Abstract
Obstructive fibrinous tracheal pseudomembrane (OFTP) is a relatively rare complication of endotracheal intubation. Despite being well documented, the exact pathogenesis of OFTP remains unclear. Some studies suggest that it may arise from the early stage of ischemic tracheal wall injury caused by the cuff pressure during intubation. Diagnosis and treatment of OFTP can be facilitated through therapeutic bronchoscopy. In this case report, we describe a patient who presented with dyspnea following repeated intratracheal interventions and was diagnosed with OFTP. The patient was successfully treated with bronchoscopic cryotherapy and was subsequently discharged from the hospital.
Introduction
Several airway injury complications, including tracheal stenosis, granuloma, and tracheomalacia, can occur as a result of endotracheal intubation or tracheostomy.Citation1 One such rare complication is obstructive fibrinous tracheal pseudomembrane (OFTP) with considerable delayed diagnosis,Citation2 the formation mechanisms of which are not well understood. It is believed that the ischemic injury to the tracheal mucosa caused by intubation may initiate a cascade leading to abnormal regeneration and the eventual formation of a fibrous membrane that obstructs the tracheal lumen.Citation3 The symptoms of OFTP can range from stridor, and acute respiratory failure depending on the extent of the obstruction.Citation4 In most cases, bronchoscopy is required for diagnosis and treatment.
Case Presentation
A 64-year-old woman was admitted to the hospital with dizziness and vomiting following a head injury. The CT scan revealed a left subdural hematoma. The patient had previously undergone a vocal cord polypectomy 15 years prior. After admission, she underwent an emergency craniotomy to remove the hematoma under general anesthesia. During the surgery, she was intubated through the mouth with a standard 7-mm cuffed endotracheal tube (ET), positioned 22 cm from the incisors. Unfortunately, the patient had poor recovery of consciousness in the postoperative course. Ten days later, a bedside tracheotomy was performed at the 2nd and 3rd tracheal rings using a bore size 7.5 mm cuffed tracheotomy tube. The procedure was uneventful. On the 15th day after surgery, the metallic tracheostomy tube was replaced.
Starting on the 31st day after surgery, the patient began to experience difficulty expectorating and positional dyspnea in the supine position. Additionally, she was producing excessive white mucoid secretion that was being aspirated in the gas channel. When attempting to insert a suction tube for mucus removal, resistance was encountered at the tracheotomy stoma, raising concern that the tracheostomy tube may have become displaced. To adjust the position of the tracheostomy cannula, it was removed. Almost immediately, the patient began to display symptoms of cyanosis of lips, sweating, dyspnea, and decreased consciousness. In response, she was immediately intubated through the mouth. During intubation, it was discovered that the patient’s airway was narrow.
On the 33rd day, a bronchoscopy was performed through the patient’s intubation tube. The examination revealed that there was obvious erosion of the tracheal mucosa 5 cm above the carina in the main airway. There was no active bleeding, or evidence of scarring or granulation hyperplasia. As the patient was conscious and had passed the spontaneous breathing test, the endotracheal tube was removed. However, 1.5 hours later, she developed symptoms of airway obstruction, dyspnea, and decreased oxygen saturation in her fingers and was immediately intubated again at the bedside.
During the intubation, significant swelling of the glottis was observed (glottidial edema). A repeat bronchoscopy was performed, and the tracheal tube was slowly withdrawn to the glottis under the guidance of a fibrobronchoscope. The examination revealed erosion of the tracheal mucosa at the cuff of the endotracheal intubation of the main airway, with no signs of bleeding or granuloma. A tracheotomy was performed again at the original tracheostomy site, and a metallic tracheostomy tube was placed under the guidance of a fibrobronchoscope.
On the 34th day, an attempt was made to close the tracheostomy tube by capping it, but the patient immediately experienced shortness of breath (dyspnea), signaling that the trial was unsuccessful.
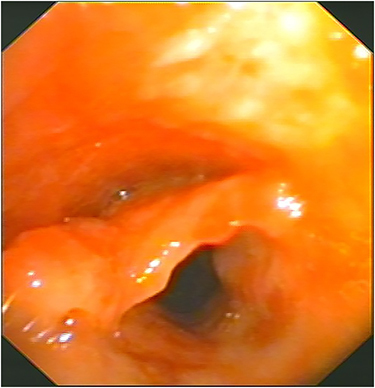
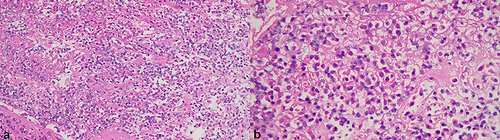
On the 37th day, a bronchoscopy was performed once more and revealed the presence of a membranous structure blocking nearly 80% of the tracheal lumen, located just below the tracheostomy stoma and about 5 cm above the carina (). The membranous structure was attempted to be removed using bronchoscopic forceps, but it proved to be difficult to remove in one piece (). With the consent of the patient’s family, bronchoscopic cryotherapy was performed. The pseudomembrane was collected () for further pathological examination (). Following the cryosurgery, the patient’s symptoms significantly improved, and there were no further issues noted during the one-month follow-up period ().
Table 1 Overview of the Repeated Intratracheal Interventions
Discussion
Airway injury caused by intubation can lead to various tracheal complications, including tracheal stenosis and tracheomalacia, whereas OFTP is a little-known condition associated with it.Citation5 The exact mechanisms of OFTP are unclear, but it is believed that high endotracheal cuff pressure can cause tracheal mucosal ischemic and necrosis.Citation3,Citation6 Hemorrhagic infarction of the submucosa and the infiltration of polymorphonuclear cells with fibrinous exudate can result in the formation of a fibrous membrane that partially or completely blocks the tracheal lumen.Citation7 Other factors, such as caustic injury from aspiration during intubation and the type of ET used, may also contribute to OFTP formation.Citation2,Citation4 This case highlights the potential damage to the airway wall that repeated intra-airway interventions can cause, leading to the formation of OFTP.
The OFTP is tubular, rubberlike pseudomembrane circumferentially impacted on the tracheal wall without infective origin, which is usually distal to the tip of the endotracheal tube.Citation7 Pseudomembranous necrotizing laryngotracheobronchitis is usually considered in the differential diagnosis of OFTP, but it is predominantly associated with an infectious cause, including gram-positive bacterial infections and viral infections, causing necrotizing damages to the larynx, trachea, and bronchial mucosa.Citation8 Necrotizing tracheobronchitis may also be distinguished from OFTP, which has been described in association with mechanical ventilation.Citation9 The injury of necrotizing tracheobronchitis is not limited to the area near the tip of the endotracheal tube, but also extends into the lower trachea and bronchi.Citation10 Ventilator-associated necrotizing tracheobronchitis is believed to be associated with insufficient humidification, excessive airway temperature, submucosal ischemia, and high operating pressure.Citation9
The exact incidence of OFTP is unknown. The symptoms of OFTP may occur anywhere from a few hours to several days after extubation, as reported in previous studies.Citation2,Citation11 In our case, the rapid onset of dyspnea after multiple extubations was observed following repeated intratracheal interventions. OFTP typically presents as upper airway obstruction, with dyspnea and stridor being the main symptoms.Citation3,Citation12 However, in some cases, positional dyspnea or exhaustion may prevent the manifestation of stridor, leading to a silent presentation of OFTP.Citation7
Sudden respiratory failure after extubation in the ICU is not uncommon and is often misdiagnosed as bronchial asthma, laryngeal edema or laryngospasm.Citation13 In the face of an urgent situation, most patients are intubated before a bronchoscopic examination can be performed.Citation3 This can result in the OFTP being detached into smaller pieces by the tube and removed through suction.
Bronchoscopy is an essential diagnostic tool for OFTP. In our case, we confirmed the diagnosis through flexible bronchoscopy (FB). Both FB and rigid bronchoscopy (RB) can effectively diagnose and remove the pseudomembranes.Citation11 While FB offers a more accurate and flexible operation, RB provides better airway maintenance and a larger operating space, making it more suitable for suctioning abundant or tenacious secretions.Citation2 In cases of thick and adherent obstructive lesions, we suggest the use of RB for mechanical ablation, as it can significantly shorten treatment time for severely dyspneic patients.Citation2 After removal of the lesion, it is crucial to conduct follow-up examinations to ensure complete expulsion of the whole membrane and prevent a recurrence.
In conclusion, when patients experience unexplained airway obstructive symptoms shortly after an endotracheal invasive procedure, healthcare providers should consider the possibility of OFTP. Early diagnosis through bronchoscopy can play a crucial role in identifying the cause and finding an effective treatment for airway obstruction.
Conclusion
OFTP may be a rare but potentially fatal condition making it important to be aware of the possibility in patients who present with stridor or dyspnea after undergoing an endotracheal intervention. Early detection and prompt intervention are crucial in ensuring the best outcome for these patients. Healthcare providers should be vigilant in recognizing the signs and symptoms of OFTP to provide prompt and effective treatment.
Ethics Approval and Consent to Participate
We identified this patient during routine clinical practice and obtained written informed consent for various invasive procedures. The ethical committee of Dazhou Central Hospital has confirmed that no ethical approval is required.
Consent for Publication
The patient signed the informed consent form to publish this report.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgments
The authors thank Dr. Liu for his help with the histological examination.
References
- Sandur S, Stoller JK. Pulmonary complications of mechanical ventilation. Clin Chest Med. 1999;20(2):223–247. doi:10.1016/S0272-5231(05)70139-8
- Sehgal IS, Dhooria S, Bal A, et al. Obstructive fibrinous tracheal pseudomembrane after endotracheal intubation. Resp Care. 2016;61(9):1260–1266. doi:10.4187/respcare.04662
- Patolia S, Enriquez D, Schmidt F, et al. Obstructive fibrinous tracheal pseudomembrane. J Bronchol Intervent Pulmonol. 2013;20(1):63–65. doi:10.1097/LBR.0b013e318281a332
- Ammar Y, Vella-Boucaud J, Launois C, et al. Obstructive fibrinous tracheal pseudomembrane. Anesth Analg. 2017;125(1):172–175. doi:10.1213/ANE.0000000000001408
- Soong WJ, Jeng MJ, Lee YS, et al. Pediatric obstructive fibrinous tracheal pseudomembrane—characteristics and management with flexible bronchoscopy. Int J Pediatr Otorhi. 2011;75(8):1005–1009. doi:10.1016/j.ijporl.2011.04.020
- Seegobin R, van Hasselt G. Endotracheal cuff pressure and tracheal mucosal blood flow: endoscopic study of effects of four large volume cuffs. Br Med J. 1984;288(6422):965–968. doi:10.1136/bmj.288.6422.965
- Deslee G, Brichet A, Lebuffe G, et al. Obstructive fibrinous tracheal pseudomembrane: a potentially fatal complication of tracheal intubation. Am J Respir Crit Care Med. 2000;162(3):1169–1171. doi:10.1164/ajrccm.162.3.9910047
- Lei W, Fei-Zhou Z, Jing C, et al. Pseudomembranous necrotizing laryngotracheobronchitis due to Mycoplasma pneumoniae: a case report and literature review. BMC Infect Dis. 2022;22(1):183. doi:10.1186/s12879-022-07160-5
- Bunt CW, Chung KK, Omron EN, et al. Ventilator-Associated Necrotizing Tracheobronchitis in a Patient on High-Frequency Oscillatory Ventilation. J Bronchol. 2005;12(2):96–99. doi:10.1097/01.laboratory.0000157385.86350.a1
- Metlay LA, Macpherson TA, Doshi N, et al. Necrotizing tracheobronchitis in intubated newborns: a complication of assisted ventilation. Pediatr Pathol. 1987;7(5–6):575–584. doi:10.3109/15513818709161421
- Lins M, Dobbeleir I, Germonpre P, et al. Postextubation obstructive pseudomembranes: a case series and review of a rare complication after endotracheal intubation. Lung. 2011;189(1):81–86. doi:10.1007/s00408-010-9263-2
- Yildirim BB, Karalezli A, Hasanoglu HC, et al. Obstructive fibrinous tracheal pseudomembrane. J Bronchol Intervent Pulmonol. 2012;19(2):129–131. doi:10.1097/LBR.0b013e31824f525f
- Niusha S, Salehi F, Shadmehr MB. Obstructive tracheal pseudomembrane. Arch Iran Med. 2017;20(11):714–715.