Abstract
Diquat is a nonselective bipyridylium herbicide and pre-harvest desiccant that is toxic to humans when ingested. However, the outcome of diquat poisoning during pregnancy has not been well described. A 32-year-old woman at 22 weeks of pregnancy was admitted to our emergency department after consuming 100 mL of diquat (200 g/L). She received emergency gastric lavage 1 h after consumption at an outside facility and was conscious with stable vital signs upon admission at our hospital. She experienced accidental abortion the following day, and the stillbirth was delivered in full. She quickly experienced multiple organ failure including kidney, liver, and central nervous system. She was then transferred to the intensive care unit and received tracheal intubation with mechanical ventilation, blood purification, toxin clearance, as well as other supporting therapies. The patient recovered after receiving treatment and was successfully discharged with no long-term sequela identified during the follow-up. Diquat has a large distribution of volume. Diquat poisoning produced stillbirth and multiple organ failure in a pregnant woman. Severe cases cause multiple organ failure. Reducing absorption, improving the excretion of poison, stabilizing organ function, and supporting care are the main treatments.
Introduction
Paraquat is banned in many developing countries due to its toxicity and as its substitute, the use of diquat has been rapidly increased. Consequently, increasing cases of diquat poisoning have been documented. The first case of diquat poisoning was reported in 1969, and the patient experienced full recovery after accidental intake of diquat [Citation1]. The most common form of diquat poisoning is by oral intake, though toxic exposures to the skin, airways, and vagina have also been reported [Citation2–4]. Diquat exposure often leads to immediate dose-dependent local and systemic symptoms. Multiple organ failure, including kidney, liver, digestive system, heart, and central nervous system, frequently happens in severe cases. We present a case of a pregnant woman who consumed a large volume of diquat and experienced life-threatening symptoms.
Case report
A 32-year-old female with 22 weeks of pregnancy reportedly ingested 100 mL of diquat (20 g/100 mL) in a suicide attempt. She experienced nausea and vomiting shortly after ingesting the substance. One hour after consumption, the patient received gastric lavage at a community hospital before transport by ambulance to our emergency department (ED). She arrived in our ED 12 h after ingestion. She was fully conscious with normal blood pressure and heart rate on arrival. She complained of upper abdomen and oropharynx pain. Examination of the oropharynx revealed erythema, but no corrosive lesion was identified. She had mild upper abdominal discomfort during the abdominal examination. She had no other abnormalities on physical examination. Chest computed tomography(CT) was normal in the ED. She was then transferred to our toxicology department to receive further treatment. The patient was in good health before poisoning and had no history of drug or alcohol misuse.
Analysis of serum and urinary obtained on hospital day 1 confirmed the presence of diquat with no paraquat. The diquat concentrations of serum and urine were >1.0 and >2.0 µg/mL, respectively, measured qualitatively by liquid chromatography-tandem mass spectrometry (LC-MS/MS). She underwent hemodialysis (HD) with hemoperfusion (HP) for both supportive care and toxin removal and for 2 h. Montmorillonite (to protect digestive mucosa) and activated charcoal were given orally to reduce residual toxin absorption in the digestive tract. She had only 400 mL urine output for 24 h despite the use of furosemide intravenously. Her alanine aminotransferase (ALT) activity increased to 70.5 U/L and creatinine concentration increased to 2.6 mg/dL two days after intoxication.
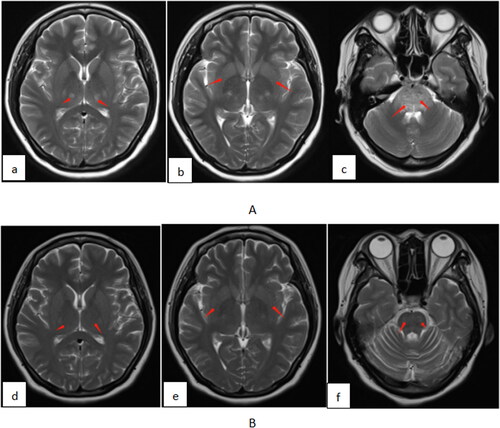
Obstetrical ultrasound revealed fetal demise at the estimated gestational age of 23 weeks. Then the patient experienced increasing oropharyngeal pain and vaginal hemorrhage on the third day. She received oxytocin to induce abortion. The placenta and fetus were fully delivered a few hours later. An autopsy on the fetus was not performed. In the meantime, her vital signs remained normal. She had no urine, and her creatinine concentration was 4.5 mg/dL. She received additional HP and HD for 2 h and slow continuous ultrafiltration (SCUF) of 1500 mL due to worsening renal failure. She appeared unfocused and drowsy. The patient then complained of feeling lightheaded and having blurry vision. Brain magnetic resonance imaging (MRI) revealed symmetrical aberrant signals in the thalamus, basal ganglia, and brainstem, with cytotoxic brain edema in the brainstem, resembling signs of toxic encephalopathy (). She again underwent HP and HD for 2 h, as well as 1600 mL of liquid ultrafiltration to treat her anuria. She was transferred to the ICU due to a continuous decline of awareness on the fourth day afternoon.
Figure 1. Brain MRI shows signs of toxic encephalopathy (A). Bilateral thalamus, basal ganglia, and brainstem edema almost improved on day 44 (B). thalamus, day 3 (a); basal ganglia, day 3 (b); brainstem edema, day 3 (c); thalamus, day 44 (d); basal ganglia, day 44 (e); brainstem edema, day 44 (f).
She became agitated after admission to the ICU, but her vital signs remained normal with SpO2 of 98% on nasal cannula 3 L/min oxygen. Her oral mucosa and tongue had widespread burns. She had a positive Babinski sign on her left foot. Over the next few hours, the patient’s condition deteriorated rapidly. Chest radiography suggested pulmonary edema and right upper lobe infiltrate (). She developed worsening shortness of breath and hypoxemia and was intubated for mechanical ventilation.
Figure 2. Chest radiography showed pulmonary edema and right upper lobe infiltrate on admission (A). Repeat chest radiography showed reduced pulmonary edema and resolved infiltrate on day 7 (B).
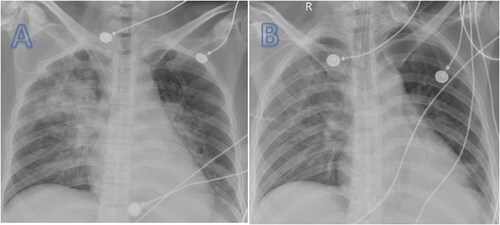
She excreted black stool, and her hemoglobin was decreased from 95 to 62 g/L. She was kept nil per os (NPO), and she received a proton pump inhibitor, antibiotics, methylprednisolone, and infusion of 2 units of red blood cells. On day 7, repeat chest radiography reduced pulmonary edema and resolved infiltrate ().
Hemoperfusion was performed for 3 h simultaneously with continuous venovenous hemodiafiltration (CVVHDF) on day 5. The patient’s oliguria persisted for 13 days during hospitalization, and she underwent CVVHDF for 7–9 h daily. She was withdrawn from CVVHDF until the urine output reached 2000 mL on day 20. Her creatinine concentration is 1.1 mg/dL on day 30.
The patient’s consciousness recovered gradually, and she was extubated on day 21. Brain MRI and chest CT showed significant improvement on day 23, and the patient was transferred from ICU to toxicology department. No obvious lesions were identified in the chest CT and brain MRI on day 44 (). At the same time, ultrasound showed that the uterus returns to normal. She was discharged on day 45. In telephone follow-up 6 months after discharge she reported in full recovery with no sequelae.
Discussion
Diquat can react with molecular oxygen, generates redox products, which can cause cell death, resulting in tissue damage and multiple organ symptoms [Citation5,Citation6]. Animal studies have shown that diquat has reproductive and developmental toxicity [Citation7]. A previous case report described a patient with 15 weeks of pregnancy who consumed ∼100–150 mL of diquat and experienced incomplete abortion and died [Citation8]. Fortunately, even though our patient reported ingesting higher-than lethal amount of diquat and experienced rapid miscarriage, she survived the treatment and fully recovered. However, due to the medical ethics, an autopsy on the fetus was not performed, and we could not get the concentration.
The patient’s condition usually deteriorates 3–5 days after diquat poisoning [Citation9]. The kidney is one of the target organs of diquat poisoning. Renal biopsy findings include lipid degeneration, acute tubular injury, and interstitial injury [Citation10,Citation11]. Patients with diquat poisoning have hypovolemia because of emesis, diarrhea, and decreased oral intake. It is unclear whether oliguria and anuria result from direct renal toxicity of diquat or from severe volume depletion [Citation4,Citation12–15]. Diquat concentrates in urine in animals [Citation6] and humans [Citation16]. Renal replacement therapy was performed for supportive care and toxin removal. HP decreased the serum diquat concentrations [Citation17]. Multiple HP within a short time can increase the elimination of toxins and enhance the therapeutic effect. A case report described a patient who consumed 36 g diquat and survived in good condition with gastric protection, HD, and HP [Citation10].
Fatal cases typically have central nervous system (CNS) pathology, especially in the brainstem region [Citation14,Citation15,Citation17,Citation18]. In our case, the patient showed blurred vision and lethargy, and MRI and CT confirmed cerebral edema. Diquat can penetrate the blood-brain barrier and can be detected in the cerebrospinal fluid (CSF). It reveals a correlation between the concentration of diquat in the CSF and both the intracranial pressure (ICP) and the severity of cerebral edema. As the concentration of diquat in CSF decreased, the patient recovered gradually [Citation19].
Toxic effects of diquat also include damage of the lung with pulmonary exudation, consolidation, and respiratory failure [Citation3,Citation9,Citation10,Citation13]. Our patient had a similar situation. Elevation in ALT indicates liver damage. Severe liver dysfunction often occurs in fatal cases [Citation9].
Conclusion
There is no specific antidote for diquat poisoning. Early gastric lavage and administration of activated charcoal may reduce diquat absorption. Because of corrosive mucosal damage, it is more important to pay attention to gastrointestinal perforation. Hemoperfusion enhances the elimination of poison. Acute renal failure may require hemofiltration or hemodialysis. Be wary of encephalopathy. Clinicians should monitor biochemical markers of organ functions and provide supportive care.
Clinical trial registration
Not applicable.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Oreopoulos DG, McEvoy J. Diquat poisoning. Postgrad Med J. 1969;45(527):1–4. doi: 10.1136/pgmj.45.527.635.
- Ronnen M, Klin B, Suster S. Mixed diquat/paraquat-induced burns. Int J Dermatol. 1995;34(1):23–25. doi: 10.1111/j.1365-4362.1995.tb04371.x.
- Wood TE, Edgar H, Salcedo J. Recovery from inhalation of diquat aerosol. Chest. 1976;70(6):774–775. doi: 10.1378/chest.70.6.774.
- Rudez J, Sepcić K, Sepcić J. Vaginally applied diquat intoxication. J Toxicol Clin Toxicol. 1999;37(7):877–879. doi: 10.1081/clt-100102470.
- Stubbs J. A new herbicide. Outlook Agric. 1958;2(2):64–68. doi: 10.1177/003072705800200203.
- Litchfield MH, Daniel JW, Longshaw S. The tissue distribution of the bipyridylium herbicides diquat and paraquat in rats and mice. Toxicology. 1973;1(2):155–165. doi: 10.1016/0300-483x(73)90029-2.
- Zhang JQ, Gao BW, Wang J, et al. Chronic exposure to diquat causes reproductive toxicity in female mice. PLOS One. 2016;11(1):e0147075. doi: 10.1371/journal.pone.0147075.
- Yu G, Cui S, Jian T, et al. Diquat poisoning in a pregnant woman resulting in a miscarriage and maternal death. Clin Toxicol. 2021;59(12):1275–1277. doi: 10.1080/15563650.2021.1905164.
- Zhou JN, Lu YQ. Lethal diquat poisoning manifests as acute central nervous system injury and circulatory failure: a retrospective cohort study of 50 cases. EClinicalMedicine. 2022;52:101609. doi: 10.1016/j.eclinm.2022.101609.
- Xia Z, Liu W, Liu L. Clinical and pathological characteristics of diquat poisoning-related acute kidney injury. Ren Fail. 2023;45(2):2283590. doi: 10.1080/0886022X.2023.2283590.
- Zeng DH, Chen XH, Li Y, et al. Clinical and pathological characteristics of acute kidney injury caused by diquat poisoning. Clin Toxicol. 2023;61(9):705–708. doi: 10.1080/15563650.2023.2262113.
- Kibby T, Ring DS. Nail injury and diquat exposure. Dermatitis. 2012;23(4):176–178. doi: 10.1097/DER.0b013e318262ca83.
- Tanen DA, Curry SC, Laney RF. Renal failure and corrosive airway and gastrointestinal injury after ingestion of diluted diquat solution. Ann Emerg Med. 1999;34(4 Pt 1):542–545. doi: 10.1016/s0196-0644(99)80059-6.
- Saeed SAM, Wilks MF, Coupe M. Acute diquat poisoning with intracerebral bleeding. Postgrad Med J. 2001;77(907):329–332. doi: 10.1136/pmj.77.907.329.
- Xing J, Chu Z, Han D, et al. Lethal diquat poisoning manifesting as Central pontine myelinolysis and acute kidney injury: a case report and literature review. J Int Med Res. 2020;48(7):300060520943824. doi: 10.1177/0300060520943824.
- McCarthy LG, Speth CP. Diquat intoxication. Ann Emerg Med. 1983;12(6):394–396. doi: 10.1016/s0196-0644(83)80474-0.
- Powell D, Pond SM, Allen TB, et al. Hemoperfusion in a child who ingested diquat and died from pontine infarction and hemorrhage. J Toxicol Clin Toxicol. 1983;20(5):405–420. doi: 10.3109/15563658308990609.
- Sechi GP, Agnetti V, Piredda M, et al. Acute and persistent parkinsonism after use of diquat. Neurology. 1992;42(1):261–263. doi: 10.1212/wnl.42.1.261.
- Wang P, Lin LY, Lu YQ. Mid-to-late stage diquat accumulation in the central nervous system: a severe case of oral poisoning. Am J Emerg Med. 2024;75:198.e1–198.e5. doi: 10.1016/j.ajem.2023.10.005.

