ABSTRACT
Limited data are available regarding the association between pre-admission thyroid-stimulating hormone (TSH) levels and prognosis in hospitalized surgical patients treated for hypothyroidism. We retrospectively evaluated a cohort of 1,451 levothyroxine-treated patients, hospitalized to general surgery wards. The 30-day mortality risk was 2-fold higher for patients with TSH of 5.0–10.0 mIU/L (adjusted OR, 2.3; 95% CI 1.1–5.1), and 3-fold higher for those with TSH > 10.0 mIU/L (3.4; 95% CI 1.3–8.7). Long-term mortality risk was higher in patients with TSH of 5.0–10.0 and above 10.0 mIU/L (adjusted HR, 1.2; 95% CI, 1.0–1.6, and 1.7; 95% CI 1.2–2.4, respectively). We found that in levothyroxine-treated adults hospitalized to surgical wards, increased pre-admission TSH levels are associated with increased short- and long-term mortality.
Introduction
Altered thyroid function may have important implications in hospitalized patients, with data suggesting that thyroid dysfunction during hospitalization is associated with increased short- and long-term mortality risk.Citation1–4 On the other hand, studies that included ambulatory patients suggested that mildly increased thyroid-stimulating hormone (TSH) levels may have a protective effect.Citation5,Citation6 The different impact of altered thyroid function between ambulatory and hospitalized patients may be due to the potential changes in thyroid function tests due to non-thyroidal illness during hospitalization, changes in thyroid function secondary to various medications or contrast agents, or other agents that may falsely impact the laboratory assessment of thyroid function tests (TFTs). The measurement of thyroid function during hospitalization may be less accurate than TFTs assessment prior to hospitalization, as TSH and thyroid hormone levels may alter during acute illness.
While hypothyroidism is not considered an absolute contraindication to surgery, especially in cases of an urgent or emergent intervention, thyroid dysfunction may affect cardiovascular, respiratory, hematopoietic, and renal organ systems.Citation7,Citation8 Hypothyroidism may slow drug metabolism, and patients with thyroid dysfunction may be at increased risk for of an overdose of anesthetics and other medications used during the surgical treatment.Citation9 As the pathophysiologic changes associated with altered thyroid function are reversible with replacement of thyroid hormone, there is a general consensus to measure TSH levels whenever possible as part of the preoperative evaluation of any surgical candidate, and to postpone elective surgery until euthyroidism is achieved.Citation7,Citation8,Citation10
The objective of this study was to determine the association between over- and under-treatment of overt hypothyroidism and short- and long-term mortality in patients admitted to general surgery wards, as well as the effect on length of hospital stay (LOHS).
Methods
Retrospective data were extracted from electronic medical records of all patients who were admitted to general surgery wards in Rabin Medical Center (RMC), Israel, between January 2011 and December 2017. RMC, encompassing two campuses, is a tertiary-care facility with more than 1300 beds. Most of the admissions to the four general surgery wards are through the emergency department, and all patients’ data are recorded in electronic medical charts, based on the same database platform used in community primary care facilities. Deaths are entered into the hospital’s mortality database, which is updated according to the population registry of the Ministry of Interior. Mortality data was collected until April 15, 2018.
Our cohort included all adult patients ≥18 years of age with a prior diagnosis of hypothyroidism based on either an ICD-10 code (E03.2-E03.9) of hypothyroidism or a documented chronic use of levothyroxine. In patients with multiple admissions, only the first hospital stay was analyzed. All subjects were actively treated with levothyroxine and had an available TSH measurement up to 6 months before hospitalization. In patients with multiple TFTs prior to admission, only the last measurement prior to admission was analyzed. We excluded patients with central hypothyroidism and subjects without documented TSH levels up to 180 days prior to hospitalization.
Electronic records of study subjects were manually searched for TSH measurements up to 6 months before admission. Chemiluminescence assay (Immulite 2000, Siemens Corp, Los Angeles, California) was used for measuring TSH levels, for which the normal range limits are 0.55 to 4.78 mIU/L. Free thyroxine (FT4) lower and upper limits are 10 to 20 pmol/L. Thyroid function blood tests were performed in the ambulatory setting, between 7:00 and 9:00 am (patients were given information on the timing of taking levothyroxine at the discretion of the treating physician). These are the normal values defined by the central laboratory at Clalit Health Services. TSH levels were classified into four categories: (1) ≤0.5, (2) 0.5–5.0, (3) ≥5.0 and ≤ 10.0, and (4) >10.0 mIU/L. FT4 levels were classified into three categories: (1) low (<10 pmol/L), (2) normal (10–20 pmol/L), and (3) high (>20 pmol/L).
Data on comorbidities () were extracted from the medical records. The cause for each hospitalization was determined according to discharge diagnoses as reported on the electronic medical record. Reasons for hospitalization were classified into five categories ().
Table 1. Baseline characteristics and comorbidities of patients according to TSH levels before admission.
Study was IRB approved by RMC with waiver of consent.
Statistical Analysis
The statistical analysis was generated using SAS Software, version 9.4 (SAS Institute Inc., Cary, NC, USA). Continuous variables were presented by mean ± SD, categorical variables were presented by (n, %). Analysis of Variance (ANOVA) was used to compare continuous variables between study groups.
Outcome measures included length of hospital stay (LOHS), 30-day mortality and mortality at the end of follow-up according to TSH category. Furthermore, we investigated the association between TSH category and mortality for patients who underwent a surgical intervention during the hospital stay.
Logistic regression was used to compare dichotomous variables (including 30-day mortality) between study groups. Kaplan–Meier analysis was used to assess the effect of TSH on survival.
Cox proportional hazards model was used to assess the end of follow-up survival adjusted for study variables, including age, gender, smoking, alcohol, malignancy, chronic renal failure, ischemic heart disease, congestive heart failure, hypertension, diabetes, chronic renal failure, cerebrovascular disease, cause of hospital admission, and surgical procedure performed during hospitalization. The assumptions behind Cox proportional hazards analysis were verified graphically. Complete data were obtained for all the study variables, other than BMI and smoking. No imputation for missing data was done because missing at random cannot be assumed.
Two-sided p-values less than .05 were considered statistically significant.
Results
Study Cohort
There were 42,187 admissions to the 4 surgical wards during the study period. After exclusion of repeat admissions (11,961 admissions), 30226 unique patients were identified. Of these, 2,281 individuals had a prior diagnosis of hypothyroidism, including 2,070 patients receiving levothyroxine. After exclusion of 618 subjects without documented TFTs before admission, and one patient with central hypothyroidism, the final sample included 1,451 participants (mean age 67 ± 16 years, 76% female) ().
On average, TSH levels were determined 66.1 ± 56.0 days prior to admission. Most subjects (988 patients, 68.0%) were well controlled with TSH levels in the normal range (mean TSH, 2.53 ± 1.18 mIU/L), 120 (8.3%) patients were over-treated with TSH levels ≤0.5 mIU/L (mean TSH 0.20 ± 0.16 mIU/L), 233 (16.1%) individuals were under-treated with TSH levels between 5.0 and 10.0 mIU/L (mean TSH 6.86 ± 1.44 mIU/L), and 110 (7.6%) individuals had TSH levels >10.0 mIU/L (mean TSH 24.18 ± 19.59 mIU/L) ().
Patients with TSH levels >10.0 were older, compared to those with normal TFTs (mean age 71.7 ± 15.1 vs. 66.7 ± 16.1 years, p < 0.05), and those with TSH levels ≤0.5 mIU/L were younger (64.1 ± 16.4 years, p < 0.05). Approximately 80% of patients with normal or low TSH levels were women, compared with 69.5% of those with TSH ≥ 5.0 and ≤10.0 mIU/L, and two-thirds of patients with TSH levels above 10.0 mIU/L. There were no differences in mean body mass indices or in rates of lifestyle habits (smoking and alcohol consumption). As for comorbidities, ischemic heart disease was more common among patients with TSH levels ≥5.0 mIU/L, while hypertension, congestive heart failure and chronic renal failure were more common among patients with TSH levels >10.0 mIU/l. Malignancy was more common in those with TSH levels between 5.0 and 10.0 mIU/L. Rates of diabetes mellitus and cerebrovascular disease were similar between study groups ().
The reasons for hospitalization were similar and equal in prevalence between study groups, except for higher prevalence of hepatobiliary and gallbladder surgery in the group of patients with low TSH ().
Nine percent of patients underwent urgent surgical intervention during their hospitalization (with similar rates between study groups, ). In addition, 710 patients (48.9%) underwent elective surgery during their hospitalization. Patients with TSH levels above 5.0 mIU/L had fewer elective surgical procedures ().
Length of Hospital Stay
The mean LOHS (±SD) in the entire cohort was 5.2 ± 5.3 days. The mean LOHS was longer for patients with TSH level below 0.5 mIU/L, TSH levels between 5.0 and 10.0 mIU/L and TSH above 10.0 mIU/L (5.9 ± 6.9, 5.7 ± 7.0 and 6.2 ± 5.7 days, respectively) compared to 4.9 ± 4.6 days for patients with normal TSH levels (p < 0.05) ().
Table 2. Length of hospital stay, 30-day and end-of-follow-up mortality according to TSH levels before admission.
30-Day Mortality
Mortality at 30-days after hospital discharge was 3.8% (55 of 1,451 patients), with a 30-day mortality rate of 5.0% (6 of 120 patients), 2.4% (24 of 988 patients), 6.0% (14 of 233) and 10.0% (11 of 110 patients) among those with TSH ≤ 0.5 mIU/L, normal TSH levels, TSH between 5.0 and 10.0 mIU/L, and TSH above 10.0 mIU/L, respectively (p < 0.05). Of these, 26 patients died during their index admission, including 2 patients (1.7%), 13 patients (1.3%), 6 patients (2.6%), and 5 patients (4.5%), respectively ().
Following adjustment for age, gender, smoking, alcohol, body mass index, malignancy, hypertension, diabetes mellitus, ischemic heart disease, congestive heart failure, cerebrovascular disease, chronic renal failure, cause of hospital admission, and surgical procedure performed during hospitalization, 30-day mortality risk for over- or under-treated hypothyroidism was increased compared with well-controlled levothyroxine-treated hypothyroidism (). Compared to patients with well-controlled hypothyroidism, adjusted odds ratio (OR) of 30-day mortality was 6-fold higher for those with TSH level ≤0.5 mIU/L (adjusted OR, 5.8; 95% CI 1.9–17.9), 2-fold higher for those with TSH levels between 5.0 and 10.0 mIU/L (adjusted OR, 2.3; 95% CI 1.1–5.1), and 3-fold higher for those with TSH levels above 10.0 mIU/L (adjusted OR, 3.4; 95% CI 1.3–8.7) ().
We divided our cohort into two age groups: <60 years and ≥60 years (). In patients younger than 60 years (n = 401), we observed only 3 cases of 30-day mortality, irrespective of pre-admission TSH levels (). In patients aged 60 years and over, adjusted OR of 30-day mortality was 4-fold higher for those with pre-admission TSH level ≤0.5 mIU/L (adjusted OR, 4.2; 95% CI 1.4–12.1), 2.5-fold higher for those with TSH levels between 5.0 and 10.0 mIU/L (adjusted OR, 2.5; 95% CI 1.1–5.5), and almost 4-fold higher for those with TSH levels above 10.0 mIU/L (adjusted OR, 3.7; 95% CI 1.5–9.1) ().
Table 3. 30-day and end-of-follow-up mortality according to TSH levels before admission, divided into two age groups: <60 years and ≥60 years.
End of Follow-Up Mortality
The mean (± SD) follow-up until death or end of follow-up was 2.4 ± 1.7 years in the entire cohort. During follow-up, 34 patients with TSH levels ≤0.5 mIU/L died (34/120 patients, 28.3%), as well as 253 patients with TSH levels between 0.5 and 5.0 mIU/L (253/988 patients, 25.6%), 85 patients with TSH levels between 5.0 and 10.0 mIU/L (85/233 patients, 36.5%), and 54 patients with TSH > 10 mIU/L (54/110 patients, 49.1%) ().
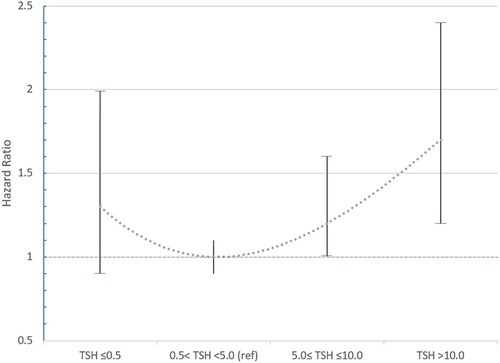
Unadjusted hazard ratio (HR) of all-cause mortality indicated increased mortality risk for patients with TSH levels ≥5.0 mIU/L compared to those with TSH levels in the normal range: HR of 1.5 (95% CI, 1.2–2.0) and 2.2 (95% CI, 1.6–3.0) for TSH levels ≥5.0 and ≤10.0 mIU/L, and TSH >10.0 mIU/L, respectively (). The risk remained significantly increased following adjustment for study variables: adjusted HR of 1.2 (95% CI, 1.0–1.6) and 1.7 (95% CI, 1.2–2.4), respectively. The end-of-follow-up mortality risk for patients with TSH levels ≤0.5 mIU/L was not different than the risk of those with normal TSH levels.
In patients younger than 60 years, the adjusted OR for 30-day mortality was 4-fold higher in patients with pre-admission TSH above 10.0 mIU/L (). In patients aged 60 years and over, adjusted OR for 30-day mortality was higher for those with pre-admission TSH levels between 5.0 and 10.0 mIU/L (adjusted OR, 1.3; 95% CI 1.0–1.8) and for those with TSH levels above 10.0 mIU/L (adjusted OR, 1.7; 95% CI 1.2–2.5) ().
Kaplan–Meier analysis of patient survival following admission demonstrated low survival rates during follow-up for levothyroxine-treated patients with pre-admission TSH levels between 5.0 and 10.0 mIU/L, with a further decrease in survival rates for patients with pre-admission TSH above 10.0 mIU/L (). Although there was no difference in long-term mortality among patients younger than 60 years (), similar findings were observed for patients aged 60 years and over ().
Surgical Intervention Vs. Observation Only
Of the 1,451 levothyroxine-treated patients hospitalized to surgical wards during the study period, 841 (58.0%) patients underwent surgical intervention during hospital stay (9.1% underwent urgent surgery and 48.9% underwent elective surgery, ) and 610 (42.0%) patients were not treated surgically. While most patients with TSH ≤ 0.5 mIU/L (77 of 120, 64.2%) or with normal TSH levels (608 of 988, 61.5%) underwent surgical intervention, less than half of those with TSH levels between 5.0 and 10.0 mIU/L (114 of 233, 48.9%) or TSH levels >10.0 mIU/L (42 of 110, 38.2%) were operated during the hospitalization (p < 0.05) ().
Among those who underwent surgery during hospital stay, mortality rate at the end of follow-up was 20.7% (174 of 841 patients), compared with a mortality rate of 41.3% (252 of 610 patients) among those who were not operated during the hospitalization (p < 0.05).
The end of follow-up mortality risk of patients with TSH ≤ 0.5 mIU/L and patients with normal TSH levels was comparable, whether they had surgery (24.7% vs. 18.6%, respectively; p = 0.22) or not (34.9% vs. 36.8%, respectively; p = 0.86). In comparison to patients with well-controlled TSH levels, patients with TSH between 5.0 and 10.0 mIU/L showed a trend of higher mortality rates, whether they had surgery (26.5% vs. 18.6%, respectively; p = 0.05) or not (46.2% vs. 36.8%, respectively; p = 0.08). Compared with patients with well-controlled TSH levels, the mortality risk was significantly higher for those with TSH levels >10.0 mIU/L hospitalized without surgical intervention (61.8% vs. 36.8%, respectively; p < 0.05), and non-significantly higher for those patients that underwent surgery (27.9% vs. 18.6%, respectively; p = 0.10).
Abnormal Free T4 Levels
Data regarding FT4 levels were available for 118 of 120 (98.3%) patients with low TSH, 474 of 988 (48.0%) patients with normal TSH, 230 of 233 (98.7%) patients with TSH ≥5.0 and ≤10.0 mIU/L, and for all 110 patients with TSH above 10 mIU/L ().
Of the 118 patients with TSH ≤ 0.5 mIU/L and available FT4 measurements, 92 (78.0%) patients had normal FT4 levels, 24 (20.3%) patients had elevated FT4 levels, and 2 (1.7%) patients had low FT4 levels. Of the 230 patients with TSH between 5.0 and 10.0 mIU/L and available FT4 values, 215 (93.5%) patients had normal FT4, 6 (2.6%) patients had elevated FT4, and 9 (3.9%) patients had low FT4. Of the 110 patients with TSH levels >10.0 mIU/L and available FT4 levels, 83 (75.5%) patients had normal FT4 levels, 2 (1.8%) patients had elevated FT4 levels, and 25 (22.7%) patients had low FT4 levels (, ).
Mortality rates at 30-days after hospital discharge in patients with normal FT4 levels were 5.4% (5/92), 2.1% (9/434), 4.7% (10/215) and 7.2% (6/83) among those with TSH levels ≤0.5 mIU/L, normal TSH levels, TSH levels between 5.0 and 10.0 mIU/L and TSH above 10.0 mIU/L, respectively (p < 0.05).
For patients with available FT4 measurement, 30-day mortality rates were generally higher in those with low FT4 compared to those with normal FT4: 6.7% vs. 2.1% for patients with normal TSH levels, 22.2% vs. 4.7% for patients with TSH levels ≥5.0 and ≤10.0 mIU/L, and 20.0% vs. 7.2% for patients with TSH above 10.0 mIU/L (no statistical analysis performed due to the small number of fatalities) ().
At the end of follow-up, mortality risks were similar for patients with normal FT4 who had normal TSH (26.0%) or low TSH (27.2%), but the risk was increased for those with TSH levels ≥5.0 mIU/L and normal FT4 levels: 34.0% and 49.4% for TSH levels between 5.0 and 10.0 mIU/L, and TSH above 10 mIU/L, respectively. The combination of TSH levels ≥5.0 mIU/L with low FT4 was associated with the highest mortality risk (66.7% and 52%, respectively) ().
Discussion
In this study, we found that suboptimal thyroid hormone replacement therapy was associated with worse short- and long-term outcomes in levothyroxine-treated patients with hypothyroidism admitted to surgical wards. Patients with levothyroxine under-treatment admitted to surgical wards with TSH levels between 5.0 and 10.0 mIU/L had an increased risk for short- and long-term mortality, with an additional risk increase in patients with TSH levels above 10.0 mIU/L. We found that TSH levels above 5.0 mIU/L were associated with an increased risk of long-term mortality, whether the patients had surgery or not. These findings indicate low survival rates in patients hospitalized to surgical wards with inadequately treated hypothyroidism, raising the possibility that adjusting treatment to achieve normal TSH levels may improve outcomes.
The literature is sparse with regard to thyroid dysfunction and surgical outcomes in a mixed patient population of the general surgery ward. It may be related to the fact that demonstrating proper care can be technically problematic: TSH and thyroid hormone levels change during stressful times (e.g., hospitalizations) and should be evaluated before, but in proximity to, hospitalization. For this reason, we elected to use TFT determined prior to the hospital stay, but within 6 months of admission.
In our cohort of patients with a diagnosis of levothyroxine-treated hypothyroidism, who were admitted to the surgical ward, 23.7% were under-treated with TSH levels above 5 mIU/L, and 8.3% were over-treated with TSH levels below 0.5 mIU/L.
We found worse short-term outcomes in under-treated patients, compared to patients with well-controlled hypothyroidism: The LOHS was longer, and the 30-day mortality risk was 2-fold higher for those with TSH levels between 5.0 and 10.0 mIU/L, and 3-fold higher for those with TSH levels above 10.0 mIU/L (). The long-term outcomes in under-treated patients were also worse compared with well-controlled patients: adjusted mortality HR of 1.2 and 1.7 for TSH levels ≥5.0 and ≤10.0 mIU/L, and TSH > 10.0 mIU/L, respectively ().
In a publication by Hollowell et al.,Citation11 where the general population was studied, age 60 appears to be the point where TSH levels begin to rise. This also applies to our cohort: the TSH increases as the average age increases (). In this study, we divided our cohort into two age-groups: below 60 years and ≥60 years, in order to investigate mortality outcomes. This observed increase in TSH levels does not seem to have any protective effect on our study population. We found that, in patients aged 60 and over, long-term mortality is higher as TSH levels are higher (, ). We do not know whether these findings are also valid for those aged 60 and under, given the small sample size of this subgroup in our study.
The large proportion of under-treated hypothyroidism in our cohort is probably the result of low treatment compliance or malabsorption, although the physician’s judgment regarding TSH target levels in this relatively older population (with a mean age of 67.2 years) cannot be ruled out. The increased mortality of surgical patients with high TSH levels may reflect a tendency of these patients to delay medical treatment, which in this case manifested as uncontrolled hypothyroidism, and may be associated with other uncontrolled comorbidities. Higher rates of comorbidities in the group of under-treated patients are another possible explanation for the increased mortality: ischemic heart disease, congestive heart failure and chronic renal failure were more prevalent among patients with high TSH levels (). To address this matter, we adjusted for comorbidities associated with increased mortality.
And yet, residual confounding is possible in a retrospective study. It is possible, for example, that patients with more significant (maybe even life-threatening) comorbidities were less adherent to levothyroxine treatment.
Hypothyroidism itself may cause increased postoperative complications and mortality rates.Citation12,Citation13 It should be noted that while previous studies have investigated the association between TSH levels and mortality in patients with untreated subclinical hypothyroidism, we studied a cohort of patients with levothyroxine-treated hypothyroidism.
Uncontrolled levothyroxine-treated hypothyroidism before admission to medical wards was found to be associated with increased long-term mortality.Citation1–4 Considering the survival benefit reported in this study, the authors recommended maintaining TSH levels within the normal reference range in this population.Citation4 The guidelines for the treatment of hypothyroidism by the American Thyroid Association recommend that hospitalized (but not critically ill) patients should seek long-term normalization of serum TSH.Citation14 We found that patients admitted to the general surgery ward, with background hypothyroidism not properly replaced, are at increased risk for short- and long-term mortality.
In agreement with the recommendations above, maintaining TSH levels within the normal reference range (0.5–5.0 mIU/L) in patients with levothyroxine-treated hypothyroidism for whom surgery or hospitalization has been scheduled may be advisable. However, as our study provides retrospective data, prospective studies are needed to further clarify this issue. In the absence of sufficient data, we suggest that the decision to postpone surgery in patients with suboptimal hypothyroidism treatment should be individualized, according to patient’s comorbidities, surgery type and urgency, and TSH level. In fact, a recommendation to delay surgery in all cases of under-treated hypothyroidism may harm patients, due to delayed treatment, without a proven benefit of delayed surgery for TSH correction. Therefore, further interventional studies are needed.
The 30-day mortality risk was 6-fold higher for those with TSH level ≤0.5 mIU/L. This effect of levothyroxine overtreatment on mortality may be explained by the higher mortality rates observed in hyperthyroid hospitalized heart failure patients in comparison to euthyroid and hypothyroid patients.Citation15 Over-treatment may also represent non-adherence to medical follow-up, as it is plausible that these patients did not adjust their levothyroxine dosage according to their lab results.
The mortality at the end of follow-up corresponds to a J-shaped curve (), as mortality is (non-significantly) higher in patients with low TSH levels (HR of 1.3) compared to patients with normal TSH and rise dramatically with TSH levels (adjusted HR of 1.2 and 1.7 for TSH levels ≥5.0 and ≤10.0 mIU/L, and TSH > 10.0 mIU/L, respectively). The appearance of this curve illustrates the difference in the clinical impact of hypothyroidism under-treatment and over-treatment in patients admitted to the surgical ward, and the dose–response effect in hypothyroidism under-treatment (i.e., long-term mortality rises with TSH levels).
Mortality rate at the end of follow-up was lower in patients that underwent surgery during hospitalization, compared with those who were not (20.7% vs. 41.3%). This is probably the result of patient selection for surgery which may be influenced by performance status, comorbidities, personal preferences, life expectancy, etc. However, the end of follow-up mortality risk in patients with and without surgical intervention during hospitalization was higher in all patients without proper thyroid hormone replacement.
We examined the subgroup of patients with normal FT4 levels and found that the rise in TSH category (from normal TSH levels, to TSH between 5.0 and ≤10.0, to TSH >10.0 mIU/L) was associated with both short- and long-term mortality. The combination of high TSH and low FT4 (i.e., overt hypothyroidism) was associated with the highest long-term mortality risk (above 50%). These findings support to our conclusion, that levothyroxine under-treatment is associated with increased short- and long-term mortality in patients hospitalized to surgical wards.
Our study has several limitations. The use of a single TFT value as a predictor of mortality on long-term follow-up is a limitation. The retrospective nature of the study did not allow identification of the exact time point before surgery in which TFTs should be examined. Additionally, cause-and-effect associations cannot be inferred. We could not assess whether an abnormal TFT results led to a subsequent levothyroxine dose adjustment. However, it is likely that if such a change would have been executed, a repeated TFT would follow. Examining pre-admission TFTs not during hospitalization and acute illness reduces the fluctuations that may be seen during an acute illness. And yet, it is possible that non-thyroidal illness affected patients even before hospitalization, especially in those with chronic medical conditions (such as chronic infection or malignancy).
In conclusion, elevated TSH levels before surgical procedures in levothyroxine-treated adults are associated with excess risk of short- and long-term mortality, supporting the recommendation to achieve normal thyroid function prior to elective surgical interventions. As noted, the decision to postpone surgery in patients with suboptimal hypothyroidism treatment should be individualized, according to patient’s comorbidities, surgery type and urgency, and TSH level.
Financial Support Statement
This research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
Disclosure statement
No potential conflict of interest was reported by the authors.
Data availability statement
The data that support the findings of this study are available from the corresponding author, AA, upon reasonable request.
Additional information
Funding
References
- Iglesias P, Ridruejo E, Muñzoz A, et al. Thyroid function tests and mortality in aged hospitalized patients: a 7-year prospective observational study. J Clin Endocrinol Metab. 2013;98(12):4683–4690. doi:10.1210/jc.2012-3849.
- Sforza N, Rosenfarb J, Rujelman R, et al. Hypothyroidism in hospitalized elderly patients: a sign of worse prognosis. J Endocrinol Invest. 2017;40(12):1303–1310. doi:10.1007/s40618-017-0690-2.
- Mingote E, Meroño T, Rujelman R, et al. High TSH and low T4 as prognostic markers in older patients. HJ. 2012;11(3):350–355. doi:10.14310/horm.2002.1364.
- Akirov A, Shochat T, Shechvitz A, Shimon I, Diker-Cohen T, Robenshtok E. Pre-admission TSH levels predict long-term mortality in adults treated for hypothyroidism. Endocrine. 2017;58(3):481–487. doi:10.1007/s12020-017-1453-8.
- Gussekloo J. Thyroid status, disability and cognitive function, and survival in old age. JAMA. 2004;292(21):2591–2599. doi:10.1001/jama.292.21.2591.
- Pearce SHS, Razvi S, Yadegarfar ME, et al. Serum thyroid function, mortality and disability in advanced old age: the Newcastle 85+ Study. J Clin Endocrinol Metab. 2016;101(11):4385–4394. doi:10.1210/jc.2016-1935.
- Stathatos N, Wartofsky L. Perioperative management of patients with hypothyroidism. Endocrinol Metab Clin North Am. 2003;32(2):503–518. doi:10.1016/s0889-8529(03)00007-0.
- Palace MR. Perioperative management of thyroid dysfunction. Health Serv Insights. 2017;10:1178632916689677. Published 2017 Feb 20. doi:10.1177/1178632916689677.
- Bajwa SJ, Sehgal V. Anesthesia and thyroid surgery: the never ending challenges. Indian J Endocrinol Metab. 2013;17(2):228–234. doi:10.4103/2230-8210.109671.
- Vacante M, Biondi A, Basile F, et al., Hypothyroidism as a predictor of surgical outcomes in the elderly. Front Endocrinol. 2019;10:258. Published 2019 Apr 24. doi:10.3389/fendo.2019.00258.
- Hollowell JG, Staehling NW, Flanders WD, et al. Serum TSH, T 4, and thyroid antibodies in the United States Population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab. 2002;87(2):489–499. doi:10.1210/jcem.87.2.8182.
- Jing W, Long G, Yan Z, Ping Y, Mingsheng T. subclinical hypothyroidism affects postoperative outcome of patients undergoing total knee Arthroplasty. Orthop Surg. 2021;13(3):932–941. doi:10.1111/os.12934.
- Kim H, Kong SH, Moon JH, et al. Subclinical hypothyroidism affects the long-term outcomes of patients who undergo coronary artery bypass grafting surgery but not heart valve surgery. Endocrinol Metab (Seoul). 2020;35(2):308–318. doi:10.3803/EnM.2020.35.2.308.
- Haugen BR, Alexander EK, Bible KC, et al. 2015 American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016;26(1):1–133. doi:10.1089/thy.2015.0020.
- Udani K, Patel D, Hart L, Nambudiri V. Impact of hyperthyroidism on in-hospital outcomes of patients with heart failure. J Community Hosp Intern Med Perspect. 2021;11(1):158–162. Published 2021 Jan 26. doi:10.1080/20009666.2020.1840739.