Abstract
Objective
The QRS complex duration is commonly used to prognosticate severity, predict outcomes, and indicate treatment in overdose. However, literature to support this practice is mixed in tricyclic antidepressant overdoses and absent in non-tricyclic antidepressant overdoses. Our objective was to assess the validity of QRS complex duration as a prognostic marker in overdose.
Methods
This was a secondary analysis of cases reported to the Toxicology Investigators Consortium between January 1, 2010, and December 31, 2022. Cases were assessed to determine the six xenobiotics most associated with QRS complex prolongation. All cases involving these six xenobiotics, regardless of QRS complex duration, constituted the study cohort. Inclusion criteria were cases of patients older than 12 years old with single-xenobiotic exposures. Clinical outcomes evaluated were seizure, ventricular dysrhythmia, metabolic acidosis, and death.
Results
Of 94,939 total cases, diphenhydramine, amitriptyline, bupropion, quetiapine, nortriptyline, and cocaine were most associated with QRS complex prolongation. Inclusion criteria were met by 4,655 cases of exposure to these xenobiotics. QRS complex prolongation was associated with increased odds ratio of seizure in all included xenobiotics, of ventricular dysrhythmia in all included xenobiotics except nortriptyline, and of metabolic acidosis or death in all included xenobiotics except nortriptyline and quetiapine. A normal QRS complex duration had a negative predictive value of greater than or equal to 93.0 percent of developing metabolic acidosis and 98.0 percent of developing a ventricular dysrhythmia or death from the xenobiotics studied.
Discussion
This study demonstrates that patients with QRS complex prolongation from all six xenobiotics studied had an increased prevalence and odds of developing severe outcomes. Furthermore, patients who did not develop QRS complex prolongation were unlikely to develop a ventricular dysrhythmia, metabolic acidosis, or death. These findings were noted in six xenobiotics that mechanistically can cause QRS complex prolongation through sodium channel or gap junction inhibition.
Conclusion
Identification of patients at risk for severe outcomes after overdose can be aided by measuring the QRS complex duration. If prospectively validated, these outcomes have implications on risk stratification, disposition level of care, and appropriateness of treatments.
Introduction
Early identification of patients at risk of severe toxicity after overdose has widespread implications for clinical management. Given the prevalence and mortality of tricyclic antidepressant overdoses in the second half of the twentieth century, numerous studies sought to identify early markers of severe tricyclic antidepressant toxicity. Multiple studies demonstrate that the sodium channel blocking effects of tricyclic antidepressant toxicity slows phase 0 depolarization of the cardiac action potential through impaired His-Purkinje and myocardial conduction velocity leading to QRS complex prolongation [Citation1–4]. The QRS complex duration was proposed by Boehnert et al. [Citation5] as a means of prognosticating the clinical course for these patients. Their study demonstrated that patients with a maximum limb lead QRS complex duration of 100 milliseconds (ms) or greater were at increased risk of seizures, while only patients with a QRS complex duration of 160 ms or greater were at risk of ventricular dysrhythmias [Citation5]. Several follow-up studies supported the prognostic ability of QRS complex duration in tricyclic antidepressant toxicity [Citation6,Citation7]. In a canine model, increased amitriptyline concentrations lead to QRS complex prolongation, and a QRS complex greater than 110 ms was associated with ventricular dysrhythmias [Citation6]. In a retrospective analysis of patients with tricyclic antidepressant ingestions, a QRS complex duration greater than 100 ms was one of the multiple markers found to have an elevated odds ratio of major toxicity [Citation7].
However, other studies have questioned the prognostic ability of the QRS complex duration in tricyclic antidepressant overdose, and literature to support this practice in non-tricyclic xenobiotics is nearly nonexistent [Citation8–11]. In the years following the publication by Boehnert et al. [Citation5] multiple studies displayed an inconsistent association between QRS complex duration and severe outcomes such as ventricular dysrhythmias, seizures, and death [Citation8–10]. A 2004 meta-analysis of 18 studies by Bailey et al. [Citation11] reported that the sensitivity and specificity of a QRS complex duration greater than 100 ms for seizures, ventricular dysrhythmias, and death ranged from 46% to 81%. While they concluded that electrocardiogram (ECG) findings poorly predicted complications after tricyclic antidepressant overdose, they acknowledged that “anecdotal clinical experience suggests that the ECG is a far better prognostic test than that indicated by the results” [Citation11]. There are multiple possible explanations for this conclusion. This includes the time-dependent relationship between overdose and ECG, which was inconsistent between studies, and the use of alternate QRS complex duration thresholds other than 100 ms.
Despite these mixed results, QRS complex duration is commonly used to prognosticate severity, predict severe outcomes, inform level of care decisions, and as an indication for hypertonic sodium bicarbonate therapy in tricyclic antidepressant overdoses [Citation12]. The mechanistic justification for this practice stems from the known inhibition of tricyclic antidepressants for voltage-sensitive sodium channels in the heart, which leads to QRS complex prolongation as well as the potential to change the morphology of the R wave in lead aVR, alter the axis of the terminal 40 ms frontal QRS complex plane, produce a right bundle branch block-like pattern, or unmask a Brugada pattern [Citation13–18]. Through this same mechanism, the use of QRS complex duration to predict clinical outcomes and guide management is commonly extrapolated to non-tricyclic sodium channel blocking xenobiotics. Literature to support this practice in non-tricyclic xenobiotics is exceptionally sparse for several xenobiotics and nonexistent for most [Citation19–21]. This is despite the prevalence and potential severity of non-tricyclic sodium channel blocking xenobiotics. For example, diphenhydramine, which is a known sodium channel blocker, had the second most medical outcomes of moderate, major, or death in the 2022 National Poison Data System Annual Report after paracetamol (acetaminophen) [Citation22,Citation23]. Therefore, research is needed to guide whether the practices of prognostication based on QRS complex duration should be used in tricyclic antidepressant or non-tricyclic xenobiotic ingestions.
We hypothesized that QRS complex prolongation is associated with severe clinical features in overdose on tricyclic antidepressant and non-tricyclic xenobiotics with sodium channel-blocking properties. The first objective was to determine if patients with QRS complex prolongation were at increased risk of severe clinical features compared to patients without QRS complex prolongation after tricyclic antidepressant and non-tricyclic xenobiotic overdoses. The second outcome was to determine how well QRS complex prolongation performs in predicting severe clinical features.
Methods
Study design and setting
This was a secondary analysis of cases reported to the Toxicology Investigators Consortium (ToxIC) Core Registry. The ToxIC Core Registry is a database of patient cases that received medical toxicology consultation at approximately 50 participating sites in the United States and internationally [Citation24]. This data source collects de-identified data. This project was exempt from review by our Institutional Review Board and was approved by the ToxIC research committee. De-identified case data was provided on standardized spreadsheets (Microsoft Excel 2022, version 16.70).
Patient population
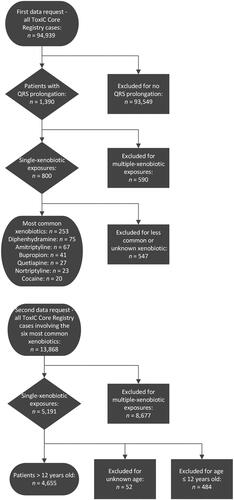
We studied all cases of QRS complex prolongation in the ToxIC Core Registry, regardless of the xenobiotic, reported between January 1, 2010, and December 31, 2022. These cases were analyzed to obtain the six most frequent single-xenobiotic exposures associated with QRS complex prolongation (). Cases of xenobiotic withdrawal were not included.
All cases involving one of the six most commonly associated xenobiotics, regardless of the QRS complex duration, constituted our study cohort. The inclusion criteria were patients older than 12 years of age with single-xenobiotic exposures to one of these six xenobiotics. All routes of exposure were included. Patients 12 years old or younger or without a specified age were excluded to minimize exploratory exposures. Multiple-xenobiotic exposures were excluded to minimize confounding.
Variables
The clinical outcomes evaluated were seizure, ventricular dysrhythmia, metabolic acidosis, and death. These clinical outcomes were chosen as markers of severe toxicity due to their clinical importance and based on their utilization in prior studies evaluating the role of QRS complex duration in overdose [Citation5,Citation8,Citation19]. Variables were defined based on the ToxIC Core Registry documentation criteria including QRS complex prolongation as greater than 120 ms and metabolic acidosis as a pH of less than 7.2 that is metabolic in nature. The ToxIC Core Registry does not specify a standard QRS complex duration measurement method. Therefore, QRS complex duration measurements may be manual or computer-generated depending on the treating provider’s discretion.
Analysis
Statistical analyses were performed using odds ratios, positive predictive value (PPV), and negative predictive value (NPV) calculations. Odds ratios (OR) were calculated using contingency analysis of categorical variables. Statistical significance was defined using 95% confidence intervals (CI). Predictive values were chosen as the appropriate statistical measurement to assess whether QRS complex duration could stratify patients for developing clinical outcomes. The JMP® Pro 16.0.0 statistical software was used for analyses.
Results
Characteristics of study subjects
During the study period, there were 94,939 total cases reported to the ToxIC Core Registry (). QRS complex prolongation occurred in 1,390 (1.5%) of these cases; 800 single-xenobiotic exposures and 590 multiple-xenobiotic exposures. The most frequent single-xenobiotic exposures associated with a prolonged QRS complex duration were diphenhydramine (n = 75), amitriptyline (n = 67), bupropion (n = 41), quetiapine (n = 27), nortriptyline (n = 23), and cocaine (n = 20).
There were 13,868 total cases of exposure to diphenhydramine, amitriptyline, bupropion, quetiapine, nortriptyline, or cocaine during the study period. This included 5,191 single-xenobiotic exposures, which were included, and 8,677 multiple-xenobiotic exposure, which were excluded. Cases were then excluded for patients 12 years old or younger (n = 484) or without a specified age (n = 52). The inclusion criteria were met by 4,655 cases, which formed our study cohort.
The demographics of these patients are shown in . The median, interquartile range, and range of ages are reported due to the non-normally distributed age of the patient population. The route of exposure was known in 3,515 (75.5%) cases. For cases with a known exposure route, oral was the most common route (n = 3,299, 93.9%) and was more common than all non-oral routes combined (n = 216, 6.1%). Most non-oral exposures were exposure to cocaine (n = 180, 83.3%). This included 83 inhalational cases, 74 intranasal cases, 19 parenteral cases, 3 rectal cases, and 1 other exposure case, which were 30.3%, 27.0%, 6.9%, 1.1%, and 0.4% of the overall cocaine cases with a known exposure route, respectively.
Table 1. The demographics of patients in the study cohort who met inclusion criteria.
Main results
Comparative analyses between patients with normal and prolonged QRS complex durations for each xenobiotic are shown in . There were increased overall rates of seizure, ventricular dysrhythmia, metabolic acidosis, and death in patients with QRS complex prolongation compared to patients with normal QRS complex duration for all xenobiotics, except for metabolic acidosis and death in quetiapine exposures. Additionally, QRS complex prolongation was associated with increased odds of seizure in all included xenobiotics, of ventricular dysrhythmias in all included xenobiotics except nortriptyline, and of metabolic acidosis or death in all included xenobiotics except nortriptyline and quetiapine ().
Figure 2. Odds ratios for clinical outcomes in patients with prolonged QRS complex compared to a normal QRS complex duration. Columns with no bar and an asterisk (*) signify an odds ratio where the 95% confidence interval did not show a significant difference in outcomes between patients with a prolonged compared to normal QRS complex duration. The error bars display the 95% confidence interval for each odds ratio, which may also be seen in .
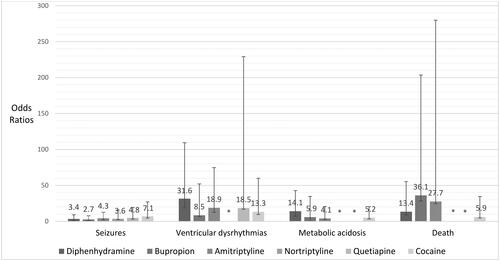
Table 2. Statistical analyses for patients with normal and prolonged QRS complex durations for developing seizures.
Table 3. Statistical analyses for patients with normal and prolonged QRS complex durations for developing ventricular dysrhythmias.
Table 4. Statistical analyses for patients with normal and prolonged QRS complex durations for developing metabolic acidosis.
Table 5. Statistical analyses for patients with normal and prolonged QRS interval durations for deaths.
The predictive value of QRS complex duration is also shown in . The PPV of QRS complex prolongation for these clinical outcomes was generally low for the six xenobiotics, although the exact values varied by outcome and xenobiotic. The NPV of a normal QRS complex duration was strongest in predicting the absence of ventricular dysrhythmias, metabolic acidosis, and death. A normal QRS complex duration had a NPV of 93.0% or greater that patients did not develop metabolic acidosis and 98.0% or greater that patients did not develop ventricular dysrhythmia or death from all xenobiotics.
Discussion
The role of QRS complex prolongation in predicting severe toxicity in overdose has implications for the management and disposition of the poisoned patient. These results suggest that patients with a prolonged QRS complex duration have increased odds of seizure, metabolic acidosis, ventricular dysrhythmias, and death for these xenobiotics with few exceptions. These exceptions are potentially due to low incidence rates of certain outcomes for certain xenobiotics. For instance, none of the 26 patients with a prolonged QRS complex duration after quetiapine exposure developed metabolic acidosis or death, which led to a lower rate of these outcomes than in patients with a normal QRS complex duration. Furthermore, patients with a prolonged QRS complex duration after nortriptyline exposure did not have statistically different odds ratios of ventricular dysrhythmia, metabolic acidosis, or seizure. However, given that nortriptyline is a metabolite of amitriptyline with the same mechanism of action, a larger sample size for nortriptyline could have yielded similar results to amitriptyline. This has implications on patient disposition as patients with QRS complex prolongation in the setting of overdose are more likely to necessitate a higher level of care and are at greater risk of decompensation.
Another important finding from this study was the NPV of severe outcomes in patients with a normal QRS complex duration. A normal QRS complex duration had a NPV of 93.0% or greater that the patient would not develop metabolic acidosis and 98.0% or greater that a patient would not develop ventricular dysrhythmia or death for each xenobiotic. The clinical importance of this finding is that patients with a normal QRS complex duration are unlikely to develop ventricular dysrhythmias, metabolic acidosis, or death. Therefore, patients who continued to display a normal QRS complex duration were unlikely to have a fatal ingestion or necessitate interventions to treat ventricular dysrhythmias or metabolic acidosis in this study.
As hypothesized, QRS complex prolongation in this study was associated with increased odds of severe outcomes. We believe this is due to the mechanism of toxicity of the xenobiotics. Blocking voltage-sensitive sodium channels in the myocardium and conducting system slows phase 0 (depolarization) of the myocyte action potential. This leads to QRS complex prolongation as well as the other potential electrocardiographic findings mentioned previously. This altered sodium conduction impairs contraction and predisposes patients to the development of ventricular dysrhythmias [Citation3].
Five of the six xenobiotics most frequently associated with QRS complex prolongation in the ToxIC Core Registry have known sodium channel-blocking properties: diphenhydramine [Citation25], amitriptyline [Citation13], quetiapine [Citation26], nortriptyline [Citation27], and cocaine [Citation28]. In contrast, experimental evidence from in vitro and animal studies suggests that bupropion induces QRS complex prolongation through myocardial gap junction inhibition rather than sodium channel blockade [Citation29,Citation30]. This slows myocyte electrical impulse communication and therefore slows the rate of depolarization [Citation29,Citation30]. Therefore, all six xenobiotics act through a mechanism that may result in QRS complex prolongation.
Finally, the threshold for a normal QRS duration used in this study was less than 120 ms. Although many prior studies have used 100 ms, we felt that 120 ms was a more appropriate threshold. There is a significant proportion of the population whose baseline QRS complex duration is between 100 ms and 120 ms. A study using cohorts from the Framingham Heart Study identified that 4% of patients had QRS complex durations between 100–120 ms and 3% greater than or equal to 120 ms after excluding patients with pacemakers or taking antidysrhythmics [Citation31]. Furthermore, another study following 2,537 healthy 18–30 years old patients with QRS complex durations of less than 100 ms at year 0 found that 11.5% of patients developed QRS complex durations of greater than 100 ms by year 20 [Citation32]. Furthermore, the inclusion of patients with a baseline QRS complex duration of greater than 120 ms in our analysis would likely bias the results toward the null hypothesis, thereby strengthening the positive conclusions of this study.
Ultimately, QRS complex prolongation in these six xenobiotics is predictive of severe toxicity. The QRS complex prolongation is the electrocardiographic representation of the sodium channel blockade and gap junction inhibition that occurs with these xenobiotics. The sodium channel blockade and gap junction inhibition may directly predispose patients to ventricular dysrhythmias. The causes of seizures and metabolic acidosis are multifactorial and partially driven by other mechanisms not related to the QRS complex. However, we demonstrated that the QRS complex prolongation is still predictive of these outcomes, likely because it is a marker of greater xenobiotic toxicity in the patient.
Limitations
There are limitations to this study. First, documentation was based on history, not on laboratory confirmation. Second, the ToxIC Core Registry is limited by the documentation of treating medical toxicologists. The ToxIC quality assurance process does not verify ToxIC entries with patients’ medical records and undetected errors in data entry might occur. Despite this, there is no reason to believe that there were categorical differences in the histories or data entry between patients with normal and prolonged QRS complex duration. Third, this study utilized QRS complex prolongation on any ECG as a positive finding, but did not associate it with any timeframe. Additionally, the ToxIC database does not specify the method of QRS complex duration measurement and leaves this interpretation to the entering provider. Fourth, all exposure routes were included in this study. We chose to include all exposure routes instead of just oral exposures due to the different patterns of use between xenobiotics. In this study, 93.9% of cases with a known exposure route were oral exposures, although the proportion of oral exposures was lower for cocaine (34.3%). However, this is reflective of a different pattern of cocaine exposures compared to the other xenobiotics studied. Fifth, ToxIC data methodologically represents only a subset of all overdoses that the primary team sought medical toxicology consultation, typically due to case severity or complexity. We expect that this only strengthens the conclusion because even in a population with high rates of severe outcomes, QRS complex prolongation was still largely predictive. Sixth, this study only looks at the six xenobiotics most frequently reported to have QRS complex prolongation in a national database. All these xenobiotics act through a mechanism that could lead to QRS complex prolongation. Therefore, the potential generalizability of this study pertains only to xenobiotics that mechanistically function like these six xenobiotics. Further study is needed to prospectively validate the prognostic value of QRS complex prolongation and to determine if QRS complex prolongation has prognostic value in xenobiotics without a mechanism for QRS complex prolongation.
Conclusions
In summary, the identification of patients at risk of severe clinical outcomes in overdose can be aided by evaluating the QRS complex duration on electrocardiography. Patients with QRS complex prolongation from these xenobiotics had an increased prevalence and odds of developing severe clinical outcomes. Furthermore, patients who did not develop QRS complex prolongation were unlikely to develop ventricular dysrhythmias, metabolic acidosis, or death. If prospectively validated, these outcomes have implications on risk stratification, disposition level of care, and appropriateness of treatments.
Meetings
This work was presented as a poster presentation at the North American Congress of Clinical Toxicology in Montreal, Quebec, Canada on 30 September 2023.
Authors’ contributions
MS, SK, KM, CH, and JB conceived the study. MS, SK, and KM performed the data request and data analysis. MS drafted the manuscript. MS, SK, KM, CH, and JB contributed substantially to the revisions and rewriting of the manuscript. MS takes responsibility for the paper as a whole.
Disclosure statement
No potential conflict of interest was reported by the authors.
Data availability statement
Data for this manuscript was obtained by request from the American College of Medical Toxicology’s Toxicology Investigators Consortium: https://www.acmt.net/toxic/
Additional information
Funding
References
- Vohra J, Burrows G, Hunt D, et al. The effect of toxic and therapeutic doses of tricyclic antidepressant drugs on intracardiac conduction. Eur J Cardiol.1975;3(3):219–227.
- Rawling DA, Fozzard HA. Effects of imipramine on cellular electrophysiological properties of cardiac purkinje fibers. J Pharmacol Exp Ther. 1979;209(3):371–375.
- Nattel S, Mittleman M. Treatment of ventricular tachyarrhythmias resulting from amitriptyline toxicity in dogs. J Pharmacol Exp Ther. 1984;231(2):430–435.
- Sasyniuk BI, Jhamandas V. Mechanism of reversal of toxic effects of amitriptyline on cardiac purkinje fibers by sodium bicarbonate. J Pharmacol Exp Ther. 1984;231(2):387–394.
- Boehnert MT, Lovejoy FH. Jr. Value of the QRS duration versus the serum drug level in predicting seizures and ventricular arrhythmias after an acute overdose of tricyclic antidepressants. N Engl J Med. 1985;313(8):474–479. doi: 10.1056/nejm198508223130804.
- Sasyniuk BI, Jhamandas V, Valois M. Experimental amitriptyline intoxication: treatment of cardiac toxicity with sodium bicarbonate. Ann Emerg Med. 1986;15(9):1052–1059. doi: 10.1016/s0196-0644(86)80128-7.
- Caravati EM, Bossart PJ. Demographic and electrocardiographic factors associated with severe tricyclic antidepressant toxicity. J Toxicol Clin Toxicol. 1991;29(1):31–43. doi: 10.3109/15563659109038595.
- Foulke GE, Albertson TE. QRS interval in tricyclic antidepressant overdosage: inaccuracy as a toxicity indicator in emergency settings. Ann Emerg Med. 1987;16(2):160–163. doi: 10.1016/s0196-0644(87)80006-9.
- Lavoie FW, Gansert GG, Weiss RE. Value of initial ECG findings and plasma drug levels in cyclic antidepressant overdose. Ann Emerg Med. 1990;19(6):696–700. doi: 10.1016/s0196-0644(05)82482-5.
- Foulke GE. Identifying toxicity risk early after antidepressant overdose. Am J Emerg Med.1995;13(2):123–126. doi: 10.1016/0735-6757(95)90076-4.
- Bailey B, Buckley NA, Amre DK. A meta-analysis of prognostic indicators to predict seizures, arrhythmias or death after tricyclic antidepressant overdose. J Toxicol Clin Toxicol. 2004;42(6):877–888. doi: 10.1081/clt-200035286.
- Bruccoleri RE, Burns MM. A literature review of the use of sodium bicarbonate for the treatment of QRS widening. J Med Toxicol.2016;12(1):121–129. doi: 10.1007/s13181-015-0483-y.
- Barber MJ, Starmer CF, Grant AO. Blockade of cardiac sodium channels by amitriptyline and diphenylhydantoin. Evidence for two use-dependent binding sites. Circ Res. S1991;69(3):677–696. doi: 10.1161/01.res.69.3.677.
- Niemann JT, Bessen HA, Rothstein RJ, et al. Electrocardiographic criteria for tricyclic antidepressant cardiotoxicity. Am J Cardiol. 1986;57(13):1154–1159. doi: 10.1016/0002-9149(86)90691-0.
- Liebelt EL, Francis PD, Woolf AD. ECG lead aVR versus QRS interval in predicting seizures and arrhythmias in acute tricyclic antidepressant toxicity. Ann Emerg Med. 1995;26(2):195–201. doi: 10.1016/s0196-0644(95)70151-6.
- Berkovitch M, Matsui D, Fogelman R, et al. Assessment of the terminal 40-millisecond QRS vector in children with a history of tricyclic antidepressant ingestion. Pediatr Emerg Care. 1995;11(2):75–77. doi: 10.1097/00006565-199504000-00004.
- Yates C, Manini AF. Utility of the electrocardiogram in drug overdose and poisoning: theoretical considerations and clinical implications. Curr Cardiol Rev. 2012;8(2):137–151. doi: 10.2174/157340312801784961.
- Bebarta VS, Phillips S, Eberhardt A, et al. Incidence of Brugada electrocardiographic pattern and outcomes of these patients after intentional tricyclic antidepressant ingestion. Am J Cardiol. 2007;100(4):656–660. doi: 10.1016/j.amjcard.2007.03.077.
- Hughes AR, Lin A, Hendrickson RG.. Clinical and patient characteristics associated with severe outcome in diphenhydramine toxicity. Clin Toxicol . 2021;59(10):918–925. doi: 10.1080/15563650.2021.1891244.
- Buckley NA, Chevalier S, Leditschke IA, et al. The limited utility of electrocardiography variables used to predict arrhythmia in psychotropic drug overdose. Crit Care.2003;7(5):R101–107. doi: 10.1186/cc2345.
- Isbister GK, Duffull SB. Quetiapine overdose: predicting intubation, duration of ventilation, cardiac monitoring and the effect of activated charcoal. Int Clin Psychopharmacol. 2009;24(4):174–180. doi: 10.1097/YIC.0b013e32832bb078.
- Simon M, Heard K. May . Are antimuscarinic effects common in hydroxyzine overdose? A cohort analysis of antimuscarinic effects in hydroxyzine and diphenhydramine-poisoned patients. Clin Toxicol. 2023;61(5):379–386. doi: 10.1080/15563650.2023.2200575.
- Gummin DD, Mowry JB, Beuhler MC, et al. 2022 Annual report of the national poison data system(®) (NPDS) from America’s poison centers(®): 40th annual report. Clin Toxicol . 2023;61(10):717–939. doi: 10.1080/15563650.2023.2268981.
- Love JS, Karshenas DL, Spyres MB, et al. The toxicology investigators consortium case registry-the 2021 annual report. J Med Toxicol. 2022;18(4):267–296. doi: 10.1007/s13181-022-00910-6.
- Kuo CC, Huang RC, Lou BS. Inhibition of Na(+) current by diphenhydramine and other diphenyl compounds: molecular determinants of selective binding to the inactivated channels. Mol Pharmacol. 2000;57(1):135–143.
- Kim DH, Park KS, Park SH, et al. Norquetiapine blocks the human cardiac sodium channel Na(v)1.5 in a state-dependent manner. Eur J Pharmacol. 2020;885:173532. Epub 2020. doi: 10.1016/j.ejphar.2020.173532.
- Bardai A, Amin AS, Blom MT, et al. Sudden cardiac arrest associated with use of a non-cardiac drug that reduces cardiac excitability: evidence from bench, bedside, and community. Eur Heart J. 2013;34(20):1506–1516. doi: 10.1093/eurheartj/eht054.
- O'Leary ME, Chahine M. Cocaine binds to a common site on open and inactivated human heart (Na(v)1.5) sodium channels. J Physiol. 2002;541(Pt 3):701–716. doi: 10.1113/jphysiol.2001.016139.
- Caillier B, Pilote S, Castonguay A, et al. QRS widening and QT prolongation under bupropion: a unique cardiac electrophysiological profile. Fundam Clin Pharmacol. 2012;26(5):599–608. doi: 10.1111/j.1472-8206.2011.00953.x.
- Shaikh Qureshi WM, Latif ML, Parker TL, et al. Evaluation of bupropion hydrochloride developmental cardiotoxic effects in chick cardiomyocyte micromass culture and stem cell derived cardiomyocyte systems. Birth Defects Res B Dev Reprod Toxicol.2014;101(5):371–378. doi: 10.1002/bdrb.21121.
- Cheng S, Larson MG, Keyes MJ, et al. Relation of QRS width in healthy persons to risk of future permanent pacemaker implantation. Am J Cardiol. 2010;106(5):668–672. doi: 10.1016/j.amjcard.2010.04.021.
- Ilkhanoff L, Soliman EZ, Ning H, et al. Factors associated with development of prolonged QRS duration over 20 years in healthy young adults: the coronary artery risk development in young adults study. J Electrocardiol. 2012;45(2):178–184. doi: 10.1016/j.jelectrocard.2011.11.001.