ABSTRACT
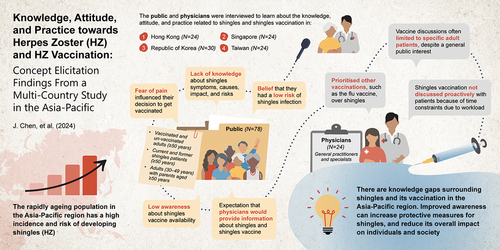
Herpes zoster (HZ) is a prevalent disease characterized by a painful rash. A multi‑country study was conducted to elicit public and physician knowledge, attitude, and practice (KAP) toward HZ disease and vaccination for the assessment of local factors influencing HZ vaccine perceptions in four Asian-Pacific countries/territories One-to-one qualitative interviews were conducted in 2022, among the public (people aged ≥ 50 years, adults with parents aged ≥ 50 years, zoster vaccine live-vaccinated individuals aged ≥ 50 years in Republic of Korea, and HZ patients; n = 78) and physicians (general practitioners and specialists; n = 24). Themes surrounding KAP toward HZ and HZ vaccination were summarized using a thematic analysis. A substantial knowledge gap related to HZ was observed among the public, including its causes, long-term impacts, and the at-risk population. There was a low perceived risk of HZ and low general awareness of HZ vaccine availability, although country/territory-specific differences existed. Fear of HZ-associated pain contributed toward vaccination intent among HZ patients and adults with parents aged ≥ 50 years. HZ-naïve adults who were encouraged to receive the vaccine by others were not motivated to do so due to optimism bias. Physicians were perceived to be a reliable source of information. However, physicians did not always proactively discuss HZ vaccination due to time constraints and a perceived need to prioritize other vaccinations including influenza and pneumococcal vaccines. Initiatives are needed to improve public awareness of HZ and its complications, in terms of overall impact on individuals and society, and highlight the important role of physicians in recommending vaccination.
Introduction
Herpes zoster (HZ, commonly known as shingles) is a prevalent and debilitating disease characterized by a painful, blistering rash,Citation1 with a lifetime risk of approximately 30% worldwide.Citation2–4 Additionally, approximately 5–30% of HZ patients have experienced postherpetic neuralgia (PHN), defined as pain persisting for at least 3 months after rash onset.Citation5 Pain and resulting discomfort due to HZ and PHN is a significant problem experienced by HZ patients and is related to reduced quality of life (QoL), impaired activity levels and work productivity, and higher healthcare resource utilization,Citation6–9 therefore resulting in a significant socioeconomic burden. The greatest burden of disease is seen in older adults and immunocompromised individuals.Citation1,Citation5
The average HZ incidence in the rapidly aging population of the Asia-Pacific region has been estimated at 3–10 per 1,000 person-years, whilst HZ incidence rises steeply above 40 years and peaks at 70–80 years.Citation2 Furthermore, almost all adults aged ≥40 years in the Asia-Pacific region are varicella zoster virus (VZV)-seropositive and are therefore at risk of developing HZ.Citation2 Previous studies in the Asia-Pacific region have also shown that HZ incidence increases in adults aged ≥50 years.Citation10,Citation11 While HZ symptoms can be managed using antiviral therapy and analgesics, limitations exist with current treatments. For example, many patients with HZ often initiate treatment too late, limiting its effectiveness. Even with prompt intervention, a substantial portion of patients experience poor or inadequate control of their symptoms.Citation2 HZ is, however, vaccine-preventable, and HZ vaccination has been reported to reduce the incidence of HZ, associated complications and disease burden.Citation2,Citation4,Citation12,Citation13 Currently, there are two main types of HZ vaccines available – the live attenuated zoster vaccine (ZVL) and the adjuvanted recombinant zoster vaccine (RZV). Both types of vaccines are licensed in several countries/territories in the Asia-Pacific region for the prevention of HZ in adults aged ≥50 years.Citation14 In some countries/territories, RZV is also licensed for people aged ≥18 years at increased risk of HZ.Citation15
There are limited studies describing the knowledge, attitude, and practice toward HZ disease and vaccination, and assessing local factors influencing HZ vaccination in the AsiaPacific in adults aged ≥50 years.Citation2,Citation13 This suggests an under-recognition of both HZ burden and the need for prevention of HZ in the region. Aside from factors influencing HZ vaccination at the individual level, it is well established that interactions with healthcare professionals (HCPs) play a major role in driving the healthcare-seeking behaviors of the public.Citation16 Indeed, effective communication between HCPs and patients can improve patients’ knowledge about health issues, alleviate their concerns regarding vaccine safety and side effects, and encourage vaccine uptake.Citation16,Citation17 As such, there is a need to better understand knowledge, attitude, and practice toward HZ disease and vaccination amongst the public, as well as among HCPs.
Therefore, the primary objective of this study was to evaluate knowledge, attitude, and practice related to HZ disease and HZ vaccination among public and physicians in four countries/territories within the Asia-Pacific, namely, Hong Kong, Republic of Korea, Singapore, and Taiwan. The secondary objective was to explore key differences in terms of knowledge, attitude, and practice related to HZ disease and HZ vaccination across different countries/territories, different respondent groups and sub-groups. Finally, the exploratory objective of this study was to understand whether any respondent characteristics or factors may be associated with gaps in knowledge, attitude, or practice.
Methods
Study population
The respondents included in this study comprised individuals in the following groups from Hong Kong, Republic of Korea, Singapore, and Taiwan: (i) HZ-naïve older adults aged ≥50 years; (ii) HZ-vaccinated older adults aged ≥50 years; (iii) adults aged 30–49 years with parents aged ≥50 years; (iv) current or former HZ patients; (v) physicians, including general practitioners (GPs) and specialists (i.e., infectious disease specialists, geriatricians, dermatologists).
All respondents were recruited via purposive/selective sampling and were screened over phone calls and/or e-mails. The detailed inclusion and exclusion criteria for enrollment in the study can be found in . Non-physician respondents were recruited via Kantar Profiles’ proprietary double opt-in panel, LifePoints (LifePoints is a high-quality, proprietary research panel which is a compliant and rich source of first-party data) and/or its partners’ databases.Citation18 Physician respondents were recruited via local HCP databases or panels. Upon successful screening and recruitment of participants, none of the participants withdrew from the study.
Table 1. Screening criteria for respondents enrolled in the study.
A total of 102 respondents from the public and 24 physicians were included in this study. The sample size of respondents per country/territory can be found in ; the sample size was based on previous mixed methods studies where 10–15 interview participants for each market were recruited. This approach was deemed sufficient for studying the themes significant to those interviewed and for identification of factors that influence treatment decision making.Citation19–21 From a subgroup perspective, it was assumed that respondents within subgroups were homogeneous in nature, and previous studies have suggested that the majority of themes (80% saturation) can be captured with six interviews in a homogeneous sample in qualitative research.Citation22
Table 2. Sample size of respondents per country/territory for qualitative interviews.
Study design
A thematic and purposive literature review was conducted to gather insights in order to inform development of the qualitative discussion guide for the interviews. Search terms included ‘Herpes Zoster/shingles epidemiology’, ‘Herpes Zoster/shingles incidence’, ‘Herpes Zoster/shingles disease burden’, and ‘Herpes Zoster/shingles symptoms’. Pilot interviews were conducted for each respondent type to assess the interview duration and participants’ understanding of questions and prompts; no adjustments to the guide were required following the pilot interviews. Published materials providing examination of recent or current literature, covering a wide range of subjects at various levels of completeness and comprehensiveness, were also referenced.
Informed consent was obtained from all individual participants included in the study prior to the interview. Informed consent forms (ICF) were disseminated to participants via e-mail, and participants were requested to thoroughly review the document and confirm their participation by signing the form. The ICF included information about the objectives of the study, the approximate length of the interview, honoraria for participation, and potential risks and benefits from participation. The study team’s contact information was also provided for participants to share any questions or concerns about the study. To avoid bias, the name of the study sponsor was not disclosed in the ICF and was only disclosed after participation in the study.
Thirty-minute one-to-one virtual concept elicitation interviews were conducted via video calls between January and March 2022 to elucidate the relevant themes surrounding the respondents’ knowledge, attitude, and practice toward HZ disease and vaccination. Interviews for the five respondent groups were conducted by interviewers of Oracle Life Sciences and/or its partners, who were native speakers with experience in conducting healthcare-specific interviews. All Oracle Life Sciences’ local partners, including recruiters and moderators, were trained to ensure consistency in carrying out the screening and qualitative interviews. Interviews were conducted in English or Mandarin (Singapore), English or Cantonese (Hong Kong), Mandarin (Taiwan), and Korean (Republic of Korea). Questions were designed specifically for each respondent group to cater to differences between these groups. All interviews were recorded with respondents’ consent and were fully transcribed and reviewed by the respective interviewers. Insights from interviewers were also captured in the analysis. During the study, all data files and data management/analysis syntax were stored on Oracle Life Sciences cloud-based servers, where permission to access the files was only granted to specific team members.
Interview transcripts were thematically analyzed using NVivo software by three data coders. The key researcher was in charge of establishing the code book by developing the code structure, after reviewing transcripts from the initial interviews. After the code book was established, the researchers and coders reconvened as a team to align on the initial codes before establishing the codes for remaining transcripts. These codes were then used to establish themes for the final report upon reaching data saturation.
The prominent themes and sub-themes identified and extracted from the responses were validated with the hypotheses generated from the literature. The overall aim of this analysis was to identify gaps in the understanding of the general population and physicians in specific areas, identify potential areas for behavioral change interventions, and provide insights through the Capability, Opportunity, Motivation, and Behavior (COM-B) behavioral model at the heart of the Behavior Change Wheel framework.Citation23 The study flowchart and the COM-B model can be found in and Supplementary Figure S1, respectively.
Figure 1. Study flowchart.

The study protocol, ICF, screener and discussion guide were submitted to and reviewed by the above-country central Institutional Review Board (IRB), Pearl IRB, fully accredited by the Association of Accreditation of Human Resource Protection Program Inc. (AAHRPP), which confirmed that no ethical approval was required. In addition, this study covered multiple countries/territories and posed minimal risk to study participants. Finally, this study adhered to the consolidated criteria for reporting qualitative research (COREQ) checklist, which comprises of study design, methodology, analysis, and reporting considerations, for ensuring comprehensive reporting of qualitative studies.
Results
General population
Lack of knowledge about HZ symptoms, causes, risk factors and long-term complications
Current knowledge of HZ as a disease was limited in the study population, with some awareness of its symptoms (e.g., blisters, pain), causes, risk factors, and long-term complications (e.g., neuralgia, and vision, hearing, brain, and renal impairment). Across the countries/territories surveyed, although educational information had been communicated about the disease and the need for vaccination in both media and healthcare settings, disease awareness was generally low. Respondents in the Republic of Korea were an exception, and their awareness of HZ was relatively higher than respondents in the other countries/territories. Korean respondents who demonstrated awareness of HZ and the HZ vaccine reported learning about these from educational information shared over medical programs on television, and educational posters in hospitals on HZ and its prevention.
Overall, most of the study population reported that while they were unaware of the initial symptoms of HZ (e.g., pain, itchy skin), they tended to be more aware of obvious symptoms (i.e., painful blisters). Respondents aware of HZ symptoms reported learning about these from current or former HZ patients whom they knew. A widespread belief, particularly among the elderly in Hong Kong, Singapore, and Taiwan, was that HZ is a “snake-like infection,” which may be lethal if it forms a ring around the body. HZ patients reported that they delayed seeking medical attention until symptoms worsened, as there was a tendency to mistake HZ symptoms for other illnesses (e.g., cold sores, stroke), until HZ diagnosis was confirmed by a physician.
Limited knowledge of vaccines in general
Knowledge of vaccines among respondents in the study population was limited to recent information that could readily be recalled based on memory and personal experience. The recency of the COVID-19 pandemic and COVID-19 vaccination seemed to have raised vaccine awareness and increased willingness toward vaccination; however, it also created fear and confusion around vaccine scheduling, efficacy, and potential side effects. Although respondents agreed that vaccines offered some level of protection against illnesses, they were less inclined to believe that they might be at risk of infection. It is likely that saliency and availability biases influenced the perceived likelihood of being infected by these illnesses. Hence, there was a lack of urgency and motivation among respondents to be vaccinated.
Low awareness about HZ vaccine availability
Respondents in Republic of Korea indicated a higher awareness of the HZ vaccine, compared with respondents in other countries/territories. Overall, respondents’ awareness of the vaccine was linked to word-of-mouth, education from the government, and recommendations by physicians.
It is likely that social norming influenced the intention to seek HZ vaccination, especially after the COVID-19 pandemic. However, HZ-naïve individuals were hindered by cost barriers, or knowledge gaps about the purpose of and when to receive the vaccine.
Individuals’ self-perceived risk of HZ varied, which may have contributed to a hot-to-cold empathy gap that was reportedly observed among respondents in the study population. In this case, “hot” state refers to a current or former HZ patient, whereas “cold” state refers to a HZ-naïve individual, who may find it difficult to empathize with a person who has experienced HZ. Consequently, current and former HZ patients reported a higher level of motivation to seek vaccination due to their fear of HZ-associated pain and its long-term complications. Similarly, adults with parents aged ≥50 years may have been influenced by accounts from current and former HZ patients about HZ-associated pain, motivating them to take preventative measures for their parents.
Individuals in the study population with chronic illnesses expressed concerns about the potential effects of the HZ vaccination on their chronic illness, highlighting a gap in knowledge. Finally, there was a desire across all respondents to learn more about the symptoms and impact of HZ and its vaccines, in order to make a more informed decision regarding HZ vaccination.
Information sources and influence
Awareness and knowledge of the HZ vaccine was mostly spread by word-of-mouth across the population, except for the Republic of Korea, where multiple sources of information were readily available. Patient advocates and social circles influenced public awareness and interest to learn more about the HZ vaccine. The younger generation (i.e., adults aged 30–49 years with parents aged ≥50 years) also sought information about HZ vaccines via Internet searches, and relayed information to their parents. In contrast, the older generation (i.e., adults aged ≥50 years) reported that they expected to learn more about HZ and HZ vaccines from physicians, whom they saw as a reliable source of information, and recommendations by a trusted doctor were usually accepted.
Physicians
Delayed disease recognition, diagnosis and treatment
Delayed disease recognition by physicians may have contributed to delayed HZ diagnosis and treatment; only a minority of physicians recognized the importance of early diagnosis. Additionally, occurrence of pain on its own tended to be misdiagnosed by physicians as other related diseases. However, some physicians, particularly specialists, reported that they would remind patients to seek medical treatment immediately once they experienced HZ-associated pain or once a blister appeared. Physicians had mixed views on whether or not women were at greater risk of HZ infection.
Vaccine prioritization by HCPs
Physicians reported that their beliefs surrounding vaccines were based on disease severity and seasonal prevalence, especially for vulnerable populations, such as older adults. They prioritized the influenza and pneumococcal vaccines over the HZ vaccine, due to the higher prevalence of influenza infections and the higher perceived severity of pneumococcal infections. Although physicians had ample knowledge about HZ vaccines and understood that the vaccine can contribute to prevention of HZ, opinions and knowledge of HZ varied within the group. For instance, physicians reported mixed views on the expected duration of efficacy of RZV vaccination (i.e., lifetime efficacy vs 10–20 years), whether patients with chronic conditions should be recommended HZ vaccines, and the safety of HZ vaccines (i.e., RZV, ZVL).
Physicians’ practice regarding HZ vaccine recommendation was reported to be driven by perceptions of disease severity, vaccine availability and accessibility on the national immunization board, as well as physicians’ own beliefs and clinical goals around positively impacting a patient’s quality of life. In general, physicians were less likely to recommend live HZ vaccines to high-risk patients (e.g., those receiving immunosuppressants, or who are pregnant) to limit potential complications due to contraindications. Cost and convenience were also reported as key considerations when making vaccine recommendations.
In Hong Kong, HZ vaccines were only available in private hospitals and not in public hospitals. Meanwhile, in Singapore and Taiwan, it was reported that the cost of vaccines limited vaccine recommendations by physicians, potentially deterring patients from seeking vaccination, and may render the vaccine inaccessible to some lower income groups.
Information sources and influence
By and large, physicians preferred to receive information from influential peers, representatives from pharmaceutical companies, or official government sources. Journals of internal medicine, publications, and medical or academic societies were also considered trusted sources of information for physicians. Although physicians were seen as trusted messengers by the public, physicians reported that they did not proactively initiate conversations regarding the HZ vaccine with their patients due to time constraints, particularly as a result of additional time and resources being diverted toward COVID-19 at the time of the interviews being conducted.
Physicians also reported that they tend to recommend vaccines that they are familiar with and have experience with. Physicians’ relationships with patients also affected communication, as physicians were only able to effectively recommend vaccinations when rapport or a level of trust had been established, although nuances were seen across clinical specialties. In addition, HCPs considered affordability when making vaccination recommendations to their patients.
Discussion
In this study, one-to-one concept elicitation interviews were conducted with respondents in Hong Kong, Republic of Korea, Singapore, and Taiwan. The objective of the study was to assess and understand the knowledge, attitude, and practice relating to HZ and HZ vaccines in order to identify factors which may influence the acceptance and recommendation of HZ vaccination. The results of this study indicated that there are substantial knowledge gaps surrounding HZ and HZ vaccination. Although educational information about HZ and HZ vaccination has been communicated in both media and healthcare settings across government, clinic, and hospital websites, as well as newspapers in the countries/territories surveyed,Citation24–32 disease awareness was still low among the public. In addition, several cognitive biases affected vaccination decisions. Although physicians had ample knowledge about HZ and HZ vaccination, existing issues, including the delayed diagnosis of HZ, low prioritization of HZ vaccines compared with flu and pneumococcal vaccines, lack of proactivity in initiating discussions about HZ vaccines, as well as cost and access barriers were identified. For high-risk patients (e.g., those receiving immunosuppressants, or who are pregnant), live HZ vaccines (i.e., ZVL) were not recommended by physicians due to concerns that HZ vaccination could potentially complicate pre-existing conditions or their treatment.
Our study provides a unique perspective by using qualitative interviews to elicit thoughts and feelings related to knowledge, attitude and practice toward HZ and HZ vaccines. In addition, the application of a comprehensive, evidence-based behavioral change framework (i.e., COM-B model) enriched the identification and understanding of the key gaps in knowledge, attitude, or practice and how they may be addressed. The three factors outlined in the COM-B model, which encompass both individual (i.e., ‘Capability’ and ‘Motivation’) and contextual determinants of behavior (i.e., ‘Opportunity’), interact with each other to influence behavioral changes.Citation23 Overall, the results of this study are consistent with existing studies which have also evaluated the knowledge, attitude, and practice associated with HZ and HZ vaccines in different populations.Citation33–38
The results of this study also demonstrated several cognitive biases associated with HZ and HZ vaccines. Of note, vaccine hesitancy, defined as the “delay in acceptance or refusal of vaccination despite availability of vaccination services,” is a worldwide cause of concern.Citation39 Several cognitive biases can affect the decision-making process surrounding vaccines, thus increasing vaccine hesitancy in the population.Citation40 In our study, availability biases and the tendency to attribute higher weight to factors that could readily be recalled were noted, as respondents were more aware of COVID-19 vaccines due to the recency of the COVID-19 pandemic and thereby attributed lower weight to HZ vaccines. Authority bias, or the tendency to attribute more weight to the opinion of authoritative figures, was also suggested in several of the responses captured, in which physicians and the government were perceived as reliable sources of information. Although authoritative figures are supportive of vaccines, vaccine uptake remained low as the public were heavily reliant on physicians and expected them to proactively communicate vaccine-related information. However, physicians did not initiate conversations about HZ vaccinations due to time constraints in the clinics, concerns on cost and convenience, and accessibility of HZ vaccines in their hospitals or countries/territories.
Among physicians, a perception bias was noted, as physicians’ willingness to recommend HZ vaccines appeared to be driven by their perception of disease severity, vaccine availability on the national immunization board, perceived patient acceptance of vaccines, and their beliefs and goals around positively impacting patients’ quality of life. HCPs play a major role in driving the healthcare-seeking behaviors of the public, thereby addressing the ‘Opportunity’ aspect of the COM-B model. Communication between HCPs and their patients provides patients with the opportunity to gain more knowledge about health issues and support them in assessing the severity of and susceptibility to a disease, whilst empowering them to make informed choices regarding their own health.Citation17 Furthermore, HCPs can provide reassurance and reduce patients’ uncertainties surrounding vaccine safety and side effects.Citation17 This, in turn, could influence the ‘Motivation’ factor of the COM-B model, and may encourage vaccine uptake among the general population. Given the key role that HCPs play in encouraging vaccination, it is crucial to strengthen connections with patients to reduce hesitancy surrounding vaccines.Citation16
Optimism bias, the tendency to have an unrealistically optimistic view about individual HZ risk, also appeared to play a role in respondents’ decisions to seek HZ vaccination. Respondents who had no personal experience, or second-hand knowledge from friends or family members with experience of HZ, were more likely to have a low perceived risk of HZ. These cognitive biases need to be taken into consideration when reconstructing vaccine-related communication to increase trust in vaccines and promote HZ vaccine uptake.Citation40
Following the concept elicitation interviews, an online survey with a larger number of respondents from the same respondent subgroups was conducted. Findings from the online survey may provide a better understanding of factors associated with the knowledge, attitude, and practice toward HZ and HZ vaccines, and may influence positive behavioral changes. Furthermore, it may facilitate communication with relevant stakeholders to evaluate current guidelines and policies surrounding HZ disease and HZ prevention, to optimize vaccination strategies in the Asia-Pacific countries/territories that were surveyed.
Limitations
People who are not aware of HZ, are rejectors of preventive vaccines, and individuals from low-income groups were not included in this study because many of the interview questions were not of relevance to these populations. Additionally, individuals who are unable to read and understand English and/or other region-specific languages were not included due to the interview methodology. As the inclusion criteria required respondents to be able to provide informed consent via e-mail and complete the interview via virtual platforms, respondents who were generally well-informed or well-versed in technology were more likely to participate and have an interest in the research. Taken altogether, the purposive/selective sampling during recruitment may have introduced a degree of selection bias into the study. Therefore, the findings from this study are not representative of the overall population in the countries/territories included. Nevertheless, the purpose of this study was to gain insights about knowledge, attitude, and practice toward HZ disease and vaccination and assess local factors influencing HZ vaccine perceptions in four locales within the Asia-Pacific region.
Another limitation of this study was that the survey panel included more individuals in the 30–49 and 50–64 years age groups, compared with the ≥65 years age group. To increase the representation of age groups within the sample, the recruitment of respondents ≥50 years was further stratified into two age groups (). The researcher’s presence or respondents’ awareness of being recorded during the interviews may have potentially affected responses. In addition, older participants may not have been as comfortable and communicative over a virtual interview, as compared to a face-to-face interview.
Finally, neurologists were not included among the specialists who were interviewed as part of this study. Given that neurologists may be more specialized in the diagnosis and management of HZ and PHN, the inclusion of neurologists may have provided specific insights into physicians’ knowledge, attitude, and practice toward HZ and HZ vaccination. A previous study conducted in China reported that patients with HZ, PHN, and zoster-associated pain primarily visited dermatology and pain management specialists.Citation41 Neurologist consultations were more important in severe cases of HZ, where neuropathic zoster-associated pain and PHN cause extensive nerve injuries (e.g., VZV vasculitis).Citation41 As neurologists are not frequently involved in the management of HZ cases and assessment of vaccinations, they were not interviewed in this study.
Conclusions
Knowledge gaps surrounding HZ and HZ vaccination remain. Therefore, initiatives are needed to improve public and physicians’ knowledge and awareness of HZ and its complications, in terms of the overall HZ disease burden and its impact on individuals and society, as well as to provide physicians with confidence in recommending HZ vaccination.
Authors’ Contributions
Substantial contributions to study conception and design: JC, SS, JS, RG, FC, MC, WSC, EH, KCH, LMH, HK, CKL, HNL, YS, CW, and ATYW; substantial contributions to analysis and interpretation of the data: JC, SS, JS, RG, RP, MC, WSC, EH, KCH, LMH, HK, HNL, YS, CW, and ATYW; drafting the article or revising it critically for important intellectual content: JC, SS, JS, RG, RP, FC, MC, WSC, EH, KCH, LMH, HK, CKL, HNL, YS, CW, and ATYW; final approval of the version of the article to be published: JC, SS, JS, RG, RP, FC, MC, WSC, EH, KCH, LMH, HK, CKL, HNL, YS, CW, and ATYW.
Ethics approval and consent to participate
This study covered multiple countries/territories and posed minimal risk to study participants. The above-country central Institutional Review Board (IRB), Pearl IRB, fully accredited by the Association of Accreditation of Human Resource Protection Program Inc. (AAHRPP) has confirmed that no ethical approval is required. Informed consent was obtained from all individual participants included in the study.
Ph1 KAP ZOASIS Manuscript_Supplementary Material_6Nov23.docx
Download MS Word (682.7 KB)Supplementary Figure 1_600dpi.jpg
Download JPEG Image (1.3 MB)Acknowledgments
This study was funded by GlaxoSmithKline Biologicals SA. The authors acknowledge Audrey Colliou, GSK, for operational support, and Roeland van Kerckhoven, GSK, Singapore for publication management. Authors also thank Costello Medical for editorial assistance and publication coordination, on behalf of GSK, and acknowledge Loveena Sharma, Costello Medical, Singapore for medical writing and editorial assistance based on authors’ input and direction.
Disclosure statement
JC, RP, and SS are employed by and have stock ownership in the GSK Group of Companies. MC was employed by the GSK Group of Companies when this study was conducted. EH, HK, and CW are employed by the GSK Group of Companies. JS and RG are employees of Oracle Life Sciences (previously Cerner Enviza), which received fees related to the conduct of this study from the GSK Group of Companies. WSC has received honoraria from the GSK Group of Companies. CKL has received honoraria from the GSK Group of Companies, is a member of the Singapore Medical Council, founder of GP+ Co-operative Ltd, and Chair of Primary Care Networks Council. LMH, HNL, and ATYW have received consulting fees from the GSK Group of Companies. FC, KCH, and YS have nothing to declare.
Data availability statement
The datasets generated and/or analyzed during the current study are not publicly available due to maintaining participant confidentiality in qualitative interview recordings.
Supplementary data
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2024.2317446.
Additional information
Funding
References
- Sampathkumar P, Drage LA, Martin DP. Herpes zoster (shingles) and postherpetic neuralgia. Mayo Clin Proc. 2009;84(3):274–9. doi:10.4065/84.3.274.
- Chen LK, Arai H, Chen LY, Chou MY, Djauzi S, Dong B, Kojima T, Kwon KT, Leong HN, Leung EM, et al. Looking back to move forward: a twenty-year audit of herpes zoster in Asia-Pacific. BMC Infect Dis. 2017;17(1):213. doi:10.1186/s12879-017-2198-y.
- Choi WS, Noh JY, Huh JY, Jo YM, Lee J, Song JY, Kim WJ, Cheong HJ. Disease burden of herpes zoster in Korea. J Clin Virol. 2010;47(4):325–9. doi:10.1016/j.jcv.2010.01.003.
- Johnson RW, Alvarez-Pasquin MJ, Bijl M, Franco E, Gaillat J, Clara JG, Labetoulle M, Michel JP, Naldi L, Sanmarti LS, et al. Herpes zoster epidemiology, management, and disease and economic burden in Europe: a multidisciplinary perspective. Ther Adv Vacc. 2015;3(4):109–20. doi:10.1177/2051013615599151.
- van Oorschot D, Vroling H, Bunge E, Diaz-Decaro J, Curran D, Yawn B. A systematic literature review of herpes zoster incidence worldwide. Hum Vaccin Immunother. 2021;17(6):1714–32. doi:10.1080/21645515.2020.1847582.
- Curran D, Schmidt-Ott R, Schutter U, Simon J, Anastassopoulou A, Matthews S. Impact of herpes zoster and postherpetic neuralgia on the quality of life of Germans aged 50 or above. BMC Infect Dis. 2018;18(1):496. doi:10.1186/s12879-018-3395-z.
- Gater A, Uhart M, McCool R, Préaud E. The humanistic, economic and societal burden of herpes zoster in Europe: a critical review. BMC Public Health. 2015;15:193. doi:10.1186/s12889-015-1514-y.
- Song H, Lee J, Lee M, Choi WS, Choi JH, Lee MS, Hashemi M, Rampakakis E, Kawai K, White R, et al. Burden of illness, quality of life, and healthcare utilization among patients with herpes zoster in South Korea: a prospective clinical-epidemiological study. Int J Infect Dis. 2014;20:23–30. doi:10.1016/j.ijid.2013.11.018.
- Weinke T, Edte A, Schmitt S, Lukas K. Impact of herpes zoster and post-herpetic neuralgia on patients’ quality of life: a patient-reported outcomes survey. Z Gesundh Wiss. 2010;18(4):367–74. doi:10.1007/s10389-010-0323-0.
- Imafuku S, Matsuki T, Mizukami A, Goto Y, de Souza S, Jégou C, Bianco V, Rosillon D, Ito C, Curran D, et al. Burden of herpes zoster in the Japanese population with immunocompromised/chronic disease conditions: results from a cohort study claims database from 2005–2014. Dermatol Ther (Heidelb). 2019;9(1):117–33. doi:10.1007/s13555-018-0268-8.
- Kim YJ, Lee CN, Lim CY, Jeon WS, Park YM. Population-based study of the epidemiology of herpes zoster in Korea. J Korean Med Sci. 2014;29(12):1706–1710. doi:10.3346/jkms.2014.29.12.1706.
- Melegaro A, Marziano V, Del Fava E, Poletti P, Tirani M, Rizzo C, Merler S. The impact of demographic changes, exogenous boosting and new vaccination policies on varicella and herpes zoster in Italy: a modelling and cost-effectiveness study. BMC Med. 2018;16(1):117. doi:10.1186/s12916-018-1094-7.
- Yin D, Van Oorschot D, Jiang N, Marijam A, Saha D, Wu Z, Tang H, Diaz-Decaro J, Watson P, Xie X, et al. A systematic literature review to assess the burden of herpes zoster disease in China. Expert Rev Anti Infect Ther. 2021;19(2):165–79. doi:10.1080/14787210.2020.1792290.
- Dooling KG, Patel M, Lee GM, Moore K, Belongia EA. Harpaz R. Recommendations of the advisory committee on immunization practices for use of herpes zoster vaccines. Morb Mortal Wkly Rep. 2018;67(3):103–8. doi:10.15585/mmwr.mm6703a5.
- Centers for Disease Control and Prevention. Clinical considerations for use of recombinant zoster vaccine (RZV, Shingrix) in immunocompromised adults aged ≥19 years. Centers For Disease Control And Prevention; 2022 Jan 20 [accessed 2023 Mar 31]. https://www.cdc.gov/shingles/vaccination/immunocompromised-adults.html.
- Dubé E, Laberge C, Guay M, Bramadat P, Roy R, Bettinger JA. Vaccine hesitancy. Hum Vaccin Immunother. 2013;9(8):1763–1773. doi:10.4161/hv.24657.
- Zheng H, Jiang S, Wu Q. Factors influencing COVID-19 vaccination intention: the roles of vaccine knowledge, vaccine risk perception, and doctor-patient communication. Patient Educ Couns. 2022;105(2):277–283. doi:10.1016/j.pec.2021.09.023.
- Kantar, LifePoints. Kantar; 2023 Nov 23 [accessed 2023 Nov 23]. https://www.kantar.com/campaigns/pf/lifepoints.
- Akakura K, Bolton D, Grillo V, Mermod N. Not all prostate cancer is the same – patient perceptions: an Asia-Pacific region study. BJU Int. 2020;126 (S1):38–45. doi:10.1111/bju.15129.
- Ferrante JM, Fyffe DC, Vega ML, Piasecki AK, Ohman-Strickland PA, Crabtree BF. Family physicians’ barriers to cancer screening in extremely obese patients. Obesity (Silver Spring). 2010;18(6):1153–9. doi:10.1038/oby.2009.481.
- McMullen S, Hess LM, Kim ES, Levy B, Mohamed M, Waterhouse D, Wozniak A, Goring S, Müller K, Muehlenbein C, et al. Treatment decisions for advanced non-squamous non-small cell lung cancer: patient and physician perspectives on maintenance therapy. Patient. 2019;12(2):223–233. doi:10.1007/s40271-018-0327-3.
- Guest G, Namey E, Chen M, Soundy A. A simple method to assess and report thematic saturation in qualitative research. PLos One. 2020;15(5):e0232076. doi:10.1371/journal.pone.0232076.
- Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6(1):42. doi:10.1186/1748-5908-6-42.
- Gleneagles Hospital. New generation shingles vaccination (Gleneagles Medical Clinic Central). Gleneagles Hospital; 2022 Nov 16 [accessed 2022 Nov 16]. https://gleneagles.hk/promotions/new-generation-shingles-vaccination-gleneagles-medical-clinic-central.
- Marina Medical. Shingles (also known as “Herpes zoster”) vaccination. Marina Medical; 2022 Nov 16 [accessed 2022 Nov 16]. https://marinamedical.hk/en/services/vaccination/shingles-vaccination.
- Centre for Health Protection. Chicken Pox. Department of health, the government of the Hong Kong special administrative region; 2019 Jul 5 [accessed 2022 Nov 16]. https://www.chp.gov.hk/en/healthtopics/content/24/15.html.
- Cheong K. 1 in 5 shingles patients had pain for more than a month; illness can cost more than $300. The Straits Times; 2014 Jun 16 [accessed 2022 Nov 16]. https://www.straitstimes.com/singapore/health/1-in-5-shingles-patients-had-pain-for-more-than-a-month-illness-can-cost-more-than.
- Chew J. 5 things to know about shingles. The Straits Times; 2022 Feb 18 [accessed 2022 Nov 16]. https://www.straitstimes.com/singapore/health/5-things-to-know-about-shingles.
- Health Hub. Herpes zoster (shingles). 2023 Sep 15 [accessed 2023 Nov 2]. https://www.healthhub.sg/a-z/diseases-and-conditions/141/herpes_zoster.
- Narae Medical Foundation. Shingles vaccination price and recommended target (should people who have already had shingles also get vaccinated) [Translated from Korean]. Narae Medical Center; 2021 Oct 3 [accessed 2022 Nov 16]. https://blog.naver.com/naraemedical01/222270561792.
- Chen C-C, Chung J. Shingles affecting young people more often: doctor. Taipei Times; 2019 Jan 1 [accessed 2022 Nov 16]. https://www.taipeitimes.com/News/taiwan/archives/2019/01/01/2003707150.
- Tri-Service General Hospital. Herpes zoster. Tri-service general hospital; 2023 Feb 11 [accessed 2023 Nov 2]. https://wwwv.tsgh.ndmctsgh.edu.tw/uniten/10016/28899.
- Paek E, Johnson R. Public awareness and knowledge of herpes zoster: results of a global survey. Gerontology. 2010;56(1):20–31. doi:10.1159/000240046.
- Lam AC, Chan MY, Chou HY, Ho SY, Li HL, Lo CY, Shek KF, To SY, Yam KK, Yeung I. A cross-sectional study of the knowledge, attitude, and practice of patients aged 50 years or above towards herpes zoster in an out-patient setting. Hong Kong Med J. 2017;23(4):365–73. doi:10.12809/hkmj165043.
- Al-Khalidi T, Genidy R, Almutawa M, Mustafa M, Adra S, Kanawati NE, Binashour T, Barqawi HJ. Knowledge, attitudes, and practices of the United Arab Emirates population towards herpes zoster vaccination: a cross-sectional study. Hum Vaccin Immunother. 2022;18(5):2073752. doi:10.1080/21645515.2022.2073752.
- Tsui E, Gillespie C, Perskin M, Zabar S, Wu M, Cohen EJ. Evaluating physician attitudes and practices regarding herpes zoster vaccination. Cornea. 2018;37(8):947–51. doi:10.1097/ico.0000000000001582.
- Valente N, Lupi S, Stefanati A, Cova M, Sulcaj N, Piccinni L, Gabutti G. Evaluation of the acceptability of a vaccine against herpes zoster in the over 50 years old: an Italian observational study. BMJ Open. 2016;6(10):e011539. doi:10.1136/bmjopen-2016-011539.
- Baalbaki NA, Fava JP, Ng M, Okorafor E, Nawaz A, Chiu W, Salim A, Cha R, Kilgore PE. A community-based survey to assess knowledge, attitudes, beliefs and practices regarding herpes zoster in an urban setting. Infect Dis Ther. 2019;8(4):687–94. doi:10.1007/s40121-019-00269-2.
- Casigliani V, Menicagli D, Fornili M, Lippi V, Chinelli A, Stacchini L, Arzilli G, Scardina G, Baglietto L, Lopalco P, et al. Vaccine hesitancy and cognitive biases: evidence for tailored communication with parents. Vaccine. 2022;11:100191. doi:10.1016/j.jvacx.2022.100191.
- Azarpanah H, Farhadloo M, Vahidov R, Pilote L. Vaccine hesitancy: evidence from an adverse events following immunization database, and the role of cognitive biases. BMC Public Health. 2021;21(1):1686. doi:10.1186/s12889-021-11745-1.
- Xu G, Xu S, Gong W, Dong S, Yu H. Low trend for VZV-Associated disease patients to visit neurologists. J Multidiscip Healthc. 2023;16:1379–1392. doi:10.2147/JMDH.S412398.