ABSTRACT
Vaccination is a critical tool in the global response to the COVID-19 pandemic. Yet, COVID-19 vaccine hesitancy has not been well explored in parts of Nigeria. We assessed the predictors of acceptability of the COVID-19 vaccine and identified reasons for vaccine hesitancy among adults in urban Kano, northern Nigeria. Using a mixed-methods design, we administered structured questionnaires to a cross-section of adults (n = 446), complemented with 20 in-depth interviews. Binary logistic regression and the framework approach were used to analyze the data. About one-half (51.1%, n = 228) of the respondents were willing to take the COVID-19 vaccine. Vaccine acceptance was higher among older respondents (≥30 years) (adjusted Odds Ratio (aOR) = 1.76, 95% Confidence Interval (CI): 1.14–2.99 (≥30 vs. <30), higher-income earners (≥30,000 Naira) (aOR = 2.06, 95%CI:1.12–3.80, ≥30,000 vs. <30,000), and those with a history of a chronic medical disorder (aOR = 1.90, 95%CI:1.06–3.72). Vaccine acceptance was also higher in persons with high risk perception (aOR = 1.61, 95%CI:1.13–2.81, high vs. low), those who were unconcerned about vaccine safety (aOR = 1.71, 95%CI:1.13–3.55), and those who were not worried about efficacy (aOR = 2.02, 95%CI:1.14–4.11) and infertility-related rumors (aOR = 1.98, 95%CI:1.24–3.18). Themes revealed doubts about the existence of COVID-19, mistrust for authorities, and popular credence to rumors and conspiracy theories. In conclusion, COVID-19 vaccine acceptance was sub-optimal and influenced by respondent’s age, income, co-morbidities, risk perception, and concerns about vaccine safety, efficacy, and rumors. Context-specific, evidence-based risk communication strategies and trust-building measures could boost vaccine confidence in similar settings.
Introduction
Clusters of atypical pneumonia in Wuhan, China in 2019 escalated into a historic pandemic of coronavirus disease 2019 (COVID-19) attributed to novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).Citation1 By the end of May 2021, COVID-19 had claimed more than 3.5 million lives, with over 170 million cases globally.Citation2,Citation3 In sub-Saharan Africa, 3.5 million cases and >87,000 deaths were recorded, with >166,000 cases and >2000 deaths in Nigeria alone.Citation2,Citation4
This global public health crisis galvanized efforts to develop and approve vaccines at an unparalleled speed.Citation5 Many African countries, including Nigeria, received the first tranche of vaccines through the COVID-19 Vaccines Global Access (COVAX) initiative in early March 2021.Citation6 However, even before the COVID-19 pandemic, there was waning public support for vaccines, with vaccine hesitancy making the list of the top 10 global health threats.Citation7 This situation has been partly attributed to anti-vaccination campaigns on social media eroding public confidence.Citation8,Citation9 Vaccine hesitancy is a major hurdle toward attaining herd immunity in many countries, estimated at 67% for COVID-19.Citation10
A recent systematic review reported public acceptance of the COVID-19 vaccine to range from 23.6% in Kuwait to 97.0% in Ecuador.Citation11 In sub-Saharan Africa, intent to accept COVID-19 vaccines ranged from 59% in the Democratic Republic of Congo to 94% in Ethiopia and Niger.Citation12 Among the Nigerian public, COVID-19 vaccine acceptance ranges from 40.5% to 79.5%.Citation13–16 However, these figures likely mask sub-national differences and could be skewed in certain demographic groups.
Studies report that vaccine hesitancy was influenced by sociodemographics (sex, age, education, income, and occupation),Citation11,Citation17–19 health-related (risk perception, severity, knowing someone who had COVID-19, having co-morbidities), and vaccine-related (vaccine confidence, source of information about vaccines, perceived vaccine efficacy, safety, adverse effects, and protection duration) attributes.Citation12,Citation20,Citation21 Others identified political factors, including trust in government and public health authorities, confidence in vaccine developers, the vaccine approval process, national origin of vaccine, and endorsements as important factors influencing vaccine hesitancy.Citation22,Citation23
Other major reasons driving vaccine hesitancy include disinformation and anti-vaccine campaigns, especially, on social media, negative perceptions of the pharmaceutical industry, and concerns about the reliability or source of vaccines.Citation8,Citation24 Further, mistrust, negative stories, and a feeling of invincibility were reported.Citation12,Citation25 In Nigeria, most studies were conducted before the availability of the vaccine and were web-based. With the roll-out of COVID-19 vaccines, it is not clear if these parameters remain the same. Vaccine hesitancy has been a historically important issue in northern Nigeria, considering its conservative culture and previous challenges with vaccination programs.Citation26–29 Our findings could inform context-specific interventions to boost COVID-19 vaccine confidence.
This study determined COVID-19 vaccine acceptability, predictors, and reasons for vaccine hesitancy among adults in urban Kano, Northern Nigeria. We hypothesize higher vaccine hesitancy in view of historical antecedents related to polio vaccines and distrust of pharmaceutical companies as a fall out of a meningitis clinical trial in the mid-1990s.Citation30
Materials and methods
Study area and population
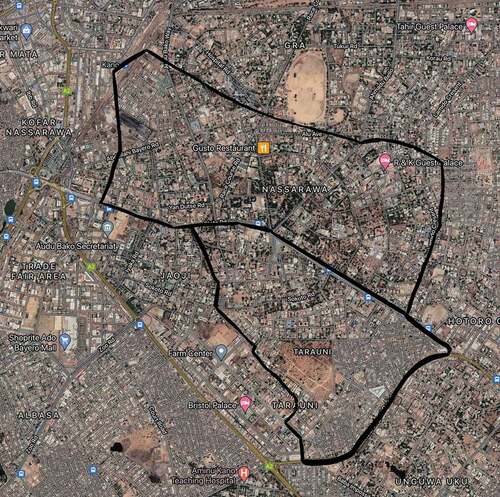
This study was carried out in March 2021 in Tarauni and Nassarawa local government areas of metropolitan Kano, in northern Nigeria (). The estimated population of Kano State is 13,076,892.Citation31 The inhabitants are mostly traders, entrepreneurs, civil servants, farmers, and homemakers of Hausa-Fulani ethnicity. Other major Nigerian tribes are, however, represented. The study population included adult men and women (≥ 18 years) resident in Kano for ≥ 6 months. We excluded persons who were not competent to provide consent and those who withheld consent.
Study design and sampling
The study was cross-sectional. Using Fisher’s formula,Citation32 the proportion of adult Nigerians who were willing to receive a potential COVID-19 vaccine from a previous study (58.2%),Citation33 95% confidence level, and 5% margin of error, we obtained a minimum sample size of 374. This sample size was increased by 10% to account for non-response, and finally rounded up to 450.
A multistage sampling method was used. In the first stage, half of the ten wards in each of the two local government areas were sampled using a simple ballot. In the second stage, one settlement was selected from each sampled ward using the same method. Numbers were then allocated to the selected settlements. After household enumeration, a sampling interval was determined. The systematic sampling method was used to select respondents in each settlement. The first household was selected by simple random sampling between 1 and the settlement’s sampling interval. Subsequent households were obtained by adding the sampling interval to the preceding household’s serial number. Finally, within each sampled household, eligible adults were consented after a detailed explanation about the study. When more than one eligible respondent was encountered in a household, one respondent was sampled through a simple ballot.
Measures and data collection
For the survey, we adapted validated structured survey questionnaires from previous studies.Citation34,Citation35 The first section documented socio-demographic characteristics, including age, sex, marital status, ethnicity, education, religion, occupation, number of children, and history of a chronic medical disorder. The second section assessed awareness of COVID-19 and self-perceived risk of COVID-19 using the question “How would you assess your chance of getting COVID-19? The responses were (‘high’ or ‘low’), whether or not the respondent was worried about getting COVID-19, perceived severity and whether the respondent knew someone who had COVID-19 and whether the respondents had had COVID-19 test. The third section elicited facilitators and barriers to vaccination, including whether the respondent was concerned about vaccine efficacy, safety, side effects, and rumors. Finally, the fourth section determined vaccine acceptability by asking ‘Are you willing to take the COVID-19 vaccine or not?.’ Response options included ‘I am very keen,’ ‘I am pretty positive,’ ‘not sure,’ ‘I am quite uneasy,’ and ‘I am against it.’ Those who chose “I am very keen’ or ‘I am pretty positive’ were considered as willing to receive the vaccine.
A 10% sample was used for pretest and assessment of the psychometric properties (re-validation and reliability) of the questionnaires in another location (Gwale local government area, Kano, Nigeria). All scales were reliable and sections consistent, with Cronbach’s alpha of ≥ 0.80.
To elucidate survey findings, a sub-sample of survey respondents were interviewed in-depth. Participants were sampled purposively, stratified by ward of residence (two wards each in Tarauni and Nassarawa local government areas), sex (two males, two females), age (two younger < 30 years, two older ≥ 30 years respondents), occupation, and acceptability of COVID-19 vaccine (two accepting, two vaccine hesitant). The qualitative interview guide had open-ended questions with probes for detailed descriptions. The guide explored the motivations for vaccine acceptance and the roots of vaccine hesitancy. All participants provided written or thumb-printed informed consent. Confidentiality in reporting qualitative findings was ensured by removing identifiers.
The study protocol was reviewed and approved by the AKTH research ethics committee. Using the local Hausa language, trained research assistants informed eligible persons in sampled households about the study objectives, eligibility criteria, sampling process, and the procedure. Participants were also informed that involvement was voluntary and that withholding of consent had no consequences. Literate men provided signed informed consent, while non-literate persons thumb-printed the consent form before the interviews. Interviews were conducted face-to-face, observing recommended COVID-19 precautions, in the respondents’ homes, away from family members. Completed questionnaires were checked and verified in the field by the supervisors. Questionnaires were double-entered independently by two data clerks into a password-protected database at Aminu Kano Teaching Hospital. Research staff were trained on establishing rapport, obtaining informed consent, protecting human research participants, and interview techniques.
Statistical analysis
Data were analyzed using SPSS Version 22 (IBM Corp., Armonk, NY). Mean and standard deviation were used to summarize numeric data. Frequencies and percentages were obtained for categorical variables. Pearson’s Chi-square or Fisher’s exact test as appropriate was used to assess the association between socio-demographic, health-related variables, risk perception, concerns about efficacy, safety, side effects, and rumors, and the primary outcome (willingness to be vaccinated against COVID-19).Citation36 Type I error was fixed at 5% for all tests. Binary logistic regression models were developed for willingness to be vaccinated. Independent variables with p < .10 at the bivariate level were included in the logistic regression model. A more liberal cutoff (p < .10) was suggested than the conventional cutoff for significance (p < .05) since the purpose is to identify potential predictor variables rather than to test a hypothesis. The more conservative or stringent p < .05 could exclude potential predictors due to confounding or effect modification.Citation37 Adjusted odds ratios (aORs) and their 95% confidence intervals (CIs) were used to measure the strength and direction of the effect of predictors. Hosmer-Lemeshow statistic and Omnibus tests were conducted to determine model fitness, with a Hosmer-Lemeshow chi-square yielding a p-value of > .05 considered a good fit.Citation38
Qualitative data analysis
Qualitative interviews were recorded and transcribed verbatim. Thematic analysis was performed based on the ‘Framework Approach’Citation39 and included familiarization through repeated reading, coding, theme generation, applying the codes to the transcripts, matrix formation, and interpretation. Findings from the two components of the mixed-methods study were integrated.Citation40
Results
Nearly all those approached (99.0%, n = 446) completed the interviews, with a respondents’ sex ratio of approximately 1:1. The majority of respondents were of Hausa ethnicity (86.6%, n = 386) and Muslim (98.4%, n = 439). The mean age (±standard deviation (SD) of respondents was 31.4 ± 10.59 years, and most (81.7%, n = 364) had at least secondary education. About one-tenth (11.4%, n = 51) had a history of a chronic medical disorder and 1 in 5 (20.9%, n = 93) had ever tested for COVID-19 ().
Table 1. Socio-demographic characteristics of adult respondents, Kano, Nigeria, 2021
COVID-19 risk perception, facilitators and barriers to vaccine uptake
Less than 1-in-5 (17.3%, n = 77) of the respondents considered themselves to be at high-risk for COVID-19 infection, and about 1-in-10 knew someone who had COVID-19. Most respondents viewed COVID-19 complications as serious (83.4%, n = 371). Themes from interviews confirmed familiarity of some participants with someone affected by COVID-19, while others were not:
Yes, I know someone who got infected with COVID-19 but he is late. He was my in-law, my wife’s uncle. I didn’t go near him when he was hospitalized, but, I took part in the burial and when I enquired from the cemetery security guard, he told me that daily they received at least 40 dead bodies. So that confirmed to us that this COVID-19 is real. 36 years, Male Trader
I have not seen anybody infected with COVID. But, I have heard so many stories about those who were affected by the disease from media houses and discussions among the public. I also heard about the mass burial of people who died every day from COVID-19 and were taken to Dandolo Cemetery in Kano city. 48 years, Male Businessman
Although majority of the respondents felt vaccination could reduce the risk of COVID-19 (70.3%, n = 313), over three-fourths were concerned about side effects, efficacy, and safety, while over half were worried about the rumors relating the COVID-19 vaccine to infertility and population control. Themes from in-depth interviews confirmed vaccine awareness, but low interest in getting vaccinated for a range of reasons:
Yes, I heard there is a vaccine for COVID-19 on the radio. The state Governor was also vaccinated on television. But, most people are saying they will not accept the vaccine. They don’t believe in the vaccine and the COVID-19 disease itself. They also think there are some foreign interests behind the vaccine. They scared us with a non-existent disease and produced a vaccine, but we doubt if COVID-19 disease exists. 28 years, Female Homemaker
Most respondents would consider taking the vaccine if provided adequate information (72.6%, n = 324), and if government officials and more people get vaccinated without consequences. Other facilitators of vaccine uptake include recommendations by health care professionals, traditional and religious leaders (). The existence of conspiracy theories and safety concerns were recurrent themes during in-depth interviews:
Yes, I heard about the vaccine. It is a good development and I wish people would receive it in good faith and the Almighty will protect them. I also told people that this vaccine is very safe and authentic. However, some people are saying even if they are offered one million Naira, they will not take the vaccine. I told them that this vaccine was developed in Europe and I believe 100% in the quality of products from Europe compared to our local products. Though they are not Muslim, they do not intend any harm on us since they are also using it. If they wish to harm us, there are easier ways. However, recent reports linking the vaccine to blood clots and discontinuation in some western countries is a major setback. 36 years, Male community leader
Table 2. COVID-19 risk perception and vaccination willingness (N = 446), Kano, Nigeria
Willingness to receive a COVID-19 vaccine
About one-half (51.1%, n = 228) of the respondents were willing to take the COVID-19 vaccine, and 61.9% (n = 276) would encourage family members and friends to take the vaccine. This was corroborated by themes from in-depth interviews, with some eagerly waiting to receive the vaccine, while others were ambivalent, and some rejected the vaccine outrightly:
Yes, some people are very eager to get vaccinated. Because they don’t want another lockdown like what happened last year. If this vaccine is the lasting solution to COVID-19, they are ready to take it once and for all. 45 years Female Homemaker
No! People are not eager to get vaccinated with the COVID-19 vaccine. They are saying it is not safe nor is it effective. They even instructed their children to reject it when offered at school. 32 years, Female, Petty trader
Some are willing and ready to receive the vaccine. But, others are saying they won’t take it. I think most of the people when sensitized would be willing to receive the vaccine. 52 years, Female Homemaker
COVID-19 vaccine acceptability
Bivariate analyses showed significant association between COVID-19 vaccine acceptability and age, marital status, occupation, income, history of chronic medical disorders and self-perceived COVID-19 risk. Similarly, there was a significant association with concerns about COVID-19 vaccine safety, efficacy, side effects, and rumors (p < .05). However, at the multivariate level, only respondent’s age, income, history of a chronic medical disorder, risk perception, concerns about safety, efficacy, and rumors remained independent predictors of vaccine acceptability.
Respondents who were in the 4th decade of life had 76% increased likelihood of accepting the COVID-19 vaccine compared to younger respondents (adjusted odds ratio, aOR = 1.76, 95% confidence interval CI: 1.14–2.99). Those who earned more than the Nigeria national minimum wage (>30,000 Naira) monthly had a two-fold increased likelihood (aOR = 2.06, 95% CI, 1.12–3.80) to accept the COVID-19 vaccine relative to those who earned less. Likewise, those with a history of a chronic medical disorder had almost two-fold increased odds (aOR = 1.90, 95% CI, 1.06–3.72) of accepting the vaccine. Persons who perceived themselves to be at higher risk of COVID-19 were 61% (aOR = 1.61, 95% CI, 1.13–2.81) more likely to take the vaccine. Further, those who were not worried about vaccine safety, efficacy and infertility-related rumors had 71% (aOR = 1.71, 95% CI, 1.13–3.55), two-fold (aOR = 2.02, 95% CI, 1.14–4.11) and two-fold (aOR = 1.98, 95% CI, 1.24–3.18) increased odds of taking the vaccine, respectively ().
Table 3. Logistic regression model for predictors of acceptability of COVID-19 vaccination among adults, Kano, Nigeria (N = 446)
Discussion
We assessed COVID-19 vaccine acceptability, predictors, and reasons for vaccine hesitancy among adults in urban Kano, northern Nigeria. We found that about one-half of the respondents were willing to take the COVID-19 vaccine. However, 3-in-4 respondents were worried about vaccine side effects, efficacy, and safety, while more than one-half were concerned about infertility-related rumors. Themes revealed doubts about the existence of COVID-19, mistrust in authorities, and reliance on rumors and conspiracy theories. Acceptability of the COVID-19 vaccine was predicted by respondent’s age, income, history of a chronic medical disorder, risk perception, and concerns about safety, efficacy, and infertility-related rumors.
The COVID-19 vaccine acceptance (51.1%) was lower than in parts of Nigeria (south-south, southwest, northwest) (59.1%–79.5%),Citation13–16,Citation41,Citation42 but similar to others (southeast) (40.5%–50.0%).Citation16,Citation22 Our figure was also low compared to average numbers from Nigeria (76%), Africa (79%)Citation12 and Asia (91.3%-94.3%).Citation11 The figures reported from Europe (53.7%- 58.9%)Citation11 and the US (56.9%-67.0%)Citation9,Citation18,Citation43 were also higher. Apart from variations in study timing, population, and methods, these differences could be accounted for by disparities in COVID-19 burden, health literacy, risk perception, perceived COVID-19 severity, rumors, and intensity of anti-vaccination campaigns.Citation17 For instance, compared to sub-Saharan Africa, the burden of COVID-19 is higher in Asia, the US, and Europe.Citation44,Citation45 Similarly, less than one-fifth (17.3%) of our respondents considered themselves to be at high risk for COVID-19, compared to 41% and 46% in Ethiopia and South Africa, respectively.Citation12 Further, while about 1-in-10 (12.3%) of our respondents knew someone who had COVID-19, the corresponding proportions in Ethiopia and South Africa were 23% and 42%.Citation12 These variations could be important when selecting context-specific messaging and risk communication strategies.
The reasons for vaccine hesitancy in our sample were similar to those reported in other parts of Nigeria and Africa.Citation12,Citation22 However, the proportion of respondents who expressed concern about vaccine safety, efficacy, and infertility-related rumors in our sample were higher than in other parts of Nigeria and Africa.Citation12 For instance, while more than three-quarters (79%) of our respondents were concerned about safety, the proportion in Ethiopia was less than 1 in 5 (12%).Citation12 Similarly, across Africa, 20% of respondents doubted the efficacy of COVID-19 vaccines. Likewise, a lower proportion of respondents in Africa (25–49%) were disturbed by rumors and conspiracy theories compared to our respondents (58.3%).Citation12 However, themes related to doubts about the existence of COVID-19, its perception as a deliberate invention, and mistrust were also reported in parts of Nigeria,Citation22 Africa,Citation12, and elsewhere.Citation46 The high proportion of respondents expressing concerns about safety, efficacy, and infertility-related rumors indicate the potential gains of strategies to address these concerns and rumors.
The sociodemographic variables sex, ethnicity, religion and education were not significantly associated with COVID-19 vaccine acceptance at bivariate level, hence their exclusion from the logistic regression model. Our study confirmed the skepticism reported among young people in other studies.Citation12,Citation47 This finding could be related to the rebellious nature of young adults, perceived low risk, and a feeling of invincibility. The influence of income on vaccine acceptance was not surprising, as the effects of socioeconomic status on health behavior are well known.Citation48,Citation49 Apart from the ability to pay, higher-income earners are likely to be more educated, which could influence their outlook and attitude toward community well-being. Similarly, persons with co-morbidities are likely to have had repeated contacts with the health system, thereby enhancing health literacy and risk perception.Citation50,Citation51 In contrast, concerns about vaccine safety and efficacy could discourage vaccine uptake. This situation was the basis for halting the COVID-19 vaccine roll-out in some countries.Citation52,Citation53 Finally, the inhibitory effects of rumors, mistrust, and conspiracy theories on vaccine acceptance are expected,Citation25 pre-dated the COVID-19 pandemic,Citation26–29 and led to the interruption of polio campaigns in northern Nigeria.Citation26,Citation27 These effects underscore the importance of proactive steps by health authorities to understand and address community concerns before vaccine roll-out.
Our findings suggest the need for a multi-pronged strategy to improve vaccine acceptance. First, risk communication should be employed to fill information gaps by adapting evidence to the local context. Second, the revered traditional and religious leaders should be considered strategic partners for community engagement. Third, specific responses should counter rumors and dispel conspiracy theories using conventional and social media.
The strengths of this study include the mixed-methods design, face-to-face interviews, and the conduct of the study just as the COVID-19 vaccine rollout was occurring in Nigeria. The qualitative component added participants’ voices and contextual depth to the survey responses. A limitation, however, was the conduct of the study in one urban location in northern Nigeria, restricting the potential generalizability of findings.
Conclusions
We found sub-optimal COVID-19 vaccine acceptance among adults in Kano metropolis, in northern Nigeria. Acceptability of the COVID-19 vaccine was influenced by co-morbidities, respondent’s income, risk perception, concern about vaccine safety, efficacy, and infertility-related rumors. We recommend community engagement through revered traditional and religious leaders, the use of context-specific, evidence-based risk communication strategies, and trust-building measures to boost confidence and improve COVID-19 vaccine uptake in similar settings.
Authors’ contributions
ZI, HA, AK, TA FT, HS and MA contributed to conception, design, planning and interpretation of the results. AU and RG contributed to study interpretation. All authors contributed to the manuscript draft and editing for intellectual content. All authors critically reviewed the manuscript and approve the final version.
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
Acknowledgments
We thank the participants in this study.
References
- Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91(1):157–60. doi:10.23750/abm.v91i1.9397.
- World Health Organization (WHO). [accessed 2021 May 25]. https://covid19.who.int .
- Johns Hopkins University. [accessed 2021 May 25]. https://coronavirus.jhu.edu .
- Nigeria Centre for Disease Control (NCDC). [accessed 2021 May 25]. https://covid19.ncdc.gov.ng .
- Lurie N, Sharfstein JM, Goodman JL. The development of COVID-19 vaccines: safeguards needed. JAMA. 2020;324(5):439–40. doi:10.1001/jama.2020.12461.
- Nachega JB, Sam-Agudu NA, Masekela R, van der Zalm MM, Nsanzimana S, Condo J, Ntoumi F, Rabie H, Kruger M, Wiysonge CS, et al. Addressing challenges to rolling out COVID-19 vaccines in African countries. Lancet Glob Health. 2021;9(6):e746–8. doi:10.1016/S2214-109X(21)00097-8.
- Editorial. Vaccine hesitancy: a generation at risk. Lancet Child Adolesc Health. 2019;3(5):281. doi:10.1016/S2352-4642(19)30092-6.
- Wilson SL, Wiysonge C. Social media and vaccine hesitancy. BMJ Global Health. 2020;5:e004206. doi:10.1136/bmjgh-2020-004206.
- Puri N, Coomes EA, Haghbayan H, Gunaratne K. Social media and vaccine hesitancy: new updates for the era of COVID-19 and globalized infectious diseases. Hum Vaccin Immunother. 2020;16(11):2586–93. doi:10.1080/21645515.2020.1780846.
- Randolph HE, Barreiro LB. Herd Immunity: understanding COVID-19. Immunity. 2020;52(5):737–41. doi:10.1016/j.immuni.2020.04.012.
- Sallam M. COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines (Basel). 2021;9(2):160. doi:10.3390/vaccines9020160.
- Samarasekera U. Feelings towards COVID-19 vaccination in Africa. Lancet. 2021;21:324. doi:10.1016/S1473-3099(21)00082-7.
- Tobin EA, Okonofua M, Azeke A, Ajekweneh V, Akpede G. Willingness to accept a covid-19 vaccine in Nigeria: a population-based cross-sectional study. Cent Afr J Public Health. 2021;7(2):53–60. doi:10.11648/j.cajph.20210702.12.
- Adebisi YA, Alaran AJ, Bolarinwa OA, Akande-Sholabi W, Lucero-Prisno III DE. When it is available, will we take it? Social media users’ perception of hypothetical COVID-19 vaccine in Nigeria. Pan Afr Med J. 2021;38(230). doi:10.11604/pamj.2021.38.230.27325.
- Ilesanmi O, Afolabi A, Uchendu O. The prospective COVID-19 vaccine: willingness to pay and perception of community members in Ibadan, Nigeria. PeerJ. 2021;9:e11153. doi:10.7717/peerj.11153.
- Eniade OD, Olarinmoye A, Otovwe A, Akintunde FE, Okedare OO, Aniyeloye AO. Willingness to accept COVID-19 vaccine and its determinants among Nigeria citizens: a web-based cross-sectional study. J Adv Med Med Res. 2021;33(8):13–22. doi:10.9734/jammr/2021/v33i830881.
- Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, Kimball S, El-Mohandes A. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27(2):225–28. doi:10.1038/s41591-020-1124-9.
- Khubchandani J, Sharma S, Price JH, Wiblishauser MJ, Sharma M, Webb FJ. COVID-19 vaccination hesitancy in the United States: a rapid national assessment. J Community Health. 2021;46(2):270–77. doi:10.1007/s10900-020-00958-x.
- Murphy J, Vallières F, Bentall RP, Shevlin M, McBride O, Hartman TK, McKay R, Bennett K, Mason L, Gibson-Miller J, et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat Commun. 2021;12(1):1–15. doi:10.1038/s41467-020-20226-9.
- MacDonald NE. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–64. doi:10.1016/j.vaccine.2015.04.036.
- Murphy J, Vallières F, Bentall RP, Shevlin M, McBride O, Hartman TK, McKay R, Bennett K, Mason L, Gibson-Miller J, et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat Commun. 2021;12(1):29. doi:10.1038/s41467-020-20226-9.
- Tobin EA, Okonofua M, Azeke A, Ajekweneh V, Akpede G. Willingness to accept a COVID-19 vaccine in Nigeria: a population-based cross-sectional study. J Med Res. 2021;5:1–15.
- Kreps S, Prasad S, Brownstein JS, Hswen Y, Garibaldi BT, Zhang B, Kriner DL. Factors associated with US adults’ likelihood of accepting COVID-19 vaccination. JAMA Netw Open. 2020;3(10):e2025594. doi:10.1001/jamanetworkopen.2020.25594.
- Germani F, Biller-Andorno N. The anti-vaccination infodemic on social media: a behavioral analysis. PLoS ONE. 2021;16(3):e0247642. doi:10.1371/journal.pone.0247642.
- Daly M, Jones A, Robinson E. Public trust and willingness to vaccinate against COVID-19 in the US from October 14, 2020, to March 29, 2021. JAMA. 2021 May 24;325(23):2397. doi:10.1001/jama.2021.8246.
- Kapp C. Nigerian states again boycott polio-vaccination drive. Muslim officials have rejected assurances that the polio vaccine is safe–leaving Africa on the brink of reinfection. Lancet. 2004;363(9410):709. doi:10.1016/s0140-6736(04)15665-1.
- Jegede AS. What led to the Nigerian boycott of the polio vaccination campaign? PLoS Med. 2007;4(3):e73. doi:10.1371/journal.pmed.0040073.
- Clements CJ, Greenough P, Shull D. How vaccine safety can become political–the example of polio in Nigeria. Curr Drug Saf. 2006;1(1):117–19. doi:10.2174/157488606775252575.
- Ghinai I, Willott C, Dadari I, Larson HJ. Listening to the rumours: what the northern Nigeria polio vaccine boycott can tell us ten years on. Glob Public Health. 2013;8(10):1138–50. doi:10.1080/17441692.2013.859720.
- Wise J. Pfizer accused of testing new drug without ethical approval. BMJ. 2001;322(7280):194. doi:10.1136/bmj.322.7280.194.
- National Bureau of Statistics. Demographic statistics bulletin 2017. 2018 May [accessed 2021 Aug 2]:7–8. https://nigerianstat.gov.ng.
- Lwanga SK, Lemeshow S. Sample size determination in health studies: a practical manual. Geneva, Switzerland: World Health Organization; 1991. 29–32.
- Olomofe CO, Soyemi VK, Udomah BF, Owolabi AO, Ajumuka EE, Igbokwe CM, Ashaolu UO, Adeyemi AO, Aremu-Kasumu YB, Dada OF, et al. Predictors of uptake of a potential Covid-19 vaccine among Nigerian adults. J Vaccines Vaccin. 2021;12:442.
- Freeman D, Loe BS, Chadwick A. COVID-19 vaccine hesitancy in the UK: the Oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II. Psychol Med. 2021:1–15. doi:10.1017/S0033291720005188.
- Schwarzinger M, Watson V, Arwidson P, Alla F, Luchini S. COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Public Health. 2021;6(4):e210–e221. doi:10.1016/S2468-2667(21)00012-8.
- Kim H. Statistical notes for clinical researchers: chi-squared test and Fisher’s exact test. Resor Dent Endod. 2017;42(2):152–55. doi:10.5395/rde.2017.42.2.152.
- Ranganathan P, Pramesh CS, Aggarwal R. Common pitfalls in statistical analysis: logistic regression. Perspect Clin Res. 2017 Jul-Sep;8(3):148–51. doi:10.4103/picr.PICR_87_17.
- Hosmer DW, Lemeshow S. Applied logistic regression. New York (NY): Wiley; 2013.
- Pope C, Ziebland S, Mays N. Qualitative research in health care. Analyzing qualitative data. BMJ. 2000;320(7227):114–16. doi:10.1136/bmj.320.7227.114.
- Farmer T, Robinson K, Elliott SJ, John ED. Developing and implementing a triangulation protocol for qualitative health research. Qual Health Res. 2006;16:377. doi:10.1177/1049732305285708.
- Akinyemi PA, Fajobi O, Owoade IA, Elugbaju OT, Wuraola FO. Community perception and determinants of willingness to uptake COVID-19 vaccines among residents of Osun State, South-West Nigeria. Int J Community Med Public Health. 2021;8(4):1551–57. doi:10.18203/2394-6040.ijcmph20211202.
- Habib MA, Dayyab FM, Iliyasu G, Habib AG. Knowledge, attitude and practice survey of COVID-19 pandemic in Northern Nigeria. PLoS One. 2021;16(1):e0245176. doi:10.1371/journal.pone.0245176.
- Malik AA, McFadden SM, Elharake J, Omer SB. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020;26:100495. doi:10.1016/j.eclinm.2020.100495.
- Rice BL, Annapragada A, Baker RE, Bruijning M, Dotse-Gborgbortsi W, Mensah K, Miller IF, Motaze NV, Raherinandrasana A, Rajeev M, et al. Variation in SARS-CoV-2 outbreaks across sub-Saharan Africa. Nat Med. 2021;27:447–53. doi:10.1038/s41591-021-01234-8.
- Clark A, Jit M, Warren-Gash C, Guthrie B, Wang HHX, Mercer SW, Sanderson C, McKee M, Troeger C, Ong KL, et al. Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: a modelling study. Lancet Glob Health. 2020 Aug8;8:e1003–e1017. doi:10.1016/S2214-109X(20)30264-3.
- Al-Qerem WA, Jarab AS. COVID-19 vaccination acceptance and its associated factors among a middle eastern population. Front Public Health. 2021;9:632914. doi:10.3389/fpubh.2021.632914.
- Enitan SS, Oyekale AO , Akele RY , Olawuyi KA, Olabisi EO, Nwankiti AJ, Adejumo EN , Enitan CB. Assessment of knowledge, perception and readiness of Nigerians to participate in the COVID-19 vaccine trial. Int J Vaccine Immunizat. 2020;4(1). doi:10.16966/2470-9948.123.
- Alobaidi S. Predictors of intent to receive the COVID-19 vaccination among the population in the Kingdom of Saudi Arabia: a survey study. J Multidiscip Healthc. 2021;14:1119–28. doi:10.2147/JMDH.S306654.
- Viswanath K, Bekalu M, Dhawan D, Pinnamaneni R, Lang J, McLoud R. Individual and social determinants of COVID-19 vaccine uptake. BMC Public Health. 2021;21:818. doi:10.1186/s12889-021-10862-1.
- Choi WS, Cheong HJ. COVID-19 vaccination for people with comorbidities. Infect Chemother. 2021;53(1):155–58. doi:10.3947/ic.2021.0302.
- Wiedemann PM, Schütz H. The precautionary principle and risk perception: experimental studies in the EMF area. Env Health Perspect. 2005;113:402–05. doi:10.1289/ehp.7538.
- Madhi SA, Baillie V, Cutland CL, Voysey M, Koen AL, Fairlie L, Padayachee SD, Dheda K, Barnabas SL, Bhorat QE, et al. Efficacy of the ChAdOx1 nCoV-19 Covid-19 vaccine against the B.1.351 variant. N Engl J Med. 2021;384(20):1885–98. doi:10.1056/NEJMoa2102214.
- Irfan N, Chagla Z. In South Africa, a 2-dose Oxford/AZ vaccine did not prevent mild to moderate COVID-19 (cases mainly B.1.351 variant). Ann Intern Med. 2021;174(5):JC50. doi:10.7326/ACPJ202105180-050.