Abstract
HIV community peer navigators and treatment officers are important sources of information and guidance for people living with HIV. We conducted an anonymous online survey with members of the treatment outreach network of the Australian National Association of People Living with HIV. The survey explored understandings and acceptance of HIV cure research and was disseminated before and following an interactive workshop on HIV cure. We demonstrated an improvement in understandings of HIV cure science and increased willingness to participate in interventional clinical trials after the workshop. Concerns around interrupting HIV treatment and detrimental impacts on health were identified as barriers to participation. Altruism was a motivator to enrol in HIV cure trials, along with endorsement from a trusted member of community.
Scientific and community interest in curing human immunodeficiency virus (HIV) has increased over the last decade, and there are currently over 100 trials focusing on HIV cure being conducted worldwide [Citation1]. Many of these trials involve interventions that are not expected to provide personal medical benefit to participants and could potentially cause adverse effects [Citation2]. Therefore, enrolment in these studies often relies on the altruism of the people with HIV (PHIV) who choose to participate. Australia has a relatively small population of PHIV (<30,000 people), however has been an active site investigating HIV cure strategies and interventions aimed at achieving remission, or durable control of virus in the absence of antiretroviral therapy [Citation3]. Australia has a universal healthcare system, with subsidised access to HIV care and antiretroviral therapy irrespective of citizenship status.
Studies exploring community (in this case referring to people living with HIV, and affected by HIV, and the organisations that represent them) expectations and motivations to participate in HIV cure research are required to improve recruitment and community interest in the field. It is also critical that HIV cure research is done ethically and in ways that communities find acceptable [Citation4]. One important component of HIV cure clinical trials are antiretroviral treatment interruptions (ATIs), where clinical, virological, and immunological parameters are closely monitored while off HIV treatment. ATIs are increasingly used as they are one of the most robust clinical outcomes to test an intervention aimed at controlling or curing HIV [Citation5]. Importantly all international HIV treatment guidelines recommend uninterrupted ART to treat HIV, so there are significant ethical and clinical challenges to implementing ATIs into trials for both PHIV and their providers [Citation6–8]. There is a critical need to document people with HIV’s understandings of ATIs, acceptance of the practice, and their willingness to participate in these types of trials.
The National Association of People Living with HIV Australia (NAPWHA) is the peak representative organisation advocating for people with HIV in Australia. The Treatment Outreach Network is a group of peer educators from the Australian HIV community sector workforce who engage with PHIV to provide health and treatment information specific to HIV. An online survey was developed by NAPWHA, with collaborative input from HIV cure clinical researchers to assess current understandings and acceptability of HIV cure focused research amongst the Network, as part of an overarching effort to improve HIV cure scienc literacy.The non-validated survey tool was developed by NAPWHA executive members, to explore understandings of HIV cure science, interest in participating in cure research, and concerns about participating in cure research (Appendix 1). We also aimed to evaluate the impact of the intervention of providing an educational workshop on Australian HIV peer navigators.
The survey was disseminated amongst members of the Network in August 2022 (n = 20) and again following a 75-minute interactive workshop on HIV cure research (n = 15), conducted at a NAPWHA Treatment Officer Network meeting in Melbourne on the 9th of November 2022. The workshop included a presentation on the basics of HIV cure science from a clinical researcher and a question-and-answer discussion with a participant who had recently completed an HIV cure trial in Melbourne. The surveys were completed anonymously and were approved by the human ethics committee at Alfred Health (project no. 603/22). Questions were in the form of a five-point likert scale, for example ‘How would you assess your own knowledge/understand of HIV Cure research? Far above average/Above average/Average/Below average/Far below average’; or free text responses, such as ‘What would be some of your worries or concerns about participating in cure research?’. A descriptive analysis was conducted, with thematic qualitative analysis on free text answers.
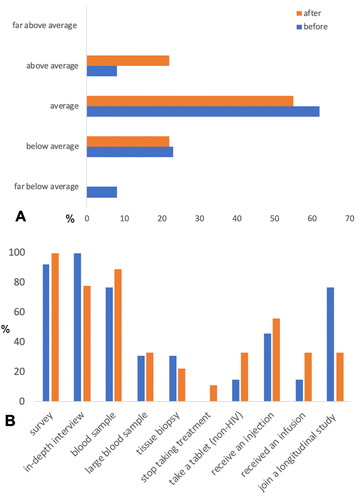
Thirteen Treatment Outreach Network members responded to the first survey, and 9 responded to the second survey. Similar proportions thought researchers were ‘somewhat not close’ or ‘not close’ to a cure (61% before vs 67% after workshop). Perceived understandings of HIV cure science increased following the interactive educational workshop. The number of respondents who stated that their knowledge and understanding of HIV cure research was ‘above average’ more than doubled from 8% before the workshop to 22% after (). Following the workshop, Network members were more willing to participate in studies where blood samples were collected, or studies that tested interventions such as a non-HIV tablet, injection, or infusion. Only one respondent was willing to stop HIV treatment in a cure study (no respondents were willing in the pre-workshop survey, ).
Figure 1. (A) Perceived knowledge and understanding of HIV cure research; (B) willingness to contribute to different types of HIV cure research.
The reluctance to interrupt HIV treatment for a cure trial is likely related to concerns around the safety of the trial process. When asked about worries or concerns about participating in cure research, an emphasis was placed on ‘stopping [HIV] treatment’ and the ‘ability to maintain undetectable viral load’. Another focus was potential harm to the individual’s health as noted by the following quotes: ‘potential negative side effects to any trial’, ‘danger to health’, the ‘experimental nature of some of the studies’ and worries about ‘[my] body being experimented on’. Another respondent raised the time commitment needed to participate in complex interventional trials as a deterrent to participation. The concerns identified mirrors findings from previous surveys exploring barriers to participation [Citation4, Citation9, Citation10].
Motivations to participate include ‘ending HIV’, ‘altruism’, and ‘doing my bit for humanity’. This is consistent with previous surveys of people with HIV in Australia [Citation10], including those who have completed HIV cure studies [Citation3]. These previous studies had found social and altruistic reasons, in particular the opportunity to help others as a driving motivating factor. One respondent also stated that an ‘endorsement by respected community members and organisations’ would motivate them to participate. This suggests that peer navigators and other HIV positive peers working in community-based organisations could play an important role in promoting or advocating for HIV cure research. While the importance of peer navigators in HIV treatment engagement and retention in care, including quality of life assessments, has been well established [Citation11], no studies have reported specific peer navigator education or interventions in the context of HIV cure research. This highlights an important avenue for community engagement in HIV cure science, that has not yet been thoroughly explored. This work also demonstrates that it is pertinent that HIV peer navigators understand the current landscape of HIV cure science.
This study was limited by the small sample size of those currently active in providing HIV treatment related information at a community base level. As the surveys were completed anonymously, we cannot confirm if the same people completed both surveys. However, this is the first study to measure the impact of an interactive educational workshop on HIV cure.
This study demonstrated that a brief interactive workshop on HIV cure research improved participants understandings of HIV cure science. Interest in interventional studies and treatment interruption may have increased amongst this group following the workshop, however concerns around the safety of HIV cure research were expressed. To address these concerns, in particular the reluctance to undertake ATIs, further collaboration between community, clinicians and researchers is required. Specifically, discussion and education around the known and potential risks of interrupting HIV treatment, and the role of HIV pre-exposure prophylaxis for sero-discordent sexual partners during ATIs.
HIV peer navigators could play an important role for broader communication of HIV cure science to community members, because of their existing links to PHIV and because they are already trusted sources of information about HIV among some PHIV. Furthermore, peer navigator can be valuable contributors to the co-design of prospective HIV cure clinical studies, in light of their lived experiences and perspectives from within the HIV community. This study also demonstrated that collaborations across researchers, community-based organisations and HIV positive peers is potentially a productive way forward for communication of HIV cure research and science. Specific educational activities linking community-based organisations and HIV peer navigators to researchers should therefore be prioritised.
Appendix 1 Cure survey TON.docx
Download MS Word (30.4 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Jefferys R. Research toward a cure trials treatment action group 2022 [updated November 15, 2022; cited 2022 4th December]. Available from: http://www.treatmentactiongroup.org/cure/trials.
- Pitman MC, Lau JSY, McMahon JH, et al. Barriers and strategies to achieve a cure for HIV. Lancet HIV. 2018;5(6):e317–e28.
- McMahon JH, Elliott JH, Roney J, et al. Experiences and expectations of participants completing an HIV cure focused clinical trial. AIDS. 2015;29(2):248–250.
- Dubé K, Evans D, Dee L, et al. “We need to deploy them very thoughtfully and carefully”: perceptions of analytical treatment interruptions in HIV cure research in the United States-a qualitative inquiry. AIDS Res Hum Retroviruses. 2017;34(1):67–79.
- Lau JSY, Smith MZ, Lewin SR, et al. Clinical trials of antiretroviral treatment interruption in HIV-infected individuals. AIDS. 2019;33(5):773–791.
- BHIVA guidelines on antiretroviral treatment for adults living with HIV-1 2022. HIV Med. 2022;23 Suppl 3:3–14.
- Australasian Society for HIV, Viral Hepatitis and Sexual Health Medicine Antiretroviral Guidelines. US DHHS Guidelines with Australian commentary: ASHM; 2019 updated December 2019]. Available from: https://arv.ashm.org.au.
- EACS. EACS Guidelines 2021, 11th edition: Available from: https://www.eacsociety.org/media/final2021eacsguidelinesv11.0_oct2021.pdf.
- Lau JSY, Smith MZ, Allan B, et al. Perspectives on analytical treatment interruptions in people living with HIV and their health care providers in the landscape of HIV cure-Focused studies. AIDS Res Hum Retroviruses. 2019;36(4):260–267.
- Power J, Westle A, Dowsett GW, et al. Perceptions of HIV cure research among people living with HIV in Australia. PLoS One. 2018;13(8):e0202647.
- Krulic T, Brown G, Bourne A. A scoping review of peer navigation programs for people living with HIV: Form, function and effects. AIDS Behav. 2022; Dec26(12):4034–4054.

