Figures & data
Figure 1 Procurement at the US Navy Tissue Bank, Bethesda, Maryland (1950).

Figure 2 Different phases of processing of skin allograft procedure (A) and quality control in Grade B area (B).
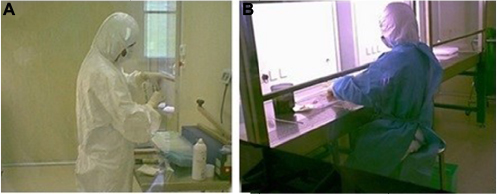
Figure 3 Battery-operated dermatome Aesculap-GA630 (A) and harvesting levels (B) determining skin allograft thickness.

Table 1 Recommendation for microbiological testing of skin samples
Figure 4 Histological study showing cryostat tissue sections of skin allograft samples after MTT assay: the purple formazan pigment marks viable cells and is limited to the epidermal layers.
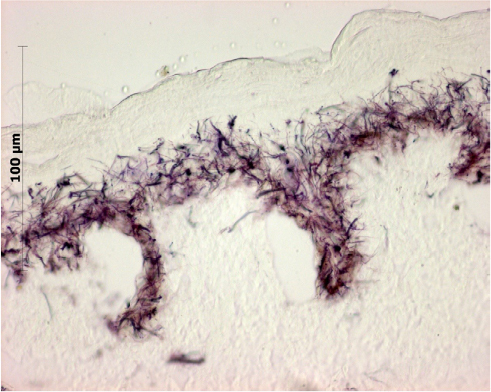
Table 2 Overview of current storage methods
Table 3 Temperature range for storage of tissues and: updated terminology
Figure 5 Skin allograft histopathologic study (hematoxylin and eosin staining) after 15 days of storage at −80°C (original magnification 100×): morphology of skin layers is preserved.
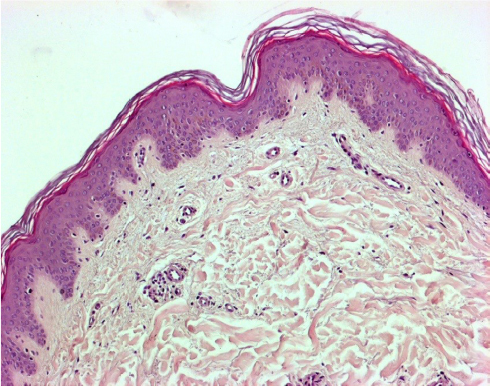
Figure 6 Electron transmission microscopy showing preserved the architectural structure of the dermis, integrity of the basal membrane and skin polarization (A). Histocompatibility test with human fibroblasts, colonizing the dermal surface (B).
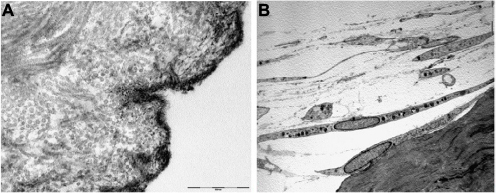
Figure 7 Classification of skin allografts according to their thickness and site of dermatome cleavage.
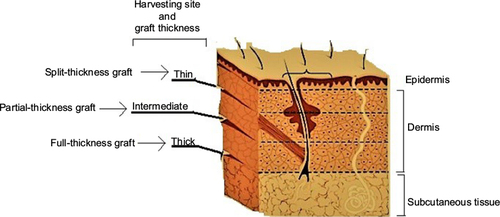
Table 4 Classification of skin allografts according to their thickness
Table 5 Indication of skin bank bioproducts: classification and clinical use
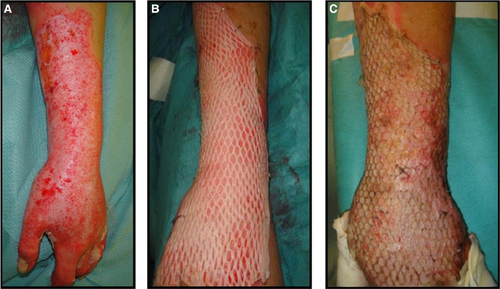
Figure 11 “Alexander” original technique: meshed allograft overlay of an underlying meshed autograft (A). “Sandwich technique”, variant of “Alexander” original technique (B).
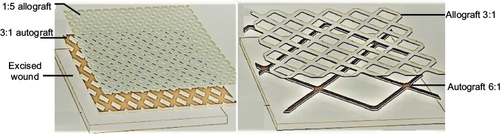
Figure 12 Cryopreserved meshed de-epidermized dermis integration onto the wound bed of a leg ulcer (A) and a full-thickness burn (B).

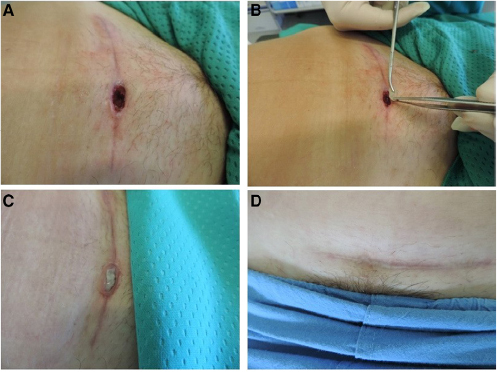
Figure 13 Coverage of tendons exposure and dermal component reconstruction in a deep traumatic wound by glycerolized dermis. Wound appearance after adequate debridement (A), application of glycerolized DED (B), and final re-epithelization after 2 months (C).

Figure 14 Application of lyophilized acellular gamma-irradiated dermis (DED LIO) over a dehisced surgical wound (gastric-onchologic surgery). (A,B,C) Complete healing assessed after 30 days; (D) with integration of DED LIO into the wound bed