Figures & data
Figure 1. Clinical course of the 41-year-old female patient with a disseminated Hormographiella aspergillata infection.
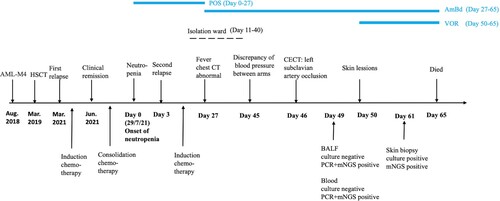
Figure 2. Contrast-enhanced CT showing a pulmonary mass in the left upper lobe invading the left subclavian artery. CT angiography (A) showing the left subclavian artery stenosis (white arrow) and occlusion (red arrow). CT image of the coronal view (B) showing a mass in the left apex of the lung (white arrow) extending into the left subclavian artery. CT images of the lung window (C) and soft tissue window (D) revealed patchy consolidation in the left apex of the lung (red arrow).
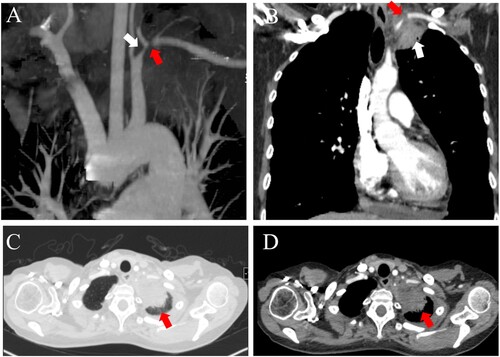
Figure 3. Cutaneous lesions evolution throughout disease progression. A: Onset of red papules located on the medial left forearm. B, C: Development of purplish-red plaques and subcutaneous nodules on the left forearm, left anterior chest wall, and left upper back. D: Appearance of erythematous subcutaneous nodules on the inner left forearm. E, F: Presence of a purpuric plaque with necrotic centre on the left forearm. G: Erythematous subcutaneous nodule on the left anterior chest wall.

Figure 4. Macroscopic and microscopic characteristics of Hormographiella aspergillata. A: Skin tissue cultures on two Sabouraud dextrose agar (SDA) slopes both yielded multiple white, cotton-like, dense pure colonies after seven days of incubation at 25°C. B: White cotton-like colonies on an SDA plate after 10 days of incubation at 35°C. C: Lactophenol cotton blue mount of H. aspergillata slide culture showing branched, septate hyphae with cylindrical arthroconidia accumulating around the conidiophore (original magnification ×400).
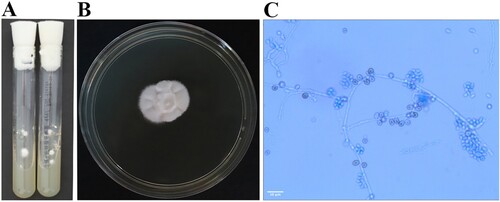
Figure 5. Histological examination of cutaneous Hormographiella aspergillata infection. A: Intravascular thrombosis in both dermal and subcutaneous vessels. (original magnification ×20, haematoxylin and eosin stain). B: Fibrin thrombus in the dermal blood vessels. (original magnification ×400, haematoxylin and eosin stain). C: Branched septate hyphae embedded in fibrin thrombi in the vessels (original magnification ×600, Grocott-Gomori methenamine silver stain).
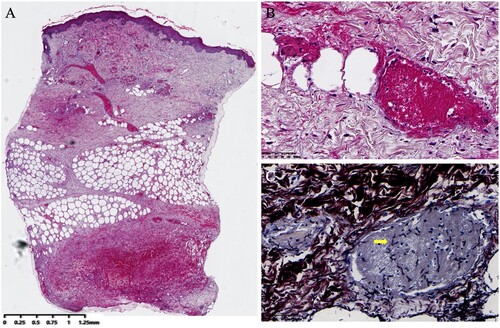
Table 1. Characteristics of invasive Hormographiella aspergillata infection in patients with haematological malignancies.
Table 2. Antifungal susceptibility profile of Hormographiella aspergillata clinical isolates.
Data availability statement
Data supporting the findings of this study are openly available in online repository at: https://www.ncbi.nlm.nih.gov/sra/PRJNA913408.
