Abstract
Background
Paediatric HIV data shows a variable and sometimes catastrophic response in the initial stage of ART regimen administration. The burden of disease that affects children in their first year of treatment is not comprehensively available.
Objective
Objective of our study was to describe patterns of admission in children; before ART initiation, within the first six months, and post-six months of ART between 2001 and 2016.
Methods
Principal caregivers of 260 children (45.7% females 54.2% males, all <15 years) on ART for at least six months were interviewed about admissions of their children. Diagnoses were verified from the health passport books. Data on age, sex, date of ART initiation was obtained from the database of Baylor College of Medicine in Lilongwe. Data were analysed using Excel for descriptive analysis. Chi Square Test was used to test for significance.
Results
There were more admissions before starting ART 74% (95%CI 68.67–79.33%) vs. 42% (95%CI 36.00–48.00%), after starting ART (p = <0.001 at 5% significance level); after six months of ART 34% (95%CI 28.24–39.76) vs. 20% (95% CI 15.51–24.86%) (p = <0.001 at 5% significance level). The commonest causes of admission were pneumonia, malaria, tuberculosis, anaemia; no difference in causes of admission within the first and after six months of ART initiation.
Conclusion
ART significantly reduces admission in children living with HIV. The common causes of admission are HIV non-specific conditions. No difference between causes of admission within and after six months of ART.
Introduction
Substantial progress has been made in the management of paediatric HIV infection with the implementation of mother-to-child-prevention programmes and the introduction of antiretroviral therapy (ART) [Citation1–3]. However, an estimated 1.5 million children are still living with HIV, of whom 85% million live in sub-Saharan Africa [Citation1]. In Malawi by 2020, 65,000 children aged 0–14 were living with HIV and 79% of these children were on antiretroviral therapy [Citation4].
Many studies have been done on the effectiveness and outcomes of ART in adults living with HIV [Citation5–9]. In paediatrics, HIV data shows a variable and sometimes a catastrophic response in the initial stage of ART regimen administration [Citation10–14]. Adult response to ART and the burden of disease that affects them has been extensively studied. Adult studies have shown that tuberculosis (TB), Cryptococcus meningitis, chronic diarrhoea, Kaposi Sarcoma, wasting, and bacterial infections are the commonest causes of admission in the HIV positive population in Sub-Saharan Africa including Malawi. In addition, it has been shown that most admissions occur within the first 3 months of ART initiation and that male gender is associated with higher mortality [Citation10,Citation12,Citation13,Citation15–17].
A South African cohort study in children living with HIV, found that 85% of deaths occurred in the first six months of ART. Of these deaths, 28% died due to TB while 18% due to diarrhoea, dehydration, and malnutrition. Interestingly, this study found that female gender and age group below three was associated with higher mortality. These findings are contrary to the adult study above [Citation18].
A study, done in Thailand, showed that the first 6 months of ART are associated with most admissions and that ART significantly reduces admission in the subsequent 6 months. In addition, the causes of admissions were pneumonia and other bacterial infections [Citation19]. Similar to the above finding, a Malaysian study found that in children, mortality was high in the first six months and there was a strong association with malnutrition [Citation20]. In addition, Ethiopian prospective cohort study found that nearly two-thirds of the admissions were within 6 months of initiation of ART; and the presence of opportunistic infections and duration of ART were the only predictors of admission [Citation11]. However, contrary to the findings of the two studies above, a multicentre prospective West Africa study found that 75% of causes of admission in this population were HIV defining condition [Citation21].
A retrospective cohort study was done at the same site as our study assessed clinical factors associated with mortality among HIV-exposed infants and children living with HIV of <18 years. They found that opportunistic infections and malnutrition made a significant contribution to mortality in children living with HIV on ART. The most encountered outpatient diagnoses before outpatient mortality were pneumonia, gastroenteritis, and malaria. It was noted that poor nutritional status and female gender were among the factors associated with mortality [Citation14].
The studies reviewed suggest that in the children living with HIV: causes of admission are variable; first six months of ART are associated with high prevalence of admission and mortality; age group below three and female gender may be associated with mortality.
Due to the scarcity of studies on admission and disease burden as well as the incomplete and contradictory findings of the studies in our literature review, we conducted a study that would help us understand the response of children to ART, the disease burden in age, and sex differences in Malawian children population. Our overall objective was to describe admission patterns of children on antiretroviral therapy in Lilongwe, Malawi. Our specific objectives were to compare pre-ART and post-ART prevalence of admissions; to estimate the prevalence of admission in children within first and post-six months of ART; to identify the most common diseases leading to admission within and after six months; and to describe the disease burden by age groups and sex within and after six months of ART.
Methodology
Study place
The study was conducted at Baylor College of Medicine, a non-governmental organisation in Lilongwe, which focuses on paediatric HIV, situated at Kamuzu Central Hospital. This site was chosen because it gave a platform where we could meet the guardians as well as extract the information we needed from the database of the institution.
Study population
The study participants were from Lilongwe rural and urban areas who go to Baylor College of Medicine clinic. We included children on ART for more than 6 months but <15 years of age. Defaulters, those with no documentation of the diagnoses, and those who did not come with primary guardians were excluded from the study. In terms of age, we categorised into those <2 years of age and those above 2 years. The assumption was the first 2 years of vertical transmission of HIV are critical to the baby [Citation22].
Study period
The study period was from 1st September to 10th October 2016.
Study design, sample size, sampling technique
It was a retrospective quantitative cross-sectional study. The target sample size was 362 and it was calculated using a formula N = Z2P(1 − P)/e2 with Z = 1.96 and p = 62% (prevalence of admission in children on ART within the first 6 months found in one study) and error marginal of 5.0% [Citation19]. A convenient sampling technique was employed.
Data collection
Primary data was collected through interviews with guardians and documented on a case report form. The guardians were asked if they were the primary guardian of the child. The guardian was asked to recall if the child ever got admitted/admitted. If yes, the documentation of the admissions was checked in the health-passports. If there is no documentation the participant was left out of the study. The primary data collected included: age of child, pre-ART admissions, and all admissions and diagnoses after ART. Secondary data was taken from health passports and hospital registers, medical records, and local databases. This included date of ART initiation, duration on ART, and diagnoses on admission. We compared the date of diagnosis and date of ART initiation to decide if the admission was pre-ART, within six months of ART, or six months post ART.
Data management and analysis
Paper Case Report Forms data was manually transferred to an electronic database (Microsoft Excel 2010). Data anonymised to preserve confidentiality. Only designated investigators had access to the database. The data was analysed using simple statistical techniques in excel, to evaluate mean, median, and mode of age, height, and weight for descriptive statistics. Chi-square tests were used for comparisons.
Ethical consideration
Our study was approved by the Kamuzu University of Health Sciences Research Ethics Committee (previously University of Malawi College of Medicine) approval number: MBBS/08/16/01. Baylor College of Medicine gave us permission to conduct the study at their institution. A written informed consent, to interview them as well as extract data from the database, was read out to the participants in Chichewa and signed thereafter. Caretakers who assented were interviewed for a maximum of 10 min because children could not consent and due to issues of disclosure.
When interviewing the parents/guardians the term ‘HIV/AIDS’ was not mentioned because some of the children had not been disclosed yet. Unique identifier numbers were used to record patients rather than names. The data collected was not handed to anyone else except the research team. No names were recorded. Non-invasive procedures were done. No identifiable information is presented in this manuscript.
Results
Demographics
We collected data from 260 participants. Out of the 260 participants, 119 (45.9%) were female and 141 (54.2%) were male with an average of 9.2 years. The average age at HIV diagnosis was 2 years 10 months. The average duration of ART was 5 years and 5 months. The average number of admissions pre-ART was 0.95, six months into ART was 0.3, and six months post-ART initiation was 0.35.
Prevalence of admission
Prevalence of admission before ART was 74% (95%CI 68.67–79.33%) while after ART initiation was 42% (95%CI 36.00–48.00%), p = <0.001 at 5% level of significance. In terms of the total number of admissions, there were 249 admissions before the initiation of ART and 206 admissions after the initiation of ART (). Prevalence of admission within the first six months of ART was 20% (95% CI 15.51–24.86%) while six months after ART initiation was 34% (95%CI 28.24–39.76), p = <0.001 at 5% level of significance ().
Table 1. Prevalence of admissions before and after ART initiation.
Table 2. Prevalence of admission in the first 6 months of ART and after.
Causes of admission within and after six months of ART
There was no difference in the causes of admission within and after six months of ART initiation p = >0.05 except for meningitis (p = <0.05). Both within the first six months and after six months of ART; pneumonia, malaria, and tuberculosis, were the leading causes of admissions ().
Table 3. Common cause of admission in children on ART.
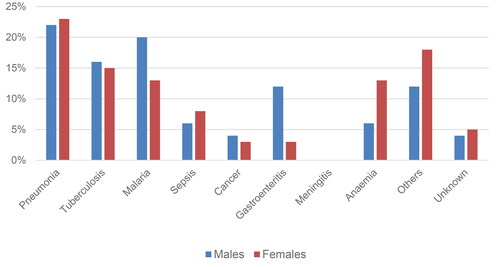
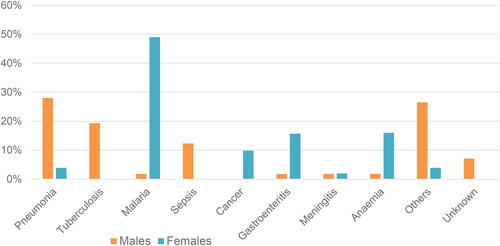
Causes of admission by gender
Females
Within the first six months, pneumonia, tuberculosis, and malaria were the leading causes of admission. After six months, malaria, anaemia, and gastroenteritis were the leading causes of admission ( and ).
Males
Both within and after six months of ART, pneumonia and tuberculosis were the leading causes of admission.
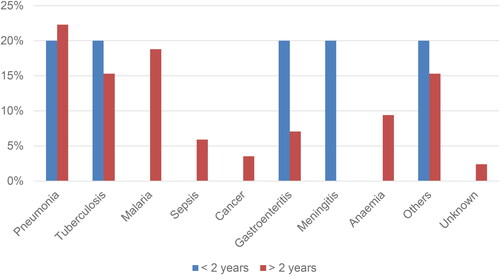
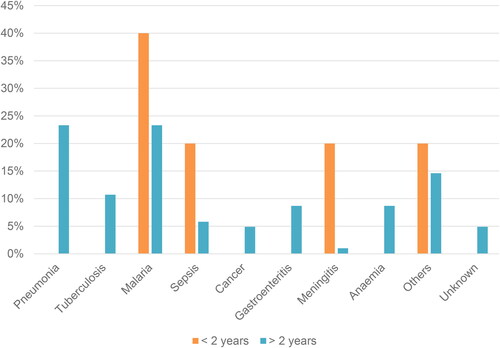
Causes of admission by age group
Less or equal to 2 years
Within the first six months of ART, pneumonia, tuberculosis, gastroenteritis, and meningitis contributed equally to the total disease burden. After six months, malaria was the leading cause of admission ( and ).
More than 2 years
Pneumonia, malaria, and tuberculosis were the leading causes of admission both within and after six months of ART ( and ).
Discussion
Our study has shown a significant reduction in the number of children who got admitted after initiating ART. A study done in India [Citation19] noted the same trend in a similar population of people. As such, the fact that in Malawi only 79% of the HIV positive children on ART calls for extra effort to bring the remaining 21% into HIV care [Citation4]. There is a need to develop novel strategies to retain children living with HIV in care. Comparing the absolute number of admissions there is no significant difference. One notable finding in our study in the post-ART group is that there were a few children who got sick multiple times and contributed to the increase in the absolute number of admissions. Others could get admitted up to seven times. We were wondering if this is the ‘catastrophic events’ described in other studies [Citation18,Citation20]. However, this observation could be because the children were already very sick at the time of ART initiation, not that it is really ART related; due to poor adherence to ART; or due to other underlying diseases not even related to HIV. Hence, this warrants further research.
Our assumption was that children in the first six months of ART should get admitted more often therefore leading to higher rates of admission since their immune system has not yet improved. Contrary to this, we observed a higher prevalence of admission in the post six months of ART period. Some studies have shown that the first six months of ART are associated with high mortality [Citation18,Citation20]. Since we did not have a technically efficient way of including all children who had died, the dead group could explain the high rates of admission that have been observed in other studies [Citation11]. Another line of thought would be due to the long period of observation after six months of treatment (some participants up to 14 years on ART). So, since this period is longer than just the first six months of ART, those in this category stand a higher chance of getting admitted more due to time factor. Likely, if the analysis was limited to 6, 12, or 18-months period after ART, the observed increase in admission would disappear. In addition, after initiating ART, there is more likelihood of more visits to the hospital as the guardian may be more sensitive to child sickness after counselling. Additionally, other admissions could be due HIV non-related diseases [Citation23,Citation24]. Nonetheless, our study has shown that the period before and immediately after starting ART could be very critical [Citation19].
We found causes of admission to be HIV non-defining conditions except for TB in both within and after six months of ART initiation. Similar to our findings, a study done at the same site found that the most commonly encountered OPD visit diagnoses were pneumonia, gastroenteritis, and malaria [Citation14,Citation23–26]. These are conditions that cause most of the admissions even in children who are not living with HIV. This observation was also seen in the study done in Thailand [Citation19]. Contrary to this, some West African studies [Citation18,Citation21] reported the causes of admission to be HIV related. This could be due to the 18 years age cut-off used in these two studies. Additionally, these two studies particularly focussed on opportunistic infections in their design. However, our study has shown that the disease burden affecting these children is not much different from general paediatric causes of admission [Citation27] except for TB. Therefore, scaling up the efforts to deal with these conditions at a national level should be able to curb this burden too.
Our study did not find any significant difference in causes of admission within six and post-six months of ART period. For meningitis, the p-value shows some significance because in the ‘within six months category’ there is no one who ever got admitted. One reason for this finding could be that our facility was not representative. Baylor College of Medicine is a special facility not representative of what happens in the district health facilities. Secondly, deaths were excluded. Lastly, our sample size was limited. Hence a need for a study that can avoid these potential confounders.
Looking at disease burden by sex and age category, although there appear to be differences in disease burden, these results cannot be confidently applied to the public because our sample size was not powered to detect such differences between the groups. Additionally, the observed differences in diagnoses particularly in children <2 years old could be attributed to limited diagnostic capacity in this setting and loss to follow-up [Citation28]. Our study, however, gives a direction of what may be expected at a large scale.
Conclusion
Our study has shown that ART significantly reduces admissions; there are less admissions within the first six months of ART; common causes of admissions are the usual burden of disease in Malawi and tuberculosis; and there is no significant difference amongst the causes of admission within and after 6 months of being on ART.
Recommendations
There is a need for further studies on the causes of admissions and deaths during the first 6 months of ART. A case-control or cohort design that includes deaths would be a better design to confirm our findings.
Limitations of the study
This study used both primary and secondary data. Some guardians could not recall how many times their child got admitted. Some guardians lost health passport books for the children. Lack of, or vague documentation of the diagnosis in the health-passports. Most importantly, our study sample size is small in relation to the period in which our participants were spread such that due to dynamics in HIV diagnosis and diagnosis, it was slightly challenging to make definitive conclusions. The plan was to do the study at two sites, Lighthouse and Baylor College of Medicine, but data was collected only at Baylor College of Medicine. This may present a selection bias due to specialised patients that are seen in this facility. This was because Lighthouse deals mainly with teens who do not come with parents during clinics. The proposed sample size of 360 was not reached due to limited time funding as well as the reasons described above. We had a very skewed age group towards the older age group.
Acknowledgements
We would like to thank the late Dr. Kazembe of Baylor College of Medicine and his entire team for allowing us to conduct the study at their institution. This was undergraduate research work required for completion of a degree. The views expressed in this article are our own, not those of the Kamuzu University of Health Sciences. We developed the concept, designed the study, collected data, ran the analyses, and wrote the paper ourselves as students. This work was earlier presented at Paediatric and Child Health Association Conference in 2017, Kamuzu University of Health Sciences Research Dissemination Conference in 2017, and International Student Congress Of (Bio) Medical Science in 2018, Groningen, Netherlands.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Global HIV Programme [Internet]. [cited 2023 Oct 24]. Available from: https://www.who.int/teams/global-hiv-hepatitis-and-stis-programmes/hiv/treatment
- Mother-to-child transmission of HIV [Internet]. [cited 2023 Nov 17]. Available from: https://www.who.int/teams/global-hiv-hepatitis-and-stis-programmes/hiv/prevention/mother-to-child-transmission-of-hiv
- Prevention of Mother-to-Child HIV Transmission – Elizabeth Glaser Pediatric AIDS Foundation [Internet]. [cited 2023 Nov 17]. Available from: https://www.pedaids.org/our-expertise/prevention-of-mother-to-child-hiv-transmission/
- Malawi – EGPAF [Internet]. Elizabeth Glaser Pediatric AIDS Foundation. [cited 2023 Nov 16]. Available from: https://pedaids.org/country/malawi/
- Huang P, Tan J, Ma W, et al. Outcomes of antiretroviral treatment in HIV-infected adults: a dynamic and observational cohort study in Shenzhen, China, 2003–2014. BMJ Open. 2015;5(5):e007508.
- Evans D, Menezes C, Mahomed K, et al. Treatment outcomes of HIV-infected adolescents attending public-sector HIV clinics across Gauteng and Mpumalanga, South Africa. AIDS Res Hum Retroviruses. 2013;29(6):892–900.
- Oguntibeju O. Quality of life of people living with HIV and AIDS and antiretroviral therapy. HIV AIDS. 2012;4:117–124.
- Steegen K, Luchters S, Dauwe K, et al. Effectiveness of antiretroviral therapy and development of drug resistance in HIV-1 infected patients in Mombasa, Kenya. AIDS Res Ther. 2009;6(1):12.
- Ayele W, Mulugeta A, Desta A, et al. Treatment outcomes and their determinants in HIV patients on anti-retroviral treatment program in selected health facilities of Kembata and Hadiya zones, southern nations, nationalities and peoples region, Ethiopia. BMC Public Health. 2015;15(1):826.
- Chandrasekaran P, Shet A, Srinivasan R, et al. Long-term virological outcome in children receiving first-line antiretroviral therapy. AIDS Res Ther. 2018;15(1):23.
- Haileamlak A, Hagos T, Abebe W, et al. Predictors of hospitalization among children on ART in Ethiopia: a cohort study. Ethiop J Health Sci. 2017;27(Suppl 1):53–62.
- Mussa FM, Massawe HP, Bhalloo H, et al. Magnitude and associated factors of anti-retroviral therapy adherence among children attending HIV care and treatment clinics in Dar es Salaam, Tanzania. PLOS One. 2022;17(9):e0275420.
- Munthali T, Michelo C, Mee P, et al. Survival of children living with HIV on art in Zambia: a 13-years retrospective cohort analysis. Front Public Health. 2020;8:96.
- Rees CA, Flick RJ, Sullivan D, et al. An analysis of the last clinical encounter before outpatient mortality among children with HIV infection and exposure in Lilongwe, Malawi. PLOS One. 2017;12(1):e0169057.
- Gupta A, Nadkarni G, Yang WT, et al. Early mortality in adults initiating antiretroviral therapy (ART) in low- and middle-income countries (LMIC): a systematic review and meta-analysis. PLOS One. 2011;6(12):e28691.
- May M, Boulle A, Phiri S, et al. Prognosis of patients with HIV-1 infection starting antiretroviral therapy in sub-Saharan Africa: a collaborative analysis of scale-up programmes. Lancet. 2010;376(9739):449–457.
- Lewden C, Drabo YJ, Zannou DM, et al. Disease patterns and causes of death of hospitalized HIV-positive adults in West Africa: a multicountry survey in the antiretroviral treatment era. J Int AIDS Soc. 2014;17(1):18797.
- Zanoni BC, Phungula T, Zanoni HM, et al. Risk factors associated with increased mortality among HIV infected children initiating antiretroviral therapy (ART) in South Africa. PLOS One. 2011;6(7):e22706.
- Puthanakit T, Aurpibul L, Oberdorfer P, et al. Hospitalization and mortality among HIV-infected children after receiving highly active antiretroviral therapy. Clin Infect Dis. 2007;44(4):599–604.
- Moy FS, Fahey P, Nik Yusoff NK, et al. Outcomes of human immunodeficiency virus-infected children after anti-retroviral therapy in Malaysia: HIV infected children in Malaysia. J Paediatr Child Health. 2015;51(2):204–208.
- Dicko F, Desmonde S, Koumakpai S, et al. Reasons for hospitalization in HIV-infected children in West Africa. J Int AIDS Soc. 2014;17(1):18818.
- Shapiro RL, Lockman S. Mortality among HIV‐exposed infants: the first and final frontier. Clin Infect Dis. 2010;50(3):445–447.
- Bronzan RN, Taylor TE, Mwenechanya J, et al. Bacteremia in Malawian children with severe malaria: prevalence, etiology, HIV coinfection, and outcome. J Infect Dis. 2007;195(6):895–904.
- Gordon S, Graham S. Epidemiology of respiratory disease in Malawi. Malawi Med J. 2007;18(3):134–146.
- Nosek CA, Buck WC, Caviness AC, et al. Hospital admissions from a pediatric HIV care and treatment program in Malawi. BMC Pediatr. 2016;16(1):22.
- Molyneux EM, Tembo M, Kayira K, et al. The effect of HIV infection on paediatric bacterial meningitis in Blantyre, Malawi. Arch Dis Child. 2003;88(12):1112–1118.
- Phillips JA, Kazembe PN, Nelson EAS. A paediatric handbook for Malawi. 4th ed. Lilongwe: Baylor College of Medicine, Texas Children’s Hospital; 2015. p. 1–2.
- Mpinganjira S, Tchereni T, Gunda A, et al. Factors associated with loss-to-follow-up of HIV-positive mothers and their infants enrolled in HIV care clinic: a qualitative study. BMC Public Health. 2020;20(1):298.