ABSTRACT
Coronavirus disease 2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 and presents with pneumonia as the most frequent and serious manifestation. COVID-19 vaccination is an important and urgent interest globally due to COVID-19’s rapid spread and high rates of mortality and morbidity. Vestibular neuritis (VN) is an acute vestibular syndrome that causes acute and spontaneous vertigo due to unilateral vestibular deafferentiation, leading to nausea or vomiting and unsteadiness that can last from days to weeks. Reactivation of latent type 1 herpes simplex virus, autoimmune disorders, and microvascular ischemia are hypothesized to be etiologies. Herein, the case of a 54-year-old man who developed VN within three days after COVID-19 vaccination is presented. There have been no reports of VN after vaccination for COVID-19 or other viral diseases. Although the association between VN and COVID-19 vaccination remains unclear, clinicians should be aware that VN may occur as an adverse event of COVID-19 vaccination.
Introduction
Coronavirus disease 2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and pneumonia is the most frequent and serious manifestation.Citation1–3
In this situation, COVID-19 vaccination is an important and urgent interest worldwide. The United States Food and Drug Administration (FDA) issued emergency use authorizations for Pfizer-BioNTech and Moderna mRNA-based COVID-19 vaccines in December 2020, and for the Janssen recombinant adenovirus-vector COVID-19 vaccine in February 2021.Citation4,Citation5 Pfizer-BioNTech COVID-19 vaccine subsequently received full FDA approval in August 2021. COVID-19 vaccination has been expedited in many countries. More than 6 billion vaccine doses had been administered by early October 2021.
Several serious adverse events have been reported, including Guillan-Barré syndrome and thrombosis with thrombocytopenia syndrome after Janssen COVID-19 vaccination, and myocarditis after Pfizer-BioNTech and Moderna COVID-19 vaccination.Citation4 Sudden hearing loss after COVID-19 vaccination has also been reported, although the association remains unclear.Citation5,Citation6
Vestibular neuritis (VN) is an acute vestibular syndrome leading to acute and spontaneous vertigo due to unilateral vestibular deafferentiation, with nausea or vomiting and unsteadiness lasting from days to weeks.Citation2,Citation7,Citation8 VN has not been reported previously as an adverse event of COVID-19 vaccination. Herein, the case of a 54-year-old man who developed VN within three days after COVID-19 vaccination is presented.
Case presentation
A 54-year-old man visited the emergency department for acute vertigo that occurred one day prior. He had hypertension that was well controlled with medication. He had received his first Pfizer-BioNTech COVID-19 vaccine two days before vertigo onset. He had no symptoms of hearing loss and no history of recent upper respiratory infection. There were no neurologic signs or symptoms suspicious of central vertigo. On physical examination, both ear drums were intact and right horizontal-torsional spontaneous nystagmus was observed. He was admitted for conservative care due to intolerable vertigo symptoms.
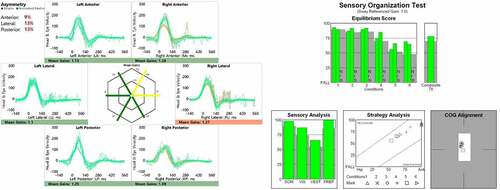
Three days after onset, caloric test, video head impulse test, cervical vestibular evoked myogenic potential, and dynamic posturography were performed. Canal paresis on the caloric test was within normal range and there were responses on both sides in cervical vestibular evoked myogenic potential. However, a decrease in the vestibulo-ocular reflex gain without catch-up saccade was observed in the left lateral semicircular canal on video head impulse test, and the composite score was low on dynamic posturography (). Thus, left superior VN was diagnosed. After five days of hospitalization with vestibular suppressants, vertigo symptoms improved and spontaneous nystagmus disappeared; thus, the patient was discharged after instruction on vestibular rehabilitation.
Figure 1. Three days after onset, there was a decrease in vestibulo-ocular reflex gain without catch-up saccade in the left lateral semicircular canal on video head impulse test (a), and a low composite score on dynamic posturography (b).
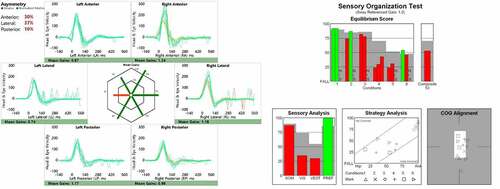
Two weeks after onset, vertigo symptoms had improved further but there were residual mild symptoms. The patient was instructed to continue vestibular rehabilitation. Six weeks after onset, the patient had no symptoms of vertigo. Vestibulo-ocular reflex gain had recovered to normal without catch-up saccade in the left lateral semicircular canal on video head impulse test, and composite score on dynamic posturography had also recovered to normal ().
Discussion
Audiovestibular symptoms in COVID-19 are rare, and long-term audiovestibular consequences have not been reported.Citation9 In a study comparing the number of admissions for VN in five hospitals in France before and during COVID-19, there was no correlation between VN and COVID-19.Citation10 However, COVID-19-induced vestibular symptoms seem to be more common than once thought.Citation11 Several cases of VN in patients with COVID-19 have been reported.Citation1–3,Citation8,Citation9,Citation11,Citation12
Although VN may be preceded by or concurrent with viral illnesses, serological evidence of systemic viral infection remains sparse.Citation7,Citation10 Reactivation of latent type 1 herpes simplex virus has been suggested as the cause.Citation2,Citation3,Citation7,Citation8,Citation12 Autoimmune and microvascular ischemia are thought to be other etiologies.Citation3,Citation7,Citation10,Citation12 However, VN in patients with COVID-19 or within three days after COVID-19 vaccination might have another pathophysiological mechanism.
Viral or post-viral inflammation could be the mechanism of VN in patients with COVID-19.Citation2,Citation13 It has been hypothesized that SARS-CoV-2 affects the central nervous system through hematogenous or neuronal retrograde dissemination.Citation2,Citation3 The effect of SARS-CoV-2 on the central nervous system could reflect direct infection or related vascular damage due to vasculitis or vasculopathy. COVID-19 can induce hypercoagulability leading to vascular compromise of neurons.Citation11 Cell entry of SARS-CoV-2 depends on angiotensin-converting enzyme 2 receptors and transmembrane protease serine 2. These receptors in the epithelium could function as a gate for SARS-CoV-2 to enter the vestibule resulting in VN. Ischemia of the vasa nervorum and demyelination induced by inflammation could be another cause of VN. In addition, triggering for reactivation of type 1 herpes simplex virus by SARS CoV-2 could also be an etiology.Citation8
In the study of otologic symptoms after COVID-19 vaccination, sudden sensorineural hearing loss (SSNHL) increased from 2019 to 2021, indicating the possibility of an association between COVID-19 or COVID-19 vaccination and SSNHL; however, the causality of this relationship remains unsupported.Citation5 The etiology of VN is similar to SSNHL. Thus, the possibility of COVID-19 vaccination-induced VN should be considered.
Treatment of VN includes symptomatic care with vestibular suppressants during the acute phase, and ongoing vestibular rehabilitation.Citation1,Citation2,Citation7,Citation11 In the present patient, vertigo symptoms improved gradually and the initial decrease in vestibular function recovered within six weeks. The efficacy of corticosteroids remains controversial.Citation7 However, corticosteroids could be used in severe cases.Citation1,Citation2,Citation11,Citation13 The effects of systemic steroids after vaccination have not been investigated. Thus, steroids should be used carefully in patients after vaccination because immediate systemic steroid use could affect antibody formation in response to vaccination.
In this case, VN occurred within three days after COVID-19 vaccination. There have been no reports of VN after vaccination for COVID-19 or other viral diseases. Although the association between VN and COVID-19 vaccination remains unclear, clinicians should be aware that VN may occur as an adverse event of COVID-19 vaccination.
Ethical approval
The Institutional Review Board of the National Health Insurance Service Ilsan Hospital exempted the review of this study (NHIMC 2021-10-018).
Acknowledgments
The author thanks the patient for contribution to the case report.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Malayala SV, Raza A. A case of COVID-19-induced vestibular neuritis. Cureus. 2020;12(6):e8918. doi:10.7759/cureus.8918. PMID: 32760619; PMCID: PMC7392187.
- Vanaparthy R, Malayala SV, Balla M. COVID-19-induced vestibular neuritis, hemi-facial spasms and Raynaud’s phenomenon: a case report. Cureus. 2020;12(11):e11752. doi:10.7759/cureus.11752. PMID: 33403182.
- Giannantonio S, Scorpecci A, Montemurri B, Marsella P. Case of COVID-19-induced vestibular neuritis in a child. BMJ Case Rep. 2021;14(6):e242978. doi:10.1136/bcr-2021-242978. PMID: 34078625.
- Rosenblum HG, Hadler SC, Moulia D, Shimabukuro TT, Su JR, Tepper NK, Ess KC, Woo EJ, Mba-Jonas A, Alimchandani M, et al. Use of COVID-19 vaccines after reports of adverse events among adult recipients of Janssen (Johnson & Johnson) and mRNA COVID-19 vaccines (Pfizer-BioNTech and Moderna): update from the advisory committee on immunization practices - United States, July 2021. MMWR Morb Mortal Wkly Rep. 2021;70(32):1094–99. doi:10.15585/mmwr.mm7032e4. PMID: 34383735.
- Wichova H, Miller ME, Derebery MJ. Otologic manifestations after COVID-19 vaccination: the house ear clinic experience. Otol Neurotol. 2021;42(9):e1213–e1218. doi:10.1097/MAO.0000000000003275. PMID: 34267103.
- Formeister EJ, Chien W, Agrawal Y, Carey JP, Stewart CM, Sun DQ. Preliminary analysis of association between COVID-19 vaccination and sudden hearing loss using US centers for disease control and prevention vaccine adverse events reporting system data. JAMA Otolaryngol Head Neck Surg. 2021;147(7):674–76. doi:10.1001/jamaoto.2021.0869. PMID: 34014263.
- Jeong SH, Kim HJ, Kim JS. Vestibular neuritis. Semin Neurol. 2013;33(3):185–94. doi:10.1055/s-0033-1354598. PMID: 24057821.
- Mat Q, Noël A, Loiselet L, Tainmont S, Chiesa-Estomba CM, Lechien JR, Duterme JP. Vestibular neuritis as clinical presentation of COVID-19. Ear Nose Throat J. 2021 Feb 11:145561321995021. Epub ahead of print. doi:10.1177/0145561321995021. PMID: 33570425.
- Babu TA, Sarkar MK, Sharmila V. COVID-19 vestibular neuritis (CVN) in a healthcare worker: a rare complication of COVID-19 infection. J R Coll Physicians Edinb. 2021;51(2):199–207. doi:10.4997/JRCPE.2021.224. PMID: 34131685.
- Charpiot A, Hautefort C, Jourdaine C, Lavieille JP, Levy D, Poillon G, Tighilet B, Weckel A, Chabbert C. Study of the comorbidity between cases of acute peripheral vestibulopathies and COVID-19. Otol Neurotol. 2021;42(8):e1072–e1076. doi:10.1097/MAO.0000000000003216. PMID: 34238895.
- Malayala SV, Mohan G, Vasireddy D, Atluri P. A case series of vestibular symptoms in positive or suspected COVID-19 patients. Infez Med. 2021;29(1):117–22. PMID: 33664181.
- Halalau A, Halalau M, Carpenter C, Abbas AE, Sims M. Vestibular neuritis caused by severe acute respiratory syndrome coronavirus 2 infection diagnosed by serology: case report. SAGE Open Med Case Rep. 2021;9:2050313X211013261. doi:10.1177/2050313X211013261. PMID: 34035914.
- Motawea KR, Monib FA. New onset vertigo after COVID-19 infection. A case report. Indian J Otolaryngol Head Neck Surg. 2021 July 4:1–3. Epub ahead of print. doi:10.1007/s12070-021-02715-5. PMID: 34249665.