ABSTRACT
Introduction: Healthcare workers (HCWs) often experience morally challenging situations in their workplaces that may contribute to job turnover and compromised well-being. This study aimed to characterize the nature and frequency of moral stressors experienced by HCWs during the COVID-19 pandemic, examine their influence on psychosocial-spiritual factors, and capture the impact of such factors and related moral stressors on HCWs’ self-reported job attrition intentions.
Methods: A sample of 1204 Canadian HCWs were included in the analysis through a web-based survey platform whereby work-related factors (e.g. years spent working as HCW, providing care to COVID-19 patients), moral distress (captured by MMD-HP), moral injury (captured by MIOS), mental health symptomatology, and job turnover due to moral distress were assessed.
Results: Moral stressors with the highest reported frequency and distress ratings included patient care requirements that exceeded the capacity HCWs felt safe/comfortable managing, reported lack of resource availability, and belief that administration was not addressing issues that compromised patient care. Participants who considered leaving their jobs (44%; N = 517) demonstrated greater moral distress and injury scores. Logistic regression highlighted burnout (AOR = 1.59; p < .001), moral distress (AOR = 1.83; p < .001), and moral injury due to trust violation (AOR = 1.30; p = .022) as significant predictors of the intention to leave one’s job.
Conclusion: While it is impossible to fully eliminate moral stressors from healthcare, especially during exceptional and critical scenarios like a global pandemic, it is crucial to recognize the detrimental impacts on HCWs. This underscores the urgent need for additional research to identify protective factors that can mitigate the impact of these stressors.
HIGHLIGHTS
This study explored the nature of moral stressors encountered by health care workers, along with impacts on moral injury and intentions to leave their jobs.
Morally distressing encounters were common, with the most prevalent and distressing experiences being organizational or team-based in nature.
Findings revealed that severity of moral injury, particularly related to trust violation or betrayal, was a key factor influencing healthcare workers’ intentions to leave their jobs.
Introducción: Los trabajadores de la salud (TS) a menudo experimentan situaciones moralmente desafiantes en sus lugares de trabajo que pueden contribuir a la rotación laboral y comprometer su bienestar. Este estudio tuvo como objetivo caracterizar la naturaleza y frecuencia de los estresores morales experimentados por los TS durante la pandemia por COVID-19, examinar su influencia en los factores psicosociales-espirituales y capturar el impacto de dichos factores y los estresores morales relacionados a las intenciones de abandono laboral de los TS.
Métodos: Se incluyó en el análisis una muestra de 1.204 TS canadienses a través de una encuesta en plataforma web en la que se analizaron factores relacionados con el trabajo (p. ej., años trabajados como TS, brindando atención a pacientes con COVID-19), angustia moral (evaluado con MMD-HP), daño moral (evaluado con MIOS), sintomatología de salud mental y rotación laboral debido a angustia moral.
Resultados: Los estresores morales con mayor frecuencia reportados y tasas de angustia incluyeron requerimientos de atención al paciente que excedieron la capacidad en la que los TS se sentían seguros/cómodos de manejarlos, falta de disponibilidad de recursos y la creencia de que la administración no estaba abordando los problemas que comprometían la atención al paciente. Los participantes que consideraron dejar sus trabajos (44%; N = 517) demostraron mayores puntuaciones de angustia y daño moral. La regresión logística destacó el burnout (AOR = 1,59; p < 0,001), la angustia moral (AOR = 1,83; p < 0,001) y el daño moral debido a la violación de la confianza (AOR = 1,30; p = 0,022) como predictores significativos asociados a la intención de dejar el trabajo.
Conclusión: Si bien, es imposible eliminar por completo los estresores morales de la atención sanitaria, especialmente durante escenarios críticos y excepcionales como una pandemia global, es crucial reconocer los impactos perjudiciales para los TS. Esto subraya la necesidad urgente de realizar investigaciones adicionales para identificar factores protectores que puedan mitigar el impacto de estos factores estresantes.
1. Introduction
Healthcare workers (HCWs) face a multitude of morally challenging situations in the workplace due to the nature of their profession. These challenges may include encountering life-and-death decisions, balancing patient autonomy against the duty to provide appropriate care, and adapting to organizational pressures related to resource limitations, financial constraints, efficiency demands, and productivity targets (Corley et al., Citation2005; Riedel et al., Citation2022). Moral distress is a term most commonly used to describe HCWs’ inability to adhere to their own personal values due to internal or external constraints (Jameton, Citation1993). Exposure to distressing situations of this nature has been shown to induce enduring functional impairments and psychological consequences, including increased levels of depression, anxiety, and posttraumatic stress disorder (PTSD) (Amsalem et al., Citation2021; Colville et al., Citation2019; Mantri et al., Citation2020; Plouffe et al., Citation2021). Data collected during the recent COVID-19 pandemic has shown that moral distress is linked to burnout (Plouffe et al., Citation2021), and in light of reported global HCW shortages (Poon et al., Citation2022), its impact on patient care, job satisfaction, productivity, and attrition, should not be understated (De Hert, Citation2020). Despite the urgent need to address the healthcare crisis, including significant demoralization and prevalence of moral stressors experienced by HCWs (Mewborn et al., Citation2023), the extent to which exposure to moral stressors relates to psychosocial impairments among HCWs and how these factors independently relate to negative professional outcomes such as job turnover are not well-understood.
To compound the issue of healthcare system strain, public health emergencies, such as mass casualty events, endemics, and pandemics, pose unique challenges to HCWs, often summarized as the three ‘Rs’: rationing, restrictions, and responsibilities (Wynia, Citation2007). In the case of the COVID-19 pandemic, these challenges were reflected in limitations placed on the use of resources (e.g. insufficient personal protective equipment [PPE]; Burki, Citation2020), the repeated delays or cancellations of diagnostic and surgical procedures (COVIDSurg Collaborative, Citation2020; The Lancet Rheumatology, Citation2021), and changes to assigned occupational duties and responsibilities (e.g. caring for highly contagious patients in unfamiliar care environments; Woo & Freeze, Citation2022). A survey of HCWs conducted by Statistics Canada (Citation2022) found that over 95% of respondents reported that their jobs had been impacted by the pandemic, with the majority (86.5%) reporting greater work-related stress. Other pandemic-related experiences reported by HCWs included dramatically increased workloads (e.g. increased screening and infection control requirements; 74.6%) and being required to work outside one’s usual scope of practice (55.5%; Statistics Canada, Citation2022). Despite the potential moral and ethical implications of constraints imposed by such stressors (Jameton, Citation1984), research on the consequences of moral distress experienced by HCWs during the pandemic has been limited, with inconsistencies observed in both findings (e.g. moral stress exposure higher vs. lower in ICU nurses, Donkers et al., Citation2021; Lake et al., Citation2022, respectively) as well as constructs measured (e.g. moral stress exposure vs. moral injury outcomes; Lake et al., Citation2022 and Wang et al., Citation2022, respectively). Operationalizations of moral distress as measured by different scales further obscure the nature and significance of moral stressors and their effects in the context of the COVID-19 pandemic (e.g. Measure of Moral Distress for Healthcare Professionals [MMD-HP] vs. Moral Distress Thermometer, Donkers et al., Citation2021; Miljeteig et al., Citation2021, respectively). As such, there is little clarity about which types of moral stressors have been most prevalent and potentially traumatogenetic among HCWs during the pandemic. Further, quantitative studies exploring the link between moral distress among HCWs and vocational outcomes (e.g. the intention to leave one’s employment) have been limited to bivariate explorations (Colville et al., Citation2019; Hally et al., Citation2021; Sheppard et al., Citation2022; Shoorideh et al., Citation2015; Silverman et al., Citation2022). Whether moral distress is an independent predictor of intentions to leave one’s position when considering the potential impact of occupation-specific factors, related constructs (e.g. moral injury), and factors such as burnout and psychiatric symptoms, also remains largely unexplored.
Adequately capturing the psychological sequelae of exposure to moral stressors is contingent upon developing and applying appropriate theoretical frameworks and operationalizations of moral injury and moral distress (Varcoe et al., Citation2012). Although there is a recent explosion of interest in, and research on, moral injury and moral distress, these two related (and often interchangeably used) constructs have historically lacked conceptual clarity (Riedel et al., Citation2022). Both moral injury and moral distress fundamentally refer to the psychological, social, and spiritual consequences experienced in the aftermath of an action/inaction or witnessing an event that is perceived to violate deeply held values and moral commitments. While both moral distress and injury are characterized by heightened feelings of guilt, shame, anger, and withdrawal (Jameton, Citation1993; Litz et al., Citation2009; Varcoe et al., Citation2012; Wilkinson, Citation1987), moral injury has been considered a more severe and incapacitating outcome on a spectrum of psychosocial-spiritual impairments, which, unlike moral distress, involves disturbances to the sufferer’s core moral beliefs and identity (Litz & Kerig, Citation2019). Importantly, studies assessing moral distress in the healthcare context often assume implications related to the consequences noted above, whilst most moral distress scales capture only a single, generalized stress reaction to potential moral stressors and, therefore, should only be understood to capture exposure rather than expression. Importantly, this limitation precludes the formation of accurate inferences around the relative effects of exposure and the nature of expressed outcomes (i.e. injury presentation) on tertiary outcomes (e.g. job turnover). Recent efforts to enhance the conceptual clarity of what is meant by moral injury (Litz & Kerig, Citation2019) and the availability of psychometrically valid measurements of moral injury outcomes (Litz et al., Citation2022) provide an opportunity to gain more accurate insights into this phenomenon and in turn, create opportunities for interventions to mitigate the downstream effects of exposure to moral stressors in the healthcare context (Kolbe & de Melo-Martin, Citation2023).
The objectives of the present study, therefore, are to (a) describe the nature and impacts of moral stressors encountered in a large sample of HCWs during the COVID-19 pandemic, and (b) examine the relative influences of moral stressor exposure and outcomes on HCWs’ intentions to leave their jobs.
2. Methods
2.1. Participants and procedures
Data were drawn from the baseline timepoint of a larger longitudinal study exploring the psychological impact of the COVID-19 pandemic on Canadian HCWs (see Liu et al., Citation2021, for detailed methodology and study protocol). Participants were eligible for inclusion if they were 18 years of age or older and employed as HCWs in Canada at some point during the COVID-19 pandemic. Baseline data were collected using an online survey between June 26, 2020, and December 31, 2020. This study was approved by the Institutional Research Ethics Boards of Western University (WREM #115894) and Lawson Health Research Institute (ReDA #9968).
2.2. Measures
2.2.1. Work context and demographics
Participants were asked what percentage of their workload involved the direct provision of care to patients, the number of years they spent working as HCWs, and whether they had been involved in providing care to suspected or confirmed COVID-19 patients. Participants also completed questions about their occupational roles and responsibilities (e.g. occupation type, workplace setting) and demographic characteristics (e.g. gender, age, province of residence).
2.2.2. Exposure to moral stressors and stressor-specific moral distress
Exposure to moral stressors was evaluated using the MMD-HP (Epstein et al., Citation2019), which is a version of the Moral Distress Scale-Revised (MDS-R; Hamric et al., Citation2012) that was modified to better capture team- and system-level sources of moral distress, and to be appropriate for diverse healthcare disciplines. Participants were presented with 27 potentially morally challenging situations specific to the HCW context and were prompted to list any additional situations they may have found morally challenging but that were not covered by the existing items. Participants rated each original and ‘other’ situation according to its frequency (0 = never to 4 = very frequently) and perceived level of distress (0 = none to 4 = very distressing). According to MMD-HP original formulation (Epstein et al., Citation2019), participants are required to provide both frequency and distress ratings for all items, even if they have not experienced the situation personally. For the present study, however, participants only provided distress ratings for items with frequency ratings of 1 or higher. This change was made to appropriately capture only the level of distress of specific stressors that respondents had personally encountered. Composite scores of moral distress exposure were then calculated by multiplying participants’ frequency scores by their distress scores and then summing the products on the original 27 items, with possible scores ranging from 0–432 (Epstein et al., Citation2019). To reflect the nuanced relation between moral stressor exposure and expression, we also calculated separate scores for exposure frequency and level of distress by summing the respective ratings across the original 27 items. For all three summary scores (i.e. total distress, frequency, and level of distress), higher scores represented more severe ratings. Prior to calculating MMD-HP scores, open-ended (‘other’) responses were reviewed by study investigators and items that were deemed to reflect original item content had their associated frequency and distress ratings recoded into the original items (see below). Where participants had already input ratings for the original MMD-HP item, the highest ratings were retained.
2.2.3. Moral injury
Moral injury was measured using the 14-item Moral Injury Outcome Scale (MIOS; Litz et al., Citation2022). Participants were instructed to reflect upon the event that currently causes them the most moral distress. They were then asked to rate their agreement from 0 (strongly disagree) to 4 (strongly agree) for statements reflecting moral feelings and beliefs about themselves, the world, and others (reflecting over the past month). Sum scores were calculated for the full scale and two subscales, reflecting shame-related outcomes (7 items; e.g. People would hate me if they really knew me) and trust violation-related outcomes (7 items; e.g. I have lost faith in humanity). Past research supports the validity and reliability of the MIOS total scale and subscales (α from .72 to .90; Litz et al., Citation2022), with good internal consistency in the current sample (from .78 to .87).
2.2.4. Mental health symptoms
Symptoms of PTSD were assessed using the 20-item PTSD checklist for the DSM-5 (PCL-5; Weathers et al., Citation2013), in which participants indicated the extent to which they experienced PTSD symptoms in the past month from 0 (not at all) to 4 (extremely). Depressive symptoms were assessed using the 9-item Patient Health Questionnaire (PHQ-9; Spitzer et al., Citation1999), in which participants indicated how frequently they experienced depressive symptoms in the past two weeks from 0 (not at all) to 3 (nearly every day). General anxiety symptoms were assessed using the 7-item General Anxiety Disorder scale (GAD-7; Spitzer et al., Citation2006), where participants indicated how frequently they had experienced anxiety symptoms over the past two weeks from 0 (not at all) to 3 (nearly every day). Sum scores were calculated for each scale, with higher scores indicative of greater symptom severity. Burnout was assessed using the 9-item Expanded Well-Being Index (WBI; Dyrbye et al., Citation2016), whereby participants rated burnout on seven dichotomous (yes/no) items, indicated whether they found their work meaningful (single item, 1 = very strongly disagree to 7 = very strongly agree), and whether they had enough time for personal/family life (one item, 1 = strongly disagree to 5 = strongly agree). Total WBI scores were calculated according to scoring guidelines, ranging from −2 to 9, with higher scores indicating higher burnout (Dyrbye et al., Citation2016). Research has supported the validity and reliability of the scales, with good internal consistency in the current sample for PCL-5 (e.g. α = .94; Blevins et al., Citation2015; current sample α = .96), PHQ-9 (e.g. α = .90; Kroenke et al., Citation2001; current sample α = .90), GAD-7 (e.g. α = .89; Löwe et al., Citation2008; current sample α = .93), and WBI (Dyrbye et al., Citation2016; current sample α = .67).
2.2.5. Intention to leave job due to moral distress
Whether participants wished to leave their jobs in response to exposure to moral stressors was assessed using an item embedded in the MMD-HP: ‘Are you considering leaving your position now due to moral distress?’ (yes/no).
2.3. Data analytic strategy
2.3.1. Pre-analysis
Analyses were restricted to participants with complete MMD-HP data because the MMD-HP follows a formative measurement model, which renders missing data imputation techniques less reliable (Coltman et al., Citation2008). Mode imputation was used to estimate missing data for other self-report scores (i.e. moral injury, depression, PTSD, anxiety, and burnout) for participants who completed at least 80% of the corresponding scale. Listwise deletion was used for regression models, and pairwise deletion was used for t-tests and correlations, such that participants with more than 20% missing data on a scale were retained in the analytic frame but excluded from certain analyses. Chi-square tests were used to assess potential differences in age, gender, education, marital status, geographic region, residential area, degree of patient care, and intention to leave their job between individuals with complete and incomplete MMD-HP data, and between individuals with more than 20% and 20% or less missing data on the MIOS.
2.3.2. Qualitative analysis of MMD-HP responses
Any additional (i.e. ‘other’) moral stressors provided by participants were analyzed by a team of three researchers (IK, TL, CF) with NVivo 12 Pro using a process outlined by Braun and Clarke (Citation2006). The steps involve (a) familiarizing with the data, (b) generating and applying initial codes to responses, (c) searching for themes by sorting codes into categories, (d) reviewing themes for cohesiveness and representativeness with the data, (e) defining and naming themes, and (f) reporting findings (Braun & Clarke, Citation2006). This process was modified whereby the original 27 MMD-HP items were included as a priori codes, such that responses that replicated any original items could be flagged and, if all coders agreed, have their frequency and distress ratings incorporated into their respective original items for quantitative analyses. Responses deemed distinct from the original 27 MMD-HP items were analyzed in accordance with the aforementioned 6-step process (Braun & Clarke, Citation2006).
2.3.3. Quantitative analysis
Descriptive statistics were calculated for continuous variables, and bivariate correlations were calculated for all predictors used in regression modelling. To understand HCWs’ experiences with moral stressors, their MMD-HP frequency and distress ratings were visualized and sorted according to each item’s derived importance, where an item’s importance score was generated by multiplying each response option (e.g. 4 = very distressing) by the number of respondents who selected that option, and then summing those products. The most important items thus were those encountered most frequently or felt with the most distress according to the greatest number of participants.
Independent samples t-tests assessed group differences in the degree of moral stress exposure as well as moral injury between participants who were considering leaving their jobs and those who reported they were not considering leaving. A conservative p-value of < .01 was adopted for t-test significance testing to account for familywise error.
Three-step hierarchical logistic regression models were run to predict the intention to leave one’s job due to moral distress. Predictors were entered as follows: Step 1. occupational variables (years of experience, COVID-19 contact, and percentage of patient involvement); Step 2. MMD-HP score and MIOS score; and Step 3. mental health outcomes (PHQ-9, PCL-5, GAD-7, WBI scores). To prevent multicollinearity among predictor variables, predictors which exhibited a correlation of .80 or higher were entered in separate models for Step 2. Similarly, MMD-HP and MIOS subscale totals were individually entered in Step 2 if their correlations were less than .80; otherwise, full-scale totals were used. Where relevant, variables were standardized prior to entry in the logistic regression models to account for different score ranges. All quantitative analyses and visualizations were performed using R Version 4.1.3.
3. Results
The analytic frame consisted of 1,204 HCWs. The most common age range for participants was between 41 and 60 years (n = 499; 48.1%), women (n = 921; 88.9%), and from Ontario or Quebec (n = 418; 56.9%). Participant occupations varied, with the most common occupation being a nurse (n = 493; 45.7%). Most participants worked directly with patients (n = 1,046; 88.0%), with patient work comprising 75–100% of their role (n = 869; 72.4%). Over half of the participants (n = 698; 58.1%) were directly engaged in clinical activities (e.g. diagnosing, treating) with COVID-19 patients. Additional participant characteristics are provided in .
Table 1. Participant sociodemographic characteristics.
3.1. Pre-analysis
Apart from age (χ2 = 9.00, p = .03) and job function (χ2 = 6.95, p = .01), participants with complete and incomplete MMD-HP data were similar with respect to demographic characteristics, occupational factors, and the proportion who intended to leave their jobs. Compared to those who did not complete the MMD-HP, those who completed the MMD-HP had a smaller proportion of participants aged 41–60 years, a larger proportion of participants aged 26–40 years, and a larger proportion of participants working directly with patients compared to those with other primary responsibilities. Participants with more than 20% missing MIOS data were similar on all demographic and occupational variables compared to those with 20% or less missing MIOS data; however, there was a larger proportion of participants who wanted to leave their jobs among those with 20% or less missing MIOS data (χ2 = 6.60, p = .01). Distributions for continuous variables were normal, based on accepted standards (Kline, Citation2016).
3.2. Experiences with morally distressing situations
Frequency and distress ratings on MMD-HP ‘other’ fields were reassigned to original items for 73 and 74 participants, respectively (see Supplementary Figure S1 and S2 for original [i.e. pre-processed] distribution of responses). The frequency and distress ratings in response to potential moral stressors on the MMD-HP are shown in and , respectively. Most participants reported experiencing at least one of the situations ‘very frequently’ (65%) and found at least one of the situations to be ‘very distressing’ (78%). Overall, participants reported some degree of exposure to each of the situations presented (i.e. there were no situations that either never occurred or never caused participants any stress). Of the sample, 21% also described experiencing an ‘other’ situation not captured by the original MMD-HP, which fell into one of four broad themes: inadequate resources or resource allocation, unsupportive work environment, patient-related issues, and personal issues (i.e. highlighting personal distress/burden associated with their workplace). The number of participants who described experiencing situations within each of the themes and related subthemes is shown in .
Figure 1. Reported frequencies of exposure to moral stressors in the workplace, ordered by sample proportions. Higher ordering weight is applied to stressors with higher endorsement of frequency. Numbers in parentheses reflect the corresponding MMD-HP scale item number. ‘Other misc experiences’ refer to the morally distressing experiences that participants described in their open-ended responses.
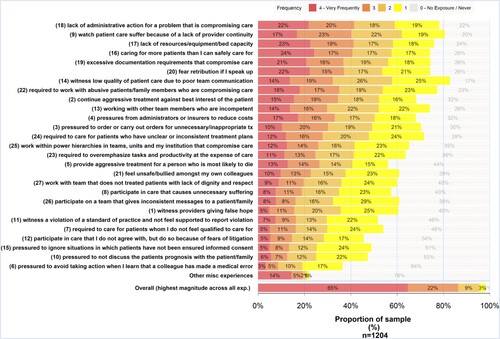
Figure 2. Reported level of distress associated with moral stressors in the workplace, ordered by sample proportions. Note. Higher ordering weight is applied to stressors with higher endorsement of distress severity. Numbers in parentheses reflect the corresponding MMD-HP scale item number. ‘Other misc experiences’ refer to the morally distressing experiences that participants described in their open-ended responses.
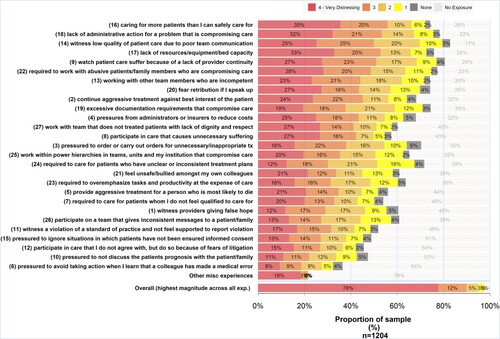
Table 2. Themes from the additional open-ended moral distress situations provided on the MMD-HP.
3.3. Distress and intention to leave job
Means and standard deviations for continuous variables and bivariate correlations for all predictor variables are reported in . Of the 1,184 individuals (98%) who answered the attrition question, 517 participants (44%) indicated they were considering leaving their jobs due to situations presented in the MMD-HP. Compared to participants who did not consider leaving their job, those who did consider leaving had significantly higher scores for MMD-HP total, t(1032.1) = 12.99, p < .001, frequency of exposure, t(1182) = 13.05, p < .001, and level of distress associated with stressors encountered, t(1159) = 10.42, p < .001. The same pattern was observed for total moral injury scores, t(701) = 7.33, p < .001, and for subscale scores of moral injury-related shame, t(662.8) = 5.31, p < .001, and trust-violation, t(701) = 7.64, p < .001.
Table 3. Descriptive Statistics and Bivariate Relations.
Due to most participants having 75% or more of their work comprising patient care (see ), this variable was collapsed into a binary variable (i.e. less than 75% patient care, 75% or more patient care) for the regression analyses. MIOS subscales were individually entered due to intercorrelations less than .80 and the MMD-HP total score was entered due to a high intercorrelation (r = .88). Unstandardized regression estimates (Step 1) and partially standardized regression coefficients (i.e. predictors only; Steps 2 and 3) are presented in . None of the occupational variables were significantly related to the intention to leave one’s job. In Step 2, MMD-HP total and MIOS trust-violation subscale scores were associated with considering leaving the job due to moral distress, whereas the MIOS shame subscale score was not. In Step 3, MMD-HP total and MIOS trust-violation subscale scores remained significant predictors (p < .001; p = .022, respectively) after considering symptom severity of PTSD, depression, anxiety, and burnout. Among the mental health variables, burnout was the only independent predictor of intention to leave one’s job (p < .001). Controlling for the other variables, each standard deviation increase in the predictor increased the odds of considering leaving one’s job by 83%, 30%, and 59% for moral distress, moral injury due to trust violation, and burnout, respectively. The final model accounted for 24% of the variance in the intention to leave one’s job.
Table 4. Hierarchical logistic regression predicting intention to leave job due to moral stressor exposure (n = 689).
4. Discussion
This study characterizes the nature and prevalence of potential moral stressors and their effects as experienced by HCWs during the COVID-19 pandemic. Our results showed that HCWs reported increased prospects of leaving their jobs due to the experience and impacts of moral stressors, an outcome that is consistent with the findings of others using the same measure in ICUs (Petrisor et al., Citation2021; Silverman et al., Citation2022), neonatal ICUs (Hally et al., Citation2021), and with nurses more generally (Sheppard et al., Citation2022). Using categorisations provided by Epstein et al. (Citation2019) to classify moral stressors, four out of the five most frequently endorsed situations were classified as originating at the organizational level, which is consistent with findings from smaller-scale studies of HCWs during the COVID-19 pandemic (Latimer et al., Citation2022; Petrisor et al., Citation2021). Stressors that fell into both the high-frequency and high-distress categories included those involving patient care requirements that exceeded the capacity that HCWs felt comfortable managing, a perceived lack of resource availability, and a belief that healthcare administrators were not adequately addressing issues that had the potential to compromise the quality of patient care. The latter theme, which was also identified in participants’ free-form responses, may broadly capture moral stressors experienced by HCWs which, due to their relative rarity when the measure was created (i.e. prior to the onset of COVID-19), were not included as potential MMD-HP items.
Based on the nature of the questions asked and the scale’s implied formative structure (Coltman et al., Citation2008), the MMD-HP most appropriately is considered a measure of the degree of reported exposure to moral stressors, rather than an indicator of the severity of psychological outcomes (Houle et al., Citation2023). For instance, in its typical application, the MMD-HP treats moral stressor exposures as operationally equivalent to the experience of moral distress (i.e. psychological disturbance) in that frequency and level of distress prompted by the stressor are treated as having equal weight relative to the situation’s impact on the individual. As such, events with high frequencies and low intensities could be scored and considered to be just as distressing as those of low frequency, but which prompt a high level of distress. As noted recently by Kolbe and de Melo-Martin (Citation2023), this practice confounds the true nature of moral stressors and their outcomes and obscures appropriate targets for effective upstream (i.e. organizational) and downstream (i.e. psychological care) interventions. In contrast, the MIOS captures a broader range of behavioural and psychosocial-spiritual disturbances (e.g. guilt, shame, loss of faith in humanity) appropriately conceptualized as responses to moral stressor exposure and operationalized collectively as the outcome of moral injury. In addition, all items are anchored to the ‘worst/most currently morally distressing event’ and captured within a past-month period, which is consistent with common models of psychiatric taxonomy (DSM-5; American Psychiatric Association, Citation2013). Results from this study, therefore, provide useful information by separating out the nature, frequency and level of distress prompted by particular moral stressors experienced during the COVID-19 pandemic as well as the morally injurious outcomes, information which is currently absent from existing research in this domain (Dean et al., Citation2020; Kolbe & de Melo-Martin, Citation2023).
Indeed, the frequency of organizational-level moral stressors (as they are presently observed) may explain why MIOS trust-violation subscale scores significantly predicted attrition intention in this study, while MIOS shame subscale scores did not. According to Litz et al. (Citation2009), feelings of shame and guilt can stem from a dissonance between how an individual believes they should have acted to alter a morally transgressive situation and how they actually acted, which may have led to a particular negative outcome. As many of the scenarios endorsed in this study are reflective of HCWs’ perceptions of lacking personal agency to influence outcomes, it follows that HCWs who feel powerless to mitigate potential moral stressors are also those who express a lack of trust in those making decisions that constrict such agency (e.g. healthcare administrators). While the demonstrated effects of system-level causes of moral stress are not novel (Latimer et al., Citation2022; Silverman et al., Citation2022), the increased strains imposed by the pandemic, as well as improved methods for measuring moral stress outcomes (Litz et al., Citation2022), allows for a clearer picture of such variables and their effects. Given the vulnerabilities of the healthcare system, which were exposed by the COVID-19 pandemic, appropriate separation of and communication about moral stress exposure and its effects is likely to provide an impetus for exploring enduring solutions to this problem (Kolbe & de Melo-Martin, Citation2023). Notably, factors such as adequate organization and distribution of patient caseloads, strong communication between leaders and employees, policies promoting HCW autonomy, and inclusive, collaborative, and flexible work environments may help reduce these tensions (Lake et al., Citation2022; Murphy et al., Citation2022). More focus on HCW engagement in co-designing institutional policies should also be explored, with approaches that can be drawn from the employee experience body of literature (Murphy et al., Citation2022).
Despite previous research which demonstrated associations between moral stress exposure and mental health outcomes such as PTSD, depression and anxiety (Amsalem et al., Citation2021; Colville et al., Citation2019; Mantri et al., Citation2020; Plouffe et al., Citation2021), we observed that among the mental health symptom scales included in the models, burnout alone significantly predicted intention to leave one’s job as a consequence of exposure to moral stressors. One explanation for this finding may be that where moral stressors precede mental health problems, the moral nature of the events may serve to catalyse various presentations of distress (i.e. no specific presentation stands out independently), serving as a transdiagnostic risk factor (Easterbrook et al., Citation2023). Given that burnout is considered an occupational problem, and this study focuses on occupational stressors, it may be that in the context of the COVID-19 pandemic, which presented unique challenges and strong demand on HCWs, this aspect of work-related mental health difficulties was most dominant relative to other problems. Still, these findings highlight the extent to which organizational factors beyond years of experience, extent of patient contact, and potential COVID-19 exposure are likely at play in intentions to leave one’s job. They, therefore, highlight the need for systemic interventions.
Of note, due to the high correlation between the frequency and level of distress subscales on the MMD-HP (r = .88), it was not possible to examine the effects of these features on attrition intentions separately. Still, given advances in our understanding of the utility of the MMD-HP and similar scales (i.e. as measures of degree of exposure rather than outcomes; Houle et al., Citation2023), findings related to MIOS outcomes are able to provide additional relevant information as to the potential impact of moral stress exposure among HCWs. Importantly, the cross-sectional nature of this analysis limits the breadth of conclusions that can be drawn. As longitudinal data become available, future analytical approaches may be better positioned to examine the moderating mechanisms of risk and protective factors, along with longitudinal trajectories of moral injury and related psychological outcomes experienced by HCWs. Future longitudinal analyses may also explore metrics of actual staff attrition and not rely on a proxy measure of the intention to leave the job. In addition, while the online survey was available to all HCWs across Canada, it may not be fully representative of the entire Canadian HCW population, which includes more than 1.6 million employees (Government of Canada, Citation2022). Moreover, our survey data may not entirely generalize to other countries, as national differences in pandemic responses and healthcare may pose unique conditions for Canadian HCWs. For instance, Canada’s pandemic response was among the most stringent worldwide and it was associated with lower death and infection rates compared to peer countries (Razak et al., Citation2022). Though, relative to other high-income countries, Canada ranks poorly on metrics of healthcare accessibility, equity, and workforce data quality (Bourgeault, Citation2021; McAlister, Citation2018). Response bias may also contribute to generalizability limits, as exemplified by a response pattern seen in this survey where younger individuals and those who worked with COVID patients being slightly more likely to complete the MMD-HP scale (other factors were not found to be related with scale completion). Another limitation is related to the design of the MMD-HP scale, in that the wording of the question capturing the intention to leave the job explicitly refers to moral distress as being one of the reasons behind this intention; this may have a bias towards the identified predictor variables related to moral distress. Future research should consider departing from the original design of the scale to fully disaggregate the question regarding intention to leave employment from the reasons behind this intention. Another consideration is that the event that participants may have chosen to evaluate against when completing the MIOS may not be limited to their experiences in the workplace. Whether reported features of distress were prompted by specific events captured on the MMD-HP is, therefore, unknown. Given our observation that trust-violation scores were associated most significantly with job attrition intentions, it would be worthwhile for future research to examine the extent to which these features of distress may serve to exacerbate moral appraisals of workplace stressors and related distress over time, as well as look for any relations to mental health challenges. In addition, while the MIOS is well-validated in military populations, specific validation work among HCWs is forthcoming. Finally, although this study was not designed to capture demographic information that could determine whether some groups are disproportionately burdened by factors that violate/impair HCWs’ trust, this is an important gap that requires attention.
4.1. Conclusion
This study used a well-known measure of moral stress exposure in conjunction with a measure of moral injury in a large sample of HCWs in order to assess the influence of each factor on HCWs’ intentions to leave their jobs. Our findings showed that after considering occupational factors (e.g. years of experience, patient contact) and mental health symptoms (i.e. PTSD, depression, anxiety), moral stress exposure, trust-based moral injury symptoms and burnout all impacted HCW attrition intentions. This provides further insight with respect to the nature and influence of moral stressors among HCWs during the COVID-19 pandemic. Leaders of healthcare organizations need to take intentional and effective steps to reduce preventable exposure to moral stressors (Kolbe & de Melo-Martin, Citation2023) and should pay particular attention to policies and team dynamics that create a risk for moral distress and loss of trust among HCWs (Kreh et al., Citation2021).
Figure_S2.png
Download PNG Image (659.7 KB)Figure_S1.png
Download PNG Image (620.8 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596.
- Amsalem, D., Lazarov, A., Markowitz, J. C., Naiman, A., Smith, T. E., Dixon, L. B., & Neria, Y. (2021). Psychiatric symptoms and moral injury among US healthcare workers in the COVID-19 era. BMC Psychiatry, 21(1), 1–8. https://doi.org/10.1186/s12888-021-03565-9
- Blevins, C. A., Weathers, F. W., Davis, M. T., Witte, T. K., & Domino, J. L. (2015). The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28(6), 489–498. https://doi.org/10.1002/jts.22059
- Bourgeault, I. (2021). A path to improved health workforce planning, policy & management in Canada: The critical coordinating and convening roles for the federal government to play in addressing 8% of its GDP. The School of Public Policy Publications, 14(1), https://doi.org/10.11575/sppp.v14i1.74064
- Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. https://doi.org/10.1191/1478088706qp063oa
- Burki, T. (2020). Global shortage of personal protective equipment. The Lancet Infectious Disease, 20(7), 785–786. https://doi.org/10.1016/S1473-3099(20)30501-6
- Coltman, T., Devinney, T. M., Midgley, D. F., & Venaik, S. (2008). Formative versus reflective measurement models: Two applications of formative measurement. Journal of Business Research, 61(12), 1250–1262. https://doi.org/10.1016/j.jbusres.2008.01.013
- Colville, G. A., Dawson, D., Rabinthiran, S., Chaudry-Daley, Z., & Perkins-Porras, L. (2019). A survey of moral distress in staff working in intensive care in the UK. Journal of Intensive Care Society, 20(3), 196–203. https://doi.org/10.1177/1751143718787753
- Corley, M. C., Minick, P., Elswick, R. K., & Jacobs, M. (2005). Nurse moral distress and ethical work environment. Nursing Ethics, 12(4), 381–390. https://doi.org/10.1191/0969733005ne809oa
- COVIDSurg Collaborative. (2020). Elective surgery cancellations due to the COVID-19 pandemic: Global predictive modelling to inform surgical recovery plans. British Journal of Surgery, 107(11), 1440–1449. https://doi.org/10.1002/bjs.11746
- Dean, W., Talbot, S. G., & Caplan, A. (2020). Clarifying the language of clinician distress. JAMA: The Journal of the American Medical Association, 323(10), 923–924. https://doi.org/10.1001/jama.2019.21576
- De Hert, S. (2020). Burnout in healthcare workers: Prevalence, impact and preventative strategies. Local and Regional Anesthesia, 13, 171–183. https://doi.org/10.2147/LRA.S240564
- Donkers, M. A., Gilissen, V., Candel, M., van Dijk, N. M., Kling, H., Heijnen-Panis, R., Pragt, E., van der Horst, I., Pronk, S. A., & van Mook, W. (2021). Moral distress and ethical climate in intensive care medicine during COVID-19: A nationwide study. BMC Medical Ethics, 22(1), 73. https://doi.org/10.1186/s12910-021-00641-3
- Dyrbye, L. N., Satele, D., & Shanafelt, T. (2016). Ability of a 9-item well-being index to identify distress and stratify quality of life in US workers. Journal of Occupational and Environmental Medicine, 58(8), 810–817. https://doi.org/10.1097/JOM.0000000000000798
- Easterbrook, B., Plouffe, R. A., Houle, S. A., Liu, A., McKinnon, M. C., Ashbaugh, A. R., Mota, N., Afifi, T. O., Enns, M. W., Richardson, J. D., & Nazarov, A. (2023). Moral injury associated with increased odds of past-year mental health disorders: A Canadian Armed Forces examination. European Journal of Psychotraumatology, 14(1), https://doi.org/10.1080/20008066.2023.2192622
- Epstein, E. G., Whitehead, P. B., Prompahakul, C., Thacker, L. R., & Hamric, A. B. (2019). Enhancing understanding of moral distress: The Measure of Moral Distress for Health Care Professionals. AJOB Empirical Bioethics, 10(2), 113–124. https://doi.org/10.1080/23294515.2019.1586008
- Government of Canada. (2022, December 13). Immigration matters in health care. Canada. https://www.canada.ca/en/immigration-refugees-citizenship/campaigns/immigration-matters/growing-canada-future/health.html.
- Hally, S. M., Settle, M., & Nelson, B. D. (2021). Relationship between moral distress and intent to leave a position among neonatal intensive care nurses. Advances in Neonatal Care, 21(6), E191–E198. https://doi.org/10.1097/ANC.0000000000000891
- Hamric, A. B., Borchers, C. T., & Epstein, E. G. (2012). Development and testing of an instrument to measure moral distress in healthcare professionals. AJOB Primary Research, 3(2), 1–9. https://doi.org/10.1080/21507716.2011.652337
- Houle, S., Ein, N., Gervasio, J., Plouffe, R. A., Litz, B. T., Carleton, R. N., Hansen, K., Liu, J. J. W., Ashbaugh, A. R., Callaghan, W., Thompson, M., Easterbrook, B., Smith-MacDonald, L., Rodrigues, S., Belanger, S., Bright, K., Lanius, R., Baker, C., Younger, W., … Nazarov, A. (2023). Measuring moral distress and moral injury: A systematic review and content analysis of existing scales [Manuscript submitted for publication]. Department of Psychiatry, Western University.
- Jameton, A. (1984). Nursing practice: The ethical issues Englewood Cliffs. Copyright Jim W. Summers. Business and Professional Ethics Journal, 4(1), 83.
- Jameton, A. (1993). Dilemmas of moral distress: Moral responsibility and nursing practice. AWHONN's Clinical Issues in Perinatal and Women's Health Nursing, 4(4), 542–551.
- Kline, R. B. (2016). Principles and practice of structural equation modelling (4th ed.). The Guilford Press.
- Kolbe, L., & de Melo-Martin, I. (2023). Moral distress: What are we measuring? The American Journal of Bioethics, 23(4), 46–58. https://doi.org/10.1080/15265161.2022.2044544
- Kreh, A., Brancaleoni, R., Magalini, S. C., Chieffo, D. P. R., Flad, B., Ellebrecht, N., & Juen, B. (2021). Ethical and psychosocial considerations for hospital personnel in the COVID-19 crisis: Moral injury and resilience. PLoS One, 16(4), e024960. https://doi.org/10.1371/journal.pone.0249609
- Kroenke, K., Spitzer, R., & Williams, J. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. doi:10.1046/j.1525-1497.2001.016009606.x
- Lake, E. T., Narva, A. M., Holland, S., Smith, J. G., Cramer, E., Rosenbaum, K. E. F., French, R., Clark, R. R. S., & Rogowski, J. A. (2022). Hospital nurses’ moral distress and mental health during COVID-19. Journal of Advanced Nursing, 78(3), 799–809. https://doi.org/10.1111/jan.15013
- The Lancet Rheumatology. (2021). Too long to wait: The impact of COVID-19 on elective surgery. The Lancet Rheumatology, 3(2), e83. https://doi.org/10.1016/S2665-9913(21)00001-1
- Lake, E. T., Narva, A. M., Holland, S., Smith, J. G., Cramer, E., Rosenbaum, K. E. F., French, R., Clark, R. R. S., & Rogowski, J. A. (2022). Hospital nurses' moral distress and mental health during COVID-19. Journal of Advanced Nursing, 78(3), 799–809. https://doi.org/10.1111/jan.15013
- Latimer, A. L., Otis, M. D., Mudd-Martin, G., & Moser, D. K. (2022). Moral distress during COVID-19: The importance of perceived organizational support for hospital nurses. Journal of Health Psychology, 28(3), 279–292. https://doi.org/10.1177/13591053221111850
- Litz, B. T., & Kerig, P. K. (2019). Introduction to the special issue on moral injury: Conceptual challenges, methodological issues, and clinical applications. Journal of Traumatic Stress, 32(3), 341–349. https://doi.org/10.1002/jts.22405
- Litz, B. T., Plouffe, R. A., Nazarov, A., Murphy, D., Phelps, A., Coady, A., Houle, S. A., Dell, L., Frankfurt, S., Zerach, G., Levi-Belz, Y., & Moral Injury Outcome Scale Consortium. (2022). Defining and assessing the syndrome of moral injury: Initial findings of the Moral Injury Outcome Scale consortium. Frontiers in Psychiatry, 13, 923928. https://doi.org/10.3389/fpsyt.2022.923928.
- Litz, B. T., Stein, N., Delaney, E., Lebowitz, L., Nash, W. P., Silva, C., & Maguen, S. (2009). Moral injury and moral repair in war veterans: A preliminary model and intervention strategy. Clinical Psychology Review, 29(8), 695–706. https://doi.org/10.1016/j.cpr.2009.07.003
- Liu, J. J. W., Nazarov, A., Plouffe, R. A., Forchuk, C. A., Deda, E., Gargala, D., Le, T., Bourret-Gheysen, J., Soares, V., Nouri, M. S., Hosseiny, F., Smith, P., Roth, M., MacDougall, A. G., Marlborough, M., Jetly, R., Heber, A., Albuquerque, J., Lanius, R., … Richardson, J. D. (2021). Exploring the well-being of health care workers during the COVID-19 pandemic: Protocol for a prospective longitudinal study. JMIR Research Protocols, 10(9), e32663. https://doi.org/10.2196/32663
- Löwe, B., Decker, O., Müller, S., Brähler, E., Schellberg, D., Herzog, W., & Yorck Herzberg, P. (2008). Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Medical Care, 46(3), 266–274. doi:10.1097/MLR.0b013e318160d093
- Mantri, S., Lawson, J. M., Wang, Z., & Koenig, H. G. (2020). Identifying moral injury in healthcare professionals: The Moral Injury Symptom Scale-HP. Journal of Religion and Health, 59(5), 2323–2340. https://doi.org/10.1007/s10943-020-01065-w
- McAlister, F. A., Cram, P., & Bell, C. M. (2018). Comparing Canadian health care to that in other countries: Looking beyond the headlines. CMAJ: Canadian Medical Association Journal, 190(8), E207–E208. https://doi.org/10.1503/cmaj.171527
- Mewborn, E. K., Fingerhood, M. L., Johanson, L., & Hughes, V. (2023). Examining moral injury in clinical practice: A narrative literature review. Nursing Ethics, 30, 960–974. https://doi.org/10.1177/09697330231164762
- Miljeteig, I., Forthun, I., Hufthammer, K. O., Engelund, I. E., Schanche, E., Schaufel, M., & Onarheim, K. H. (2021). Priority-setting dilemmas, moral distress and support experienced by nurses and physicians in the early phase of the COVID-19 pandemic in Norway. Nursing Ethics, 28(1), 66–81. https://doi.org/10.1177/0969733020981748
- Murphy, T. G., Sampalli, T., Bourque Bearskin, L., Cashen, N., Cummings, G., Elliott Rose, A., Etowa, J., Grinspun, D., Jones, E. W., Lavoie-Tremblay, M., MacMillan, K., MacQuarrie, C., Martin-Misener, R., Oulton, J., Ricciardelli, R., Silas, L., Thorne, S., & Villeneuve, M. (2022). Investing in Canada’s nursing workforce post-pandemic: A call to action. FACETS, 7, 1051–1120. https://doi.org/10.1139/facets-2022-0002
- Petrisor, C., Breazu, C., Doroftei, M., Maries, I., & Popescu, C. (2021). Association of moral distress with anxiety, depression, and an intention to leave among nurses working in intensive care units during the COVID-19 pandemic. Healthcare, 9(10), https://doi.org/10.3390/healthcare9101377
- Plouffe, R. A., Nazarov, A., Forchuk, C. A., Gargala, D., Deda, E., Le, T., Bourret-Gheysen, J., Jackson, B., Soares, V., Hosseiny, F., Smith, P., Roth, M., MacDougall, A. G., Marlborough, M., Jetly, R., Heber, A., Albuquerque, J., Lanius, R., Balderson, K., … Richardson, J. D. (2021). Impacts of morally distressing experiences on the mental health of Canadian health care workers during the COVID-19 pandemic. European Journal of Psychotraumatology, 12(1), 1984667. https://doi.org/10.1080/20008198.2021.1984667
- Poon, Y. R., Lin, Y. P., Griffiths, P., Yong, K. K., Seah, B., & Liaw, S. Y. (2022). A global overview of healthcare workers’ turnover intention amid COVID-19 pandemic: A systematic review with future directions. Human Resources for Health, 20(1), 70. https://doi.org/10.1186/s12960-022-00764-7
- Razak, F., Shin, S., Naylor, C. D., & Slutsky, A. S. (2022). Canada’s response to the initial 2 years of the COVID-19 pandemic: A comparison with peer countries. CMAJ: Canadian Medical Association Journal, 194(25), E870–E877. https://doi.org/10.1503/cmaj.220316
- Riedel, P. L., Kreh, A., Kulcar, V., Lieber, A., & Juen, B. (2022). A scoping review of moral stressors, moral distress and moral injury in healthcare workers during COVID-19. International Journal of Environmental Research and Public Health, 19(3), 1666. https://doi.org/10.3390/ijerph19031666
- Sheppard, K. N., Runk, B. G., Maduro, R. S., Fancher, M., Mayo, A. N., Wilmoth, D. D., Morgan, M. K., & Zimbro, K. S. (2022). Nursing moral distress and intent to leave employment during the COVID-19 pandemic. Journal of Nursing Care Quality, 37(1), 28–34. https://doi.org/10.1097/NCQ.0000000000000596
- Shoorideh, F. A., Ashktorab, T., Yaghmaei, F., & Alavi Majd, H. (2015). Relationship between ICU nurses’ moral distress with burnout and anticipated turnover. Nursing Ethics, 22(1), 64–76. https://doi.org/10.1177/0969733014534874
- Silverman, H., Wilson, T., Tisherman, S., Kheirbek, R., Mukherjee, T., Tabatabai, A., McQuillan, K., Hausladen, R., Davis-Gilbert, M., Cho, E., Bouchard, K., Dove, S., Landon, J., & Zimmer, M. (2022). Ethical decision-making climate, moral distress, and intention to leave among ICU professionals in a tertiary academic hospital center. BMC Medical Ethics, 23(1), 45. https://doi.org/10.1186/s12910-022-00775-y
- Spitzer, R. L., Kroenke, K., & Williams, J. B. W. (1999). The validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. JAMA: The Journal of the American Medical Association, 282(18), 1737–1744. https://doi.org/10.1001/jama.282.18.1737
- Spitzer, R. L., Kroenke, K., Williams, J. B. W., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. https://doi.org/10.1001/archinte.166.10.1092
- Statistics Canada. (2022). Experiences of health care workers during the COVID-19 pandemic, September to November 2021. The Daily, 1-8. https://www150.statcan.gc.ca/n1/en/daily-quotidien/220603/dq220603a-eng.pdf?st=UtVSZY7R.
- Varcoe, C., Pauly, B., Webster, G., & Storch, J. (2012). Moral distress: Tensions as springboards for action. HEC Forum, 24(1), 51–62. https://doi.org/10.1007/s10730-012-9180-2
- Wang, Z., Koenig, H. G., Tong, Y., Wen, J., Sui, M., Liu, H., Zaben, F. A., & Liu, G. (2022). Moral injury in Chinese health professionals during the COVID-19 pandemic. Psychological Trauma: Theory, Research, Practice and Policy, 14(2), 250–257. https://doi.org/10.1037/tra0001026.
- Weathers, F. W., Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schnurr, P. P. (2013). The PTSD Checklist for DSM-5 (PCL-5) – Standard [Measurement Instrument]. https://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp.
- Wilkinson, J. M. (1987). Moral distress in nursing practice: Experience and effect. Nursing Forum, 23(1), 16–29. doi:10.1111/j.1744-6198.1987.tb00794.x
- Woo, A., & Freeze, C. (2022, January 16). Health care system hit hard by staffing shortages amid COVID-19 surge. The Globe and Mail. https://www.theglobeandmail.com/canada/article-health-care-system-hit-hard-by-staffing-shortages-amid-covid-19-surge/.
- Wynia, M. K. (2007). Ethics and public health emergencies: Encouraging responsibility. The American Journal of Bioethics, 7(4), 1–4. https://doi.org/10.1080/15265160701307613
