10.1001/jamanetworkopen.2022.2530.
- Xu L, Dahlstrom KR, Lairson DR, Sturgis EM. Projected oropharyngeal carcinoma incidence among middle-aged US men. Head Neck. 2019;41(9):3226–3234. doi:10.1002/hed.25810.

