Abstract
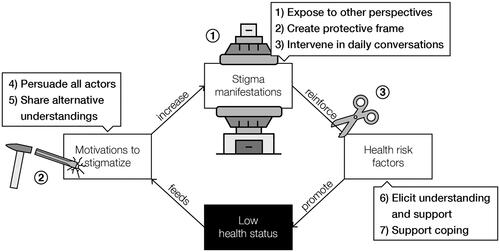
In this article we describe how designers can apply storytelling to reduce health-related stigmas. Stigma is a pervasive problem for people with illnesses, such as obesity, and it can persistently hinder coping, treatment, recovery, and prevention. Reducing health-related stigma is complex because it is multi-layered and self-perpetuating, leading to intertwined vicious circles. Interactive storytelling environments can break these vicious circles by delimiting the narrative freedom of stigma actors. We theoretically explain the potential of interactive storytelling environments to reduce stigma through the following seven functions: 1) expose participants to other perspectives, 2) provide a protective frame, 3) intervene in daily conversations, 4) persuade all stigma actors, 5) exchange alternative understandings, 6) elicit understanding and support for stigma victims, and 7) support stigma victims to cope with stigmatization. We elaborate on these functions through a demonstration of an interactive storytelling environment against weight stigma. In conclusion, this article is a call on designers for health and wellbeing, scientists, and practitioners from various disciplines to be sensitive to the pervasiveness of stigma and to collaboratively create destigmatizing storytelling environments.
Introduction
Stigma is a pervasive problem for people with illnesses (Weiss, Ramakrishna, and Somma Citation2006), such as HIV/AIDS, skin diseases, depression, and obesity. Victims of health-related stigmatization give testimonies of feeling and being bullied, secluded, and violated. As a result, they continuously feel pressure to act normal, make a good impression, and provide explanations for supposed shortcomings (Goffman Citation1963). This places a huge burden on people and it can lead to negative physical and psychological health outcomes (Pachankis Citation2007). At the same time, perpetrators of stigmatization are often not fully aware of their stigmatizing behaviour and its negative effects. They ‘just want the best for someone’, make assumptions about someone’s condition, and are sometimes just ill-informed about a disease.
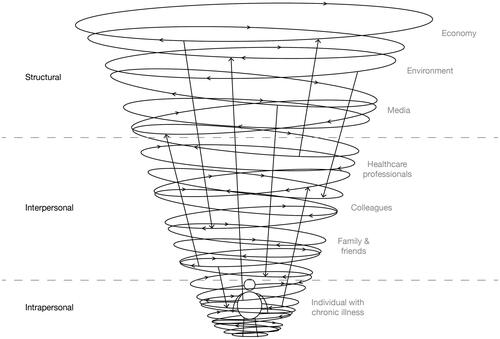
Health-related stigmatization is a complex phenomenon involving many actors, motivations, and effects that negatively impact the health of stigma victims (Quinn and Chaudoir Citation2009; Van Beugen et al. Citation2017). Health-related stigma not only manifests itself in interpersonal interaction. It also manifests itself internally (intrapersonal) and structurally. Stigmatized individuals themselves often internalize parts of the biases and stereotypes leading to self-stigma (Richman and Lattanner Citation2014). Structural health-related stigma can be found in health insurance policies that exclude certain illnesses, reduced chances on the labour market, and health inequalities among populations (Hatzenbuehler Citation2016). Hence, health-related stigma can persistently manifest itself in nearly all facets of people’s lives and this negatively influences the health of stigma victims and can lead to health inequalities (Pascoe and Smart Richman Citation2009; Paradies, Luiz Bastos, and Priest Citation2016). Some argue that stigma also serves a purpose as a motivator for healthy behaviour change (Bayer Citation2008), yet health-related stigma does more harm than good and should thus be reduced.
Unfortunately, reducing health-related stigma is a complicated endeavour. Stigmas are generally very persistent because motivations to stigmatize are often deeply ingrained in people’s norms and beliefs, and in societal structures (Scambler Citation2009). The multifaceted and multi-layered nature of stigmatization (e.g. labelling, distancing, discriminating on an intrapersonal, interpersonal, structural level) makes a centralized top-down approach, such as advertisement campaigns, ineffective in the long term (Link and Phelan Citation2001). Additionally, stigma is often subject to psychological mechanisms that perpetuate stigmatizing attitudes and behaviours (Brewis Citation2014).
We propose storytelling to be a driving force against stigmatization because, on a structural level, health-related stigmas can be characterized as a cultural web of narratives (Meretoja Citation2017) and master narratives have been widely used to uncover societal oppressive structures against marginalized communities (Syed Citation2015). Moreover, on the intrapersonal level, narratives are strongly related to personal identity formation by which individuals position themselves in conversations (Bamberg Citation2011).
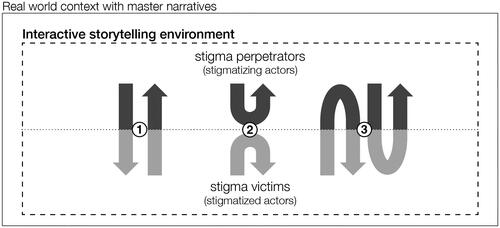
Rather than intervening on single narratives, as in conventional campaigns against stigma, we suggest targeting the exchange of narratives, i.e. the storytelling. Stigma actors may be invited to create and feel part of destigmatizing stories by safe and unprejudiced social environments with confined degrees of freedom in telling stories and interacting with them. As visualized in , ‘interactive storytelling environments’ with a designed conceptual storytelling space, i.e. the set of all possible stories that participants can tell, may provoke stigma perpetrators and stigma victims to 1) appropriate their stories for the other group, 2) reflect on one’s own stories, and 3) adapt one’s stories in collaboration with the other group.
Figure 1. We propose to design interactive storytelling environment that shape the conceptual storytelling space of stigma actors to motivate them to 1) appropriate, 2) reflect on, and 3) co-create their stories.
In this article, we explore the potential of designing interactive storytelling environments to reduce health-related stigmatization by identifying destigmatizing functions of story content and story interactions and applying them to an intervention. In the first half of the article, we review the literature on stigma, with weight stigma as an exemplary case, to better understand its pervasive and self-perpetuating nature. In the second half of the article, we define a research agenda about designing destigmatizing functions of storytelling and describe a serious game against weight stigma to demonstrate the destigmatizing potential of interactive storytelling environments.
Stigma as a psychosocial phenomenon
Stigma is a visible or invisible mark of disapproval, allowing ‘insiders’ to identify and disassociate from ‘outsiders’ (Falk Citation2001). Goffman (Citation1963) describes the day-to-day experiences of outsiders as ‘managing impressions’ and ‘managing information’. For example, people that are stigmatized by their body size particularly recall managing impressions, such as making sure to dress nicely and not eating in public (Lewis et al. Citation2011). Link and Phelan (Citation2001) define stigma as a co-occurrence of labelling, stereotyping, separating, status loss, and discrimination in a power situation that allows these processes to unfold. The power difference between a stigmatized group and the group that stigmatizes is important to point out, because stigmas are persistent when they exist within groups that have the power to find new strategies to maintain the disadvantageous status of the stigmatized group. As long as motivations for stigmatization prevail in dominant groups, combatting mediating processes is ineffective (Hatzenbuehler, Phelan, and Link Citation2013).
Stigmatization should be reviewed on an intrapersonal, interpersonal, and structural level to fully understand it (Cook et al. Citation2014). Health-related stigma that manifests itself in interpersonal interaction is often easy to identify, such as bullying, negative commenting, or excluding (Hebl and Dovidio Citation2005). Yet for people with a chronic illness, intrapersonal or self-stigma is particularly salient (Durso and Latner Citation2008; Kranke et al. Citation2011). They often go through a process of understanding the causes of their illness and thus regularly fail in their attempts to recover or manage it. This can lead to reduced self-esteem and self-worth and in effect self-stigma in the form of inhibiting or isolating oneself (Corrigan, Larson, and Rüsch Citation2009).
Structural stigmatization can be found in socioeconomic conditions, cultural norms, and institutional policies (e.g. Hatzenbuehler and Link Citation2014). For example, people with obesity have on average lower incomes (Giskes et al. Citation2010) and weight loss services are often not reimbursed by the health insurance (Puhl and Heuer Citation2009). Stangl et al. (Citation2019) explain that such structural discrimination on health conditions can be found in organizations, communities, and public spaces. Thus, in this article, ‘stigma actor’ refers to people that are the victim or perpetrator of stigmatization as well as non-human actors through which health-related stigmas are expressed, such as health insurance systems, cultural master narratives, and the media. Moreover, our use of ‘victim’ or ‘perpetrator’ in this article refers to the role of a stigma actor in a particular stigmatizing situation, rather than being or feeling a victim or perpetrator in general.
To get a more concrete understanding of the multiple levels and actors of health-related stigma, we dive deeper into the manifestations, causes, and effects of weight stigma. Weight stigma is a valuable case because many recent studies show direct negative health consequences of stigmatization, yet means to reduce weight stigma are scarce (Pearl Citation2018). Such a comprehensive understanding of health-related stigmas allows us to define mechanisms that could erase it.
Weight stigma
People with obesity are stigmatized in many ways and settings. They are called ‘lazy, unmotivated, lacking in self-discipline, less competent, non-compliant, and sloppy’ (Puhl and Heuer Citation2009, 941) in employment, healthcare, education, interpersonal relationships, and media settings. As obesity is visible, these stereotypes easily lead to separation and discrimination in the form of gazing, others making decisions for you, negative comments, being ignored or rejected, and bullying or even physical violation (De Brún et al. Citation2014; Lewis et al. Citation2011). Next to labelling by others, many people with obesity have the same anti-fat attitudes as slender people (Crandall Citation1994). This self-stigma is expressed in the form of a negative body image (Harriger and Thompson Citation2012), feeling guilty or weak (Lillis et al. Citation2010), distancing from others that have obesity (Durso and Latner Citation2008), and reduced motivation in weight loss efforts (Corrigan, Larson, and Rüsch Citation2009; Hunger et al. Citation2015).
Losing weight is complex due to the wide variety of causes for weight gain. To some extent, it is caused by unhealthy nutrition and too little physical activity, yet a substantial part of the variation in body weight is determined by other determinants, such as genetic composition and reduced access to healthy food (Kolata Citation2007; Vandenbroeck, Goossens, and Clemens Citation2010). Moreover, there are many cultural and psychosocial factors that contribute to obesity, such as role models (Lau, Lee, and Ransdell Citation2007), body image preferences (Becker et al. Citation1999), preoccupation with dieting (Bacon and Aphramor Citation2011), stress (Tomiyama Citation2014), and depression (Milaneschi et al. Citation2019). Also somatic causes may play a role, e.g. hormonal causes, medication with weight gaining side-effects and many other factors (van der Valk et al. Citation2019).
On a societal level, people with obesity are generally personally blamed for their weight (Saguy and Gruys Citation2010). This is often based on the false assumption that personal factors such as a sedentary lifestyle, poor eating behaviours, and psychological problems are the only causes of obesity (Puhl et al. Citation2015). Moreover, it is often thought that losing weight is easy, whereas compelling evidence exists that mechanisms in the body and brain counteract weight loss when a person developed obesity (Pucci and Batterham Citation2020). This leads to structural discrimination in practices such as not fitting in seats or clothing (Brewis et al. Citation2017), negative media portrayals (Heuer, McClure, and Puhl Citation2011), lower job opportunities (Brewis Citation2014; Puhl and Heuer Citation2010), insurances not covering weight loss treatments, and absence of anti-stigma legislation (Pearl Citation2018).
Thus, living with obesity and dealing with the accompanying stigma can negatively interfere with nearly all facets of people’s lives, in particular, in cultural contexts where a slender body is encouraged in many forms, e.g. social media, fashion, education. This example of weight stigma highlights the pervasive nature of health-related stigma.
Vicious circles of health-related stigma
We dive deeper into the reasons why health-related stigma is so pervasive to arrive at recommendations for sustainable stigma reduction. One explanation are the persistent motivations to stigmatize. Phelan, Link, and Dovidio (Citation2008) describe three generic motivations to stigmatize: 1) exploitation, 2) enforcement of social norms and 3) avoidance of disease. The above-described manifestations of health-related stigma and weight stigma mainly provide evidence for norm enforcement and disease avoidance. Monaghan (Citation2017) suggests that personally blaming people for obesity is rarely challenged due to a predominant ideology of personal responsibility, marketization and rolling back of the welfare state. This fits in a broader practice of stigmatizing people that burden the healthcare system and holding them personally accountable for this burden (Brelet et al. Citation2021).
Next to attributing chronic illnesses to personal responsibility, other motivations to stigmatize are cultural norms of physical attractiveness and pathogen avoidance. In many cultures there is a preference for thinness (Crandall Citation1994) and concerns of contagion may arise due to the widespread knowledge of health problems associated with certain chronic illnesses (Pearl Citation2018). Consequently, self-stigma may arise because the overall norms of being healthy may be stronger than self-interest. Moreover, people with a chronic illness often protect their self-image by distancing themselves from the negative label (De Brún et al. Citation2014), viewing their illness as a temporary condition (Durso and Latner Citation2008), and not identifying with others that are ill (Tomiyama et al. Citation2015). As a result, the stigma prevails because it is not challenged by anyone.
Health-related stigma is also pervasive because it can cause health disparities and vice versa (Hatzenbuehler, Phelan, and Link Citation2013), leading to a self-perpetuating cycle (see ). For example, stigmatization seems one of the causes for weight gain and a barrier for weight loss due to its negative social and psychological effects (Papadopoulos and Brennan Citation2015; Puhl and Suh Citation2015). If a person with obesity encounters stigma, they may start to feel more alone and isolated. This may cause depression and stress, and depression and stress cause negative health outcomes, such as weight gain (Jackson and Steptoe Citation2018; Tomiyama Citation2014). As a result, stigmatization can lead to a negative loop in which causes and effects of weight gain get intertwined.
Figure 2. The health-related stigma perpetuation model – a vicious circle (with obesity-related examples).
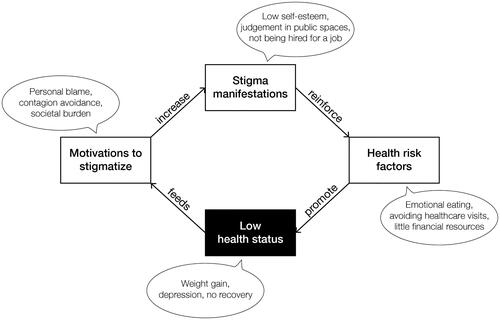
A vicious circle of health-related stigma starts when the effects of stigmatization negatively influence the victim’s physical or psychological health, and when the worsened health condition feeds motivations to stigmatize. Such vicious circles can be identified in intrapersonal, interpersonal, and structural stigmatization and are interlinked, as visualized in . For example, on an intrapersonal level, self-stigma makes people adopt maladaptive coping strategies, such as avoiding stigmatizing situations (Hayward, Vartanian, and Pinkus Citation2018). This includes avoiding exercising with others (Hunger et al. Citation2015), which negatively impacts a person’s health. In combination with structural stigmatization, such as negative media portrayals, and interpersonal stigmatization, such as colleagues making remarks, this can lead to lower self-esteem and lower self-efficacy and consequently, people may become less motivated to achieve life goals in general (Corrigan, Larson, and Rüsch Citation2009). As a result, this reinforces norms and beliefs that stigma victims lack willpower or are lazy, thereby feeding motivations to stigmatize.
Figure 3. People with chronic illnesses can experience interrelated vicious circles of health-related stigma on three levels. Examples of human and non-human actors are visible on the right.
In this way, causes and effects of stigmatization can initiate a vicious circle on one level, triggering new vicious circles on other levels. In the reviewed literature on weight stigma we found vicious circles as a result of failure and success stories of treatment (Bacon and Aphramor Citation2011), stereotype anxiety and social consensus (Pearl Citation2018), changes in social network and reduced social support (Brewis Citation2014), no in-group favouritism (Tomiyama et al. Citation2015), stress and depression (Tomiyama Citation2014), low socioeconomic position (Hulshof et al. Citation2003), and stigmas on other traits (Lewis and van Puymbroeck Citation2008). This multitude of stigma drivers not only increases the pervasiveness of a health-related stigma but also makes it very persistent and increasingly challenging to deal with for stigma victims.
In conclusion, health-related stigma is a psychosocial phenomenon from which chronically ill individuals can hardly escape, as illustrated in . The stigma often manifests itself on so many different levels with different actors that it maintains itself. Inspired by advancements in speculative design (Dunne and Raby Citation2013) and design fiction (Bleecker Citation2009), we think that design can play a role in stopping health-related stigmas from perpetuating themselves. In the following section, we argue for an approach in how to achieve this.
Towards designing destigmatizing storytelling environments
Effectively tackling health-related stigma is difficult, as it is often very subtle and difficult to grasp (Cook et al. Citation2014). For example, Lupton (Citation2018) argues that referring to obesity as an epidemic in itself is not stigmatizing, yet it does render large bodies susceptible for medical labelling. Due to the subtle nature of stigma, public health interventions sometimes even perpetuate it, because they fail to acknowledge that biases are a manifestation of social inequity (Alberga et al. Citation2016) or because the personal blame argument prevails throughout campaigns and policy (Lewis et al. Citation2011; de Boer and Lemke Citation2021).
To bring stigma perpetuation to a halt we suggest to redesign the social environments in which stigmatic interaction takes place, rather than contending against individual stigmatizing narratives or narrators. We can directly or indirectly influence the storytelling in these environments by creating an atmosphere or learning environment that makes participants feel safe, non-judgemental, and open to other perspectives. Within such a safe space, interactive narrative mechanics such as role playing and decision-making can provoke participants to interact with each other in a destigmatizing way. Such mechanics may support them to collaboratively determine the course of unfolding stories, change stories that already exist, or add new stories.
More specifically, designers can influence stigmatic storytelling or stimulate stigma-reducing storytelling by designing 1) the properties of a storytelling environment (e.g. Vaes et al. Citation2012) and 2) the rules that guide the storytelling interaction in an environment (e.g. Vegt et al. Citation2016). The first design strategy aims to influence participants’ storytelling through framing, i.e. ‘to select aspects of a perceived reality and make them more salient’ (Entman Citation1993, 52). For example, stories about obesity in the media were often accompanied by an image of a person with a large body with their head cut off (Heuer, McClure, and Puhl Citation2011). Image banks now provide images of people with large bodies in active and participating situations to foster recognition in stories about obesity. The second design strategy aims to evoke and steer storytelling by designing constraints and perceived affordances (Norman Citation1999). For example, predefined story elements and a stage and audience may guide participants towards desired or relevant storytelling.
Narrative freedom as a persuasive dimension in storytelling environments
When creating or shaping the storytelling environment to reduce health-related stigma, ethical questions appear in relation to the narrative agency of participants (Meretoja Citation2017): which stories should dominate and who should get a voice in discourses where stigmas prevail? The answers to these questions vary over place and time. Hence, the participants in a storytelling environment end up continuously negotiating between values (Korthals Altes Citation2014).
A storytelling environment influences this value negotiation by setting the narrative freedom that participants have, i.e. to tell their stories in the way they want constraint by all possible stories that the environment allows. For example, a frame narrative that explicitly introduces the role of stigma perpetrator and stigma victim stimulates participants to adopt these two perspectives and interact accordingly. Moreover, narrative freedom arises from resources in the environment to tell stories and to be heard (Zussman Citation2012). For example, the audience that encourages someone to tell one’s story compromises narrative freedom through their consent, attention, agreement, involvement, and expertise (Pasupathi and Billitteri Citation2015). In a Black Lives Matter rally, for example, protesters tell other stories than when they sit around the dinner table with their families.
Another strategy of setting narrative freedom is to confine the degrees of freedom participants have in interacting in a storytelling environment. The field of interactive digital narrative has explored various ways to interact within a narrative (e.g. Koenitz Citation2023), thereby varying the distribution of narrative agency between a narrator and its audience. We can apply such interactive narrative design heuristics on the broader storytelling environment level. Such interventions would than lead to interactive storytelling environments in which participants have a designated freedom to create, present, reflect on, and feel part of stories. Participants may, for example, build on each other’s stories or adapt their own story after hearing someone else’s story.
In relation to stigmatization, balancing this narrative freedom is crucial from an ethical as well as utilitarian point of view. Storytellers need to have a certain degree of narrative freedom to become engaged in telling their story, yet within boundaries that foster stigma reduction. Too low narrative freedom might not trigger enough interaction between stigma actors. Too high narrative freedom might only amplify the status-quo in stigma manifestations, motivations, and health effects.
Reducing health-related stigmas through storytelling
Based on our model of stigma perpetuation (), we identify three mechanisms that can break the vicious circle (as depicted in ). The first two mechanisms are to diminish stigma manifestations (mechanism 1) and deconstruct motivations to stigmatize (mechanism 2). This is supported by the claim of Link and Phelan (Citation2001) that stigma can only be effectively reduced when the power of stigmatizing groups gets limited and when fundamental motivations to stigmatize (i.e. domination, norm enforcement, disease avoidance) are taken away. Richman and Lattanner (Citation2014) add that stigma victims become empowered by promoting personal agency and control over the stigma. This supports the third mechanism of supporting stigma victims in dealing with stigmatizing situations to stop the reinforcement of health risk factors.
Figure 4. Three mechanisms to break the vicious circle in the health-related stigma perpetuation model. 1) Diminish stigma manifestations (press machine). 2) Deconstruct motivations (chisel and hammer). 3) deal with stigmatization (scissors).
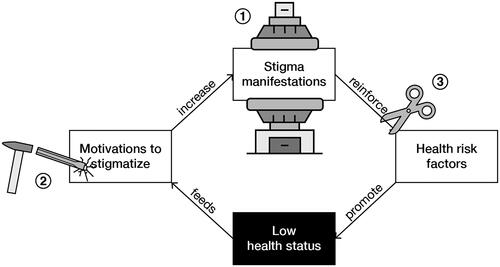
These stigma-reducing mechanisms may be well understood from a narrative perspective, as health-related stigma can be characterized as a complicated network of narratives that interact with each other and that perpetuate the stigma, as visualized in . Storytelling may provide a way to intervene in this stigmatic narrative network by conveying new experiences, persuading the stigma actors, and exploring alternative perspectives (Meretoja Citation2017). To come to a more structured understanding of the potential destigmatizing functions of storytelling, we make a distinction between story content and story interaction. In the following sections, we further detail the potential functions of story content and story interactions in relation to the three mechanisms that could stop stigma perpetuation (see ). In this way, we aim to describe a detailed research agenda regarding the destigmatizing potential of interactive storytelling environments.
Table 1. Seven potential functions of story content and story interactions in three basic stigma-reducing mechanisms.
Diminish stigma manifestations
Interventions that aim to directly reduce health-related stigmatization, such as reducing bullying at schools, are often based on inducing empathy (Knaak, Modgill, and Patten Citation2014). For example, by explaining the difficulty of losing weight through first-person narratives (Teachman et al. Citation2003) and role-playing exercises (Wiese et al. Citation1992).
1. Expose to other perspectives – A basic precondition of reducing stigma through empathy is the availability of stories from different perspectives. Carefully distributing and defining these perspectives in a storytelling environment is important. With a clear presentation of scenes through the selection or restriction of narrative information (Gérard Citation1980), stories can be used to make stigma perpetrators experience the perspective of stigma victims and vice versa. Furthermore, the story medium should be chosen carefully to reach an audience with other perspectives. Davidson et al. (Citation2018), for example, successfully reached the general public by publishing online video testimonies about mental illness among veterans and firefighters. When designing an interactive storytelling environment, it is thus advisable to already collect stories from varying perspectives and use those as prompts for destigmatizing discussions. Role playing and role shifting could be additional interactive narrative mechanisms that support participants in experiencing other perspectives.
2. Provide a protective frame – A protective frame of fiction is assumed to evoke empathic responses (Keen Citation2006; Kidd and Castano Citation2013). No conclusive evidence exists regarding the empathy-inducing effect of fictionality (Braddock and Dillard Citation2016). Yet, Carey et al. (Citation2020) show that using a shared fiction does relieve participants to disclose very personal experiences and establish shared understandings of stigmatizing situations.
This effect is similar to what happens in gaming experiences. As described by Visch et al. (Citation2013), gaming temporarily moves people’s attention away from their daily life. This mental transportation can lead to a psychological protective frame in which participants become more playful (Apter Citation1993) and feel stronger engagement, immersion, and emotional presence (Roth, Vorderer, and Klimmt Citation2009). If an interactive storytelling environment affords confidentiality or feels like a game in which exploration is allowed, stigma perpetrators may adopt a more open attitude towards their own stigmatizing behaviours. Additionally, such a protective frame may evoke a safer feeling among stigma victims to disclose personal stigmatic experiences.
3. Intervene in daily conversations – In daily conversations, stigma expressions could reduce by becoming aware of the underlying master narratives. Master narratives are ‘culturally shared stories that guide thoughts, beliefs, values, and behaviours’ (McLean and Syed Citation2015). This awareness may trigger or teach participants to counter stigmatic master narratives (Bamberg and Andrews Citation2004). An example of triggering counter narratives is the reframing of texts, such as ‘living with excess weight is not a sin, it is a quest’ (Vyncke and Van Gorp Citation2020). Participants can be triggered to counter stigmatic stories directly by providing them with ‘narrative ammunition’. For example, the labels imposed upon stigma victims, such as healthy and sick, almost never reflect reality. Being aware of such binary oppositions and normative choice of words and critiquing them (Derrida Citation1972) may support counter narratives in daily conversations. An interactive storytelling environment could provide triggers to reflect during conversations. Such ‘small story’ interventions not only affect the direct conversation but also enhance people’s reflexivity in general (Georgakopoulou Citation2015).
Another method that may fuel subversiveness towards stigmas is to recognize what is not being said (cf. Barthes and Duisit Citation1975). Health-related stigma is often felt the most when implicitly communicated, thus being able to recognize implicit messages in conversations may help in countering stigmatic narratives. Irigaray (Citation1985) provides an example of deploying stories as enacted, as opposed to stories being told. For example, if women are viewed as illogical, they should speak logically about this view, thereby enacting the counter-narrative. Although critiqued for its relatively aggressive approach (Kozel Citation1996), an interactive storytelling environment could support stigma victims in enacting counter stories through, for example, theatrical props.
Deconstruct motivations to stigmatize
The mechanism of deconstructing stigma motivations entails changes in stigmatic beliefs, attitudes, and intentions, such as the idea that an illness is fully controllable by the individual that is ill. Motivations behind obesity stigma, for example, may be altered through stories about multiple factors, not only lifestyle, that lead to weight gain. Destigmatizing education of healthcare practitioners is mainly aimed at altering motivations (Knaak, Modgill, and Patten Citation2014), such as stories about the noncontrollable causes of an illness (e.g. Puhl, Schwartz, and Brownell Citation2005) and the causes and effects of health-related stigma itself (e.g. Hague and White Citation2005).
4. Persuade stigma actors – The persuasive strength of such stories is key to alter motivations to stigmatize (De Graaf, Sanders, and Hoeken Citation2016). Van Laer et al. (Citation2013) describe that the persuasiveness of stories depends on narrative transportation, i.e. experiencing story events through feeling the emotions of a story character and vivid images of the story plot. Hence, a persuasive storytelling environment should enable participants to identify with story characters (e.g. Winskell, Sabben, and Obong’o Citation2019) and easily imaginable events, such as anecdotes and daily life situations (Boeijinga, Hoeken, and Sanders Citation2017) in familiar cultural contexts (Larkey and Hecht Citation2010). Another characteristic of narrative persuasion is that it predominantly has story-consistent effects (Braddock and Dillard Citation2016). Thus embedding destigmatizing messages and showing destigmatizing behaviour in a story is more likely to reduce stigma than showing stigmatic behaviour or literally stating the message of a story (Shen, Sheer, and Li Citation2015).
5. Exchange alternative understandings – Next to persuasive stories, we suggest feeding storytelling environments with alternative understandings. This proposal builds on social consensus mechanisms that have been studied as a destigmatizing intervention. Puhl, Schwartz, and Brownell (Citation2005) demonstrated that stigmatic attitudes of undergraduate students diminished when being exposed to positive attitudes of peers. Another strategy to evoke alternative views in storytelling environments is to value disagreement and pluralism, i.e. to adopt an agnostic approach (Mouffe Citation1999). Accordingly, variation in stories should be the denominator for distributing storytelling resources, rather than supporting every storyteller equally. Moreover, the content and message of a story should not be judged but responded to with other stories. As a result, participants in storytelling environments ideally alternate between storyteller and listener roles (cf. Hammond, Pain, and Smith Citation2007). Still, stigmatic stories may be adopted as easily as destigmatizing stories (Cavazza et al. Citation2015). Hence, in addition to agnostic resource distribution, storytelling environments should actively promote destigmatizing storytelling or penalize stigmatic stories.
Deal with stigmatization
The mechanism of dealing with stigmatization builds on literature describing how, predominantly female, stigma victims themselves develop their ways of dealing or coping with health-related stigma. First of all, ways to deal with self-stigma come down to maintaining or fostering self-esteem and self-worth, such as depersonalizing the stigma (Bombak and Monaghan Citation2017), finding social support (Chou, Prestin, and Kunath Citation2014), focus on body functionality (Alleva et al. Citation2015), and positive self-talk, self-love, and self-acceptance (Myers and Rosen Citation1999). Other examples of coping strategies for stigma victims are fighting back, rationalizing the stigmatizing behaviour as a flaw from the perpetrator, feeling competent regarding the illness, refusing to hide the illness and ignoring the stigmatizing situation (Myers and Rosen Citation1999; Lewis et al. Citation2011; van Amsterdam and van Eck Citation2019; Lu et al. Citation2003). These activities can all be supported with storytelling.
6. Elicit understanding and support - Ziebland and Wyke (Citation2012) suggest that stigma mainly reduces by learning from experiences from others. Moreover, tailoring stories to stigma victims and adopting diversity values are assumed to have an empowering effect (Reid et al. Citation2014). At the same time stories should address the perspective of stigma perpetrators to exert attitudinal and behavioural change (Larkey and Hecht Citation2010). Consequently, there is a duality between empowering stigma victims and persuading stigma perpetrators.
Explicating the roles of victim and perpetrator in a storytelling environment may solve this duality. Bruneau and Saxe (Citation2012) show that a positive attitude change happens when members of a low power group tell their perspective to members of a powerful group. Additionally, powerful group members show positive attitude changes towards the low power group after summarizing what they have heard. Hence, explicitly assigning stigma victims as storyteller and perpetrators as listener elicits understanding and support for both sides. Consequently, learning to tell the story helps to deal with stigmatization. Being able to align one’s story with other narratives and thus telling one’s experiences appropriately helps to elicit understanding and support from others.
7. Support stigma coping – The process of constructing a coherent story may support stigma coping as well. Storytelling with others can help in making sense of what has happened, thereby supporting the reflective process of dealing with stigmatizing situations (Lely et al. Citation2019). On an intrapersonal level, co-created stories may benefit education, counselling, expressive writing, belonging, and values affirmation (Cook et al. Citation2014). On an interpersonal level, collaborative storytelling could enhance coping in therapy group sessions, patient-physician interactions, parent-child dialogue, and peer support groups (Winskell, Sabben, and Obong’o Citation2019). Collaborative storytelling could support stigma coping on a structural level by initiating policy and design changes, and by providing role models (Gomillion and Giuliano Citation2011).
Demonstration of an interactive storytelling environment that reduces weight stigma
To break the vicious circles of health-related stigma, interactive storytelling environments ideally deploy all above-described destigmatizing functions of storytelling. As shown in , storytelling environments should 1) expose stigma victims and perpetrators to other perspectives, 2) provide a protective frame, 3) intervene in daily conversations, 4) persuade all stigma actors, 5) exchange alternative understandings, 6) elicit understanding and support for stigma victims, and 7) support stigma victims to cope with stigmatization. In this section we give an example of an interactive storytelling environment against obesity stigma: the game of Ball & Stick. It is not meant as a full case study, but to demonstrate how the above-described theory could be applied ().
Figure 5. Seven functions of interactive storytelling environments intervening on three mechanisms in the self-perpetuation of stigma.
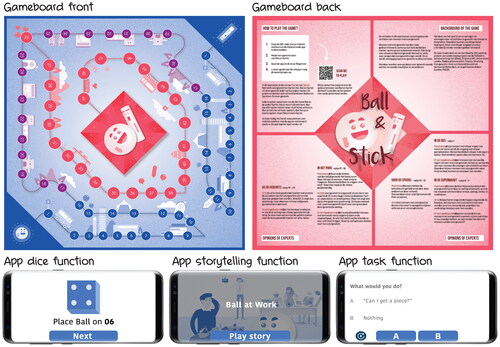
Ball & Stick
Ball & Stick is a game for community centres with the purpose of reducing the stigmatization of people with obesity. Ideally, it is played with four participants. The game consists of a gameboard, two pawns, and a mobile application that verbally guides players through the game with a virtual dice, narrated stories, and discussion tasks (see Appendix for a detailed content description). The story in the game revolves around two abstractly visualized characters (function 2) represented by two pawns: Ball – a stigma victim, and Stick – a stigma perpetrator. Participants choose which role they want to play. During the game, the players are confronted with stigmatizing situations that people with obesity encounter (function 1). The game facilitates a careful build-up of the discussion between the players through increasing narrative freedom by first choosing between response options, then generating a personal response, and finally jointly agreeing on a response. This varying narrative freedom guides the players in stepwise formulating their thoughts (function 5).
All in-game events are based on conversations with community centre visitors, people with obesity, and obesity specialists. In this way, the events in the game are familiar and easily imaginable (function 4). Additionally, narrative transportation is eased through the common overall narrative of a love story and the game rules were as simple as game of goose. The in-game stigmatic situations were based on regular daily life events, including commonly occurring conversations (function 3). The collected real stories are all from the stigma victim perspective so that the game basically serves as a message from stigma victims to stigma perpetrators (function 6). To allow for coping, next to raising awareness, the back of the gameboard features expert interpretations of several events in the game (function 7). Moreover, the closing narration in the app explicitly states the coping strategy of talking to each other about obesity stigma.
We evaluated the Ball & Stick game with 22 visitors of two community centres (age: 60 (43-83), female: 15) in low-income neighbourhoods of two Dutch cities. We targeted the game to middle aged people with a low income because low socio-economic position is significantly related to obesity prevalence and obesity often develops when people finish their working life (Robroek et al. Citation2015). Five groups of four players and one group of two played the game in a meeting room at the two community centres. Fourteen of the twenty-two participants lived in neighbourhoods that are within the 10% poorest neighbourhoods in the Netherlands and approximately half of the group had overweight (based on observation).
After a short introduction and giving informed consent the game session started. The two present researchers gave no instructions, as the game was designed to be standalone. Researchers would only intervene in case of a technical malfunction and occasionally encouraged participants to speak more clearly. After playing the game, the players started a discussion, sometimes directly triggered by the game. After their first reactions, the participants were asked to fill in a questionnaire and the researchers initiated a group discussion about the usability, experience, and effect of the game.
Nearly all participants reported a positive engaging experience. Many indicated that the events in the game were familiar to them and that the game raised their awareness. For sixteen participants the game made it easier to talk about obesity and twelve said that it changed their attitude towards people with obesity.
A significant effect of the game was the self-initiated discussion among participants after gameplay. Several groups discussed causes and solutions for discrimination, obesity, and healthy eating. Personal stories about racism, burnout, and depression, suggest that the game created an open atmosphere between the players in which varying beliefs and perspectives in relation to obesity stigma were exchanged. Many participants recognized events from their own experience and explicitly shared their personal beliefs, that were sometimes challenged by others. Moreover, participants explained that the game taught them the basic mechanisms of stigmatization. Yet they also indicated that these positive conversations probably only happen during the game and that they will ‘call each other “fatty” again’ as soon as they leave the room. Nonetheless, we conclude that the Ball & Stick game was successful in creating a storytelling environment for destigmatizing interaction between people with varying experiences, perspectives, and beliefs.
Discussion
In this article we introduce the concept of interactive storytelling environments as a means to reduce health-related stigmatization and suggest applying it to places where health-related stigma is expressed, such as bullying at community centres, judgmental recommendations at supermarkets, or blunt instructions at hospitals. Within interactive storytelling environments, participants are invited to listen and respond to stories from others and at the same time guided in telling their own. As demonstrated by the Ball & Stick game, the advantage of interactive storytelling environments is that they can be deliberately designed to evoke empathy with others, stimulate discussion and critical thinking, and guide towards consensus.
This approach could be a valuable addition to current speculative design approaches in which products and objects are designed to encourage critical reflection (Dunne and Raby Citation2013). Provocative storytelling environments can stimulate critical reflection and facilitate interactions between different stigma actors. The narrative freedom for each actor is a major parameter in such environments to influence the storytelling possibilities that stigma actors have. By designing interventions that afford or limit this freedom in storytelling, stigma actors can be directed towards 1) diminishing stigma manifestations, 2) deconstructing motivations to stigmatize, and 3) dealing with stigmatizing situations.
The benefit of interactive storytelling environments is not only restricted to health-related stigma. It can also be used to tackle other types of stigmas. Many social issues, such as women’s rights, attitudes towards migrants, and racism could be addressed with design interventions using the storytelling environment approach. More generally, many design processes could benefit from a storytelling environment perspective, in particular where vulnerable or minority groups are involved (Parrott, Carpentier, and Northup Citation2017). On the one hand storytelling feeds the design process (e.g. Maxwell et al. Citation2015) and on the other hand a deliberately designed environment can guide the storytelling.
Within the limitations of this paper, we could not give an exhaustive overview of storytelling theories, yet with the seven functions of a storytelling environment we aim to set a research agenda regarding its destigmatizing potential. The Ball & Stick case provides a first idea of designing and applying interactive storytelling environments and demonstrates that such environments contribute to health-related stigma reduction. To apply it more broadly a generic model and design method are required. The basic narratological and interactive digital narrative concepts that we briefly touched upon in this article could serve as a basis for such a model, which could also take further the field of applied narratology (Moenandar Citation2018). Moreover, knowledge from participatory design and user generated content (cf. Lukyanenko et al. Citation2016) could support the practical application of such a model.
The seven stigma-reducing functions of storytelling may be applied to a large variation of health-related storytelling environments, for example in the conversation between patients and physicians in consultation rooms. In such contexts, a narrative protective frame could comfort patients and support physicians. Moreover, to welcome storytelling in such a situation could evoke both parties’ openness to the other’s perspective and enable exchange of alternative understandings (Bury Citation2001). Storytelling tools, such as props or preformatted texts, could help to deliberate on the use of words, as well as deploy the persuasive qualities of narrative transportation. And to make it complete, the consultation room should provide patients with the tools to tell their story appropriately to elicit understanding from the physician and to counter possible unfortunate events of stigmatizing behaviour.
Eventually, the key role of an interactive storytelling environment is to activate a conversation between all stigma actors and guide them towards destigmatizing storytelling. To achieve this, questions about the properties of an interactive storytelling environment pop up. In this article, we covered narrative freedom as a core dimension. Other important properties would include the composition and interests of participants, modes of communication (e.g. verbal, visual, theatrical), and the literacy level of participants. To connect with the participants’ interests and experiences we envision a co-creative process in which all users of a storytelling environment are involved in creating the stories. For example, Whitley et al. (Citation2020) show that documentary-style videos about mental illness, created by people with a mental illness, led to informative, relatable, attention-grabbing, and change-inducing videos that have promising stigma-reducing effects among the viewers.
Finally, we think that interactive storytelling environments contribute to the transition in healthcare from paternalistic top-down approaches to deliberative patient-centred bottom-up approaches (Emanuel and Emanuel Citation1992). Accordingly, designers of storytelling environments should maintain a neutral position and focus on providing a fitting storytelling environment that stimulates empathy and an awareness and exchange of values and ideas. The environment should mainly facilitate a fair process of meaning-making among all health-related stigma actors, trusting that nearly everyone can tell stories and listen to them.
Conclusion
In this article we propose to use interactive storytelling environments to reduce health-related stigma. We first developed an understanding of the mechanisms behind stigmatization with the health-related stigma perpetuation model () to come to mechanisms on how to break the vicious circle. Due to the multi-layered and multifaceted character of stigmas, we suggest influencing stigmatic storytelling. We theorize seven stigma-reducing functions of storytelling that can be applied to social environments and discuss design considerations within these functions. Some of these considerations have been applied to a design case that demonstrates a destigmatizing interactive storytelling environment: the game of Ball & Stick.
In conclusion, this paper is mainly a call to designers, researchers, and practitioners in health and wellbeing to become aware of health-related stigmatization and create the conditions to reduce stigmas. Our hope is that our propositions in this paper inspire to further erase stigmas by design.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Notes on contributors
Niko Vegt
Niko Vegt is a Post-Doctoral Researcher at the Faculty of Industrial Design Engineering. His research revolves around social change and the interaction between people through interactive storytelling, serious gaming, and gamification, particularly in healthcare. Niko holds a MSc and BSc degree from Eindhoven University of Technology, faculty Industrial Design. In 2018, he obtained his PhD degree in Industrial Design Engineering at the Delft University of Technology. Niko worked as a human-centered design researcher at the Leiden University Medical Centre. Throughout his career his work is characterized by the research through design approach where the design process is as valuable as analysis and evaluation processes for generating knowledge.
Valentijn Visch
Valentijn Visch is Associate Professor at the Faculty of Industrial Design Engineering at TU Delft. His research is focused on Design for Health Motivation. He coordinates Persuasive Game Design research, chairs the IDE eHealth research lab, and is project leader of several health-related interdisciplinary research projects including subjects like storytelling, digital twins, eHealth & game design, health literacy, obesity prevention, reaching people with low SEP and health journeys.
Wilbert Spooren
Elisabeth F. C. van Rossum is internist-endocrinologist and professor in the field of obesity and biological stress research at the Erasmus University Medical Centre, Rotterdam, Netherlands. She is co-founder of the Obesity Centre CGG. She obtained her MD and PhD (both cum laude) in Rotterdam, and performed an obesity research fellowship in Baltimore, USA. Currently, she holds various societal/board positions: European lead of the theme Obesity and Diabetes of the European Society for Endocrinology, Chair of the National Obesity Guideline, and President of the Partnership Overweight Netherlands with an advisory role to the Ministry of Health Welfare. She published with colleague Mariette Boon an international bestseller and award-winning book ‘VET belangrijk’ or -the international edition- ‘FAT, the secret organ’. In 2020 and 2021 she was appointed as Top10 most influencing women in health care in the Netherlands.
Elisabeth F. C. van Rossum
Andrea W.M. Evers is professor of Health Psychology and chair of the Institute of Psychology at Leiden University, the Netherlands. She is also affiliated to the Technical University Delft and Erasmus University Rotterdam as Medical Delta Professor Healthy Society. After her PhD (cum laude), Andrea Evers obtained several personal grants and awards) for her innovative, interdisciplinary and translational research on psychoneurobiological mechanisms and treatments for health and disease. She was elected as a lifetime member of the Dutch Royal Academy of Science and Arts (KNAW) as well as the Royal Dutch Society of Science (KHMW). Since 2021, she is also a member of the supervisory board of the VU University Amsterdam.
Andrea W. M. Evers
Annemiek van Boeijen is Assistant Professor Industrial Design at the faculty of Industrial Design Engineering at the Delft University of Technology. Her research isfocused on the role of culture in design processes, with the goal of designing methods and tools, geared to support designers in cultivating a culture-sensitive approach. She is initiator and co-editor of the Delft Design Guide, an overview of perspectives, models, approaches and methods for design, and author of the book Culture Sensitive Design - A guide to culture in practice.
Annemiek van Boeijen
Wilbert Spooren is professor of Discourse Studies of Dutch at Centre for Language Studies (CLS), Radboud Universiteit Nijmegen. His research concerns the use of language in different genres, and its effect on communication. He has a special interest in the role of language in new media. He obtained his PhD in 1989 at Radboud University. He was one of the initiators of the NWO thematic program Comprehensible Language and Effective Communication (2010-2018). He currently supervises various PhD projects that focus on the role of language in medical communication, specifically with lower literacy target groups.
References
- Alberga, Angela S., Shelly Russell-Mayhew, Kristin M. von Ranson, and Lindsay McLaren. 2016. “Weight Bias: A Call to Action.” Journal of Eating Disorders 4 (1): 34–34. https://doi.org/10.1186/s40337-016-0112-4
- Alleva, Jessica M., Carolien Martijn, Gerard J. P. Van Breukelen, Anita Jansen, and Kai Karos. 2015. “Expand Your Horizon: A Programme That Improves Body Image and Reduces Self-Objectification by Training Women to Focus on Body Functionality.” Body Image 15: 81–89. https://doi.org/10.1016/j.bodyim.2015.07.001
- Apter, Michael J. 1993. “Phenomenological Frames and the Paradoxes of Experience.” In Advances in Reversal Theory, edited by John H. Kerr, Stephen Murgatroyd, and Michale J. Apter, 27–39. Amsterdam, NL: Swetz & Zeitlinger.
- Bacon, Linda, and Lucy Aphramor. 2011. “Weight Science: Evaluating the Evidence for a Paradigm Shift.” Nutrition Journal 10: 9. https://doi.org/10.1186/1475-2891-10-9
- Bamberg, Michael. 2011. “Narrative Practice and Identity Navigation.” In Varieties of Narrative Analysis, edited by James A. Holstein and Jaber F. Gubrium, 99–124. London, UK: SAGE.
- Bamberg, Michael, and Molly Andrews. 2004. Considering Counter-Narratives: Narrating, Resisting, Making Sense. Vol. 4. Amsterdam, NL: John Benjamins Publishing.
- Barthes, Roland, and Lionel Duisit. 1975. “An Introduction to the Structural Analysis of Narrative.” New Literary History 6 (2): 237–272. https://doi.org/10.2307/468419
- Bayer, Ronald. 2008. “Stigma and the Ethics of Public Health: not Can we but Should we.” Social Science & Medicine (1982) 67 (3): 463–472. https://doi.org/10.1016/j.socscimed.2008.03.017
- Becker, Diane M., Lisa R. Yanek, Dyann M. Koffman, and Yvonne C. Bronner. 1999. “Body Image Preferences among Urban African Americans and Whites from Low Income Communities.” Ethnicity & Disease 9 (3): 377–386.
- Bleecker, Julian. 2009. Design Fiction: A Short Essay on Design, Science, Fact, and Fiction. Near Future Laboratory.
- Boeijinga, Anniek, Hans Hoeken, and José Sanders. 2017. “Storybridging: Four Steps for Constructing Effective Health Narratives.” Health Education Journal 76 (8): 923–935. https://doi.org/10.1177/0017896917725360
- Bombak, Andrea E., and Lee F. Monaghan. 2017. “Obesity, Bodily Change and Health Identities: A Qualitative Study of Canadian Women.” Sociology of Health & Illness 39 (6): 923–940. https://doi.org/10.1111/1467-9566.12537
- Braddock, Kurt, and James Price Dillard. 2016. “Meta-Analytic Evidence for the Persuasive Effect of Narratives on Beliefs, Attitudes, Intentions, and Behaviors.” Communication Monographs 83 (4): 446–467. https://doi.org/10.1080/03637751.2015.1128555
- Brelet, Lisa, Valentin Flaudias, Michel Désert, Sébastien Guillaume, Pierre-Michel Llorca, and Yves Boirie. 2021. “Stigmatization toward People with Anorexia Nervosa, Bulimia Nervosa, and Binge Eating Disorder: A Scoping Review.” Nutrients 13 (8): 2834. https://doi.org/10.3390/nu13082834
- Brewis, Alexandra. 2014. “Stigma and the Perpetuation of Obesity.” Social Science & Medicine (1982) 118: 152–158. https://doi.org/10.1016/j.socscimed.2014.08.003
- Brewis, Alexandra, Sarah Trainer, SeungYong Han, and Amber Wutich. 2017. “Publically Misfitting: extreme Weight and the Everyday Production and Reinforcement of Felt Stigma.” Medical Anthropology Quarterly 31 (2): 257–276. https://doi.org/10.1111/maq.12309
- Bruneau, Emile G., and Rebecca Saxe. 2012. “The Power of Being Heard: The Benefits of ‘Perspective-Giving’in the Context of Intergroup Conflict.” Journal of Experimental Social Psychology 48 (4): 855–866. https://doi.org/10.1016/j.jesp.2012.02.017
- Bury, Mike. 2001. “Illness Narratives: fact or Fiction?” Sociology of Health & Illness 23 (3): 263–285. https://doi.org/10.1111/1467-9566.00252
- Carey, Hillary, Alexandra To, Jessica Hammer, and Geoff Kaufman. 2020. “Fictional, Interactive Narrative as a Foundation to Talk about Racism.” Paper Presented at the Companion Publication of the 2020 ACM Designing Interactive Systems Conference. https://doi.org/10.1145/3393914.3395885
- Cavazza, Marc, Fred Charles, Alan Lindsay, Jonathan Siddle, and Gersende Georg. 2015. “An Interactive Narrative Format for Clinical Guidelines.” KI - Künstliche Intelligenz 29 (2): 185–191. https://doi.org/10.1007/s13218-015-0354-3
- Chou, Wen-ying Sylvia, Abby Prestin, and Stephen Kunath. 2014. “Obesity in Social Media: A Mixed Methods Analysis.” Translational Behavioral Medicine 4 (3): 314–323. https://doi.org/10.1007/s13142-014-0256-1
- Cook, Jonathan E., Valerie Purdie-Vaughns, Ilan H. Meyer, and Justin T. A. Busch. 2014. “Intervening within and across Levels: A Multilevel Approach to Stigma and Public Health.” Social Science & Medicine (1982) 103: 101–109. https://doi.org/10.1016/j.socscimed.2013.09.023
- Corrigan, Patrick W., Jonathon E. Larson, and Nicolas Rüsch. 2009. “Self-Stigma and the ‘Why Try’ Effect: impact on Life Goals and Evidence-Based Practices.” World Psychiatry: official Journal of the World Psychiatric Association (WPA) 8 (2): 75–81. https://doi.org/10.1002/j.2051-5545.2009.tb00218.x
- Crandall, Christian S. 1994. “Prejudice against Fat People: Ideology and Self-Interest.” Journal of Personality and Social Psychology 66 (5): 882–894. https://doi.org/10.1037//0022-3514.66.5.882
- Davidson, Tatiana, Angela Moreland, Brian E. Bunnell, Jennifer Winkelmann, Jessica L. Hamblen, and Kenneth J. Ruggiero. 2018. “Reducing Stigma in Mental Health through Digital Storytelling.” In Deconstructing Stigma in Mental Health, 169–183. London, UK: IGI Global.
- de Boer, Bas, and Mailin Lemke. 2021. “Bringing Disgust in through the Backdoor in Healthy Food Promotion: A Phenomenological Perspective.” Medicine, Health Care, and Philosophy 24 (4): 731–743. https://doi.org/10.1007/s11019-021-10037-0
- De Brún, Aoife, Mary McCarthy, Kenneth McKenzie, and Aileen McGloin. 2014. “Weight Stigma and Narrative Resistance Evident in Online Discussions of Obesity.” Appetite 72: 73–81. https://doi.org/10.1016/j.appet.2013.09.022
- Derrida, Jacques. 1972. Positions. Paris, FR: Nouvelles Editions Latines.
- Dunne, Anthony, and Fiona Raby. 2013. Speculative Everything: design, Fiction, and Social Dreaming. Cambridge, US: MIT Press.
- Durso, Laura E., and Janet D. Latner. 2008. “Understanding Self-Directed Stigma: Development of the Weight Bias Internalization Scale.” Obesity 16 (S2): 80–86. https://doi.org/10.1038/oby.2008.448
- Emanuel, Ezekiel J., and Linda L. Emanuel. 1992. “Four Models of the Physician-Patient Relationship.” Jama 267 (16): 2221–2226. https://doi.org/10.1001/jama.1992.03480160079038
- Entman, Robert M. 1993. “Framing: Toward Clarification of a Fractured Paradigm.” Journal of Communication 43 (4): 51–58. https://doi.org/10.1111/j.1460-2466.1993.tb01304.x
- Falk, Gerhard. 2001. Stigma: How we Treat Outsiders. Buffalo, US: Prometheus Books.
- Georgakopoulou, Alexandra. 2015. “Small Stories Research.” In The Handbook of Narrative Analysis, edited by Anna De Fina and Alexandra Georgakopoulou, 255–271. Chichester: John Wiley & Sons, Inc.
- Gérard, Genette. 1980. Narrative Discourse: An Essay in Method. Translated by Jane E. Lewin. Ithaca: Cornell UP.
- Giskes, K., M. Avendano, J. Brug, and A. E. Kunst. 2010. “A Systematic Review of Studies on Socioeconomic Inequalities in Dietary Intakes Associated with Weight Gain and Overweight/Obesity Conducted among European Adults.” Obesity Reviews: An Official Journal of the International Association for the Study of Obesity 11 (6): 413–429. https://doi.org/10.1111/j.1467-789X.2009.00658.x
- Goffman, E. 1963. Stigma: The Management of Spoiled Identity. Harmondsworth: Penguin.
- Gomillion, Sarah C., and Traci A. Giuliano. 2011. “The Influence of Media Role Models on Gay, Lesbian, and Bisexual Identity.” Journal of Homosexuality 58 (3): 330–354. https://doi.org/10.1080/00918369.2011.546729
- De Graaf, Anneke, José Sanders, and Hans Hoeken. 2016. “Characteristics of Narrative Interventions and Health Effects: A Review of the Content, Form, and Context of Narratives in Health-Related Narrative Persuasion Research.” Review of Communication Research 4: 88–131. https://doi.org/10.12840/issn.2255-4165.2016.04.01.011
- Hague, Anne L., and Adrienne A. White. 2005. “Web-Based Intervention for Changing Attitudes of Obesity among Current and Future Teachers.” Journal of Nutrition Education and Behavior 37 (2): 58–66. https://doi.org/10.1016/s1499-4046(06)60017-1
- Hammond, Sean, Helen Pain, and Tim J. Smith. 2007. “Player Agency in Interactive Narrative: audience, Actor & Author.” Proceedings of AISB '07: Artificial and Ambient Intelligence, 2-4 Apr 2007, Newcastle, UK.
- Harriger, Jennifer A., and J. Kevin Thompson. 2012. “Psychological Consequences of Obesity: Weight Bias and Body Image in Overweight and Obese Youth.” International Review of Psychiatry (Abingdon, England) 24 (3): 247–253. https://doi.org/10.3109/09540261.2012.678817
- Hatzenbuehler, Mark L. 2016. “Structural Stigma and Health Inequalities: Research Evidence and Implications for Psychological Science.” The American Psychologist 71 (8): 742–751. https://doi.org/10.1037/amp0000068
- Hatzenbuehler, Mark L., and Bruce G. Link. 2014. “Introduction to the Special Issue on Structural Stigma and Health.” Social Science & Medicine (1982) 103: 1–6. https://doi.org/10.1016/j.socscimed.2013.12.017
- Hatzenbuehler, Mark L., Jo. C. Phelan, and Bruce G. Link. 2013. “Stigma as a Fundamental Cause of Population Health Inequalities.” American Journal of Public Health 103 (5): 813–821. https://doi.org/10.2105/AJPH.2012.301069
- Hayward, Lydia E., Lenny R. Vartanian, and Rebecca T. Pinkus. 2018. “Weight Stigma Predicts Poorer Psychological Well‐Being through Internalized Weight Bias and Maladaptive Coping Responses.” Obesity (Silver Spring, Md.) 26 (4): 755–761. https://doi.org/10.1002/oby.22126
- Hebl, Michelle R., and John F. Dovidio. 2005. “Promoting the “Social” in the Examination of Social Stigmas.” Personality and Social Psychology Review: An Official Journal of the Society for Personality and Social Psychology, Inc 9 (2): 156–182. https://doi.org/10.1207/s15327957pspr0902_4
- Heuer, Chelsea A., Kimberly J. McClure, and Rebecca M. Puhl. 2011. “Obesity Stigma in Online News: A Visual Content Analysis.” Journal of Health Communication 16 (9): 976–987. https://doi.org/10.1080/10810730.2011.561915
- Hulshof, K. F. A. M., J. H. Brussaard, A. G. Kruizinga, J. Telman, and M. R. H. Löwik. 2003. “Socio-Economic Status, Dietary Intake and 10 y Trends: The Dutch National Food Consumption Survey.” European Journal of Clinical Nutrition 57 (1): 128–137. https://doi.org/10.1038/sj.ejcn.1601503
- Hunger, Jeffrey M., Brenda Major, Alison Blodorn, and Carol T. Miller. 2015. “Weighed down by Stigma: How Weight-Based Social Identity Threat Contributes to Weight Gain and Poor Health.” Social and Personality Psychology Compass 9 (6): 255–268. https://doi.org/10.1111/spc3.12172
- Irigaray, Luce. 1985. This Sex Which is Not One (1977). New York, US: Cornell University Press.
- Jackson, Sarah E., and Andrew Steptoe. 2018. “Obesity, Perceived Weight Discrimination, and Hair Cortisol: A Population-Based Study.” Psychoneuroendocrinology 98: 67–73. https://doi.org/10.1016/j.psyneuen.2018.08.018
- Keen, Suzanne. 2006. “A Theory of Narrative Empathy.” Narrative 14 (3): 207–236. https://doi.org/10.1353/nar.2006.0015
- Kidd, David Comer, and Emanuele Castano. 2013. “Reading Literary Fiction Improves Theory of Mind.” Science (New York, N.Y.) 342 (6156): 377–380. https://doi.org/10.1126/science.1239918
- Knaak, Stephanie, Geeta Modgill, and Scott B. Patten. 2014. “Key Ingredients of anti-Stigma Programs for Health Care Providers: A Data Synthesis of Evaluative Studies.” The Canadian Journal of Psychiatry 59 (1_suppl): 19–26. https://doi.org/10.1177/070674371405901S06
- Koenitz, Hartmut. 2023. Understanding Interactive Digital Narrative: Immersive Expressions for a Complex Time. London, UK: Taylor & Francis.
- Kolata, Gina Bari. 2007. Rethinking Thin: The New Science of Weight Loss–and the Myths and Realities of Dieting. London, UK: Macmillan.
- Korthals Altes, Liesbeth. 2014. Ethos and Narrative Interpretation: The Negotiation of Values in Fiction. Lincoln, US: U of Nebraska Press.
- Kozel, Susan. 1996. “The Diabolical Strategy of Mimesis: Luce Irigaray’s Reading of Maurice Merleau‐Ponty.” Hypatia 11 (3): 114–129. https://doi.org/10.1111/j.1527-2001.1996.tb01018.x
- Kranke, Derrick A., Jerry Floersch, Bridget O. Kranke, and Michelle R. Munson. 2011. “A Qualitative Investigation of Self-Stigma among Adolescents Taking Psychiatric Medication.” Psychiatric Services (Washington, D.C.) 62 (8): 893–899. https://doi.org/10.1176/ps.62.8.pss6208_0893
- Larkey, Linda K., and Michael Hecht. 2010. “A Model of Effects of Narrative as Culture-Centric Health Promotion.” Journal of Health Communication 15 (2): 114–135. https://doi.org/10.1080/10810730903528017
- Lau, Patrick W. C., Antoinette Lee, and Lynda Ransdell. 2007. “Parenting Style and Cultural Influences on Overweight Children’s Attraction to Physical Activity.” Obesity (Silver Spring, Md.) 15 (9): 2293–2302. https://doi.org/10.1038/oby.2007.272
- Lely, Jeannette C. G., Geert E. Smid, Ruud A. Jongedijk, Jeroen W. Knipscheer, and Rolf J. Kleber. 2019. “The Effectiveness of Narrative Exposure Therapy: A Review, Meta-Analysis and Meta-Regression Analysis.” European Journal of Psychotraumatology 10 (1): 1550344. https://doi.org/10.1080/20008198.2018.1550344
- Lewis, Sophie, Samantha L. Thomas, R. Warwick Blood, David J. Castle, Jim Hyde, and Paul A. Komesaroff. 2011. “How Do Obese Individuals Perceive and Respond to the Different Types of Obesity Stigma That They Encounter in Their Daily Lives? A Qualitative Study.” Social Science & Medicine (1982) 73 (9): 1349–1356. https://doi.org/10.1016/j.socscimed.2011.08.021
- Lewis, Stephen T., and Marieke van Puymbroeck. 2008. “Obesity-Stigma as a Multifaceted Constraint to Leisure.” Journal of Leisure Research 40 (4): 574–588. https://doi.org/10.1080/00222216.2008.11950153
- Lillis, Jason, Jason B. Luoma, Michael E. Levin, and Steven C. Hayes. 2010. “Measuring Weight Self‐Stigma: The Weight Self‐Stigma Questionnaire.” Obesity (Silver Spring, Md.) 18 (5): 971–976. https://doi.org/10.1038/oby.2009.353
- Link, Bruce G., and Jo. C. Phelan. 2001. “Conceptualizing Stigma.” Annual Review of Sociology 27 (1): 363–385. https://doi.org/10.1146/annurev.soc.27.1.363
- Lu, Y., P. Duller, P. G. M. Van Der Valk, and A. W. M. Evers. 2003. “Helplessness as Predictor of Perceived Stigmatization in Patients with Psoriasis and Atopic Dermatitis.” Dermatology and Psychosomatics / Dermatologie Und Psychosomatik 4 (3): 146–150. https://doi.org/10.1159/000073991
- Lukyanenko, Roman, Jeffrey Parsons, Yolanda Wiersma, Renee Sieber, and Mahed Maddah. 2016. “Participatory Design for User-Generated Content: Understanding the Challenges and Moving Forward.” Scandinavian Journal of Information Systems 28 (1): 2.
- Lupton, Deborah. 2018. Fat. London, UK: Routledge.
- Maxwell, Deborah, Chris Speed, Karl Monsen, and Diego Zamora. 2015. “Creating a Collaborative Space for Creativity through a Pervasive User Experience.” Paper Presented at the Proceedings of the 2015 ACM SIGCHI Conference on Creativity and Cognition. https://doi.org/10.1145/2757226.2757234
- McLean, Kate C., and Moin Syed. 2015. “Personal, Master, and Alternative Narratives: An Integrative Framework for Understanding Identity Development in Context.” Human Development 58 (6): 318–349. https://doi.org/10.1159/000445817
- Meretoja, Hanna. 2017. The Ethics of Storytelling: Narrative Hermeneutics, History, and the Possible. Oxford, UK: Oxford University Press.
- Milaneschi, Yuri, W. Kyle Simmons, Elisabeth F. C. van Rossum, and Brenda W. J. H. Penninx. 2019. “Depression and Obesity: evidence of Shared Biological Mechanisms.” Molecular Psychiatry 24 (1): 18–33. https://doi.org/10.1038/s41380-018-0017-5
- Moenandar, Sjoerd-Jeroen. 2018. “When Not to Tell Stories: Unnatural Narrative in Applied Narratology.” Frontiers of Narrative Studies 4 (1): 6–20. https://doi.org/10.1515/fns-2018-0002
- Monaghan, Lee F. 2017. “Re-Framing Weight-Related Stigma: From Spoiled Identity to Macro-Social Structures.” Social Theory & Health 15 (2): 182–205. https://doi.org/10.1057/s41285-016-0022-1
- Mouffe, Chantal. 1999. “Deliberative Democracy or Agonistic Pluralism?.” Social Research 66 (3): 745–758.
- Myers, Anne, and James C. Rosen. 1999. “Obesity Stigmatization and Coping: relation to Mental Health Symptoms, Body Image, and Self-Esteem.” International Journal of Obesity and Related Metabolic Disorders: journal of the International Association for the Study of Obesity 23 (3): 221–230. https://doi.org/10.1038/sj.ijo.0800765
- Norman, Donald A. 1999. “Affordance, Conventions, and Design.” Interactions 6 (3): 38–43. https://doi.org/10.1145/301153.301168
- Pachankis, John. 2007. “The Psychological Implications of Concealing a Stigma: A Cognitive–Affective–Behavioral Model.” Psychological Bulletin 133 (2): 328–345. https://doi.org/10.1037/0033-2909.133.2.328
- Papadopoulos, Stephanie, and Leah Brennan. 2015. “Correlates of Weight Stigma in Adults with Overweight and Obesity: A Systematic Literature Review.” Obesity (Silver Spring, Md.) 23 (9): 1743–1760. https://doi.org/10.1002/oby.21187
- Paradies, Yin, João Luiz Bastos, and Naomi Priest. 2016. “Prejudice, Stigma, Bias, Discrimination, and Health.” In The Cambridge Handbook of the Psychology of Prejudice, edited by Chris G. Sibley and Fiona Kate Barlow, 559–581. Cambridge: Cambridge University Press.
- Parrott, Scott, Francesca R. Dillman Carpentier, and C. Temple Northup. 2017. “A Test of Interactive Narrative as a Tool against Prejudice.” Howard Journal of Communications 28 (4): 374–389. https://doi.org/10.1080/10646175.2017.1300965
- Pascoe, Elizabeth A., and Laura Smart Richman. 2009. “Perceived Discrimination and Health: A Meta-Analytic Review.” Psychological Bulletin 135 (4): 531–554. https://doi.org/10.1037/a0016059
- Pasupathi, Monisha, and Jacob Billitteri. 2015. “Being and Becoming through Being Heard: Listener Effects on Stories and Selves.” International Journal of Listening 29 (2): 67–84. https://doi.org/10.1080/10904018.2015.1029363
- Pearl, Rebecca L. 2018. “Weight Bias and Stigma: Public Health Implications and Structural Solutions.” Social Issues and Policy Review 12 (1): 146–182. https://doi.org/10.1111/sipr.12043
- Phelan, Jo, Bruce G. Link, and John F. Dovidio. 2008. “Stigma and Prejudice: One Animal or Two?” Social Science & Medicine (1982) 67 (3): 358–367. https://doi.org/10.1016/j.socscimed.2008.03.022
- Pucci, Andrea, and Rachel L. Batterham. 2020. “Endocrinology of the Gut and the Regulation of Body Weight and Metabolism.” Endotext [internet], edited by Feingold K. R., Anawalt, B., Blackman, M. R., et al. South Darmouth: MDText.com Inc.
- Puhl, Rebecca M., and Chelsea A. Heuer. 2009. “The Stigma of Obesity: A Review and Update.” Obesity (Silver Spring, Md.) 17 (5): 941–964. https://doi.org/10.1038/oby.2008.636
- Puhl, Rebecca M., and Chelsea A. Heuer. 2010. “Obesity Stigma: Important Considerations for Public Health.” Framing Health Matters 100 (6): 1019–2010.
- Puhl, R. M., J. D. Latner, K. O'Brien, J. Luedicke, S. Danielsdottir, and M. Forhan. 2015. “A Multinational Examination of Weight Bias: Predictors of Anti-fat Attitudes across Four Countries.” International Journal of Obesity 39 (7): 1166–1173. https://doi.org/10.1038/ijo.2015.32
- Puhl, Rebecca M., Marlene B. Schwartz, and Kelly D. Brownell. 2005. “Impact of Perceived Consensus on Stereotypes about Obese People: A New Approach for Reducing Bias.” Health Psychology: official Journal of the Division of Health Psychology, American Psychological Association 24 (5): 517–525. https://doi.org/10.1037/0278-6133.24.5.517
- Puhl, Rebecca M., and Young Suh. 2015. “Health Consequences of Weight Stigma: Implications for Obesity Prevention and Treatment.” Current Obesity Reports 4 (2): 182–190. https://doi.org/10.1007/s13679-015-0153-z
- Quinn, Diane M., and Stephenie R. Chaudoir. 2009. “Living with a Concealable Stigmatized Identity: The Impact of Anticipated Stigma, Centrality, Salience, and Cultural Stigma on Psychological Distress and Health.” Journal of Personality and Social Psychology 97 (4): 634–651. https://doi.org/10.1037/a0015815
- Reid, Allecia E., John F. Dovidio, Estrellita Ballester, and Blair T. Johnson. 2014. “HIV Prevention Interventions to Reduce Sexual Risk for African Americans: The Influence of Community-Level Stigma and Psychological Processes.” Social Science & Medicine (1982) 103: 118–125. https://doi.org/10.1016/j.socscimed.2013.06.028
- Richman, Laura Smart, and Micah R. Lattanner. 2014. “Self-Regulatory Processes Underlying Structural Stigma and Health.” Social Science & Medicine (1982) 103: 94–100. https://doi.org/10.1016/j.socscimed.2013.12.029
- Robroek, Suzan J. W., Anne Rongen, Coos H. Arts, Ferdy W. H. Otten, Alex Burdorf, and Merel Schuring. 2015. “Educational Inequalities in Exit from Paid Employment among Dutch Workers: The Influence of Health, Lifestyle and Work.” PLoS One 10 (8): e0134867. https://doi.org/10.1371/journal.pone.0134867
- Roth, Christian, Peter Vorderer, and Christoph Klimmt. 2009. “The Motivational Appeal of Interactive Storytelling: Towards a Dimensional Model of the User Experience.” In Interactive Storytelling: Second Joint International Conference on Interactive Digital Storytelling, ICIDS 2009, edited by Ido A. Iurgel, Nelson Zagalo and Paolo Petta, 38–43. Guimarães, Portugal: Springer.
- Saguy, Abigail C., and Kjerstin Gruys. 2010. “Morality and Health: News Media Constructions of Overweight and Eating Disorders.” Social Problems 57 (2): 231–250. https://doi.org/10.1525/sp.2010.57.2.231
- Scambler, Graham. 2009. “Health‐Related Stigma.” Sociology of Health & Illness 31 (3): 441–455. https://doi.org/10.1111/j.1467-9566.2009.01161.x
- Shen, Fuyuan, Vivian C. Sheer, and Ruobing Li. 2015. “Impact of Narratives on Persuasion in Health Communication: A Meta-Analysis.” Journal of Advertising 44 (2): 105–113. https://doi.org/10.1080/00913367.2015.1018467
- Stangl, Anne L., Valerie A. Earnshaw, Carmen H. Logie, Wim van Brakel, Leickness C. Simbayi, Iman Barré, and John F. Dovidio. 2019. “The Health Stigma and Discrimination Framework: A Global, Crosscutting Framework to Inform Research, Intervention Development, and Policy on Health-Related Stigmas.” BMC Medicine 17 (1): 31. https://doi.org/10.1186/s12916-019-1271-3
- Syed, Moin. 2015. “Theoretical and Methodological Contributions of Narrative Psychology to Ethnic Identity Research.” In Studying Ethnic Identity: Methodological and Conceptual Approaches Across Disciplines, edited by C. E. Santos and A. J. Umaña-Taylor, 27–54. New York, US: American Psychological Association. https://doi.org/10.1037/14618-003
- Teachman, Bethany A., Kathrine D. Gapinski, Kelly D. Brownell, Melissa Rawlins, and Subathra Jeyaram. 2003. “Demonstrations of Implicit anti-Fat Bias: The Impact of Providing Causal Information and Evoking Empathy.” Health Psychology: official Journal of the Division of Health Psychology, American Psychological Association 22 (1): 68–78. https://doi.org/10.1037//0278-6133.22.1.68
- Tomiyama, A. Janet. 2014. “Weight Stigma is Stressful. A Review of Evidence for the Cyclic Obesity/Weight-Based Stigma Model.” Appetite 82: 8–15. https://doi.org/10.1016/j.appet.2014.06.108
- Tomiyama, A. Janet, Laura E. Finch, Angela C. Incollingo Belsky, Julia Buss, Carrie Finley, Marlene B. Schwartz, and Jennifer Daubenmier. 2015. “Weight Bias in 2001 versus 2013: Contradictory Attitudes among Obesity Researchers and Health Professionals.” Obesity (Silver Spring, Md.) 23 (1): 46–53. https://doi.org/10.1002/oby.20910
- Vaes, Kristof, Pieter Jan Stappers, Achiel Standaert, and Kristine Desager. 2012. “Contending Stigma in Product Design: using Insights from Social Psychology as a Stepping Stone for Design Strategies.” Paper Presented at the out of Control; Proceedings of the 8th International Conference on Design and Emotion, London, Great Britain, 11-14 Sept. 2012.
- van Amsterdam, Noortje, and Dide van Eck. 2019. “‘I Have to Go the Extra Mile’. How Fat Female Employees Manage Their Stigmatized Identity at Work.” Scandinavian Journal of Management 35 (1): 46–55. https://doi.org/10.1016/j.scaman.2018.10.002
- Van Beugen, S., H. Van Middendorp, M. Ferwerda, J. V. Smit, M. E. J. Zeeuwen‐Franssen, E. B. M. Kroft, E. M. G. J. De Jong, A. R. T. Donders, P. C. M. Van de Kerkhof, and A. W. M. Evers. 2017. “Predictors of Perceived Stigmatization in Patients with Psoriasis.” The British Journal of Dermatology 176 (3): 687–694. https://doi.org/10.1111/bjd.14875
- van der Valk, Eline S., Erica L. T. van den Akker, Mesut Savas, Lotte Kleinendorst, Jenny A. Visser, Mieke M. Van Haelst, Arya M. Sharma, and Elisabeth F. C. van Rossum. 2019. “A Comprehensive Diagnostic Approach to Detect Underlying Causes of Obesity in Adults.” Obesity Reviews: An Official Journal of the International Association for the Study of Obesity 20 (6): 795–804. https://doi.org/10.1111/obr.12836
- Van Laer, Tom, Ko De Ruyter, Luca M. Visconti, and Martin Wetzels. 2013. “The Extended Transportation-Imagery Model: A Meta-Analysis of the Antecedents and Consequences of Consumers’ Narrative Transportation.” Journal of Consumer Research 40 (5): 797–817. https://doi.org/10.1086/673383
- Vandenbroeck, Philippe, Jo Goossens, and Marshall Clemens. 2010. Foresight: Tackling Obesities: Future Choices. Obesity System Atlas: Government Office for Science.
- Vegt, Niko, Valentijn Visch, Arnold Vermeeren, and Huib de Ridder. 2016. “Player Experiences and Behaviors in a Multiplayer Game: Designing Game Rules to Change Interdependent Behavior.” International Journal of Serious Games 3 (4), 69-85. https://doi.org/10.17083/ijsg.v3i4.150
- Visch, V. T., N. J. H. Vegt, H. Anderiesen, and K. Van der Kooij. 2013. “Persuasive Game Design: A Model and Its Definitions.” Proceedings of CHI 2013: Workshop Designing Gamification: Creating Gameful and Playful Experiences, Paris, France, 27 April-2 May 2013
- Vyncke, Bart, and Baldwin Van Gorp. 2020. “Using Counterframing Strategies to Enhance anti-Stigma Campaigns Related to Mental Illness.” Social Science & Medicine (1982) 258: 113090. https://doi.org/10.1016/j.socscimed.2020.113090
- Weiss, Mitchell G., Jayashree Ramakrishna, and Daryl Somma. 2006. “Health-Related Stigma: rethinking Concepts and Interventions.” Psychology, Health & Medicine 11 (3): 277–287. https://doi.org/10.1080/13548500600595053
- Whitley, Rob., Kathleen C. Sitter, Gavin Adamson, and Victoria Carmichael. 2020. “Can Participatory Video Reduce Mental Illness Stigma? Results from a Canadian Action-Research Study of Feasibility and Impact.” BMC Psychiatry 20 (1): 16. https://doi.org/10.1186/s12888-020-2429-4
- Wiese, Helen J., John F. Wilson, R. A. Jones, and M. Neises. 1992. “Obesity Stigma Reduction in Medical Students.” International Journal of Obesity and Related Metabolic Disorders: journal of the International Association for the Study of Obesity 16 (11): 859–868.
- Winskell, Kate, Gaëlle Sabben, and Christopher Obong’o. 2019. “Interactive Narrative in a Mobile Health Behavioral Intervention (Tumaini): Theoretical Grounding and Structure of a Smartphone Game to Prevent HIV among Young Africans.” JMIR Serious Games 7 (2): e13037. https://doi.org/10.2196/13037
- Ziebland, Sue, and Sally Wyke. 2012. “Health and Illness in a Connected World: How Might Sharing Experiences on the Internet Affect People’s Health?” The Milbank Quarterly 90 (2): 219–249. https://doi.org/10.1111/j.1468-0009.2012.00662.x
- Zussman, Robert. 2012. “Narrative Freedom.” Sociological Forum 27 (4): 807–824. https://doi.org/10.1111/j.1573-7861.2012.01357.x