Abstract
Objectives:
This survey explores how physicians perceive chronic non-cancer pain, and examines their opinions on current treatment options.
Methodology:
The computer-based survey comprises a questionnaire that is completed by physicians, mostly at professional conferences and congresses, but also online. The focus is on pain specialists, primary care physicians and other specialists (such as neurologists and rheumatologists), to discover any differences in their approach to treating chronic non-cancer pain.
Results:
No common understanding existed of where severe pain starts on an 11-point Numeric Rating Scale. Overall, two-thirds of respondents aim for treatment to reduce pain intensity to an NRS score of 2–4, with primary care physicians tending to aim for lower scores. All three groups considered reduction of pain to be the most important treatment goal, followed by quality of life. Asked to rank the most important factors when choosing an analgesic agent to treat severe, chronic non-cancer pain, respondents ranked efficacy first, tolerability second, and quality of life third. In each rank, more primary care physicians chose these options than in the specialist groups. More pain specialists used classical strong opioids often or very often – and for longer – than did physicians in the other two groups. Nausea/vomiting, bowel dysfunction and somnolence were ranked the first, second and third main reasons, respectively, for treatment failure with these agents. Over 90% of respondents used combination treatment rather than monotherapy to treat severe, chronic pain, but no fewer than 176 different combinations were cited.
Conclusions:
Pain reduction and improvement in quality of life are the most important treatment goals. Wide variation in treatment indicates that no single drug is particularly good for managing chronic pain, and suggests that current treatment is not evidence-based. Differences between the groups imply that first-line treatment is more cautious and conventional. The key limitations of this survey include its small sample size, informal implementation and lack of detail regarding the respondents surveyed.
Introduction
Various national and international guidelines have been developed for the treatment of chronic pain, and more recent recommendations take into account the underlying pain mechanisms involvedCitation1. However, there is evidence that the incorporation of guidelines into daily practice is marginalCitation2, and many physicians are reluctant to consult treatment algorithms regularly when treating chronic painCitation3. Among the barriers to implementation are lack of knowledge, shortage of time, disagreement with the guideline content, and confusion owing to the large number of guidelines receivedCitation4. It should not be surprising, therefore, that a 2008 survey by IMS Health found huge variations in the consumption of analgesics in different European countries, both in terms of quantity and the specific agents prescribed. Measured in patient treatment days per capita, overall analgesic consumption varied by a factor of 6, and the consumption of weak opioids by a factor of >20. This suggests that there is no general consensus as to what constitutes best practice in the management of chronic pain, and the treatment prescribed for a given pain condition is highly dependent on geographical location. The prescription of opioids, for example, is influenced by ethical, cultural and legislative considerations, particularly for patients with chronic non-cancer painCitation5,Citation6.
The CHANGE PAIN initiative, funded by Grünenthal GmbH, was begun in 2009 with the express intention of increasing the medical community’s understanding of chronic pain and improving pain therapy. To pursue these objectives, it funds relevant research and supports publication of the results. Another role is to produce continuing medical education (CME) materials; these currently include a range of evidence-based CME modules covering topics such as physician/patient communication and mechanism-orientated pain therapy, as well as local and regional workshops in various European countries.
Members of the international CHANGE PAIN Advisory Board are leading pain specialists from Europe and the USA, who were selected on the basis of their research activity and considerable experience in pain management. They meet regularly to discuss various aspects of pain management and develop guidance for healthcare professionals. The initiative was begun in Europe, but is expected to be rolled out in Latin America and Australia in the near future.
In September 2009 an international survey was begun, to explore how physicians from different disciplines perceive chronic non-cancer pain, and to elicit their opinions on current treatment options. This article presents an analysis of the results from the beginning of the survey until December 2010.
Methodology
The computer-based survey, which is endorsed by the European Federation of IASP Chapters (EFIC), takes the form of a questionnaire which is completed by the participants themselves. The nine questions (see Appendix 1) were identified following discussions by the international CHANGE PAIN Advisory Board. During 2009 and 2010 the survey was implemented – via touch screens in the Grünenthal booths – at 19 national and international congresses across Europe that were thought to be of particular relevance to physicians interested in pain management. All visitors could participate, but had to provide information on their specialty and country of origin. The survey has also been available on several CHANGE PAIN websites (International, Germany, Switzerland, Spain, UK, Ireland, Sweden, Denmark, Italy, Portugal) and been promoted by Grünenthal representatives who visit physicians from the relevant specialties. Participants have to register to validate their credentials. As no individuals have been specifically invited to participate and respondents are essentially self-selected, it is not possible to calculate a response rate, which is one limitation of the study. Results for the relevant period were automatically fed into a monitoring tool, provided by the agency (Antwerpes AG, Cologne, Germany) who performed the descriptive analysis of the findings. The p-values given are overall values comparing the three physician groups by a chi-square test, in order to show possible differences in treatment habits and opinions. These values were calculated by a Grünenthal statistician.
The focus is on three different groups of healthcare professionals – pain specialists (anesthesiology, pain medicine), primary care physicians (primary care, internal medicine/general physician) and other specialists (many specialties, including neurology, palliative medicine, rheumatology, emergency medicine and oncology) – to see whether they differ in their approach to treating chronic non-cancer pain.
Results
Demographics
A total of 2919 participants responded between September 2009 and December 2010. Of these, 1398 (48%) were pain specialists (including anesthesiologists), 629 (22%) were primary care physicians, and 892 (31%) were other specialists. Most (2683: 92%) came from Europe, and this sample was subdivided into those who came from Northern Europe (1389: 48% of total survey sample), Southern Europe (883: 30%), Central Eastern Europe (300: 10%), or another European country (111: 4%).
Treatment goals
When participants were asked to identify the point on an 11-point Numeric Rating Scale (NRS; 0 = no pain, 10 = worst pain imaginable) above which pain should be regarded as severe, the responses implied that no common understanding exists. Overall, most considered the threshold of severe pain to be somewhere in the 5–8 range, i.e. a 4-point spread on an 11-point scale, but 134 respondents (4.6% of the total sample) believed that pain should not be regarded as severe below a score of 9 or 10.
Previous studies have shown that patients with chronic pain do not require a complete absence of symptoms in order to consider treatment successfulCitation7. When treating patients with chronic pain, two-thirds (66.2%) of the physicians in this survey aimed to reduce the intensity of pain to an NRS score of 2–4. However, primary care physicians aimed for lower scores than the other two groups; 25.1% aimed for a score of 2, compared to 18.5% of pain specialists and 17.0% of other specialists (p < 0.0001).
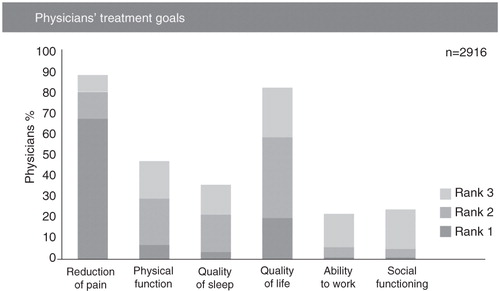
Survey participants were asked to rank their three main treatment goals for patients with severe, chronic non-cancer pain in order of importance (i.e., 1st, 2nd and 3rd) from a list of six options (). Reduction of pain was considered most important by over two-thirds of participants (67.0%). The results for pain specialists and other specialists were very similar, with reduction of pain being ranked first by 66.1% and 62.9%, respectively. The proportion of primary care physicians who considered this the main treatment goal was higher, at 75%, and the differences between physician groups were overall statistically significant (p < 0.0001). Quality of life was chosen by the pain specialist and other specialist groups for both Rank 2 (approximately one-third of both groups) and Rank 3 (approximately one-quarter of both groups). The primary care physicians also ranked quality of life second (chosen by almost half the group), but social functioning was ranked third (chosen by just under one-quarter of the group).
Choice of analgesic agent
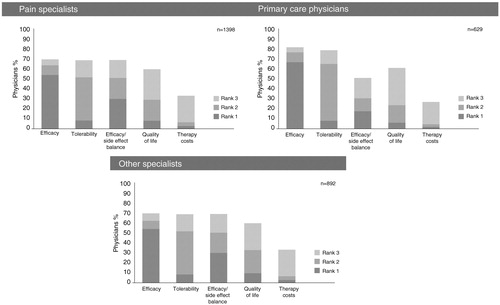
Participants were similarly asked to rank the three main factors that determine their choice of analgesic agent for a patient with severe, chronic non-cancer pain, this time from a list of five options. Efficacy was ranked first, chosen by 57.1% of participants, with efficacy/side-effect balance chosen by 26.5% and quality of life by 7.8%. The most frequent choice for Rank 2 was tolerability, and for Rank 3 was quality of life. Again there were differences between the physician groups. In Ranks 1, 2 and 3, the percentage of primary care physicians choosing efficacy, tolerability and quality of life, respectively, was higher than for either pain specialists or other specialists. For example, 68.0% of primary care physicians chose efficacy for Rank 1, compared to 54.1% of pain specialists and 53.9% of other specialists (p < 0.0001). The corresponding figures for Rank 2 and Rank 3 are 58.0% versus 44.1% and 45.4%, and 37.8% vs.31.0% and 30.9%, respectively. It is notable that 29.8% of pain specialists and 27.7% of other specialists considered that efficacy/side-effect balance was the most important factor in choosing an analgesic, compared to 17.6% of primary care physicians (p < 0.0001) ().
Prescription of opioids
Differences between the groups were also recorded with respect to their use of classical strong opioids for severe, chronic non-cancer pain. These are prescribed often or very often by 41% of the total survey sample, sometimes by 46%, and never by 13%. However, a higher proportion (50.4%) of pain specialists use these agents often or very often and only 9% never use them. By contrast, 30.4% and 33.8% of primary care physicians and other specialists use them often or very often, with 14.5% and 20.2%, respectively, never using them.
The average duration of treatment for severe, chronic non-cancer pain with a specific opioid varied between the different physician groups. Overall, 50.4% of respondents considered the average duration to be >3 months, but the figure for pain specialists was 57.7%, while for primary care physicians and other specialists it was lower at 38.7% and 40.3%, respectively. Conversely, 29.4% of other specialists and 23.2% of primary care physicians estimated the average duration to be ≤4 weeks, but this figure fell to 18.3% for pain specialists.
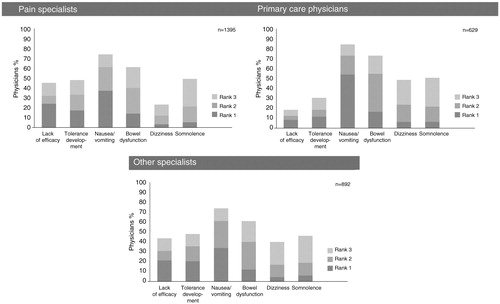
In the present survey participants were asked to rank, from a list of six options, the three main reasons for the failure of treatment with classical strong opioids. Results from all three groups of healthcare professionals, and the overall survey sample, ranked nausea/vomiting as the main limiting factor (i.e., Rank 1; 39.8%). Bowel dysfunction (28.8%) and somnolence (26.3%) were the most frequent choices for Rank 2 and Rank 3, respectively. Compared to the specialist groups, these side-effects were chosen more frequently by primary care physicians; for example, 53.3% placed nausea/vomiting in Rank 1, compared with 37.3% of pain specialists and 34.3% of other specialists (p < 0.0001). Although 24.2% of pain specialists and 21.5% of other specialists rated lack of efficacy as the most important reason for treatment failure, this was ranked first by only 7.8% of primary care physicians (p < 0.0001; ). Development of tolerance was similarly placed first by more other specialists (20.9%) and pain specialists (16.8%) than by primary care physicians (11.1%) (p < 0.0001; ).
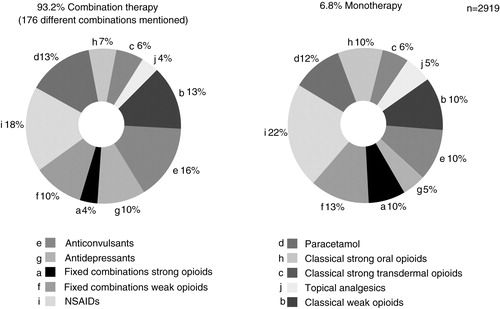
As chronic pain often involves more than one causative mechanism, it is seldom controlled by a single agent. Combining drugs with different mechanisms of action increases the probability of interrupting the pain signalCitation8–10 by producing additive or synergistic effects for analgesiaCitation11,Citation12. When asked for their main pharmacological approach for treating severe chronic low back pain, a large majority of survey participants (93.2%) reported using combination treatment rather than monotherapy, and there was little variation between the different physician groups (pain specialists 96.9%, primary care physicians 90.9%, other specialists 89.0%). The overall proportions of the different pharmacological agents used in combination therapy and monotherapy are shown in . It should be pointed out that fixed combinations, i.e. single formulations combining two agents with different mechanisms of action (e.g., tramadol 37.5 mg and acetaminophen 325 mg), were classified as monotherapy.
A total of 176 different combinations were reported, again demonstrating a wide variation in the current treatment of chronic pain. shows the ten most frequently reported drug combinations for each group. The top ten combinations in each group were reported by only 34% of pain specialists, 41% of primary care physicians and 36% of other specialists, emphasizing the diversity of treatment approaches in all three physician groups. None of the listed combinations for primary care physicians includes antidepressants. Classical strong opioids feature in three of the top ten drug combinations for pain specialists, but only two of the top ten drug combinations for the other two groups. The more extensive use of classical strong opioids by pain specialists is also seen in monotherapy, when the proportions of pain specialists, primary care physicians and other specialists prescribing classical strong opioids are 34.1%, 15.8% and 25.5%, respectively.
Table 1. The ten most frequently reported drug combinations for severe chronic low back pain.
Opinion of current treatment for chronic pain
Participants were asked to rate the extent to which they agreed with four statements relating to the current treatment of chronic pain, using a 5-point scale (1 = disagreement, 5 = total agreement). More than half the primary care physicians (56.0%) agreed that there is little knowledge of the pharmacological characteristics of different analgesic therapies within the broad medical community (i.e., gave ratings of 3–5), and this figure rose to 79.3% for other specialists and 90.1% for pain specialists (p < 0.0091). This pattern was repeated for the statement that there is limited awareness of the physiological difference between nociceptive and neuropathic pain within the broad medical community; 65.3% of primary care physicians agreed with this, compared with 84.6% of other specialists and 89.3% of pain specialists (p < 0.0001).
There was broad agreement among all three groups that a neuropathic component is often not clearly diagnosed in patients with severe, chronic low back pain. The percentages of pain specialists, primary care physicians and other specialists who agreed with this statement (i.e., gave a rating of 3–5 on the 5-point scale) were 92.8%, 88.7% and 90.8%, respectively (p < 0.0001). A statement that pain with a neuropathic component is often more severe and more difficult to treat produced an even greater consensus; 97.0%, 94.3% and 93.2% of pain specialists, primary care physicians and other specialists, respectively, agreed (p < 0.0001).
Conclusions
The data presented show that physicians’ opinions on the intensity of pain which should be regarded as severe is highly individual. Although differences between the physician groups were slight, NRS scores within each group ranged from 3 to 10 – i.e., across almost three-quarters of the NRS scale, indicating a general lack of consensus. Establishing a mutually agreed benchmark would provide greater consistency and allow for closer harmonization of treatment.
Pain reduction and improvement in quality of life are by far the most important treatment goals for physicians from all three groups. This is supported by the finding that more than a quarter of pain specialists and other specialists rated efficacy/side-effect balance as the key determinant when choosing an analgesic. The considerable influence of side-effects on successful pain management is shown by the fact that all three physician groups ranked gastrointestinal side-effects first and second as the main factors limiting successful treatment with classical strong opioids, and 42.5% of participants chose CNS side-effects for Rank 3.
In the treatment of severe, chronic low back pain, more than 90% of the survey participants relied on combination therapy as their main pharmacological approach to pain reduction, but the range of drugs used was extremely diverse. Even among the small percentage of physicians who preferred monotherapy, there was little consistency in the type of agent prescribed. This indicates that no single drug is particularly good in the management of severe chronic low back pain, while the sheer variety of combinations suggests that current treatment is not evidence-based. An additional factor may be that the importance of causative mechanisms is widely acknowledged, but they are often not taken into consideration if they cannot be identified and targeted.
Recent evidence suggests that very little time is currently devoted to teaching pain management during both undergraduate and postgraduate medical training. A UK survey found that the median time spent by undergraduate medical students on pain education was 13 hours, with some spending only 6 hoursCitation13. Moreover, the subject was taught piecemeal as a part of other topics, and not as a discrete moduleCitation13. A German survey of physicians who specialize in pain therapy revealed that their knowledge of WHO recommendations and the pharmacological aspects of pain was poorCitation14. The results of the present survey are consistent with these results. More than 60% of the physicians in all three groups agreed that the treatment of chronic pain is currently compromised by an apparent lack of knowledge of the physiological difference between nociceptive and neuropathic pain, a fundamental requirement for mechanism-based pain therapy. Similarly, nine out of ten pain specialists felt that there is little knowledge of the pharmacological characteristics of different analgesic therapies within the broad medical community. There was also widespread agreement that it is often difficult to diagnose the presence of a neuropathic component in a patient with chronic pain, and that pain with a neuropathic component is often more severe and difficult to treat. These conclusions could partially explain the high levels of dissatisfaction found in a recent pan-European patient survey that explored how chronic pain patients perceive their conditionCitation15, and strongly endorse the CHANGE PAIN focus on medical education.
The results revealed a number of differences between the three physician groups. For example, a higher percentage of the pain specialists used classical strong opioids to treat severe, chronic non-cancer pain, and they tended to prescribe them for a longer time. Various factors may contribute to this more widespread prescription of opioids, such as more extensive training in their use, a greater willingness to give opioids for chronic non-cancer pain, and the fact that patients referred to pain specialists often have more intense pain and are more difficult to treat. This illustrates a wider point, that variation in the responses of the three physician groups may be partly attributable to differences in the types of patient that they treat.
Differences between primary care physicians and the specialist groups suggest that first-line treatment tends to be more cautious and conventional, as might be expected. A smaller range of drug combinations was prescribed by primary care physicians, while a higher proportion chose the most popular answers to the factors governing choice of analgesic. Also, social functioning and ability to work were given a higher position in the ranking of treatment goals by this group, possibly as a result of more frequent contact between primary care physicians and their patients, as well as a broader, less focused clinical approach.
Among the limitations of the study are that the number of respondents is relatively small, and that 20% of the other specialist group did not give details of their specialty. Another is that the physicians who respond may not be representative of the physician group to which they were allocated; for example, general practitioners attending a conference on rheumatoid arthritis may have a particular interest in chronic pain. The geographic location of physicians may also influence results, because the management of chronic pain varies widely between different countries and more than 90% of respondents came from Europe. Requesting more detailed personal information from participants – e.g., on length of experience, training and type of practice – may have enabled additional conclusions to be drawn. As no individuals were specifically invited to participate, it is not possible to establish any differences between respondents and non-respondents.
These results are based on a survey sample of just under 3000 physicians. As the number of participants increases, the results should provide further clarification of physicians’ clinical practice and opinions. Ultimately, the goal is to be able to draw firm conclusions as to what constitutes best practice in pain management, and to disseminate this knowledge as widely as possible in the medical community.
Transparency
Declaration of funding
The survey questionnaire was developed based on feedback from the CHANGE PAIN Advisory Board meeting held in November 2009. This article is based on a survey of physicians which was supported by Grünenthal GmbH, Aachen, Germany, who also paid for descriptive analysis by Antwerpes AG, Cologne, Germany, and for editorial support in the preparation of this article.
Declaration of financial/other relationships
G.M-S. and G.Va. have been chairmen of Grünenthal’s International CHANGE PAIN Advisory Board since June 2009, and receive honoraria in this context.
CMRO peer reviewers may have received honoraria for their review work. The peer reviewers on this manuscript have disclosed that they have no relevant financial relationships.
Acknowledgments
The authors thank Derrick Garwood Ltd, Cambridge, UK, for editorial support, which was sponsored by Grünenthal GmbH, Aachen, Germany.
References
- Dworkin R, O’Connor AB, Backonja M, et al. Pharmacologic management of neuropathic pain: evidence based recommendations. Pain 2007;132:237-51
- Corbett M, Foster N, Ong BN. GP attitudes and self-reported behaviour in primary care consultations for low back pain. Fam Pract 2009;26:359-64
- Jamison RN, Gintner L, Rogers JF, et al. Disease management for chronic pain: barriers of program implementation with primary care physicians. Pain Med 2002;3:92-101
- van Tulder M, Koes B. Chronic low back pain. In: Stannard C, Kalso E, Ballantyne J, eds. Evidence-Based Chronic Pain Management. Oxford: Wiley-Blackwell 2010:74-82
- Jacobsen R, Sjøgren P, Møldrup C, et al. Physician-related barriers to cancer pain management with opioid analgesics: a systematic review. J Opioid Manag 2007;3:207-14
- Bhamb B, Brown D, Hariharan J, et al. Survey of select practice behaviours by primary care physicians on the use of opioids for chronic pain. Curr Med Res Opin 2006;22:1859-65
- Robinson ME, Brown JL, George SZ, et al. Multidimensional success criteria and expectations for treatment of chronic pain: the patient perspective. Pain Med 2005;6:336-45
- Raffa RB. Pharmacology of oral combination analgesics: rational therapy for pain. J Clin Pharm Ther 2001;26:257-64
- Besson M, Piguet V, Dayer P, et al. New approaches to the pharmacotherapy of neuropathic pain. Expert Rev Clin Pharmacol 2008;1:683-93
- Varrassi G, Müller-Schwefe G, Pergolizzi J, et al. Pharmacological treatment of chronic pain - the need for CHANGE. Curr Med Res Opin 2010;26:1055-69
- Gilron I, Bailey JM, Tu D, et al. Morphine, gabapentin, or their combination for neuropathic pain. N Engl J Med 2005;352:1324-34
- Hanna M, O’Brien C, Wilson MC. Prolonged-release oxycodone enhances the effects of existing gabapentin therapy in painful diabetic neuropathy patients. Eur J Pain 2008;12:804-13
- Survey of undergraduate pain curricula for healthcare professionals in the United Kingdom: A short report. The Pain Education Special Interest Group of the British Pain Society. The British Pain Society, London, UK, 2009. Available at: http://www.britishpainsociety.org/members_sig_edu_short_report_survey.pdf [Last accessed 22nd January 2010]
- Pflughaupt M, Scharnagel R, Gossrau G, et al. Physicians’ knowledge and attitudes concerning the use of opioids in the treatment of chronic cancer and non-cancer pain. Schmerz 2010;24:267-75
- Müller-Schwefe GHH. European survey of chronic pain patients: results for Germany. Curr Med Res Opin 2011;27:2099-106
Appendix 1
CHANGE PAIN Physician Survey
(Q1) On a numerical rating scale (NRS) from where on do you perceive chronic non-cancer pain to be severe?
○ NRS 0 (no pain) – 10 (worst imaginable pain)
(Q2) What is your objective in pain reduction on a numerical rating scale (NRS) for chronic non-cancer pain?
○ NRS 0 (no pain) – 10 (worst imaginable pain)
(Q3) What are the main treatment goals for your severe chronic non-cancer patients?
○ Reduction of pain
○ Physical function
○ Quality of sleep
○ Quality of life
○ Ability to work
○ Social functioning
(Q4) When you choose an analgesic for managing severe chronic non-cancer pain – what are the main characteristics for your treatment decision?
○ Efficacy
○ Tolerability
○ Efficacy/side-effect balance
○ Quality of life
○ Therapy costs
(Q5) How often do you prescribe classical strong opioids (e.g., morphine, oxycodone) for severe chronic non-cancer pain?
○ Never
○ Sometimes
○ Often
○ Very often
(Q6) What are the main reasons limiting treatment success with classical strong opioids in your severe chronic non-cancer patients?
○ Lack of efficacy
○ Tolerance development
○ Nausea/vomiting
○ Bowel dysfunction
○ Dizziness
○ Somnolence
(Q7) How long do your severe chronic non-cancer pain patients stay on average on a specific opioid?
○ <1 week
○ 1–4 weeks
○ 1–3 months
○ 3–6 months
○ >6 months
(Q8) Opinions on treatment of pain with a neuropathic component (1 = I do not agree – 5 = I totally agree):
○ There is little knowledge on the pharmacological characteristics of different analgesic treatment options within the broad medical community.
○ There is limited awareness on the physiological difference between neuropathic and nociceptive pain within the broad medical community
○ Pain where a neuropathic component is involved is often more severe and more difficult to treat.
○ In severe chronic pain patients a neuropathic component is often not clearly diagnosed.
(Q9) What is your main pharmacological approach for treating your severe chronic low back pain patients?
○ Monotherapy
○ Combination therapy (choose up to three treatment options)
Treatment options given: