Abstract
Background: Numerous studies have reported variable associations between ambient particulate matter (PM) and chronic obstructive pulmonary disease (COPD) hospitalizations and mortality. Objective: To conduct a systematic study assessing the associations between hospitalizations and mortality from COPD and ambient PM10 (particulate matter with aerodynamic diameters ≤ 10 μm, PM10). Methods: Systematic searches were conducted in 6 common electronic databases. A meta-analysis was performed to estimate the odds ratio (OR) to evaluate the relationship between PM10 and COPD hospitalizations and mortality. Publication bias and heterogeneity of samples were tested by Begg funnel plot and Egger test, respectively. Study findings were analyzed using random-effect model and fixed-effect model. Results: The search yielded 31 studies suitable for the meta-analysis during the period from Jan 1, 2000 to Oct 31, 2011. A 10μg/m3 increase in PM10 was associated with a 2.7% (95%CI = 1.9%-3.6%) increase in COPD hospitalizations with an OR of 1.027 (95%CI: 1.019–1.036), and a 1.1% (95%CI: 0.8%–1.4%) increase in COPD mortality with an OR of 1.011 (95%CI: 1.008–1.014). Conclusions: Ambient PM10 is associated with increased COPD hospitalizations and mortality. Further research is needed to elucidate whether this association is causal and to clarify its mechanisms.
Introduction
Chronic obstructive pulmonary disease (COPD) is characterized by airflow limitation that is not fully reversible and chronic inflammation of the lungs (Citation1). It is a major and increasingly prevalent global health problem in both developed and developing countries. Epidemiologic studies suggest that COPD affects 5% to 19% of the adult population above 40 years of age (Citation2,3). By far, cigarette smoking (active or passive) is considered to be the major reason for the development of most COPD cases. In addition, there are other risk factors, including inflammation, occupational dust exposures, outdoor and indoor air pollution from fuel burning, and lower socioeconomic status, etc. (Citation4,5). Of all the other risk factors, exposure to ambient particulate matter (PM), especially the inhalable particulate matter (PM10), has become an important risk factor for the development of respiratory diseases including COPD.
In the last few decades, many epidemiological studies have examined the short-term effects of air pollution exposure on patients with COPD. Most of them have reported significant associations between PM and increased COPD hospitalizations and mortality (Citation6,7). Among the air pollutants, PM10 (particulate matter with aerodynamic diameters ≤ 10 μm, PM10) is now recognized as one of the potential environmental agents that is responsible for the respiratory diseases. It shows a stronger association with COPD than many other factors, even after adjusting for other major risk factors such as cigarette smoking (Citation8). However, inconsistent results have been found on the association between PM10 and COPD hospitalizations and mortality in different countries and regions; sometimes even in the same regions.
Zanobetti et al. (Citation9) demonstrated a significant and positive association between PM10 and the risk of hospitalizations for COPD in Chicago with a significant increase of 2.5% (95%CI: 1.8%–3.3%) in COPD hospitalization per 10μg/m3 increase of PM10. However, Anderson et al. (Citation10) found a decrease of 1.8% (95%CI: -6.9%–3.5%) in COPD hospitalization per 24.4μg/m3 increase in PM10 in Birmingham. Results on the association between PM10 and COPD mortality are also inconsistent. Moolgavkar (Citation11) demonstrated a significant and positive association between PM10 and the risk of mortality for COPD with a significant increase of 2.66% (95%CI: 0.12%–5.20%) in COPD mortality per 25μg/m3increase in PM10 in Cook. On the contrary, also in Cook city, Bateson and Schwartz (Citation12) found a lack of association between PM10 and the risk of mortality for COPD with an estimate percent change of 0.58% (95%CI: -0.82%–2.00%) per 10μg/m3increase in PM10.
Meanwhile, age, socioeconomic status, and education level were able to modify the effects of PM10. In addition, the PM10 concentration metrics used in previous studies are different, which makes it difficult to compare the results over studies. To quantitatively clarify the relationship between COPD and PM10, we conducted a systematic literature review and a meta-analysis of studies in order to give an over estimation on the associations between PM10 and COPD hospitalization and mortality. The results will be helpful for us to draw a quantitative and credible conclusion on the relationship between PM10 exposure and acute hospitalizations and mortality from COPD, which may also be helpful for the government to make related environmental decisions.
Methods
Search strategy
We identified related publications between Jan 1, 2000 to Dec 31, 2011 by systematic searches in English literature databases: PubMed/Medline, EMBASE, Google scholar, Ovid, and Web of science. We conducted a literature search for particulate matter/PM10; COPD hospital admissions/ emergency department visits, and mortality; using “RR/OR/Percent” and “AND” as combining terms for exposure and outcome.
Inclusion criteria
Two reviewers (Zhu and Liu) collected articles eligible for further review by performing an initial screen of identified abstracts or titles. Broad inclusion criteria for articles were: (Citation1) original studies (not review articles) and reporting the association of inhalable particulate matter (PM10) with COPD hospital admissions and mortality; (Citation2) results were reported in a quantitative exposure-response relationship expression (RR/OR /Percent and 95% confidence intervals (CIs)) and evaluated with time-series and case-crossover designs; (Citation3) daily PM10 data were obtained from multiple air monitoring stations with no missing days or only a few missing days; (Citation4) studies had defined COPD according to the American Thoracic Society (ATS) (Citation13) and Global Initiative for Obstructive Lung Disease (GOLD) (Citation14) criteria.
Exclusion criteria
The exclusion criteria for articles were (Citation1) inadequate information; (Citation2) different designs, such as panel study; (Citation3) not original; not full-length articles or did not provide calculable or reported RR/OR/ Percent and 95%CIs; (Citation4) the diagnosis of COPD was uncertain. The articles which met all the above criteria were reviewed (). Those articles that formally meet the inclusion and exclusion criteria were analyzed using a data form.
Statistical methods
The OR was used as the common measure of association. The RR was transformed to OR according to the existing literature (Citation15). Briefly, the formula OR = RR [(1-P0)+(P0×OR)] was used, in which P0 is the incidence of the outcome of interest in the non-exposed group. In the present analysis, the problem of RR and OR is of no importance given that the increased risk for COPD is generally very low and the two measures are almost equivalent. As for effects on COPD hospitalizations and mortality, we chose a 10 ug/m3 increase in PM10 as the concentration metric for daily PM10 and used the formula OR = [eβ-1]×100%. If the concentration metric was not 10 ug/m3, we used an alternative formula OR = [e(β×IQR)-1]×100% to transform the estimate, where β and IQR stand for the effect estimate and an interquartile range, respectively (Citation16). Eventually we calculated the effects size (OR) on COPD hospitalizations and mortality corresponding to an increase of 10 ug/m3 in PM10.
Meta-analysis was performed using STATA version 11.0 (STATA, College Station, Texas, USA). The natural logarithm of the RR/OR and its 95%CI of the lnOR were used to estimate the pooled effect size over different studies. The OR and 95%CI data were entered as two separate data sets for COPD in Stata11.0. To assess the heterogeneity of RR across studies, the Chi-squared (χ2 significant level at p ≤ 0.10) and the I2 were calculated before analysis. The criteria for random-effect model was determined by significant heterogeneity with an I2 statistic value > 50% or p ≤ 0.10 and fixed-effect model was determined by significant heterogeneity with an I2 statistic value ≤ 50% or p > 0.10. Heterogeneity between different studies was systematically examined by multivariable meta-regression. Begg funnel plot (Citation17,18) and the Egger test (Citation17) were used to assess publication bias.
Results
The initial search found 1322 titles, of which 1210 citations were excluded after identification based on abstracts and titles, and there were 31 original studies that met the inclusion criteria for this meta-analysis. Of all the included papers, nine were case-crossover studies and 22 were time-series studies. Data from the 31 studies were sampled across 13 different countries and 23 areas starting from Jan 1, 2000 to Oct 31, 2011. The short-term effects (lag days 0–7) of PM10 on COPD were evaluated. Of all the 31 studies, there were 18 studies dealing with PM10 and COPD hospitalizations and 13 studies dealing with PM10 and COPD mortality ().
Table 1. Studies included in the meta-analysis investigating the short term effects between PM10 on COPD
Effects estimate
COPD hospitalizations and PM10
Random-effect models were used to calculate the pooled effect size for OR (chi-squared χ2 = 117.82, [degree of freedom, df = 19], I2 = 83.9%, p < 0.001; and Z = 6.61, p < 0.001). The random pooled effect size (OR) for COPD hospitalizations due to PM10 was 1.03 (95%CI = 1.02–1.04) (). A 10 ug/m3increase in daily PM10 was associated with a 2.7% (95%CI = 1.9%–3.6%) increase in COPD hospitalizations.
Figure 2. Forest plot of COPD hospitalizations and PM10 in the meta-analysis Random-effect models were used to calculate the pooled effect size for OR (chi-squared χ2 = 117.82, [degree of freedom, df = 19], I2 = 83.9%, p < 0.001; and Z = 6.61, p < 0.001). The random pooled effect size (OR) for COPD hospitalizations due to PM10 was 1.03 (95%CI = 1.02–1.04).
![Figure 2. Forest plot of COPD hospitalizations and PM10 in the meta-analysis Random-effect models were used to calculate the pooled effect size for OR (chi-squared χ2 = 117.82, [degree of freedom, df = 19], I2 = 83.9%, p < 0.001; and Z = 6.61, p < 0.001). The random pooled effect size (OR) for COPD hospitalizations due to PM10 was 1.03 (95%CI = 1.02–1.04).](/cms/asset/13954c8d-f715-47a8-a116-0e65fc7fcdcb/icop_a_744962_f0002_b.jpg)
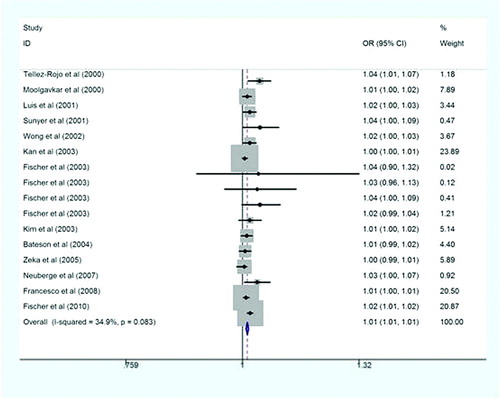
COPD mortality and PM10
Fixed effect models were used to calculate the pooled effect size for OR (χ2 = 23.03, df = 15, I2 = 34.9%, p > 0.05; and Z = 7.40, p < 0.001). The pooled effect size (OR) for COPD mortality and PM10 was 1.011 (95%CI = 1.008–1.014) (). A 10 ug/m3increase in daily PM10 was associated with a 1.1% (95%CI = 0.8%–1.4%) increase in COPD mortality.
Figure 3. Forest plot of COPD mortality and PM10 in the meta-analysis Fixed effect models were used to calculate the pooled effect size for OR (χ2 = 23.03, df = 15, I2 = 34.9%, p > 0.05; and Z = 7.40, p < 0.001). The pooled effect size (OR) for COPD mortality and PM10 was 1.011 (95%CI = 1.008 –1.014).
Publication bias
Publication bias was tested using funnel plots for both COPD hospitalization and mortality. A funnel plot of the two types of studies did not show significant Begg test results. The combined data obtained from Egger's test for COPD hospitalization (bias = 1.97, P > |t | = 0.250) and COPD mortality (bias = 0.16, P > |t| = 0.882) showed that there was no evidence of publication bias on the associations between PM10 and COPD hospitalizations and mortality ( and ).
Figure 4. Funnel plot for PM10 and COPD hospitalizations in the meta-analysis. Publication bias was tested by using funnel plots for COPD hospitalization. The combined data obtained from Egger's test for COPD hospitalization (bias = 1.97, P>|t| = 0.250) showed that there was no evidence of publication bias on the association between PM10 and COPD hospitalizations with PM10. The pseudo 95% CI is computed as part of the analysis that produces the funnel plot, and corresponds to the expected 95%CI for a given standard error (SE). OR indicates odds ratio.
Figure 5. Funnel plot for PM10 and COPD mortality in the meta-analysis. Publication bias was tested by using funnel plots for COPD mortality. The combined data obtained from Egger's test for COPD mortality (bias = 0.16, P>|t| = 0.882) showed that there was no evidence of publication bias on the association between PM10 and COPD mortality with PM10. The pseudo 95% CI is computed as part of the analysis that produces the funnel plot, and corresponds to the expected 95%CI for a given standard error (SE). OR indicates odds ratio.
Heterogeneity by meta-analysis
We performed a stratified analysis according to a set of key study characteristics including ages range and socioeconomic status for the eligible articles (). We found that these study characteristics did not contribute to the heterogeneity among studies in this meta-analysis. But they all showed significant associations with COPD hospitalizations and mortality (p < 0.05).
Table 2. Studies included in the meta-analysis in different groups between PM10 and COPD hospitalizations and mortality
Discussion
COPD, the fourth-leading cause of death in the world, represents an important public health challenge that is both preventable and treatable. Globally, the COPD burden is projected to increase in coming decades because of continuing exposure to COPD risk factors and aging of population (Citation45). Air pollution exposure has been recognized as a risk factor for cardiorespiratory illnesses, including COPD for a long time. The number of studies focusing on the association between outdoor air pollution and cardiorespiratory diseases has been increasing rapidly in developed countries such as the United States and western European countries. A better understanding of the importance of PM on the development and progression of COPD is important for the development of preventive measures including health education programs.
This systematic review yielded 31 studies that clearly and adequately evaluated COPD hospitalizations and mortality as outcomes in association with PM10. Our analysis suggests an overall PM10 effect on COPD hospitalizations and mortality, which is similar to the results reported in the European APHEA study (Citation46) and a recent meta-analysis (Citation47). We found that an increase of 10 ug/m3in PM10 was associated with a 2.7% increase in COPD hospitalizations and a 1.1% increase in COPD mortality, respectively. However, there are significant variations between the studies included in this meta-analysis in terms of study design, exposure assessment and potential confounders. All these factors added substantial statistic heterogeneity between different studies, which might have influenced the risk estimation.
Significant publication bias was not found in studies focusing on the relationship between PM10 and COPD hospitalizations and mortality. After stratification by different subgroups to test the heterogeneity, we found that ages range and different socioeconomic status also did not contribute to the heterogeneity. However, there were significant associations between these factors and COPD hospitalizations and mortality. In previous studies, these factors are individual effect modifiers of the PM10 effects. For example, higher PM10 effect estimates were found in elderly people. Chen et al. (Citation21) demonstrated a RR of 1.128 (95%CI: 1.054–1.028) for COPD hospitalizations associated with an IQR increase of 7.9 ug/m3 in the preceding 24-hour average PM10 concentration after adjusting for temperature and relative humidity in Vancouver. The authors also confirmed that the risk for COPD hospitalizations was increasing with age; the RR in people with 85+ years of age was almost the twice of that in people with 65–74 years of age. Schwartz et al. (Citation48) estimated that an increase of 50 ug/m3in PM10 was associated with a 10% to 25% increase in COPD hospitalizations according to previous studies, which is consistent with our results. We also found that PM10 effect on COPD mortality were stronger in developing countries. Because few studies about COPD hospitalizations associated with PM10 were conducted in developing countries, we were not able to estimate the overall association between PM10 and COPD hospitalizations in developing counties. Liu et al. (Citation49) performed a meta-analysis in both high and low-income countries and documented that exposure to indoor air pollutants from the combustion of solid fuels, which contributed significantly to the COPD burden in low-income counties, and non-smoking women were particularly at risk. Forastiere et al. (Citation50) also found that the effect of particulate matter on mortality among COPD patients may be more pronounced among individuals with lower income or national economic status.
We observed a similar phenomenon in the present meta-analysis. The effect of PM10 on COPD hospitalization was stronger in patients in Asian countries, while patients in European counties and the United States suffered more from COPD mortality. Asian populations commonly have lower educational level and socioeconomic status. A previous study has found effect modification by social class in area specific analysis in both low socioeconomic status and high socioeconomic status communities (Citation51) but there was little evidence of effect modification in a large study in the United States (Citation52), which involved nationwide data. Other factors including inflammation, combinations and poor nutrition are also thought to be partly responsible for high COPD hospitalizations and mortality. Previous studies have demonstrated that the association between particulate matter and health effects is stronger in persons with increased baseline systemic inflammation and oxidative stress, such as patients with diabetes, obese individuals, and people not using statins (Citation53,54). Nuvolone et al. (Citation55) reported higher risk of acute myocardial infarction death with COPD. Given the consistency between our results and previous findings, we may conclude that the relevant question should no longer be whether this association exists, but rather whether this established association is causal.
Limitations of this meta-analysis should be considered. Firstly, literatures included in the analysis were limited and may not fully reflect publication bias. Second, the measurement methods and category of PM10 in different studies were not available and the duration of exposure and documentation of outcome were variable over different study settings.
Conclusions
In this meta-analysis study, we found that PM10 was associated with increased COPD hospitalizations and mortality. We did not find significant publication bias and heterogeneity among studies. Different ages and economic levels were all significantly associated with COPD hospitalization and mortality and elderly patients and developing countries suffered more with COPD hospitalizations and mortality. Further study is needed to clarify whether this association is causal and its underlying mechanisms.
Declaration of Interest Statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Acknowledgements
The authors thank Li-Ming Niu for providing statistical advice during the preparation of this manuscript and professor Si-Yan Zhan for epidemiologic questions. This work was supported by Grants from the National Natural Science Foundation of China [No.81072267 and 81170012].
References
- Pauwels RA, Buist AS, Calverley PMA, Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2001 Mar; 163:1256–1276.
- Buist AS, McBurnie MA, Vollmer WM, International variation in the prevalence of COPD (the BOLD Study): a population-based prevalence study. Lancet 2007 Sep; 370(9589):741–750.
- Zhong N, Wang C, Yao W, Prevalence of chronic obstructive pulmonary disease in China. Am J Respir Cirt Care Med 2007 Oct; 176(8):753–760.
- Viegi G, Maio S, Pistelli F, Epidemiology of chronic obstructive pulmonary disease: health effects of air pollution. Respiratory 2006 Sep; 11(5):523–532.
- Torres-Duque C, Maldonado D, Perez-Padilla R, Biomass fuels and respiratory diseases: a review of the evidence. Proc Am Thorac Soc. 2008 Jul; 5(5):577–590.
- Moolgavkar SH, Luebeck EG, Anderson EL, Air pollution and hospital admissions for respiratory causes in Minneapolis-St. Paul and Birmingham. Epidemiology 1997 Feb; 8(4):364–370.
- Kim H, Kim Y, Hong YC, The lag-effect pattern in the relationship of particulate air pollution to daily mortality in Seoul, Korea. Int J Biometeorol 2003 May; 48(1):25–30.
- Schwartz J. Short term fluctuations in air pollution and hospital admissions of the elderly for respiratory disease. Thorax 1995 May; 50(5):531–538.
- Zanobetti A, Schwartz J, Gold D. Are there sensitive subgroups for the effect of airborne particles? Environ Health Perspect 2000 Sep; 108(9):841–845.
- Anderson HR, Bremner SA, Atkinson RW, Particulate matter and daily mortality and hospital admissions in the west midlands conurbation of the United Kingdom: associations with fine and coarse particles, black smoke and sulphate. Occup Environ Med 2001 Aug; 58(8):504–510.
- Moolgavkar SH. Air pollution and daily mortality in three US counties. Environ Health Perspect 2000 Aug; 108(8):777–784.
- Bateson TF, Schwartz J, Who is sensitive to the effects of particulate air pollution on mortality? A case-crossover analysis of effect modifiers. Epidemiology 2004 Mar; 15(2):143–149.
- Celli BR, MacNee W, ATS/ERS task force. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J 2004 Jun; 23(6):932–946.
- Rabe KF, Hurd S, Anzueto A, Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: gold executive summary. Am J Respir Crit Care Med 2007 Sep; 176(6):532–555.
- Zhang J, Yu KF. What's the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA 1998 Nov; 280(19):1690–1691.
- Dai HX, Song WM, Gao X, Study on relationship between ambient PM10, PM2.5 pollution and daily mortality in a district in Shanghai. J Hygiene Res. 2004 May; 33(3): 293–297 (in Chinese).
- Egger M, Davey Smith G, Schneider M, Bias in meta-analysis detected by a simple, graphical test. BMJ 1997 Sep; 315(7109):629–634.
- Sterne JA, Egger M, Smith GD, Systematic reviews in health care: investigating and dealing with publication and other biases in meta-analysis. BMJ 2001 Jul; 323(7304):101–105.
- Chen L, Yang W, Jennison BL, Air particulate pollution and hospital admissions for chronic obstructive pulmonary disease in Reno, Nevada. Inhal Toxicol 2000 Apr; 12(4):281–298.
- Zanobetti A, Schwartz J, Docker DW, Airborne particles are a risk factor for hospital admissions for heart and lung disease. Environ Health Perspect 2000 Nov; 108(11):1071–1077.
- Chen Y, Yang Q, Krewski D, Influence of relatively low level of particulate air pollution on hospitalization for COPD in elderly people. Inhal Toxicol 2004 Jan; 16(1): 21–25.
- Yang QY, Chen Y, Krewski D, Effect of short-term exposure to low levels of gaseous pollutants on chronic obstructive pulmonary disease hospitalizations. Environ Res 2005 Sep; 99(1):99–105.
- Peel JL, Tolbert PE, Klein M, Ambient air pollution and respiratory emergency department visits. Epidemiology 2005 Mar; 16(2):164–174.
- Medina-Ramon M, Zanobetti A, Schwartz J. The effect of ozone and PM10 on hospital admissions for pneumonia and chronic obstructive pulmonary disease: a national multicity study. Am J Epidemiol 2006 Mar; 163(6):579–588.
- Ko FW, Tam W, Wong TW, Temporal relationship between air pollutants and hospital admissions for chronic obstructive pulmonary disease in Hong Kong. Thorax 2007 Sep; 62(9):780–785.
- Lee IM, Tsai SS, Chang CC, Air pollution and hospital admissions for chronic obstructive pulmonary disease in a tropical city: Kaohsiung, Taiwan. Inhal Toxicol 2007 May; 19(5): 393–398.
- Yang CY, Chen CJ. Air pollution and hospital admissions for chronic obstructive pulmonary disease in a subtropical city: Taipei, Taiwan. J Toxicol Environ Health 2007 July; 70(14):1214–1219.
- Johnston FH, Bailie R, Pilotto LS, Ambient biomass smoke and cardio-respiratory hospital admissions in Darwin, Australia. BMC Public Health 2007 Sep; 7:240.
- Arbex MA, de Souza Conceicao GM, Cendon SP, Urban air pollution and chronic obstructive pulmonary disease-related emergency department visits. J Epidemiol Community Health 2009 Oct; 63(10):777–783.
- Sauerzapf V, Jones AP, Cross J. Environmental factors and hospitalization for chronic obstructive pulmonary disease in a rural country of England. J Epidemiol Community Health 2009 Apr; 63(4):324–328.
- Stieb DM, Szyszkowicz M, Rowe BH, Air pollution and emergency department visits for cardiac and respiratory conditions: a multi-city time-series analysis. Environ Health 2009 Jun; 8:25.
- Belleudi V, Faustini A, Stefoqqia M, Impact of fine and ultrafine particles on emergency hospital admissions for cardiac and respiratory diseases. Epidemiology 2010 May; 21(3):414–423.
- Morgan G, Sheppeard V, Khalaj B, Effect of bushfire smoke on daily mortality and hospital admission in Sydney, Australia. Epidemiology 2010 Jan; 21(1):47–55.
- Tam WW, Wong TW, Wong AH, Effect of dust storm events on daily emergency admissions for respiratory disease. Respirology 2011 Jan; 17(1):143–148.
- Tellez-Rojo MM, Romieu I, Ruiz-Velasco S, Daily respiratory mortality and PM10 pollution in Mexico City importance of considering place of death. Eur Respir J 2000 Sep; 16(3):391–396.
- Braga AL, Zanobetti A, Schwartz J. The lag structure between particulate air pollution and respiratory and cardiovascular death in 10 US cities. J Occup Environ Med 2001 Nov; 43(11):927–933.
- Sunyer J, Basagana X. Particles, and not gases, are associated with the risk of death in patients with chronic obstructive pulmonary disease. Int J Epidemiol 2001 Oct; 30(5):1138–1140.
- Wong TW, Tam WS, Yu TS, Associations between daily mortalities from respiratory and cardiovascular diseases and air pollution in Hong Kong, China. Occup Environ Med 2002 Jan; 59(1):30–35.
- Kan H, Chen B. Air pollution and daily mortality in Shanghai: a time-series study. Arch Environ Health 2003 Jun; 58(6):360–367.
- Fischer P, Hoek G, Brunekreef B, Air pollution and mortality in the Netherland: are the elderly more at risk. Eur Respir J 2003 May; 40:34s–38s.
- Zeka A, Zanobetti A, Schwartz J. Short-term effects of particulate matter on cause specific mortality: effects of lags and modification by city characteristics. Occup Environ Med 2005 Oct; 62(10):718–725.
- Neuberger M, Rabczenko D, Moshammer H. Extended effects of air pollution on cardiopulmonary mortality in Vienna. Atmospheric Environment 2007 Jul; 41:8549–8556.
- Forastiere F, Stafoggia M, Berti G, Particulate matter and daily mortality: a case-crossover analysis of individual effect modifiers. Epidemiology 2008 Jul; 19(4):571–580.
- Fischer PH, Marra M, Ameling CB, Trends in relative risk estimates for the association between air pollution and mortality in The Netherlands, 1992–2006. Environ Res 2011 Jan; 111(1):94–100.
- National Heart, Lung and Blood Institute, World Health Organization. Global initiative for chronic obstructive lung disease. Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease. http://www.goldcopd.org, 2011 update.
- Atkinson RW, Anderson HR, Sunyer J, Acute effects of particulate air pollution on respiratory admission. Results from the APHEA2 project. Air pollution and health: a European approach. Am J Respir Crit Care Med 2001 Nov; 164(10 pt 1):1860–1866.
- Anderson HR, Atkinson RW, Peacock JL, Ambient particulate matter and health effects: publication bias in studies of short-term associations. Epidemiology 2005 Mar; 16(2):155–163.
- Schwartz J, Dockery DW, Neas LM. Is daily mortality associated specially with fine particles? J Air Waste Manag Assoc 1996 Oct; 46(10):927–939.
- Liu Y, Lee K, Perez-Padilla R, Outdoor and indoor air pollution and COPD-related disease in high-and low-income countries. Int J Tuberc Lung Dis 2008 Feb; 12(2):115–127.
- Forastiere F, Stafoggia M, Tasco C, Socioeconomic status, particulate air pollution, and daily mortality: differential exposure or differential susceptibility. Am J Ind Med 2007 Mar; 50(3):208–216.
- Jerrett M, Burnett RT, Brook J, Do socioeconomic characteristics modify the short term association between air pollution and mortality? Evidence from zonal time series in Hamilton, Canada. J Epidemiol Community Health 2004 Jan; 58(1):31–40.
- Health Effect Institute. Special report: revised analysis of time series studies of air pollution and health. Part II. Revised analyses of the National Morbidity, Mortality and Air Pollution Study. In: Revised Analyses of Selected Time-Series Studies. Boston, MA: Health Effects Institute, May 2003.
- Schwartz J, Park SK, O'Neill MS, Glutathione-S-transferase M1 obesity, stains, and autonomic effects of particles: gene-by-drug-by-environment interaction. Am J Respir Crit Care Med 2005 Dec; 172(12):1529–1533.
- O'Neill MS, Veves A, Zanobetti A, Diabetes enhances vulnerability to particulate air pollution-associated impairment in vascular reactivity and endothelial function. Circulation 2005 Jun; 111(22):2913–2920.
- Nuvolone D, Balzi D, Chini M, Short-term association between ambient air pollution and risk of hospitalization for acute myocardial infarction: results of the cardiovascular risk and air pollution in Tuscany (RISCAT) Study. Am J Epidemiol 2011 July; 174(1): 63–71.