ABSTRACT
This article presents the third molar removal in a highly hypnotizable patient, who had been successfully submitted to oral surgery with hypnosis as stand-alone anesthesia in previous sessions. Unexpectedly, hypnosis initially failed, as a result of a nocebo response due to a previous dentist’s bad communication; two complaints made by the patient were associated with increased sympathetic activity (as defined by increased heart rate and electrodermal activity and decreased heart rate variability). After deepening of hypnosis, the patient achieved a full hypnotic analgesia allowing for a successful conclusion of the intervention, an event associated with decreased heart rate, electrodermal activity, and increased heart rate variability. Hence, the initial failure was paralleled by a decreased parasympathetic activity and increased sympathetic activity, while hypnotic analgesia was associated with the opposite pattern. The patient’s postoperative report indicated that the initial failure of hypnosis depended on a strong nocebo effect because of a previous dentist distrusting hypnosis and persuading her that it was not enough to face a third molar removal.
Beeinträchtigung der Hypnose durch Nocebo-Reaktion und damit verbundene neurovegetative Veränderungen: Ein Fallbericht in der Oralchirurgie
Luca Queirolo, Enrico Facco, Christian Bacci, Carla Mucignat und Gastone Zanette
Zusammenfassung: In diesem Artikel wird die Entfernung eines dritten Backenzahns bei einem hochgradig hypnotisierbaren Patienten beschrieben, der in früheren Sitzungen erfolgreich mit Hypnose als eigenständiger Anästhesie operiert worden war. Unerwarteterweise scheiterte die Hypnose zunächst aufgrund einer Nocebo-Reaktion, die auf die schlechte Kommunikation eines früheren Zahnarztes zurückzuführen war; zwei Beschwerden der Patientin waren mit einer erhöhten Sympathikusaktivität verbunden (definiert durch erhöhte Herzfrequenz und elektrodermale Aktivität und verringerte Herzfrequenzvariabilität). Nach der Vertiefung der Hypnose erreichte der Patient eine vollständige hypnotische Analgesie, die einen erfolgreichen Abschluss des Eingriffs ermöglichte, ein Ereignis, das mit einer verringerten Herzfrequenz, elektrodermalen Aktivität und einer erhöhten Herzfrequenzvariabilität einherging. Das anfängliche Versagen ging also mit einer verringerten parasympathischen Aktivität und einer erhöhten sympathischen Aktivität einher, während die hypnotische Analgesie mit dem umgekehrten Muster verbunden war. Der postoperative Bericht der Patientin deutete darauf hin, dass das anfängliche Scheitern der Hypnose von einem starken Nocebo-Effekt abhing, weil ein früherer Zahnarzt der Hypnose misstraute und sie davon überzeugte, dass sie für die Entfernung eines dritten Molaren nicht ausreiche.
Altération de l’hypnose par la réponse nocebo et les changements neurovégétatifs associés: Une étude de cas en chirurgie buccale
Luca Queirolo, Enrico Facco, Christian Bacci, Carla Mucignat et Gastone Zanette
Résumé: Cet article présente l’ablation d’une troisième molaire chez un patient très hypnotisable, qui avait été soumis avec succès à une chirurgie buccale avec l’hypnose comme anesthésie autonome lors de sessions précédentes. De manière inattendue, l’hypnose a d’abord échoué, en raison d’une réponse nocebo due à la mauvaise communication d’un dentiste précédent ; deux plaintes formulées par le patient ont été associées à une activité sympathique accrue (définie par une augmentation de la fréquence cardiaque et de l’activité électrodermique et une diminution de la variabilité de la fréquence cardiaque). Après avoir approfondi l’hypnose, le patient a atteint une analgésie hypnotique complète permettant de conclure l’intervention avec succès, un événement associé à une diminution de la fréquence cardiaque, de l’activité électrodermale et à une augmentation de la variabilité de la fréquence cardiaque. Ainsi, l’échec initial s’est accompagné d’une diminution de l’activité parasympathique et d’une augmentation de l’activité sympathique, tandis que l’analgésie hypnotique a été associée au schéma inverse. Le rapport postopératoire de la patiente indique que l’échec initial de l’hypnose dépendait d’un fort effet nocebo dû au fait qu’un dentiste précédent se méfiait de l’hypnose et l’avait persuadée qu’elle n’était pas suffisante pour faire face à l’ablation d’une troisième molaire.
Deterioro de la Hipnosis por Respuesta Nocebo y Cambios Neurovegetativos Relacionados: Un Caso Clínico en Cirugía Oral
Luca Queirolo, Enrico Facco, Christian Bacci, Carla Mucignat y Gastone Zanette
Resumen: Este artículo presenta la extracción de un tercer molar en un paciente altamente hipnotizable, que había sido sometido con éxito a cirugía oral con hipnosis como anestesia independiente en sesiones anteriores. Inesperadamente, la hipnosis fracasó inicialmente, como resultado de una respuesta nocebo debida a la mala comunicación de un dentista anterior; dos quejas del paciente se asociaron con un aumento de la actividad simpática (definida por un aumento de la frecuencia cardiaca y de la actividad electrodérmica y una disminución de la variabilidad de la frecuencia cardiaca). Tras profundizar en la hipnosis, el paciente alcanzó una analgesia hipnótica completa que permitió concluir con éxito la intervención, un acontecimiento asociado a una disminución de la frecuencia cardiaca y de la actividad electrodérmica y a un aumento de la variabilidad de la frecuencia cardiaca. Por lo tanto, el fracaso inicial fue paralelo a una disminución de la actividad parasimpática y un aumento de la actividad simpática, mientras que la analgesia hipnótica se asoció al patrón opuesto. El informe postoperatorio de la paciente indicaba que el fracaso inicial de la hipnosis dependía de un fuerte efecto nocebo debido a que un dentista anterior desconfiaba de la hipnosis y la persuadió de que no era suficiente para afrontar la extracción de un tercer molar.
Translation acknowledgments: The Spanish, French, and German translations were conducted using DeepL Translator (www.deepl.com/translator).
Introduction
Dental anxiety is a relevant, centuries-old problem (Facco & Zanette, Citation2017). Besides being the main source of perioperative discomfort and stress, anxiety and pain are the main causes of emergencies in dentistry, the most common of which is vasovagal syncope (Muller et al., Citation2008). Hypnosis is a powerful tool allowing for excellent sedation and analgesia, so that patients can face surgery with full wellbeing; hypnosis can even be used as stand-alone anesthesia in patients with a certain level of hypnotizability (Facco et al., Citation2021).
There is increasing evidence that hypnotic analgesia is the result of an intentional introspective activity able to modulate the activity of the pain neuromatrix, including the medial prefrontal cortex and the anterior cingulate cortex (ACC; Casiglia et al., Citation2020; Faymonville et al., Citation2003; Rainville et al., Citation1999). Full analgesia and the blocking of a pain-related sympathetic stress response can be obtained in less than 10 min – a time competitive with pharmacological anesthesia – allowing surgery to take place in full hemodynamic stability with hypnosis as the only anesthetic (Casiglia et al., Citation2012; Facco et al., Citation2021). A wealth of data is now available on the use of hypnosis in surgery; over 1000 subjects plus controls have been enrolled in randomized controlled trials so far, showing that hypnosis improves emotional distress, pain, medication consumption, physiological parameters, recovery, and surgical procedure time (Tefikow et al., Citation2013).
The psychosomatic implications of hypnosis, especially its capacity to modulate the activity of the neurovegetative (or autonomic nervous) system, have been mainly investigated in experimental studies with healthy volunteers but seldom with patients (Fernandez et al., Citation2022). The available data provide some evidence of decreased sympathetic and increased parasympathetic activity in hypnosis, a neuropsychological aspect of which might be the above-mentioned modulation of the ACC. Actually, the ACC is involved in the salience network and in neurovegetative regulation, and, together with the anterior insula, triggers emotional feelings and homeostatic responses (Lamotte et al., Citation2021). It also seems to be involved in both physical and social pain and enhanced attention toward painful stimuli (Rotge et al., Citation2015; Zhang et al., Citation2019). Hypnosis but not pharmacological sedation has been reported to prevent the increase of sympathetic activity in percutaneous transluminal coronary angioplasty of the left anterior descending coronary artery (Baglini et al., Citation2004). Likewise, a study on conversational hypnosis reported an increase of subjective comfort as well as the score on the Analgesia/Nociception Index – a parameter derived from heart rate variability (HRV) reflecting the parasympathetic tone – when compared to oral premedication with hydroxyzine during axillary brachial plexus block for upper limb surgery (Boselli et al., Citation2018).
In short, hypnosis may allow for both relaxation and analgesia as well a helpful modulation of the neurovegetative system, and hypnosis is able to block the sympathetic response to surgical stimuli, a fact worthy of further study. Due to the increasing evidence of the usefulness of wearable devices, it is now possible to study the stress responses to pain and anxiety both in patients and health professionals (Boucsein et al., Citation2012; Queirolo et al., Citation2023).
Here, we report on the upper left third molar removal in a high hypnotizable patient, where the initial failure of hypnosis depended on factors other than her hypnotic ability and was paralleled by changes in neurovegetative balance.
Case Report
A 50-year-old female was admitted for upper left third molar removal. The patient had previous history of dental phobia, paradoxical reaction to IV sedation, urticaria, mild asthma, allergic reactions to lidocaine, aspirin, naproxen, as well as parietaria and gramineous plants. Dental phobia was diagnosed using the Italian version of the Modified Dental Anxiety Scale, showing a score of 18 out of 25 (Facco et al., Citation2015). Given her high hypnotizability – a score of 8.3 in the Hypnotic Induction Profile (Spiegel & Spiegel, Citation2004) – she had already successfully undergone three interventions of oral surgery in our department with hypnosis as the sole anesthesia, one of which was a second-stage implant surgery for the insertion of healing screws; she successfully faced surgery using self-hypnosis by simply doing by herself what she learned during previous interventions in hypnosis (for further details, see patient no. 2 in Facco et al., Citation2021).
Heart rate (HR), blood pressure (BP), electrodermal activity (EDA), skin conductance response (SCR) and heart rate variability (HRV) were measured during the surgical procedure. HR, HRV and EDA were measured by Empatica E4 (Empatica Inc., Cambridge MA, USA), SCR by eSense (Mindfield Biosystem Hindenburgring, Gronau, Germany), and BP by SureSigns VM8 (Philips, Andover MA, USA).
Hypnosis was induced using the Eye-Roll Method (Spiegel & Spiegel, Citation2004), while the following protocol was used to achieve hypnotic focused analgesia:
Suggestion of local anesthesia was delivered while rubbing the patient’s cheek over the tooth with a finger. Immediately after, suggestions were delivered that the perceived sensation was due to the incipient local anesthesia; further suggestions of full analgesia of tooth, gum, mucosa and skin were also delivered.
Suggestion was delivered of neglect of the surgical field.
Then, the subject was invited to relax on a beautiful tropical beach (for further details see Facco, Citation2019; Facco et al., Citation2021).
The patient was allowed to open her eyes and tell the operators whatever she needed while remaining in deep hypnosis, in order to monitor her wellbeing and possible adverse events.
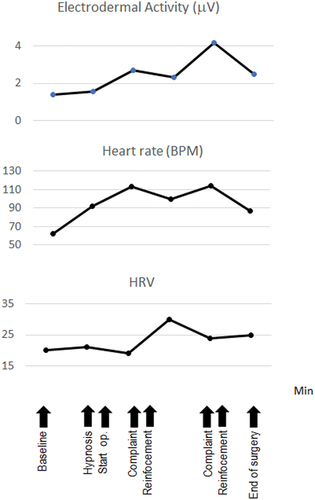
Before the induction of hypnosis, the patient reported her fear of having lost her hypnotizability; the hypnotic interventionist (EF, anesthesiologist and neurologist) reassured her that hypnotizability is a very stable trait (according to Spiegel & Spiegel, Citation2004) and she could feel fully confident of her intact capacity. Following the hypnotic induction, SCR decreased from 9 to 5 per min, HR increased from 62 to 92 BPM, and EDA increased from 1.37 to 1.55 μS. At the beginning of the intervention, the patient reported two seemingly painful events, associated to corresponding changes in the physiological parameters (). Following the first complaint, a short reinforcement was delivered by suggesting relaxation and analgesia. Following this suggestion, HR decreased from 113 to 100 BPM, EDA decreased from 2.7 to 2.3 μS, while HRV increased from 19 to 30 ms. However, this was not sufficient and a second complaint was paralleled by a similar physiological pattern a few minutes later with HR increasing from 100 to 114 BPM, EDA increasing from 2.3 to 4.17 μS and HRV decreasing from 30 to 24 ms. Therefore, a stronger reinforcement was delivered during a short recess of the intervention, by repeatedly suggesting a feeling of cold, making the cheek, gum and teeth frozen and insensitive; at the same time, the patient’s cheek was wetted with a gauze soaked in saline, in order to facilitate patient’s feeling of cold. This allowed for a full hypnotic analgesia and a successful conclusion of surgery, which was associated with decreased HR (from 117 to 87 BPM), EDA (from 4.17 to 2.5 μS) and slight increase HRV (from 24 to 25 ms).
Figure 1. Neurovegetative Fluctuations During Third Molar Removal in a Highly Hypnotizable Patient, Reflecting the Fear of Not Being Able to Face Operation
The following is the patient’s first-person perspective report of the intervention (See the supplemental material for the full transcript of the patient’s report):
I was not tranquil and relaxed like in the previous interventions, due to some new doubts I had no time to analyze and let them go. The reassuring words of the hypnotist probably were not enough to solve them.
During a previous visit a doctor [Authors’ note: this doctor did not belong to the oral surgery staff] “explained” me that the apparent success of hypnosis in previous intervention probably depended to the fact that the bone does not have the same nervous fibers of a tooth with its roots and that the wisdom tooth removal would be much more painful and problematic.
This comment has undermined my confidence and trust in myself: I started to believe that in previous interventions I was not really in hypnosis, but I just got lucky. As a result, I was still struggling to believe that I was really able to do it and this had triggered my anxiety, for I’m a basically insecure person and I’m always terrified I’m not up to the task.
All these concerns were running through my brain, preventing me from paying attention and concentrating in the induction of hypnosis: I reached my safe place, but I stayed on the “threshold” in a sort of state of waiting. When the intervention started, I was concentrated on the tooth: I did not feel pain, but I could visualize the movement of the surgical instrument and, when the surgeon started to sprain the tooth, this triggered a switch, unleashing in me the expectation of pain. Actually, I did not feel pain but only fear. It was the moment I was waiting for, the moment I expected to feel pain. I wished they would stop, and I started to complain.
At this moment the professor (EF) fortunately started talking to me. Something fresh touched my cheek, distracting me from my thoughts, returning my attention to the voice that reassured me. I followed it and from that moment I really felt safe, relaxed and detached, trespassing the threshold of my safe place. The fear had vanished. A few minutes later the professor told me to open the eyes. Unlike the previous interventions, when I felt recharged and in full wellbeing, now I felt exhausted, as if I had overcome a huge obstacle.
Summing up, I think I can still feel satisfied, for I never felt pain, not even in the days to follow. I only experienced five minutes of fear, pure and irrational fear. But eventually, with outside help, I got over it.
Discussion
The relevance of anxiety and its management in dentistry has been well established by the Association of Dental Education in Europe (ADEE). The ADEE’s Profile and Competences for the Graduating European Dentist has established that upon graduating dentists should be competent at “identifying the origins and continuation of dental fear and anxiety” and be able to “manage this fear and anxiety with both pharmacological and behavioral techniques” (Cowpe et al., Citation2010). Among these techniques, iatrosedation and hypnosis have a primary role in the management of dental patients. In fact, they allow patients’ anxiety to improve in a short time (compatible with the timing of the dental setting), overcoming fear and ultimately enabling patients to face interventions with full autonomy (Facco et al., Citation2012; Friedman, Citation1983), while pharmacological sedation only affords a temporary respite in helping to cope with a single procedure.
The APA has defined hypnosis as “A state of consciousness involving focused attention and reduced peripheral awareness characterized by an enhanced capacity for response to suggestion” (G. R. Elkins et al., Citation2015). This definition is undoubtedly correct, but risks skipping a relevant aspect of hypnosis, for example, its psychosomatic potential. In the latter 20th century, Granone, the father of Italian hypnosis, defined hypnosis as “a modified, physiological and dynamic, state of consciousness, during which psychological, somatic and visceral changes are possible by means of plastic monoideisms and by virtue of the operator-patient relationship” (Granone, Citation1987). In our opinion, it would be worth reconsidering these words emphasizing the psychosomatic potential of hypnosis, a fact of paramount importance in medicine though less relevant in psychotherapy.
The effects of hypnosis depend on patient’s hypnotizability, but its assessment is uncommon in clinical studies and its relationship with the outcome is still underexplored in surgery. On the other hand, hypnotizability does not seem the only factor affecting results. It has been reported that hypnotic analgesia might be a more widespread phenomenon than commonly thought – a belief based on anecdotal reports and on the idea that only highly hypnotizable individuals may face surgery with hypnosis as sole anesthesia. In fact, analgesia may occasionally be achieved even in low hypnotizable subjects (Benhaiem et al., Citation2001; Carli et al., Citation2008; Chaves, Citation1994), while factors other than hypnotizability – such as context, motivation and the loop between perception and unconscious processing shaping the features of future experience – should be considered (Chapman & Nakamura, Citation1998).
The concept of suggestibility is an aspect of crucial importance – a leitmotif since the 19th century and still persisting in both research and clinical practice, despite remaining ill-defined and questionable (Facco, Citation2022a; Tasso & Perez, Citation2008). It seems more reasonable to consider the “enhanced capacity of response to suggestions” as the ability to turn them into plastic monoideism, rather than to passively adopt and follow the hypnotist’s suggestions. It may involve three main systems: a) an enhanced cognitive flexibility mediated by the prefrontal cortex, orbito-frontal, hippocampal and amygdaloid system according to the Damasio’s and Thayer’s theories (Beauchaine & Thayer, Citation2015; Bechara et al., Citation2000, Citation2003; A. Damasio, Citation2010; A. R. Damasio, Citation1996; A. R. Damasio et al., Citation1991; Johnsen et al., Citation2003; Shaffer et al., Citation2014; Thayer & Lane, Citation2009; Thayer et al., Citation2009); b) the rapport with its dynamic interpersonal matrix of bidirectional, reciprocal interactions and shared meanings (Baker, Citation2000; Baker & Spiegel, Citation2020); c) the interface between wanting and liking, between subject’s intention and the fear of not reaching what is desired.
Actually, plain hypnotizability, as behaviorally checked from the third-person perspective, may be indistinguishable from acquiescence and yesmanship, two aptitudes insufficient to elicit the most outstanding effects of hypnosis.
The psychosomatic potential of hypnosis is clearly shown by the capacity to modulate the activity of the neurovegetative system, including cardiovascular activity and sympathetic stress response to surgery and pain. If this is the case, hypnosis promises to improve general well-being by promoting both psychological and physical positive functioning (G. Elkins, Citation2022). Accordingly, our main finding is the co-occurrence of physiological and psychological changes: the subjective discomfort was paralleled by increased HR and EDA and decreased HRV, a picture quickly reversed by the deepening of hypnosis. The initial discrepancy between SCR and the other parameters (the former suggesting a decreased sympathetic response) may be related to the ongoing nocebo effect. In fact, the decreased sympathetic responses in the phasic component were associated to an increased tonic component, probably reflecting a mixed interplay of trust and fear.
Though based on a single case, our data confirm the capacity of hypnosis to modulate the parasympathetic and sympathetic branches of the nervous system as components of relaxation and hypnotic analgesia, to be considered as the hallmarks of a full pain control. They lead to disproving the old Hilgard’s hypothesis of the hidden observer and the neodissociation theory (Facco, Citation2022a; Hilgard, Citation1973, Citation1977). Furthermore, they show how the success and failure of hypnosis may depend on factors other than the so-called suggestibility. In fact, our patient was highly hypnotizable and had a very good rapport with the hypnotist, allowing to successfully use hypnosis as stand-alone anesthesia in previous interventions. Nevertheless, this was not enough to get an effective hypnosis here, due to the nocebo response related to the bad communication of a previous dentist, despite being based on scientifically unfounded beliefs. As a result, her doubts, raised by wrong communication and the related fear, led her to anticipate a future experience of pain, decreasing her motivation and capacity to utilize her hypnotic ability. This resulted in a fluctuating level of hypnosis, marked by her complaints and the corresponding fluctuations of the neurovegetative balance.
A wealth of data is available on placebo and nocebo in the literature. The placebo response may cause a long-lasting improvement of pain, anxiety, and depression, depending on patient’s expectations and the doctor–patient relationship (Rutherford et al., Citation2017). The concept of nocebo – the opposite of placebo – can worsen a patient’s condition (Benedetti et al., Citation2007; Colloca et al., Citation2008; Hauser et al., Citation2012), while both placebo and nocebo involve learning mechanisms – be they driven by health professionals, mass media, Internet and/or social context (Colloca et al., Citation2020). This is in line with the observation that dental anxiety and phobia are significantly related to previous bad experiences resulting from doctors’ bad behavior (Facco & Zanette, Citation2017; Facco et al., Citation2015). Actually, nocebo may cause adverse events with a frequency ranging between 30% and 80% in the placebo group of randomized controlled studies (de la Cruz et al., Citation2010; Dimitriadis & Zis, Citation2017; Lombardi et al., Citation2008; Mondaini et al., Citation2007; Penson et al., Citation2018; Zis et al., Citation2018), while hyperalgesia and allodynia may be induced by verbal suggestions – a fact mediated by cholecystokinin release in the brain (Colloca & Benedetti, Citation2007; Colloca et al., Citation2020). The high rate of clinically relevant adverse events has led some authors to advocate the need for withdrawing nocebo from patient’s care and consider it as malpractice (Gelfand, Citation2020; Hansen et al., Citation2020).
The patient’s situation was unexpected. The hypnotist was informed of her doubts on the dental chair, when there was no opportunity to face the problem in detail and restructure it; therefore, he only reassured the patient about its groundlessness, but this was not enough. The patient’s report allows for a full understanding of the nocebo-related origin of the apparent failure of hypnosis, showing nocebo’s detrimental effect.
In conclusion, our report suggests the complexity of hypnotic phenomenology, related to patient’s ability and motivation and affected by several factors unrelated to suggestibility, including nocebo response and expectations shaping the features of future experience. Hypnosis allows for patient’s empowerment – i.e., improved control over mind and body – where the psychosomatic potential, allowing modulation of the neurovegetative balance, has a relevant role in both health and disease. The capacity of hypnosis to improve well-being and significantly decrease distress, including anxiety and depression, in a non-clinical population has been recently reported (Na et al., Citation2022). In this regard, it is worth recalling that anxiety and depression had already been recognized as psychosomatic phenomena in antiquity. Galen, of Pergamon (second century AC) named it Melancholia hypochondriaca (from the Greek μέλας mélas, black, and χολή, cholé, bile), to underscore their physical manifestation at the visceral level (Telles-Correia & Marques, Citation2015).
Since the seminal works of Claude Bernard (Citation1878) and Walter Cannon (Cannon, Citation1929a, Citation1929b), it is accepted that distress involves several organs and systems (including the neurovegetative, endocrine and immune systems) yielding specific physiological changes. Distress is involved in everyday life, as well as in dentistry, pain and several functional disorders, including Medically Unexplained Symptoms (Guo et al., Citation2019; Richardson & Engel, Citation2004) like fibromyalgia and irritable bowel syndrome. If this is the case, the broad spectrum of these disorders calls for being appraised with a holistic, integrative approach taking into account the inseparable mind-brain-body-environment unit. Here, hypnosis with its power to affect both mind and body through its neurovegetative modulation, is shown to be a candidate for a central role in therapy (Fernandez et al., Citation2022; Miller et al., Citation2009). Its understanding can benefit from the availability of noninvasive, portable equipment allowing the monitoring of the neurovegetative balance in real time, opening a new field of investigation worthy of further studies.
An integrated approach involves profound epistemological implications, since mainstream medical science is still affected by the narrow limits of Cartesianism, mainly focusing the attention on the earthen body machine. It is a topic of paramount importance already addressed by the 20thcentury physics (Appleby, Citation2013) and worth being faced by medicine, in order to better understand consciousness, hypnosis, pain, and Medically Unexplained Symptoms (Facco, Citation2021, Citation2022b).
Supplemental Material
Download MS Word (27.7 KB)Acknowledgments
The Spanish, French, and German translations were conducted using DeepL Translator (www.deepl.com/translator).
Disclosure Statement
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/00207144.2024.2311908
References
- Appleby, D. M. (2013). Mind and matter. Cornell Univeristy Library - Hystory and Philosophy of Physics, 1–26. https://arxiv.org/abs/1305.7381
- Baglini, R., Sesana, M., Capuano, C., Gnecchi-Ruscone, T., Ugo, L., & Danzi, G. B. (2004). Effect of hypnotic sedation during percutaneous transluminal coronary angioplasty on myocardial ischemia and cardiac sympathetic drive. The American Journal of Cardiology, 93(8), 1035–1038. https://doi.org/10.1016/j.amjcard.2003.12.058
- Baker, E. L. (2000). Reflections on the hypnotic relationship: Projective identification, containment, and attunement. International Journal of Clinical and Experimental Hypnosis, 48(1), 56–69. https://doi.org/10.1080/00207140008410361
- Baker, E. L., & Spiegel, E. B. (2020). Dancing in the in-between: Hypnosis, transitional space, and therapeutic action. The American Journal of Clinical Hypnosis, 62(1–2), 31–59. https://doi.org/10.1080/00029157.2019.1585328
- Beauchaine, T. P., & Thayer, J. F. (2015). Heart rate variability as a transdiagnostic biomarker of psychopathology. International Journal of Psychophysiology, 98(2 Pt 2), 338–350. https://doi.org/10.1016/j.ijpsycho.2015.08.004
- Bechara, A., Damasio, H., & Damasio, A. R. (2003). Role of the amygdala in decision‐making. Annals of the New York Academy of Sciences, 985(1), 356–369. https://doi.org/10.1111/j.1749-6632.2003.tb07094.x
- Bechara, A., Tranel, D., & Damasio, H. (2000). Characterization of the decision-making deficit of patients with ventromedial prefrontal cortex lesions. Brain a Journal of Neurology, 123(11), 2189–2202. https://doi.org/10.1093/brain/123.11.2189
- Benedetti, F., Lanotte, M., Lopiano, L., & Colloca, L. (2007). When words are painful: Unraveling the mechanisms of the nocebo effect. Neuroscience, 147(2), 260–271. https://doi.org/10.1016/j.neuroscience.2007.02.020
- Benhaiem, J. M., Attal, N., Chauvin, M., Brasseur, L., & Bouhassira, D. (2001). Local and remote effects of hypnotic suggestions of analgesia. Pain, 89(2), 167–173. https://doi.org/10.1016/s0304-3959(00)00359-6
- Bernard, C. (1878). Leçons Sur les Phénomènes de la Vie Communs aux Animaux et Végétaux. Bailliere.
- Boselli, E., Musellec, H., Bernard, F., Guillou, N., Hugot, P., Augris-Mathieu, C., Diot-Junique, N., Bouvet, L., & Allaouchiche, B. (2018). Effects of conversational hypnosis on relative parasympathetic tone and patient comfort during axillary brachial plexus blocks for ambulatory upper limb surgery: A quasiexperimental pilot study. International Journal of Clinical and Experimental Hypnosis, 66(2), 134–146. https://doi.org/10.1080/00207144.2018.1421355
- Boucsein, W., Fowles, D. C., Grimnes, S., Ben-Shakhar, G., Roth, W. T., Dawson, M. E., & Filion, D. L. (2012). Publication recommendations for electrodermal measurements. Psychophysiology, 49(8), 1017–1034. https://doi.org/10.1111/j.1469-8986.2012.01384.x
- Cannon, W. B. (1929a). Bodily changes in pain, hunger, fear and rage. An account of recent researches into the function of emotional excitement. Appleton. https://doi.org/10.1037/10013-000
- Cannon, W. B. (1929b). Organization for physiological homeostasis. Physiological Reviews, 9(3), 399–431. https://doi.org/10.1152/physrev.1929.9.3.399
- Carli, G., Suman, A. L., Biasi, G., Marcolongo, R., & Santarcangelo, E. L. (2008). Paradoxical experience of hypnotic analgesia in low hypnotizable fibromyalgic patients. Archives Italiennes de Biologie, 146(3–9829 (Linking), 75–82.
- Casiglia, E., Finatti, F., Tikhonoff, V., Stabile, M. R., Mitolo, M., Albertini, F., Gasparotti, F., Facco, E., Lapenta, A. M., & Venneri, A. (2020). Mechanisms of hypnotic analgesia explained by functional magnetic resonance (fMRI). The International Journal of Clinical and Experimental Hypnosis, 68(1), 1–15. https://doi.org/10.1080/00207144.2020.1685331
- Casiglia, E., Tikhonoff, V., Giordano, N., Andreatta, E., Regaldo, G., Tosello, M. T., Rossi, A. M., Bordin, D., Giacomello, M., & Facco, E. (2012). Measured outcomes with hypnosis as an experimental tool in a cardiovascular physiology laboratory. The International Journal of Clinical and Experimental Hypnosis, 60(2), 241–261. https://doi.org/10.1080/00207144.2012.648078
- Chapman, C. R., & Nakamura, Y. (1998). Hypnotic analgesia: A constructivist framework. The International Journal of Clinical and Experimental Hypnosis, 46(1), 6–27. https://doi.org/10.1080/00207149808409987
- Chaves, J. F. (1994). Recent advances in the application of hypnosis to pain management. The American Journal of Clinical Hypnosis, 37(2), 117–129. https://doi.org/10.1080/00029157.1994.10403124
- Colloca, L., Barsky, A. J., & Ropper, A. H. (2020). Placebo and nocebo effects. New England Journal of Medicine, 382(6), 554–561. https://doi.org/10.1056/nejmra1907805
- Colloca, L., & Benedetti, F. (2007). Nocebo hyperalgesia: How anxiety is turned into pain. Current Opinion in Anaesthesiology, 20(5), 435–439. https://doi.org/10.1097/aco.0b013e3282b972fb
- Colloca, L., Sigaudo, M., & Benedetti, F. (2008). The role of learning in nocebo and placebo effects. Pain, 136(1), 211–218. https://doi.org/10.1016/j.pain.2008.02.006
- Cowpe, J., Plasschaert, A., Harzer, W., Vinkka‐Puhakka, H., & Walmsley, A. D. (2010). Profile and competences for the graduating European dentist–update 2009. European Journal of Dental Education, 14(4), 193–202.
- Damasio, A. (2010). Self comes to mind: Constructing the conscious brain. Random House.
- Damasio, A. R. (1996). The somatic marker hypothesis and the possible functions of the prefrontal cortex. Philosophical Transactions of the Royal Society of London Series B: Biological Sciences, 351(1346), 1413–1420. https://doi.org/10.1098/rstb.1996.0125
- Damasio, A. R., Tranel, D., & Damasio, H. C. (1991). Somatic markers and the guidance of behavior: Theory and preliminary testing. In H. S. Levin, M. Eisenberg & A. L. Benton (Eds.), Frontal lobe function and dysfunction (pp. 217–229). Oxford University Press. https://doi.org/10.1093/oso/9780195062847.003.0011
- de la Cruz, M., Hui, D., Parsons, H. A., & Bruera, E. (2010). Placebo and nocebo effects in randomized double-blind clinical trials of agents for the therapy for fatigue in patients with advanced cancer. Cancer, 116(3), 766–774. https://doi.org/10.1002/cncr.24751
- Dimitriadis, P., & Zis, P. (2017). Nocebo effect in Menière’s disease: A meta-analysis of placebo-controlled randomized controlled trials. Otology & Neurotology, 38(9), 1370–1375. https://doi.org/10.1097/MAO.0000000000001555
- Elkins, G. (2022). Can hypnotherapy increase well-being? The International Journal of Clinical and Experimental Hypnosis, 70(4), 325–327. https://doi.org/10.1080/00207144.2022.2131135
- Elkins, G. R., Barabasz, A. F., Council, J. R., & Spiegel, D. (2015). Advancing research and practice: The revised APA division 30 definition of hypnosis. The American Journal of Clinical Hypnosis, 57(4), 378–385. https://doi.org/10.1080/00029157.2015.1011465
- Facco, E. (2019). Hypnosis as anesthesia for invasive procedures. In M. P. Jensen (Ed.), Hypnosis for acute and procedural pain management: Favorite strategies of MAster clinicians (pp. 48–75). Denny Creek Press.
- Facco, E. (2021). Pain, the unknown: Epistemological issues and related clinical implications. Minerva Anestesiologica, 87(11), 1255–1267. https://doi.org/10.23736/S0375-9393.21.15920-6
- Facco, E. (2022a). Hypnosis and hypnotic ability between old beliefs and new evidences: An epistemological reflection. The American Journal of Clinical Hypnosis, 64(1), 20–35. https://doi.org/10.1080/00029157.2020.1863181
- Facco, E. (2022b). A neurophenomenological theory of the three worlds. Theory & Psychology, 32(5), 733–753. https://doi.org/10.1177/09593543211068426
- Facco, E., Bacci, C., & Zanette, G. (2021). Hypnosis as sole anesthesia for oral surgery: The egg of Columbus. The Journal of the American Dental Association, 152(9), 756–762. https://doi.org/10.1016/J.ADAJ.2021.04.017
- Facco, E., Gumirato, E., Humphris, G., Stellini, E., Bacci, C., Sivolella, S., Cavallin, F., & Zanette, G. (2015). Modified dental anxiety scale: Validation of the Italian version. Minerva Stomatologica, 64(6), 295–307. PMID: 26173721.
- Facco, E., Manani, G., & Zanette, G. (2012). The relevance of hypnosis and behavioural techniques in dentistry. Contemporary Hypnosis, 29, 332–351.
- Facco, E., & Zanette, G. (2017). The odyssey of dental anxiety: From prehistory to the present. A narrative review. Frontiers in Psychology, 8(Jul), 1855, 1–15. https://doi.org/10.3389/fpsyg.2017.01155
- Faymonville, M. E., Roediger, L., Del, F. G., Delgueldre, C., Phillips, C., Lamy, M., Luxen, A., Maquet, P., & Laureys, S. (2003). Increased cerebral functional connectivity underlying the antinociceptive effects of hypnosis. Brain Research Cognitive Brain Research, 17(2), 255–262. https://doi.org/10.1016/s0926-6410(03)00113-7
- Fernandez, A., Urwicz, L., Vuilleumier, P., & Berna, C. (2022). Impact of hypnosis on psychophysiological measures: A scoping literature review. The American Journal of Clinical Hypnosis, 64(1), 36–52. https://doi.org/10.1080/00029157.2021.1873099
- Friedman, N. (1983). Iatrosedation: The treatment of fear in the dental patient. Journal of Dental Education, 47(2), 91–95. https://doi.org/10.1002/j.0022-0337.1983.47.2.tb01641.x
- Gelfand, S. (2020). The nocebo effect and informed consent-taking autonomy seriously. Cambridge Quarterly of Healthcare Ethics, 29(2), 223–235. https://doi.org/10.1017/S0963180119001026
- Granone, F. (1987). Trattato di Ipnosi. UTET.
- Guo, D., Kleinstäuber, M., Johnson, M. H., & Sundram, F. (2019). Evaluating commonalities across medically unexplained symptoms. International Journal of Environmental Research and Public Health, 16(818), 1–7. https://doi.org/10.3390/ijerph16050818
- Hansen, E., Zech, N., & Benson, S. (2020). Nocebo, informed consent and doctor-patient communication. Der Nervenarzt, 91(8), 691–699. https://doi.org/10.1007/s00115-020-00963-4
- Hauser, W., Hansen, E., & Enck, P. (2012). Nocebo phenomena in medicine: Their relevance in everyday clinical practice. Deutsches Arzteblatt International, 109(26), 459–465. https://doi.org/10.3238/arztebl.2012.0459
- Hilgard, E. R. (1973). A neodissociation interpretation of pain reduction in hypnosis. Psychological Review, 80(5), 396–411. https://doi.org/10.1037/h0020073
- Hilgard, E. R. (1977). The problem of divided consciousness: A neodissociation interpretation. Annals of the New York Academy of Sciences, 296(1), 48–59. https://doi.org/10.1111/j.1749-6632.1977.tb38160.x
- Johnsen, B. H., Thayer, J. F., Laberg, J. C., Wormnes, B., Raadal, M., Skaret, E., Kvale, G., & Berg, E. (2003). Attentional and physiological characteristics of patients with dental anxiety. Journal of Anxiety Disorders, 17(1), 75–87. https://doi.org/10.1016/S0887-6185(02)00178-0
- Lamotte, G., Shouman, K., & Benarroch, E. E. (2021). Stress and central autonomic network. Autonomic Neuroscience: Basic and Clinical, 235(102870), 1–6. https://doi.org/10.1016/j.autneu.2021.102870
- Lombardi, C., Gargioni, S., Canonica, G. W., & Passalacqua, G. (2008). The nocebo effect during oral challenge in subjects with adverse drug reactions. European Annals of Allergy and Clinical Immunology, 40(4), 138–141. http://www.eurannallergyimm.com/cont/journals-articles/133/volume-nocebo-effect-during-oral-challenge-353allasp1.pdf
- Miller, F. G., Colloca, L., & Kaptchuk, T. J. (2009). The placebo effect: Illness and interpersonal healing. Perspectives in Biology and Medicine, 52(4), 518–539. https://doi.org/10.1353/pbm.0.0115
- Mondaini, N., Gontero, P., Giubilei, G., Lombardi, G., Cai, T., Gavazzi, A., & Bartoletti, R. (2007). Finasteride 5mg and sexual side effects: How many of these are related to a nocebo phenomenon? The Journal of Sexual Medicine, 4(6), 1708–1712. https://doi.org/10.1111/j.1743-6109.2007.00563.x
- Muller, M. P., Hansel, M., Stehr, S. N., Weber, S., & Koch, T. (2008). A state-wide survey of medical emergency management in dental practices: Incidence of emergencies and training experience. Emergency Medicine Journal, 25(5), 296–300. https://doi.org/10.1136/emj.2007.052936
- Na, H., Ekanayake, V., Padilla, V., & Elkins, G. R. (2022). Pilot study of hypnotic relaxation therapy for well-being (HRT-WB): A new intervention to enhance well-being and positive affect. The International Journal of Clinical and Experimental Hypnosis, 70(4), 328–349. https://doi.org/10.1080/00207144.2022.2124375
- Penson, P. E., Mancini, G. B., Toth, P. P., Martin, S., Watts, G., Sahebkar, A., Mikhailidis, D., Banach, M., & ILEP, & LBPMC. (2018). Introducing the “drucebo” effect in statin therapy: A systematic review of studies comparing reported rates of statin-associated muscle symptoms, under blinded and open-label conditions. Journal of Cachexia, Sarcopenia and Muscle, 9(6), 1023–1033.
- Queirolo, L., Bacci, C., Roccon, A., Zanette, G., & Mucignat, C. (2023). Anxiety in a regular day of work: A 24 hour psychophysiological investigation in young dentists with gender comparison. Frontiers in Psychology, 14, 1–7. https://doi.org/10.3389/fpsyg.2023.1045974
- Rainville, P., Hofbauer, R. K., Paus, T., Duncan, G. H., Bushnell, M. C., & Price, D. D. (1999). Cerebral mechanisms of hypnotic induction and suggestion. Journal of Cognitive Neuroscience, 11(1), 110–125. https://doi.org/10.1162/089892999563175
- Richardson, R. D., & Engel, C. C., Jr. (2004). Evaluation and management of medically unexplained physical symptoms. The Neurologist, 10(1), 18–30. https://doi.org/10.1097/01.nrl.0000106921.76055.24
- Rotge, J.-Y., Lemogne, C., Hinfray, S., Huguet, P., Grynszpan, O., Tartour, E., George, N., & Fossati, P. (2015). A meta-analysis of the anterior cingulate contribution to social pain. Social Cognitive and Affective Neuroscience, 10(1), 19–27. https://doi.org/10.1093/scan/nsu110
- Rutherford, B. R., Wall, M. M., Brown, P. J., Choo, T.-H., Wager, T. D., Peterson, B. S., Chung, S., Kirsch, I., & Roose, S. P. (2017). Patient expectancy as a mediator of placebo effects in antidepressant clinical trials. American Journal of Psychiatry, 174(2), 135–142. https://doi.org/10.1176/appi.ajp.2016.16020225
- Shaffer, F., McCraty, R., & Zerr, C. L. (2014). A healthy heart is not a metronome: An integrative review of the heart’s anatomy and heart rate variability. Frontiers in Psychology, 5(1040), 1–19. https://doi.org/10.3389/fpsyg.2014.01040
- Spiegel, H., & Spiegel, D. (2004). Trance & treatment. American Psychiatric Publishing.
- Tasso, A. F., & Perez, N. A. (2008). Parsing everyday suggestibility: What does it tells us about hypnosis? In M. R. Nash & A. J. Barnier (Eds.), The oxford handbook of hypnosis (pp. 283–309). Oxford University Press. https://doi.org/10.1093/oxfordhb/9780198570097.013.0011
- Tefikow, S., Barth, J., Maichrowitz, S., Beelmann, A., Strauss, B., & Rosendahl, J. (2013). Efficacy of hypnosis in adults undergoing surgery or medical procedures: A meta-analysis of randomized controlled trials. Clinical Psychology Review, 33(5), 623–636. https://doi.org/10.1016/j.cpr.2013.03.005
- Telles-Correia, D., & Marques, J. G. (2015). Melancholia before the twentieth century: Fear and sorrow or partial insanity? Frontiers in Psychology, 6(Feb). https://doi.org/10.3389/FPSYG.2015.00081
- Thayer, J. F., Hansen, A. L., Saus-Rose, E., & Johnsen, B. H. (2009). Heart rate variability, prefrontal neural function, and cognitive performance: The neurovisceral integration perspective on self-regulation, adaptation, and health. Annals of Behavioral Medicine, 37(2), 141–153. https://doi.org/10.1007/s12160-009-9101-z
- Thayer, J. F., & Lane, R. D. (2009). Claude Bernard and the heart-brain connection: Further elaboration of a model of neurovisceral integration. Neuroscience and Biobehavioral Reviews, 33(2), 81–88. https://doi.org/10.1016/j.neubiorev.2008.08.004
- Zhang, M., Zhang, Y., & Kong, Y. (2019). Interaction between social pain and physical pain. Brain Science Advances, 5(4), 265–273. https://doi.org/10.26599/BSA.2019.9050023
- Zis, P., Hadjivassiliou, M., Sarrigiannis, P. G., Jenkins, T., & Mitsikostas, D. (2018). Nocebo in chronic inflammatory demyelinating polyneuropathy: A systematic review and meta-analysis of placebo-controlled clinical trials. Journal of the Neurological Sciences, 388, 79–83. https://doi.org/10.1016/j.jns.2018.03.009

