To the Editor,
Blastic plasmacytoid dendritic cell neoplasm (BPDCN), previously known as blastic CD4 + /CD56+NK-cell lymphoma, is a rare neoplastic disease originated from plasmacytoid dendritic cells and recently included in the WHO Classification of Tumors of hematopoietic and lymphoid tissues [Citation1]. In the great majority of cases, solitary or multiple skin lesions are the initial cause of first medical appointment [Citation2] and, in fact, cutaneous involvement is present in almost 100% of patients [Citation1]. Splenomegaly, lymphadenopathy, bone marrow and peripheral blood infiltration are variably found. Moreover, one or more cytopenias frequently occur at diagnosis, but in a minority of cases can be severe [Citation1,Citation3]. In this manner, anemia is usually of mild intensity and less common than thrombocytopenia [Citation1–4]. Given that BPDCN cases presenting without cutaneous involvement are extremely rare, we describe an unusual case of a patient with the diagnosis of BPDCN presenting with symptoms of severe transfusion dependent anemia and without skin lesions.
A 68-year-old woman presented with a two-month history of asthenia, anorexia, fever and significant weight loss. Forty-five days later she related an acute episode of dizziness, dyspnea and mental confusion. She went to an emergency medical service and received two units of packet red cells. One week later, she had another similar episode and had been transfused again. Thus, she was referred to us and admitted in the Department of Clinical Medicine in October 2010 to diagnosis elucidation.
The patient was a former heavy smoker. On physical examination, she was pale, the pulse was 120 bpm and the blood pressure was 180/80 mmHg. Abdominal examination revealed a palpable liver 5 cm from the right costal margin, fibro-elastic consistency, and a hard splenomegaly 6 cm from the left costal margin. There were no palpable lymphoid nodes or skin lesions. On admission, a complete blood count showed hemoglobin of 32 g/l, white blood cell count of 1.0 × 109/l and platelets count of 59.0 × 109/l. The levels of serum conjugated and total bilirrubin, lactate dehydrogenase, alanine and aspartate aminotransferases, alkaline phosphatase, total protein albumin and globulin were all normal. A computed tomographic of abdomen and pelvis showed hepatomegaly and splenomegaly.
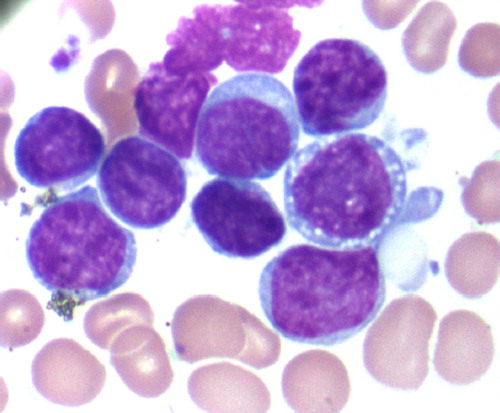
A bone marrow aspiration revealed a hypercellular marrow infiltrated by 87% of small to medium-sized cells, high nucleus-cytoplasm ratio, nucleus with regular shape displaying a moderately dispersed chromatin and inconspicuous nucleoli; the cytoplasm was basophilic and agranular. There were few cells with cytoplasmic microvacuoles (). The Sudam-Black staining was negative. The cytogenetic analysis by G-banding was not possible due to an insufficient number of metaphases. The multiparameter flow cytometry analysis was performed in a Coulter EPICS flow cytometer. Cells were stained with a panel of monoclonal antibodies using the erythrocyte lyse-wash preparation method. The immunophenothyping of malignant cells showed the typical CD4+/CD56+/CD123+ profile. Moreover, the malignant cells expressed the antigens CD7, CD45low and HLA-DR. The cells were negative for T and NK lineage antigens (CD1a, CD2, intracytoplasmic and surface CD3, CD5, CD8, CD16, TCRαβ), B lineage antigens (CD19, CD20, CD22, CD79a), myeloid-monocytic antigens (CD11c, CD13, CD14, CD15, CD33, CD41, CD61, CD235a, myeloperoxidase) and blast antigens (CD34, CD117). Based on the seminal publication of Feuillard et al. [Citation3], the immunophenothypic profile CD4+/CD56+/CD123+with low expression of CD45 and without the expression of B-cell, T-cell, NK-cell and myeloid-monocytic cell antigens is specific to BPDCN diagnosis and it is not observed in any other form of acute leukemia.
Figure 1. May-Grunwald Giemsa (MG) of the bone marrow smear preparation. BPDCN malignant cells have high nucleuscytoplasm ratio with nucleus displaying a moderately dispersed chromatin and inconspicuous nucleoli. The cytoplasm exhibited dense basophilia and the presence of microvacuoles in some cells.
The patient had an initial good response to CHOP-modified regimen (mitoxantrone instead of doxorrubicin), but evolved with neutropenia and severe sepsis. She died 45 days after the diagnosis.
The BPDCN is a rare disease accounting for only 0.7% of all primary cutaneous lymphomas [Citation5]. The neoplasm is present in the skin in practically all cases and, in fact, cutaneous involvement can be considered a hallmark of the disease [Citation1]. Hence, in an extensive review published in the last years, Petrella et al. [Citation6] analyzed the data of more than 100 patients with the diagnosis of BPDCN that have been reported in the literature and concluded that more than 94% of them manifested with cutaneous lesions. After that, series of cases have confirmed the intense tropism of the disease to the skin [Citation5,Citation7–10]. Recently, Tsagarakis et al. [Citation4] have reported, over a 12-year-period, only six patients with BPDCN without cutaneous involvement in a series of 26 patients and Jegalian et al. [Citation9] have reported seven of 29 pediatric patients with no skin manifestations. Based on these available data, there are probably less than 20 cases of patients with the diagnosis of BPDCN without cutaneous involvement published in the literature.
There is scarce information about the response to therapy of BPDCN cases without cutaneous involvement. In this manner, Jegalian et al. [Citation9] reported the outcome of 29 pediatric patients with BPDCN treated with different chemotherapy regimens. Interestingly, seven patients with no skin manifestations survived (100% survival, median follow-up six months) and, in contrast, only 11 of the 18 children with cutaneous involvement at presentation and with follow-up data available survived (61% survival). However, provided that the chemotherapy regimen applied to patients without skin lesion was more aggressive, it was not possible to conclude about the biological significance of the absence of skin disease to the prognosis of pediatric patients with BPDCN. Hence, if BPDCN cases without cutaneous involvement are a different biological form or just an uncommon variant of a rare disease is presently not known.
Given the extreme rarity of this presentation and the very small number of cases published in literature, case reports touching clinical features, immunophenothypic characteristics and response to treatment are useful to give more information about BPDCN cases without cutaneous involvement.
Acknowledgements
The authors thank to Andréa Santos do Nascimento and Fátima Guerreiro for the technical assistance with flow cytometry. The authors report no conflict of interest.
References
- Facchetti F, Jones DM, Petrella T. Blastic plasmacytoid dendritic cell neoplasm. Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri A, Stein H, . WHO classification of tumours of haematopoietic and lymphoid tissues. Lyon: IARC Press; 2008. 145.
- Garnache-Ottou F, Feuillard J, Saas P. Plasmacytoid dendritic cell leukaemia/lymphoma: Towards a well defined entity? Br J Haematol 2007;136:539–48.
- Feuillard J, Jacob MC, Valensi F, Maynadié M, Gressin R, Chaperot L, . Clinical and biologic features of CD4+CD56 + malignances. Blood 2002;99:1556–63.
- Tsagarakis NJ, Kentrou NA, Papadimitriou KA, Pagoni M, Kokkini G, Papadaki H, . Acute lymphoplasmacytoid dendritic cell (DC2) leukemia: Results from the Hellenic Dendritic Cell Leukemia Study Group. Leuk Res 2010; 34:438–46.
- Ng AP, Lade S, Rutherford T, McCormack C, Prince HM, Westerman DA. Primary cutaneous CD4+/CD56 + hematodermic neoplasm (blastic NK-cell lymphoma): A report of five cases. Haematologica 2006;91:143–4.
- Petrela T, Bagot M, Willemze R, Beylot-Barry M, Vergier B, Delaunay M, . Blastic NK-Cell lymphomas (agranular CD4+CD56+hematodermic neoplasm): A review. Am J Clin Pathol 2005;123:662–75.
- Martín JM, Nicolau MJ, Galán A, Ferrández-Izquierdo A, Ferrer AM, Jordá E, . CD4+/CD56+haematodermic neoplasm: a precursor haematological neoplasm that frequently first presents in the skin. J Eur Acad Dermatol Venereol 2006;20:1129–32.
- Dietrich S, Hegenbart U, Andrulis M, Schmitt T, Bellos F, Martens UM, . Blastic plasmacytoid dendritic cell neoplasia (BPDC) in elderly patients: Results of a treatment algorithm employing allogeneic stem cell transplantation with moderately reduced conditioning intensity. Biol Blood Marrow Transplant Epub 2011 Jan 6.
- Jegalian AJ, Buxbaum NP, Facchetti F, Raffeld M, Pittaluga S, Wayne AS, . Blastic plasmacytoid dendritic cell neoplasm in the pediatric population: Diagnostic features and clinical implications. Haematologica 2010;95:1873–9.
- Cota C, Vale E, Viana I, Requena L, Ferrara G, Anemona L, . Cutaneous manifestations of blastic plasmacytoid dendritic cell neoplasm-morphologic and phenotypic variability in a series of 33 patients. Am J Surg Pathol 2010;34: 75–87.
