To the Editor,
Rare but with ever increasing incidence and prevalence [Citation1], neuroendocrine tumors can secrete some humoral factors and cause various clinical paraneoplastic syndromes. Although three cases of coronary vasospasm reported so far [Citation2–4], generalized vasospasm associated with metastatic neuroendocrine tumor have not been reported to the best of our knowledge. Here, we present a case of octreotide resistant lung neuroendocrine tumor with systemic vasospasm presented with acute limb ischemia (ALI) secondary to severe arterial vasospasm.
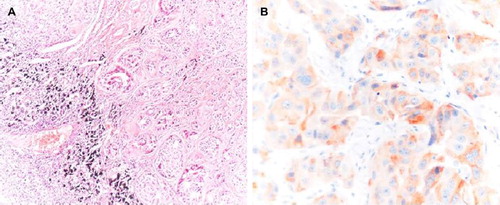
A 31-year-old woman presented to the outpatient clinic with the complaints of large volume diarrhea accompanied by crampy abdominal pain and mild dyspnea. She did not report attacks of hypotension, hypertension, and flushing. Her past medical history was unremarkable except for a mild bronchial asthma. Her physical examination was normal; she appeared healthy, and her vital signs were normal except mild tachycardia. Abdominal ultrasonography revealed multiple liver masses and a tru-cut biopsy was performed. Histopathological examination showed a neuroendocrine carcinoma (, ×100) which stained positively with synaptophysine ( synaptophysine, ×400). Detailed radiological examinations, octreotide scintigraphy, and endoscopic examination of upper and lower gastrointestinal tract failed to reveal the occult primary. No other disease involvement but liver lesions were positive on octreoscan. Chromogranin level was elevated.
Figure 1. A; Neuroendocrine tumor composed of monotonous cells with oval nuclei and visible cytoplasms in metastatic nests in a lymph node (HE, ×100). B; Positive immunohistochemical staining with synaptophysine (synaptophysine, ×400).
It was decided that she had well-differentiated metastatic neuroendocrine carcinoma of unknown primary which caused carcinoid syndrome. Long-acting octreotide at a dose of 30 mg every four weeks and interferon alpha-2b at a dose of three million international units three times a week were started. Her symptoms subsided to a large extent. However at the 8th month of treatment, interferon had to be stopped secondary to intolerable toxicity. At that time, she was totally symptom-free and radiological examination was compatible with stable disease. Since there was no evidence of extrahepatic disease, radioactive microsphere therapy was performed. One year later, a left pulmonary hilar lesion of 3 cm became apparent on computerized tomography (CT)-scan which was also detected by octreoscan. Liver lesions were stable on both octreoscan and CT-scan. However, her symptoms gradually worsened at that time and chromogranin level increased. Considering that liver lesions were stable, surgical resection of the lung tumor was planned because of worsening clinical condition of the patient and risk of unresectability over time. Histopathological examination revealed similar pathological characteristics with the previous lesion. After the surgery, her symptoms regressed for six to 10 months.
Two years after the treatment onset, the liver became enlarged and her symptoms aggravated suggesting progression. Octreotide dose was increased up to 50 mg per month upon symptom aggravation. Inconsistently, a recent octreoscan was consistent with stable disease. At that time she presented with cold and pale left lower extremity. She denied any herbal medication. Search for potential drugs from national pharmacy database revealed the recent use of any serotonin selective receptor inhibitors (SSRIs). Palpation revealed weak pulses on the femoral and popliteal arteries with no pulse over dorsalis pedis on the left. Color Doppler evaluation of the lower extremity was consistent with arterial occlusion and she was referred to vascular surgeon. The patient was put on anticoagulation. Vascular surgeons attempted thrombectomy with acute limb ischemia relying on the positive ultrasonography report. There was no embolus in the arteries, but exposed left femoral artery was smaller in diameter than normal. The most common reasons for ALI as atheroembolic disease and arterial embolus were excluded by radiological and surgical examination [Citation5]. The clinical picture was considered to be secondary to arterial vasospasm. Vasodilator calcium channel blockers and acetyl salicylic acid 300 mg/day were initiated. Pulse on the dorsalis pedis could be palpated after a week.
During the next few days, diarrhea increased, livedo reticularis developed, and systolic blood pressure decreased to as low as 80 mmHg. Color Doppler ultrsonography showed diffuse vasoconstriction of whole lower and upper extremity arteries with narrowing of the arteries and increased peak systolic velocities. Short acting octreotide infusion started. Sympathetic blockage at the level of L2 was performed to decrease arterial vasospasm. Chest and abdominal tomography still showed radiologically stable neuroendocrine tumor (), but the external iliac, the superficial and deep femoral arteries on the left were narrower than those on the right side (, white arrows). During the next few days, arterial pulses couldn't be palpated and arterial blood pressure could not be measured at all. Plasmapheresis was attempted in order to remove an unknown vasoconstrictor substance with no improvement. Vasoconstriction could not be overcome with any attempt tried. Tissue necrosis with gangrene due to severe ischemia developed starting from the toe progressing to the knee level on the left. Acute renal failure and hypoxia complicated the clinical picture. Respiratory failure requiring mechanical ventilation developed. She died at the 28th day of hospitalization.
Figure 2. A; Computed tomography shows heterogenous involvement of the liver by the tumor. Enlarged liver compresses the right kidney posteriorly. B; Severe narrowing of the arteries are prominent on the left side. CT images at the level of iliac arteries shows narrowing of the left iliac artery (white arrow) compared to the right iliac artery (white arrow). B. At more caudal level, the left superficial artery is also significantly smaller in diameter due to vasospasm than the right superficial femoral artery (arrows).
Main symptoms of our patient could be summarized as peripheral diffuse progressive vasoconstriction with accompanying diarrhea. Although we excluded drug abuse such as triptans; her symptoms, disease course and radiological examination results may suggest ergotism, in other words syndrome of ALI which was caused by ergotamine derivatives [Citation6]. Ergotism is a rare disorder that can be seen in 0.001–0.002% of patients using triptans [Citation6], which are most widely used drugs in treatment of migraine. Even though, triptans have strong affinity for central serotonin (5-HT) receptors and show their therapeutic effect via vasoconstriction of intracranial extra cerebral arteries, in case of toxicity they also can cause peripheral vasoconstriction by showing agonistic activity on 5-HT 1a and 5-HT 2a receptors [Citation6]. It may present as acute or chronic form. Acute ergotism can be presented by symptoms of nausea, vomiting, diarrhea, paresthesia, confusion to sudden death, whereas chronic ergotism can be presented with peripheral vasoconstriction as the most prominent sign in two-thirds of patients [Citation6,Citation7]. Treatment consists of cessation of the offending drug, medical and/or surgical vasodilatation, anticoagulant treatment, and sympathic blockage in more severe cases.
Although clinical features of ergotism and carcinoid syndrome are seemed to be very different, interestingly they carry strong similarity in terms of disease mechanism. It is well known that serotonin is the main mediator of carcinoid syndrome while peripheral serotonin (5-HT) receptors are the main receptor for triptans in ergotism. Although she and her family denied, she may have had been using a herb which contain ergot-producing fungi [Citation8]. We may suggest that at some point when serotonin level increases above certain level as in malignant carcinoid, it may end up with ergotism. We could not rule out the possible offending agent like stopping the drug in triptan toxicity because serotonin was produced by malignant carcinoid. However on the other hand, the fact that the severe vasoconstriction did not respond to short acting octreotide in our patient argues against the above mechanism described.
Such an extensive vasospasm may well be secondary to cathecolamines like epinephrine or norepinephrine which be secreted by the tumor. Some neuroendocrine tumors other than pheochomocytomas may secrete cathecolamines [Citation9]. It is known that neuroendocrine tumors may shift the substance they produce in time [Citation10]. Our patient had a pulmonary neuroendocrine tumor, which can trigger coronary vasospasm, an observation supporting catecholamine production [Citation2–4]. Unfortunately, we did not test for it. The fact that she was never hypertensive argues against a chatecholamine-related mechanism, although we did not measure intra-arterial the blood pressure directly to avoid endothelial injury which may presumably worsen vasoconstriction.
Neuroendocrine tumors are dynamic diseases with wide range of associated clinical paraneoplastic diseases which may be mild or rare and fatal as in our case. One should remember that even the most unlikely clinical catastrophes may be caused by neuroendocrine tumors and in depth clinical analysis in a timely manner can save lives. Whatever the mechanism is, neuroendocrine tumors can cause generalized vasospasm which can lead to death.
Declaration of interest: Kjell Oberg disclosed advisory board and speakers bureau for Novartis, Ipsen and Pfizer, Huseyin Abali received travel grants from Novartis and Pfizer.
References
- Janson ET, Sørbye H, Welin S, Federspiel B, Grønbaek H, Hellman P, . Nordic guidelines 2010 for diagnosis and treatment of gastroenteropancreatic neuroendocrine tumours. Acta Oncol 2010;49:740–56.
- Bourgault C, Bergeron S, Bogaty P, Poirier P. A most unusual acute coronary syndrome. Can J Cardiol 2006;22:429–32.
- Petersen KG, Seemann WR, Plagwitz R, Kerp L. Evidence for coronary spasm during flushing in the carcinoid syndrome. Clin Cardiol 1984;7:445–8.
- Topol EJ, Fortuin NJ. Coronary artery spasm and cardiac arrest in carcinoid heart disease. Am J Med 1984;77:950–2.
- Mitchell ME, Mohler ER, Carpenter JE. Acute arterial occlusion of the lower extremities (acute limb ischemia. Available from: http://www.uptodate.com/online/content/topic.do?topicKey = vascular/8645&view = print [accessed on 21 Jan 2011].
- Silberstein S. The pharmacology of ergotamine and dihydroergotamine. Headache 1997;37:15–22.
- Rahman A, Yıldız M, Dadas E, Donder E, Cihangiroglu M, Eken C, . Reversal of ergotamine-induced vasospasm following methyl prednisolone. Clin Toxicol 2008;46:1074–107.
- Eadie MJ. Convulsive ergotism: Epidemics of the serotonin syndrome? Lancet Neurol 2003;2:429–34.
- Whitman HH 3rd, Fishman EK, Oberg K, Wildman JM, Long AL. Catecholamine-secreting metastatic carcinoid as differential diagnosis in pheochromocytoma: clinical, laboratory, and imaging clues in the search for the lurking neuroendocrine tumor (NET). Ann N Y Acad Sci 2006;1073:59–78.
- Ozawa Y, Tomoyasu H, Takeshita A, Shishiba Y, Yamada S, Kovacs K, . Shift from CRH to ACTH production in a thymic carcinoid with Cushing's syndrome. Horm Res 1996;45:264–8.
