Abstract
Background
The unmet need for safe and effective contraception still remains high. In 2017, about 25% of women of childbearing age who wanted to avoid pregnancy in the developing world were not using a modern contraceptive method. The biggest proportion (21%) of these women live in Sub-Saharan Africa. Little attention has been paid to the health systems factors impacting the integration of family planning into HIV services. This systematic review intends to document health systems factors constraining or facilitating the integration of family planning into HIV services.
Methods
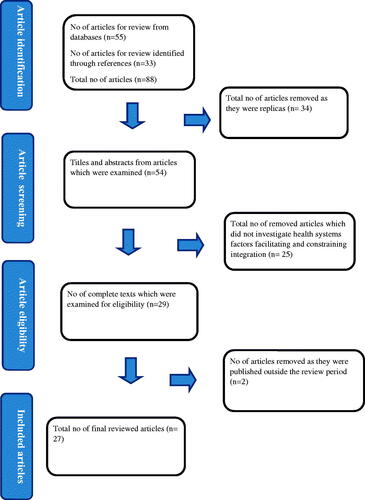
A search of electronic databases such as PubMed and Google Scholar was conducted using keywords. We considered peer-reviewed articles which were published in English between 1st January 2010 and 31st December 2020. The peer-reviewed articles which were considered focussed on identifying barriers and facilitators at the levels of the health system which influence the success or failure of integrated family planning and HIV programs, availability of integrated family planning services in HIV care, the evidence on the feasibility, effectiveness and cost-effectiveness of integrating family planning and HIV services and investigating the outcomes of programs aimed at strengthening family planning integration in HIV counselling, testing and care. Twenty-seven articles that identify factors affecting integration of family planning into HIV services met the inclusion criteria and were thematically analysed.
Results
Health systems factors constraining integration of family planning and HIV services were human resource turnover and shortages, lack of policy guidance on integrated care, poor oversight, unclear service delivery guidelines, inadequate infrastructure and insufficient monitoring systems. Facilitators to the successful integration of family planning into HIV services were identified as training in family planning for service providers, the creation of a supportive policy environment to accommodate service integration, supportive supervision and a positive attitude by service providers towards service integration.
Conclusion
Increase in the health workforce to support integrated service delivery, skills enhancement for service providers and improvement in family planning commodity stock levels play a key role in facilitating the integration of family planning into HIV services.
PLAIN ENGLISH SUMMARY
The findings of this systematic review support integration of family planning into HIV services. The results indicate that it is both possible to integrate family planning into HIV services as well as to implement an integrated model to health care service delivery. Further, the review indicates that there are a number of health systems factors that facilitate as well as constrain the integration of the two services.
Integrating family planning into HIV services addresses a number of Sexual and Reproductive Health challenges being faced by women of childbearing age. Integrated family planning and HIV services reduce high rates of unintended pregnancies among HIV-positive women, reduce high pregnancy-related maternal mortality rates and increase the chance of meeting international and national development goals and targets, particularly Sustainable Development Goal number 3. Integration also helps women receive several services during a single visit to a health facility.
Integrated family planning and HIV services ought to support the provision of comprehensive family planning and HIV services in a country. This is critical to encourage especially women living with HIV infection to access a full range of contraceptive methods. The provision of comprehensive family planning and HIV services allows HIV negative as well as HIV positive couples and individuals to meet their sexual and reproductive health needs.
The review produced sufficient knowledge on the health systems factors which facilitate and constrain the integration of family planning into HIV services.
The systematic review demonstrated the need to deal with health systems barriers in order to ensure success in integrating family planning and HIV services. The review also demonstrated the need for health systems strengthening in order to provide quality integrated family planning and HIV services.
Integration of family planning into HIV services is more and more being used as an approach for meeting the contraceptive needs of HIV-positive women of the childbearing age group.
Training for service providers, supportive supervision, a supportive policy environment and a positive attitude by service providers towards integration were identified as health systems factors facilitating to the integration of family planning and HIV services.
Staff turnover and shortage, inadequate infrastructure, stock-outs of family planning commodities, lack of coordinated leadership for integration, lack of integrated national policies and operational frameworks and separate funding for family planning and HIV services were identified as health systems barriers to integration of family planning and HIV services.
Key Messages
Background
The unmet need for contraception continues to be a global public health problem among HIV-negative and HIV-positive women of childbearing age [Citation1]. In 2017, about 214 million women aged 15–49 years reported an unmet need for contraception [Citation2]. Most of the women with unmet need for contraception live in underdeveloped regions of the world [Citation3]. Among all the regions of the world, sub-Saharan Africa has the highest rate (21%) of unmet need for contraception [Citation4]. The unmet need for contraception is greater in rural areas compared to urban areas [Citation5].
Above 80% of unintended pregnancies among HIV-negative and HIV-positive women globally are as a result of an unmet need for contraception [Citation6]. In Sub-Saharan Africa, about 55.9% of pregnancies among women living with HIV are unintended [Citation7]. Unintended pregnancies among HIV-positive women are associated with a high maternal mortality rate which is ten times more than that of women who are HIV-negative [Citation8]. Integrating family planning and HIV services is thus necessary to reduce high rates of unintended pregnancies, high pregnancy-associated maternal mortality rates and to be able to attain international and national development goals and targets, especially the Sustainable Development Goal 3 [Citation4].
Integration has been defined in many ways [Citation9]. From a recipient point of view, integration is concerned with health care that is easy to navigate [Citation9]. It is a service that is well harmonised and reduces the number of stages in an appointment and the number of separate visits required to a health facility [Citation9]. From the health systems perspective, integration takes place when decisions on policies, financing, regulation and delivery are properly sorted [Citation9].
Providing family planning and HIV services jointly is essential to guaranteeing universal access to family planning services and HIV prevention, treatment, care and support services [Citation10]. Integration also inspires efficient resource utilisation because of better administration of available resources [Citation11]. In addition, it lessens the repetition of actions and leads to shorter waiting times [Citation11]. Further, integration may be used as a tool for generating concerted effort in dealing with lost chances in HIV prevention and family planning services at all service delivery levels [Citation4]. Another benefit of integrating family planning and HIV services is that it can be used as a catalyst for the improvement of the quality of health care services delivered and for increasing the levels of client satisfaction [Citation4]. Integration also encourages the choice of services centred on the full needs of individual patients [Citation10]. Reviews conducted have mainly focussed on the evidence of the feasibility, effectiveness and cost-effectiveness of integrating family planning into HIV services and the range of models used to integrate the two programs [Citation12,Citation13].
Methods
Search strategy
Studies that investigated the integration of family planning into HIV services were identified by searching eighty-eight databases. The following terms were entered into PubMed and Google Scholar “FP” [tab] or “integration” [tab] or “HIV” [tab] or “services” [tab] or “comprehensive” [tab] or “facilitators” [tab] or “barriers” [tab] or “health” [tab] or “factors” [tab] and “systems” [tab]. To find reports on integration, we examined a number of electronic databases through the use of suitable keywords. The search was restricted to the English language.
Inclusion criteria
Studies met the inclusion criteria for the review if they were published in a peer‐reviewed journal between 1st January 2010 and 31st December 2020. Studies were also included if they provided data on the integration of family planning into HIV services. We included any model of family planning integration into HIV services in which the provision of family planning services took place at the family planning department, in the HIV department or through referrals to the family planning departments. The primary outcome of interest for the review was the health systems factors that may facilitate or constrain the integration of family planning into HIV services ().
Data analysis and synthesis
We analysed data from the chosen articles using the thematic analysis technique. Thematic analysis assisted us to find themes and associations from the data which was coded.
Main results
Three of the integrated programs were evaluated in Zambia [Citation13–15]. The remaining twenty-four integrated programs were evaluated in other African countries [Citation4,Citation16–30,Citation31–36]. The majority of the studies integrated family planning with HIV testing (n = 18) or HIV treatment and care (n = 9). Integration of family planning and HIV was found to be possible and cost-effective. Service provider training, supportive supervision, creation of a supportive policy environment and a positive attitude of service providers towards integration were identified as enablers to the integration of family planning and HIV services. Shortage of human resources, inadequate infrastructure, family planning commodity stockouts, lack of coordinated leadership for integration, lack of integrated national policies and operational frameworks and separate financing for family planning and HIV programs were identified as barriers to integration of family planning and HIV services ().
Table 1. Characteristics of included studies.
Health systems factors facilitating and constraining integration of family planning into HIV services
Factors facilitating integration
Training for service providers
Formalised training of service providers in insertions and removals of Long-Acting Reversible Contraceptives (LARC) was identified as key to the success of the provision of integrated family planning services among women who are HIV positive in health facilities [Citation37]. Training included formalised classroom-based with certification, through workshops and through ongoing practical sessions through supportive supervision within hospitals and clinics by family planning Specialists [Citation37]. Training facilitates integration by equipping service providers with the required competencies to provide quality integrated family planning and HIV services. Training also improves the skills in clinical practice as well as in professional competencies and this, in turn, ensures success in service integration.
Supportive supervision
Supportive supervision was also identified as an enabler in the integration of family planning and HIV services [Citation38]. Repetitive checks, corrective support and mentorship were identified to be critical in facilitating knowledge gain about the integration process and improving the clinical practice by service providers [Citation21]. Most on-the-job mentorship programs took place within hospitals and clinics during supportive supervisory visits [Citation37]. Regular supportive supervision helped supervisors to promptly identify the targets and determine if these targets will be met, thereby holding service providers responsible for full implementation of the family planning and HIV interventions [Citation21].
Supportive policy environment
A supportive policy environment with clear policy guidelines was identified as an enabler in the integration of family planning and HIV services [Citation39]. A safe and supportive environment with clear policy guidelines improves the willingness of service providers to support and deliver integrated family planning and HIV services [Citation39]. The Clinical Management of HIV in Children and Adults Policy in Malawi recommends that providers should offer all HIV positive clients with condoms, injectable family planning methods for female clients and refer clients to another provider or site if clients prefer another family planning method. The UNAIDS policy on HIV Testing and Counselling (1997) recommends an increase in women’s voluntary access to VCT services and those women should be offered information on reproductive health and infant feeding. The Uganda policy on Voluntary Counselling and Testing recommends that Counsellors should assess family planning needs for women and refer them to service providers.
A positive attitude by service providers towards integration
A positive attitude by service providers towards integration was also identified as a facilitator in the integration of family planning and HIV services [Citation4]. A positive attitude creates a sense of ownership of the integration process, helps service providers to understand without bias what ought to be integrated and how to integrate the two services [Citation4]. A sense of ownership of the integration process is an example of the positive attitude towards integration by service providers [Citation4]. Another positive attitude towards integration is the providers’ desire to help HIV-infected women make informed choices about birth spacing and limiting [Citation40].
Factors constraining integration
Human resource turnover and shortage
Inadequate numbers of human resources for health at HIV clinics were identified as a barrier to the integration of family planning into HIV services [Citation16]. For the client, human resource shortage is a barrier because it results in increased waiting time and delayed attention. For service providers, shortage of human resource increase workload on a few available staff leads to burnout and compromises the capacity of the already overburdened health personnel to meet service delivery requirements [Citation41]
Inadequate infrastructure
The absence of appropriate physical space in public health facilities was identified as another barrier to the integration of family planning and HIV services [Citation42]. No health care service can successfully be provided without the availability of basic infrastructure [Citation43]. The absence of physical space makes it difficult to maintain privacy and confidentiality for family planning and HIV clients [Citation39]. Lack of infrastructure also affects the process of physical co-location of family planning and HIV services [Citation39].
Stock outs of family planning commodities
Family planning commodity stockouts were identified to have negative consequences in integrated health care service delivery and were, therefore, a barrier to integration [Citation4]. For the client, family planning stockouts represent an access barrier and create anxiety and uncertainty in women because of fear of unwanted pregnancy [Citation14,Citation44]. For service providers, stockouts of family planning commodities affect the skill levels as they are unable to acquire or maintain skills to provide certain family planning methods, especially the long-acting and reversible contraceptive methods due to lack of practice [Citation44]. At the facility level, family planning stockouts affects the success of health facilities in achieving their set targets [Citation44]
Lack of coordinated leadership for integration
Lack of coordinated leadership is an impediment to the integration of family planning and HIV services [Citation41]. Uncoordinated leadership inhibits coordinated planning for integrated services, promotes program territorialism and raises budgetary concerns [Citation41].
Lack of integrated national policies and operational frameworks
Lack of integrated national policies was also identified as a barrier to the integration of family planning and HIV services. Integrated policies on integration are important because they bring together decisions and support functions across different parts of the health care service [Citation9]. Integrated policies and operational frameworks support the development of appropriate care systems, processes and quality standards [Citation45]. Further, integrated policies and national operational frameworks support the holistic evaluation of integrated systems and programs [Citation45]. The absence of integrated national policies and guidelines on the other hand results in fragmentation in service delivery as well as creating boundaries in health care service delivery [Citation45].
Separate financing for family planning and HIV services
Separate financing for family planning and HIV services was another barrier identified to integration. Separate financing undermines progress towards service integration because it affects health system quality and efficiency by compromising budgetary and planning, misalignment of incentives, and duplication and miss-targeting of services [Citation46]. Separate financing may also lead to increased administrative costs and reduced bargaining power for purchasing thereby negatively impacting the integration process [Citation46].
Discussion
The twenty-seven studies reviewed investigated barriers and facilitators to integration of family planning and HIV testing, care and treatment services. The reviewed studies showed that integration of family planning into HIV services is achievable. The studies also showed that there are a number of health systems factors that can facilitate and constrain the integration of family planning into HIV services.
Human resources for health were identified as a barrier to the success of the integration of family planning and HIV services [Citation16]. The capacity of a health system to integrate family planning and HIV services mainly hinges on the placement, enthusiasm, skills and knowledge of the health workforce. This is because a country’s health workforce is the one that is in charge of organising and providing integrated health care services. To achieve success in integration, there ought to be sufficient numbers of health workers operating in the family planning and HIV departments and these health workers ought to have the right mix of skill, knowledge and motivation. It is therefore important that before integrating health care services, the recruitment, distribution and retention processes are evaluated and strengthened. To improve skills and knowledge on integration, pre-service and in-service training for service providers may need to be conducted while incentives may also need to be provided in order to improve staff motivation.
Separate financing for family planning and HIV services were also identified as an impediment to the integration of family planning and HIV services [Citation46]. Finances are used to support health systems to procure family planning and HIV medical supplies, recruit and pay emoluments for health personnel and are also used to support health promotion and preventive activities. Financing family planning and HIV services separately undermine the progress towards service integration because it affects health system quality and efficiency by compromising budgetary and planning, misalignment of incentives, and duplication and miss-targeting of services. Separate financing may also lead to increased administrative costs and reduced bargaining power for purchasing thereby negatively impacting the integration process of family planning and HIV services.
Stock-outs of medical supplies, especially family planning commodities, is another health system factor identified as a barrier to the integration of family planning and HIV services [Citation4]. To function well, a health system must ensure equitable access to essential medical products, including family planning commodities. Regular stock out of family planning commodities is a barrier not only to the attainment of universal access to health but also to the success of the integration of family planning and HIV services. In the absence of family planning commodities, an attempt to integrate family planning and HIV services may prove to be difficult.
Leadership and governance were also identified as an impediment to the integration of family planning and HIV services [Citation39]. Leadership and governance guarantee that a strategic policy framework for service integration is in place and mechanisms for conducting regular supervisory visits are also in place. The absence of clear policy and service delivery guidelines affects effective monitoring of integrated services and coalition-building. A safe and supportive policy environment with clear policy guidelines on the other hand improves the willingness of service providers to support and deliver integrated family planning and HIV services. Clear policy guidelines at various health provision levels, therefore, assure efficiency in integrated service delivery.
Good service delivery is a key ingredient of any health system [Citation47]. Service delivery guarantees access and coverage to integrated family planning and HIV services. In a well-integrated health system, services are of high quality, people-centered and are well coordinated.
Limitations of the review
This review has some limitations. One of the limitations is that although an extensive search and screening process was carried out, we may not have identified all suitable studies. Another limitation arises from the fact that the current evidence-based on health systems factors facilitating or constraining integration is scant.
Conclusions
The results of this review indicate that it is both possible to integrate family planning into HIV services as well as to implement the integrated approach to health care service delivery. The results also show that with skill’s development for service providers, consistency in family planning commodity supply and the presence of appropriate physical infrastructure for integrated service delivery, integration of family planning into HIV services can be achieved and can lead to improved health outcomes. However, there is still a need to conduct further studies to investigate and analyse other health systems factors which act as facilitators or barriers to integration. Factors such as leadership and governance, financing, health information systems, health workforce and service delivery can affect the integration of health care services and ought to be analysed.
Ethics approval and consent to participate
All the twenty-seven studies included in this systematic review received ethical clearance with consent to participate sought from participants.
Consent for publication
This is a review and it did not contain any individual person’s data in any form. Consent for publication was therefore not required.
Author contributions
LN was the major contributor in the conception, design, analysis and interpretation of the data on factors which facilitate and constrain integration of family planning into HIV services. LN was also the writer of this review article.
JMZ and DCS offered significant help during data analysis and interpretation. The two also reviewed critically for logical content. In addition, JMZ and DCS provided the final approval for the work to be published and agreed to be held accountable for the work.
Author’s information
LN is a holder of a Master of Public Health Degree and is currently studying for a PhD in Public Health at The University of Zambia.
| Abbreviations | ||
| HIV | = | Human Immunodeficiency Virus |
| WHO | = | World Health Organisation |
| LARC | = | Long Acting Reversible Contraceptives |
| USAID | = | United States Agency for International Development |
| FP | = | Family Planning |
| UNFPA | = | United Nations Population Fund Agency |
Disclosure statement
The authors declare that they have no competing interests.
Data availability statement
Data sharing is not applicable to this article as no datasets were generated during the current study.
References
- UNFPA. The right to contraceptive information and services for women and adolescents, Briefing paper, Centre for Reproductive Rights; 2010. Accessed 23/06/2021.
- World Health Organization. Contraception: Evidence brief, human reproductive programme. Geneva, Switzerland; 2019.
- Jacobstein R, Curtis C, Spieler J, et al. Meeting the need for modern contraceptives: effective solutions to a pressing global challenge. Int J Gynecol Obstetrics, USA. 2013:1–7.
- Mutisya R, Wambua J, Nyachae P, et al. Strengthening integration of family planning with HIV and other services: Experience from three Kenyan cities. Reprod Health. 2019;16(Suppl 1):62.
- Edietah EE, Njotang PN, Ajong ABB, et al. Contraceptive use and determinants of unmet need for family planning; a cross sectional survey in the North West Region, Cameroon. BMC Womens Health. 2018;18(1):171.
- UNFPA. A deadly gap: Meeting the unmet need for reproductive health care, UFPA/Guttmacher Institute Report; 2012. Accessed on 23/06/2021.
- Feyissa TR, Harris ML, Melka ASS, et al. Unintended pregnancy in women living with HIV in Sub-Saharan Africa: a systematic review and meta-analysis. AIDS Behavior Journal. 2019.
- Teklu T, Belina S, Chemir F, et al. Unintended pregnancy and associated factors among HIV positive women in Ilu aba bora zone, South- Western Ethiopia: a facility- based cross-sectional study. HIV. 2021;13:197–203.
- World Health Organization. Integrated Health Services-What and Why, Technical Brief No.1; 2008. Accessed 25/06/2021.
- Population Action International. The benefits of integrating HIV and family planning programs: Policy and Issue Brief, Washington DC; 2012.
- World Health Organization. Integrating health services: Brief, technical series of primary health care, department of health systems and public health. WHO Regional Office of Europe; 2018. Accessed 25/06/2021
- Shade SB, Kevany S, Onono M, et al. Cost, cost-efficiency and cost-effectiveness of integrated family planning and HIV services. Europe PMC, AIDS. 2013;27(Supplement 1):S87–S92.
- Faye S, Johns B, Baruwa E, et al. Evaluating the Costs and Efficiency of Integrating family planning services into HIV and AIDS Treatment Services in Zambia, Bethesda, MD; Health Finance and Governance Project, Abt Associates; 2015.
- Silumbwe A, Nkole T, Munakampe NM, et al. Community and health systems barriers and enablers to family planning and contraceptive service provision and use in Kabwe district, Zambia. BMC Health Service Research. 2018.
- Chibwesha CJ, Michelle SL, Matoba CK, et al. Modern contraceptive and dual method use among HIV-Infected women in Lusaka, Zambia. Infect Dis Obstet Gynecol. 2011;2011:261453.
- Steinfeld RL, Newman SJ, Onono M, et al. Overcoming barriers to family planning through integration: perspectives of HIV-Positive men in Nyanza province, Kenya. AIDS Res Treat. 2013;2013:861983.
- Irani L, McGinn E, Mellish M, et al. Integration of family planning and HIV services in Malawi: an assessment at the facility level., Washington, DC: Futures Group, Health Policy Project; 2015.
- Brunie A, Patricia N, Mucheri W, et al. Integrating family planning and HIV services at community level: Formative assessment with village health teams in Uganda. Health Services Research, HI. 2017;360.
- Kosgei R, Kizito L, Shen C, et al. Impact of integrated family planning and HIV care services on contraceptive use and pregnancy outcomes: a retrospective cohort study. AIDS J Acquired Immune Deficiency Syndrome. 2011.
- Grossman DD, Onono MM, Newman SJ. S, J, et al. Integration of family planning services into HIV care and treatment in Kenya. AIDS. 2013;27(Supplement 1):S77–S85.
- Baumgartner HD, Green M, Weaver MA, et al. Integrating family planning services into HIV care and treatment clinics in Tanzania: evaluation of a facilitated referral model. Health Policy Plan. 2014;29(5):570–579.
- Wanyenze RK, Matovu JKB, Kamya MR, et al. Fertility desires and unmet need for family planning among HIV infected individuals in two HIV clinics with differing models of family planning service delivery. BMC Womens Health. 2015;15:5.
- Kanyangarara M, Sakyi K, Laar A. Availability of integrated family planning services in HIV care and support sites in Sub-Saharan Africa: a secondary analysis of national health facility surveys. Reprod Health. 2019;16(Suppl 1):60.
- Zewdie Z, Yitayal M, Kebede Y, et al. Status of family planning integration to HIV care in Amhara regional state, Ethiopia. BMC Pregnancy Childbirth. 2020;20(1):145.
- Close MA, Barden-O'Fallon J, Mejia C. Quality of family planning services in HIV integrated and non-integrated health facilities in Malawi and Tanzania. Reprod Health. 2019;16(Suppl 1):58.
- Bintabara D, Nakamura K, Seino K. Determinants of facility readiness for integration of family planning with HIV testing and counseling services: evidence from the Tanzania service provision assessment survey, 2014-2015. BMC Health Serv Res. 2017;17(1):844.
- Mak J, Birdthistle Church K, Preez NF-D, et al. Need, demand and missed opportunities for integrated reproductive health-HIV care in Kenya and Swaziland. AIDS: evidence from Household Surveys. 2013;27(Supplement 1):S55–S63.
- Tweya H, Feldacker C, Haddad BL, et al. Integrating family planning services into HIV care: use of a point-of-care electronic medical record system in Lilongwe, Malawi. Global Health Action. 2017;10(1):1383724.
- Wall MK, Bayingana R, Ingabire R, et al. Rwandan Stakeholder perspectives of integrated family planning and HIV services, Health Planning and Management International Journal; 2018. Accessed 18/8/2021
- Newmann SJ, Kavita M, Onono M, et al. Providers' perspectives on provision of family planning to HIV-positive individuals in HIV care in Nyanza Province, Kenya. AIDS Res Treat. 2013;2013:915923.
- Harrington KE, Newmann JS, Onono M, et al. Fertility intentions and interest in integrated family planning services among women living with HIV in Nyanza province, Kenya: a qualitative study. Infect Dis Obstet Gynecol. 2012;2012:809682.
- Hawkins L, Gertz MA, Badubi O, et al. Integration of family planning services into health care for HIV-positive women in Botswana; 2020.. Accessed:18/08/2021
- Awadhi B, Mboya B, Temu F, et al. Assessing the need and capacity for integration of Family Planning and HIV Counselling and testing in Tanzania; 2012. Accessed:18/08/2021.
- Hope R, Kendall T, Langer A, et al. Health systems integration and reproductive health and HIV services in Sub-Saharan Africa: a scoping study. 2014. Journal of Acquired Immune Deficiency Syndrome. Accessed:19/08/2021
- Nattabi B, Li J, Thompson CS, et al. Family planning among people living with HIV in post-conflict Northern Uganda: a mixed methods study. Confl Health. 2011;5:18.
- Makonnen AD, Roets L. Integrating HIV and family planning services: The Pros and Cons; 2020. Accessed:19/08/2021
- Haberlen SA, Norasimhan M, Laura K, et al. Integration of Family Planning Services into HIV care and Treatment Services: A systematic review; 2017.. Accessed 28/06/2021
- McCarraher R, Vance G, Gwarzo U, et al. Changes in contraceptive use following integration of family planning into ART services in Cross River state, Nigeria. Population Council. 2011;42(4):1–8.
- Wilcher R, Hoke T, Cates SE, et al. Integration of family planning into HIV services: a synthesis of recent evidence. AIDS J. 2013;27(Supplement 1):S65–S75.
- Leslie AJ, Munyambanza E, Adamchak ES, et al. Without strong integration of family planning and PMTCT services in Rwanda, clients remain with a high unmet need of effective family planning, HI/Rwanda; FHI North Carolina, Carolina population center of the university of North Carolina, chapel hill, NC. Afr J Reprod Health. 2010;14(4):151–153.
- Smit JA, Church K, Milford C, et al. Key informants’ perspective on policy-and service- level challenges and opportunities for delivering integrated sexual and reproductive health and HIV care in South Africa. BMC Health Serv Res. 2012;12(1):48.
- Johnston K, Varallyay I, Ametepi P. Integration of HIV and family planning services in Sub-Saharan Africa: a review of literature current recommendations and evidence from service provision assessment health facility surveys. Calverton, Maryland, USA: ICF International; 2012.
- Oyekale AS. Assessment of primary health care facilities' service readiness in Nigeria. BMC Health Serv Res. 2017;17(1):172.
- Grindlay K, Turyakira E, Kyamwanga I, et al. The experience and impact of contraceptive stock out among women, providers and policy makers in two districts of Uganda. International Perspectives on Sexual and Reproductive Health Journal. 2016;42(3):1–10.
- Shaw S, Rose R, Rambold B. 2011. What is integrated Care? Nuffield trust, Research report, UK.
- Siqueira M, Coube M, Millett C, et al. The impact of health systems financing fragmentation in low-and Middle-income countries: a systematic review protocol. Syst Rev. 2021;10(1):164.
- World Health Organization. Monitoring the building blocks of health systems: a handbook of indicators and their measurements strategies. Geneva, Switzerland: WHO Press; 2010.