Abstract
We report the case of a patient with Lymphocytic thrombophilic arteritis (LTA) with a history of 67 years. This is a relatively rare disease with no recognised guidelines for diagnosis and treatment. The long medical history from birth of this patient and the lack of positive progression may provide some new ideas for the treatment of this disease.
Clinical Information
One month ago, a 67-year-old female patient presented to our dermatology clinic with a strange disease. The patient had a purpura-like rash that had gradually appeared all over her body since birth. During these 67 years, the patient has been seen by several hospitals but has never received a clear diagnosis. At the time of her visit to our dermatology department, the patient reported no signs of discomfort.
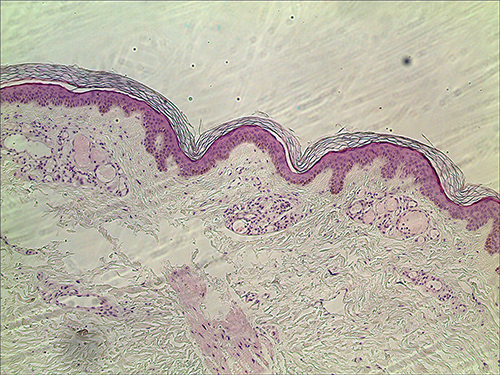
A detailed physical examination was carried out. A purpura-like rash consisting of fused purple patches the size of corn grains was seen all over the body, most frequently on the bilateral breasts and extremities, as shown in and . These rashes are non-blanchable, accompanied by no elevated skin temperature. Laboratory tests showed no abnormalities in blood count or coagulation. A histopathological examination of the skin was performed to confirm the diagnosis of the disease. Microscopic examination revealed mild hyperkeratosis of the epidermis and deposits of fibrin-like material in the capillary walls and lumen of the dermis, as shown in . Localised hyaline thrombosis was present. There is a moderate perivascular infiltration of lymphocytes and histiocytes. No obvious erythrocyte extravasation was seen. Based on the clinical presentation and histopathological examination of the skin, the patient is basically consistent with lymphocytic thrombophilic arteritis.
Discussion
Lymphocytic thrombophilic arteritis (LTA) is a newer view of the disease from a histological point of view, and is a lymphocyte-mediated vasculitis that usually occurs at the end of neutrophil-mediated vasculitis, also known as macular lymphocytic arteritis (MTA).Citation1 This disease belongs to the vascular group of lesions but has not yet been included in the Dermatological Addendum to the 2012 International Chapel Hill Consensus Conference Nomenclature of Vasculitides.Citation2 It is clinically characterised by asymptomatic plaques in the extremities. There is still much debate as to whether lymphocytic thrombophilic vasculitis and cutaneous polyarteritis nodosa (c-PAN) share the same clinicopathological disease spectrum. Pathologically, both diseases present with lymphocytic infiltration of the arterial wall. The specific typing of the infiltrating cells (lymphocytes or neutrophils) does not appear to have a significant impact on disease progression.Citation3 The number of cases reported so far is limited. The treatment options among them vary and are mostly symptomatic. Previous treatment regimens applied to patients with LTA have been mainly topical drug therapy and oral steroid hormones, anticoagulants and aminophene. In one case, narrow-spectrum UVB was used to help homogenise skin pigmentation in a patient with MLA.Citation4 Studies have shown that anticoagulants have no significant therapeutic effect on MTA. MTA is thought to be an inert middle artery vasculitis with no clear trend of progression. The aggressive systemic treatment is not advocated.Citation1
For the patient in this case, the presence of the disease, while not causing her physical pain or discomfort, severely affected her psychological well-being and became a perennial psychological burden. In the real world, it is worth further considering whether to go for an aggressive treatment plan and which medication to use for this type of dermatological condition without conscious symptoms.
Conclusion
The patient has presumably had LTA since birth without progression to a more insidious form of vasculitis, underscoring the benign nature of LTA. It is quite possible that the best management for this patient is not overly aggressive systemic therapy. We need to carefully assess the patient’s the concrete situation and weigh the risks and benefits of steroidal or non-steroidal anti-inflammatory drugs, immunosuppressants and immunoglobulins for symptomatic relief in order to achieve individualised and precise treatment. The possibility of alleviating the manifestations of the lesions in patients with LTA through physiotherapy, such as phototherapy, which has a relatively higher safety profile, is the next step to be investigated.
Statement of Consent
Written informed consent was obtained from the patients for the publication of this manuscript and the accompanying images.
This thesis was approved by the Institutional Ethics Committee of the First Hospital of Hebei Medical University ([2023] S00827).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of the relevant literature, analysis and summaries, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors have no conflicts of interest to declare.
Acknowledgments
The authors thank the patient in this case for providing understanding and support for the publication of this article.
Additional information
Funding
References
- Vakili S, Zampella JG, Kwatra SG, Blanck J, Loss M. Lymphocytic thrombophilic arteritis: a review. JCR J Clin Rheumatol. 2019;25(3):147–152. doi:10.1097/RHU.0000000000000846
- Sunderkötter CH, Zelger B, Chen K, et al. Nomenclature of Cutaneous vasculitis: dermatologic addendum to the 2012 revised international chapel hill consensus conference nomenclature of vasculitides. Arthritis Rheumatol. 2018;70(2):171–184. doi:10.1002/art.40375
- Buffiere-Morgado A, Battistella M, Vignon-Pennamen M-D, et al. Relationship between cutaneous polyarteritis nodosa (cPAN) and macular lymphocytic arteritis (MLA): blinded histologic assessment of 35 cPAN cases. J Am Acad Dermatol. 2015;73(6):1013–1020. doi:10.1016/j.jaad.2015.09.010
- Zampella JG, Vakili S, Doig S, et al. Macular lymphocytic arteritis: clinical-pathologic correlation of a rare vasculitis. JAAD Case Rep. 2017;3(2):116–120. doi:10.1016/j.jdcr.2017.01.014