KEYWORDS:
1. Introduction
Diffuse large B-cell lymphoma (DLBCL) is an aggressive B-cell lymphoma that despite modern chemoimmunotherapy, 40% of those afflicted will relapse [Citation1]. Accordingly, chimeric antigen receptor T-cells (CAR-T) therapy for refractory/relapsed DLBCL (R/R-DLBCL) has provided an opportunity for sustained remission [Citation2]. However, for those that relapse following CAR-T therapy, there is a paucity of literature indicating factors that could provide predictive information regarding relapse as well as an initial and sequential assessment that describes tumor biology.
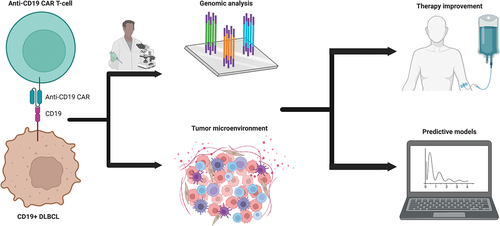
There is a strong need for pathologists to be involved beyond the microscope in the initial, and subsequent, evaluation of DLBCL in the setting of CAR-T therapy. Herein, an evaluation of molecular diagnostics and advanced laboratory techniques that can be utilized in the evaluation of DLBCL at the time of diagnosis and before and after administration of CAR-T will be explored (). Additionally, the role that pathology can serve in the application and assessment of these techniques in the future will be discussed. Lastly, an expert opinion will be rendered that serves as a call to action with the understanding of challenges in the future.
Figure 1. Workflow of engagement for the pathologist in the context of CAR-T therapy for DLBCL. Burgeoning areas of research for pathologists to be engaged include genomic analysis and qualitative assessment of the tumor microenvironment in DLBCL. This will facilitate development of predictive models for those potentially undergoing CAR-T therapy administration as well as improving the efficacy of the modern therapies. Created with BioRender.com.
2. Applications of comprehensive genomic analysis in the assessment of DLBCL and CAR-T therapy
One area that has garnered much attention is the genomic classification of DLBCL, which serves as a foundation for the genetic mechanisms that may predict aggressiveness of disease as it pertains to CAR-T therapy. Although targeted next-generation sequencing (NGS) is becoming more common place, especially for R/R-DLBCL, there are other advanced sequencing modalities that can be applied for a more comprehensive interrogation of genomic alterations that may contribute to CAR-T resistance.
One such technique is the use of whole exome sequencing (WES), which provides a thorough evaluation of coding genomic variants. Chapuy and colleagues utilized this method for the assessment and designation of clusters within DLBCL [Citation3]. Using WES, a holistic approach was pursued in studying DLBCL for single nucleotide variants, insertions/deletions, somatic copy number alterations, and structural variants (SV). A combination of informatic pipelines were used, such as MutSigCV, CLUMPS, and GISTIC2.0, which illustrates the multi-modal approach necessary to disentangle the complexity of these aggressive lymphomas.
In regard to the identified clusters, distinct phenotypic and survival differences were observed among DLBCL groups with some being implicated as more clinically aggressive or more likely to not respond to CAR-T. In brief, clusters of most interest would be those belonging to cluster 2 (characterized by TP53 alterations) and cluster 3 (characterized by BCL2 SV). As illustrated by Laurent et al., TP53 alterations were identified as being one of the most frequent genomic aberrations in pre- and post-CAR-T DLBCL samples that underwent targeted NGS [Citation4]. Such findings could codify TP53 as a predictor of resistance to CAR-T therapy. Additionally, BCL2 SV are identified in 15–20% of DLBCL cases and have been previously associated with CAR-T therapy resistance due to anti-apoptotic mechanisms [Citation5]. The knowledge of BCL2 SV has led to the possibility of modulating CAR-T to better target this group of DLBCL. Overall, comprehensive genomic analysis using advanced sequencing techniques in DLBCL preceding administration of CAR-T provides context for understanding mechanisms of disease as well as potentially predicting those that will be more resistant to CAR-T therapy. Furthermore, for those that relapse, evaluating the resultant genomic alterations may provide refinement of CAR-T manufacturing in the future and provide optimal outcomes.
3. Tumor microenvironment and its role in DLBCL in the setting of CAR-T therapy
Using single-cell RNA sequencing (RNA-seq), Ye and colleagues demonstrated the inter- and intratumoral heterogeneity observed in DLBCL, ultimately leading to the identification of unique expression profiles within the tumor microenvironment (TME) [Citation6]. This analysis undertook a multifaceted approach to elucidating the underpinnings of the TME and its cell–cell interactions by utilizing a genomic and transcriptomic studies, such as whole-genome sequencing (WGS) and RNA-seq. Although more conventional informatic pipelines may be used for WGS, single-cell RNA-seq requires a sophisticated approach to illustrate not only that the expression profiles cluster appropriately but they are assessing the cells of interest. This can be illustrated by assessing genes associated with a particular lineage and by applying a neural network along with principal component analysis, creating two-dimensional visualization by uniform manifold approximation and projection. This elegant approach allows for a robust and comprehensive analysis of the TME on a single-cell level that can be used to illustrate the heterogeneity of DLBCL.
In a more recent analysis by Wright et al., a unique approach to assessing the TME defined multiple microenvironments in relation to certain cellular, spatial, and functional elements as assessed by secondary ion mass spectrometry (MIBIscope, Menlo Park, CA) [Citation7]. Such TME can be deficient in immune cells or enriched for dendritic cells or macrophages. This finding has been supported in a recent study by Sworder et al., in which samples from patients following relapse after CAR-T therapy administration revealed enrichment for inflammatory, interferon-gamma (IFN-γ), and transforming growth factor-beta (TGF-β) signaling signatures when compared to those that responded to CAR-T [Citation8]. Additional findings demonstrated the role of intratumoral CAR-T DNA as a biomarker in that persistence of high levels of CAR-T DNA modulated the TME, particularly in relation to T-regulatory cells. As such, examination of the TME can provide clinically significant information at diagnosis as well as for patients that fail traditional chemoimmunotherapy and prediction of CAR-T therapy success.
4. Clinical predictors of relapse of DLBCL following CAR-T therapy
From the inception of using CAR-T therapy for R/R-DLBCL, there have been many challenges in predicting outcomes. Two pivotal trials (ZUMA-1 and JULIET) demonstrated the significant heterogeneity in clinical outcomes due to a difference in patient parameters and bridging therapy with ZUMA-1 using only glucocorticoids after autologous stem cell transplant as opposed to JULIET that selected for those with had a high tumor burden and bridging chemotherapy [Citation9,Citation10]. Additional factors that have provided insight into unfavorable outcomes include prior chemotherapy regimens, such as those that received more than three cycles of bendamustine with less than a three-month washout period as having a high rate of failure for CAR-T manufacturing [Citation11]. As the likelihood of relapse following CAR-T is multifactorial, future studies are needed to develop a clinicopathologic model that may predict success or the need to utilize an alternative CAR-T manufacturing strategy.
5. The pathologist’s role in the evaluation of utilizing CAR-T for DLBCL and other malignancies
In the modern era of precision medicine, the pathologist serves a pivotal role in diagnostics, discovery of biomarkers, and contribution to potential predictive factors that may identify those patients that will need alternative therapies. This has been particularly true in R/R-DLBCL and CAR-T therapy as new modalities for assessment of the genomic profile and TME have led to a better understanding of the molecular basis for DLBCL and its potential resistance to CAR-T therapy. In the author’s professional experience, an unpublished case of an adult female that had R/R-DLBCL that never achieved complete remission underwent CAR-T therapy with curative intent. However, shortly after administration of CAR-T, the patient unfortunately passed away. Upon retrospective targeted NGS, the preceding DLBCL had a BCL2 SV and a missense mutation in TP53 with concomitant deletion of the TP53 locus on chromosome 17p13. In comparison of the refractory DLBCL following CAR-T, the tumor progressed with loss of CD19 expression and acquisition of a PIK3R1, which is identical to that seen by Laurent et al. Utilizing this information, and what is now known among the genomic features of DLBCL that relapses or progresses following CAR-T therapy, this patient may have not been a suitable candidate for CAR-T. With the development and implementation of newer techniques, the pathologist will continue to serve a significant role in the management of DLBCL that may be amenable to CAR-T therapy or better suited for alternative therapeutic strategies.
6. Expert opinion
In the author’s experience, the laboratory has served a significant role for diagnostics, prognostics, and theranostics. For DLBCL, the paradigm has shifted from determining cell-of-origin [Citation12] to a more sophisticated approach for evaluating DLBCL [Citation13], particularly for those that have become refractory or relapsed following conventional chemoimmunotherapy. In the era of advanced diagnostics and cutting-edge treatments, it behooves the pathologist to have a synergistic relationship with researchers and oncologists. As pathologists oftentimes have the most intimate relationship with disease and direct access to techniques that can elucidate mechanisms of disease, it falls on the shoulders of the pathologist to push the boundaries, collaborate, and bring modern oncology to a new era. Although a great deal has been accomplished, sequential analysis of DLBCL following chemoimmunotherapy and CAR-T therapy has not been performed to the best of the author’s knowledge. DLBCL is not a static malignancy and there is both temporal and spatial heterogeneity at diagnosis and relapse [Citation14]. Most tissue-based studies have focused on a single or a minimal set of timepoints and not the evolution of disease and this is where the greatest impact lies.
There are, of course, challenges in implementing these advanced technologies and studies. First, the most pressing matter is capital investment in equipment and laboratory personnel. Additionally, with the advent of new technologies comes the generation of a tremendous amount of complex data, which will need robust informatic pipelines and visualization interfaces to fully capitalize on the technique. Lastly, the time from bench-to-bedside also serves as a rate-limiting step. As many of the previously described technologies are not routinely utilized or performed in a clinically validated space, the need for an expeditious pace from the research laboratory to the clinic is immediate. To overcome these barriers, a thorough assessment of the current precision medicine landscape is necessary. This entails perhaps a paradigm shift in DLBCL treatment from only using these technologies after multiple lines of therapy have failed but perhaps assessing the disease at the beginning to better understand what therapies may be appropriate and to serve as a baseline for the disease itself should it relapse or be refractory.
The ultimate goal would be to develop a model based on the aforementioned techniques that may not only predict response to a variety of therapies but provide a well-curated database in which further techniques and therapies could draw from for exploration. The future is bright for those engaged in the evaluation, treatment, and research of DLBCL, but there is much to be done to further expand the armamentarium of those involved.
Declaration of interest
PD Michaels receives research funding from Bionano Genomics, San Diego, CA. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or material discussed in the manuscript apart from those disclosed.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Author contributions
PD Michaels conceptually designed, reviewed the literature, wrote, and revised the manuscript.
Additional information
Funding
References
- Pasqualucci L, Trifonov V, Fabbri G, et al. Analysis of the coding genome of diffuse large B-cell lymphoma. Nat Genet. 2011 Jul 31;43(9):830–837. doi: 10.1038/ng.892. PMID: 21804550; PMCID: PMC3297422.
- Sengsayadeth S, Savani BN, Oluwole O, et al. Overview of approved CAR-T therapies, ongoing clinical trials, and its impact on clinical practice. EJHaem. 2021 Nov 24;3(Suppl 1):6–10. doi: 10.1002/jha2.338. PMID: 35844299; PMCID: PMC9175669.
- Chapuy B, Stewart C, Dunford AJ, et al. Molecular subtypes of diffuse large B cell lymphoma are associated with distinct pathogenic mechanisms and outcomes. Nat Med. 2018 May;24(5):679–690. doi: 10.1038/s41591-018-0016-8. PMID: 29713087; PMCID: PMC6613387.
- Laurent C, Syrykh C, Hamon M, et al. Resistance of B-Cell lymphomas to car t-cell therapy is associated with genomic tumor changes which can result in transdifferentiation. Am J Surg Pathol. 2022 Jun 1;46(6):742–753. doi: 10.1097/PAS.0000000000001834. Epub 2021 Nov 18. PMID: 34799485
- Lee YG, Guruprasad P, Ghilardi G, et al. Modulation of BCL-2 in both t cells and tumor cells to enhance chimeric antigen receptor t-cell immunotherapy against cancer. Cancer Discov. 2022 Oct 5;12(10): 2372–2391. doi: 10.1158/2159-8290.CD-21-1026. PMID: 35904479; PMCID: PMC9547936.
- Ye X, Wang L, Nie M, et al. A single-cell atlas of diffuse large B cell lymphoma. Cell Rep. 2022 Apr 19;39(3):110713. doi: 10.1016/j.celrep.2022.110713. PMID: 35443163
- Wright KT, Weirather JL, Jiang S, et al. Diffuse large B-cell lymphomas have spatially defined, tumor immune microenvironments revealed by high-parameter imaging. Blood Adv. 2023 Aug 22;7(16):4633–4646. doi: 10.1182/bloodadvances.2023009813. PMID: 37196647; PMCID: PMC10448427.
- Sworder BJ, Kurtz DM, Alig SK, et al. Determinants of resistance to engineered T cell therapies targeting CD19 in large B cell lymphomas. Cancer Cell. 2023 Jan 9;41(1):210–225.e5. doi: 10.1016/j.ccell.2022.12.005. Epub 2022 Dec 29. PMID: 36584673; PMCID: PMC10010070.
- Neelapu SS, Locke FL, Bartlett NL, et al. Axicabtagene Ciloleucel CAR T-Cell Therapy in Refractory Large B-Cell Lymphoma. N Engl J Med. 2017 Dec 28;377(26):2531–2544. doi: 10.1056/NEJMoa1707447. Epub 2017 Dec 10. PMID: 29226797; PMCID: PMC5882485.
- Schuster SJ, Bishop MR, Tam CS, et al. JULIET Investigators. Tisagenlecleucel in adult relapsed or refractory diffuse large b-cell lymphoma. N Engl J Med. 2019 Jan 3;380(1):45–56. doi: 10.1056/NEJMoa1804980. Epub 2018 Dec 1. PMID: 30501490.
- Jo T, Yoshihara S, Okuyama Y, et al. Risk factors for CAR-T cell manufacturing failure among DLBCL patients: a nationwide survey in Japan. Br J Haematol. 2023 Jul;202(2):256–266. doi: 10.1111/bjh.18831. Epub 2023 Apr 25. PMID: 37096915.
- Alizadeh AA, Eisen MB, Davis RE, et al. Distinct types of diffuse large B-cell lymphoma identified by gene expression profiling. Nature. 2000 Feb 3;403(6769):503–511. doi: 10.1038/35000501. PMID: 10676951.
- Özçalımlı A, Erdoğdu İH, Turgutkaya A, et al. The evaluation of gene mutation profiles by next-generation sequencing in diffuse large B-cell lymphoma. Int J Lab Hematol. 2023 Jun;45(3):310–316. doi: 10.1111/ijlh.14012. Epub 2022 Dec 28. PMID: 36576110.
- Zhang J, Grubor V, Love CL, et al. Genetic heterogeneity of diffuse large B-cell lymphoma. Proc Natl Acad Sci USA. 2013 Jan 22;110(4): 1398–1403. doi: 10.1073/pnas.1205299110. Epub 2013 Jan 4. PMID: 23292937; PMCID: PMC3557051.

