Abstract
Objective: Cancer- related fatigue (CRF) is one of the most reported long-term effects after breast cancer and severely impacts quality of life. To come towards optimal treatment of multidimensional CRF, the first step is to use a holistic approach to develop a holistic patient profile including the patient’s experience and impact of CRF on their life. Methods and measures: Four semi- structured focus groups with twenty- seven breast cancer patients and fourteen interviews with healthcare professionals (HCPs) were held. Reflexive thematic analysis was used to define (sub)themes for the holistic patient profile. The themes of the interviews and focus groups were compared for validity. Results: Breast cancer patients and HCPs described the same five major themes, consisting of experience of CRF, impact and consequences, coping, personality, and CRF treatment. Experience of CRF consists of cognitive, emotional, and physical aspects. Impact and consequences include work, family, partner relation, social contact and hobbies, body, and misunderstanding. Coping consists of twelve (mal)adaptive strategies. Personality and CRF treatment were summarised as themes. Conclusions: A first holistic patient profile was introduced for CRF for breast cancer. This profile can be conceptualized into a questionnaire to collect information for personalized treatment recommendations and monitoring of CRF over time.
Introduction
Fatigue is one of the most reported long-term effects after breast cancer. It has severe impact on the quality of life (QoL) and patients are often not adequately treated or supported to deal with this (Netherlands Comprehensive Cancer Organisation [IKNL], Citation2019; Schmidt et al., Citation2012). After breast cancer diagnosis, over 75% of breast cancer patients experience cancer-related fatigue (CRF) and 30% experience severe CRF. Additionally, one in five patients is still extremely fatigued ten years after diagnosis (Netherlands Comprehensive Cancer Organisation [IKNL], Citation2019). Moreover, breast cancer patients report more fatigue compared to age-matched controls up to fourteen years after diagnosis (Heins et al., Citation2022). Fatigue is associated with impaired work function, as for instance 75% of the patients who were employed before diagnosis changed their employment status as result of fatigue (Curt et al., Citation2000; Paalman et al., Citation2016). As both the individual and societal impact is high, CRF and the chronification of CRF should be prevented as much as possible. The National Comprehensive Cancer Network (NCCN) Clinical Practice Guideline in Oncology (Citation2022) describes CRF as ‘a distressing, persistent, subjective sense of physical, emotional and/or cognitive tiredness or exhaustion related to cancer or cancer treatment that is not proportional to recent activity and interferes with usual functioning’. Higher levels of CRF are clearly associated with lower general QoL, lower level of functioning (poor physical function, role, cognitive, emotional, social, and sexual functioning) and poor mental health (particularly depression, anxiety and distress) (Abrahams et al., Citation2018; de Ligt, Heins, Verloop, Ezendam, et al., Citation2019). Factors influencing CRF are demographic, medical, psychosocial, behavioural, and biological. Demographic factors protective for the experience of CRF are having a partner, social support, being a strong religious believer, whereas having lower income, belonging to an ethnic minority or being younger result in an increased CRF burden (Bower, Citation2014; Fagundes et al., Citation2015; Kuhnt et al., Citation2019; Puigpinós-Riera et al., Citation2020; Thong et al., Citation2020). Medical factors relate to cancer treatment, with higher risk of fatigue for higher disease stages, more removed lymph nodes, chemotherapy, and cumulative effects of treatment (Abrahams et al., Citation2016; Bower et al., Citation2018; Joly et al., Citation2019; Kuhnt et al., Citation2019; Mitchell, Citation2010; Thong et al., Citation2020). With regard to psychosocial factors, depression, sleep disturbance, negative thoughts, negative self-esteem, catastrophising, and fear of recurrence can increase the risk of fatigue (Abrahams et al., Citation2018; Bower, Citation2014; Bower & Ganz, Citation2015; Curt et al., Citation2000; Huber et al., Citation2011; Joly et al., Citation2019; Kuhnt et al., Citation2019; Mitchell, Citation2010; Thong et al., Citation2020). Physical deconditioning or physical inactivity, and elevated BMI, are behavioural risk factors of CRF (Bower, Citation2014). Anaemia, as a biological factor, can result in CRF (Bower, Citation2014). CRF can be experienced as cognitive (Person et al., Citation2020; Schmidt et al., Citation2018), emotional (Person et al., Citation2020; Schmidt et al., Citation2018), and/or physical (Joly et al., Citation2019; Kuhnt et al., Citation2019; Mitchell, Citation2010; Person et al., Citation2020; Schmidt et al., Citation2018) sensations of tiredness (CRF dimensions), respectively, experienced as but not limited to, diminished concentration or attention, emotional lability and generalised weakness (Bower, Citation2014). Factors that can perpetuate CRF and influence the individuals’ perception of CRF are insufficient coping with the experience of cancer or stress (Bootsma et al., Citation2020; Broeckel et al., Citation1998; Gielissen et al., Citation2006; Glaus et al., Citation1996; Mitchell, Citation2010; Servaes et al., Citation2002a), fear of disease recurrence (Gielissen et al., Citation2006; Young & White, Citation2006), dysfunctional cognitions concerning fatigue (Broeckel et al., Citation1998; Gielissen et al., Citation2006; Servaes et al., Citation2002b; Young & White, Citation2006), patient’s personality and vulnerability (Bootsma et al., Citation2020; Glaus et al., Citation1996; Mitchell, Citation2010), patient’s general well-being (Bootsma et al., Citation2020; Glaus et al., Citation1996), dysregulation of sleep (Bootsma et al., Citation2020; Broeckel et al., Citation1998; Gielissen et al., Citation2006; Mitchell, Citation2010; Prue et al., Citation2006; Servaes et al., Citation2002a, Citation2002b), dysregulation of activities (Bootsma et al., Citation2020; Gielissen et al., Citation2006; Mitchell, Citation2010; Prue et al., Citation2006; Servaes et al., Citation2002a, Citation2002b), and low social support and negative social interactions (Bootsma et al., Citation2020; Gielissen et al., Citation2006; Glaus et al., Citation1996; Servaes et al., Citation2002a, Citation2002b). As the individual perception varies as well as the risk and perpetuating factors, there is a need for a holistic overview of the experience and impact of CRF of the individual patient.
Although CRF has been shown to be multifactorial, previously mentioned studies only focused on parts of the problem of CRF, for example predictors of fatigue (Kuhnt et al., Citation2019), and did not use a holistic approach which applies a biopsychosocial model and recognises a person as a whole (Zamanzadeh et al., Citation2015). The holistic approach can be used to identify different factors related to CRF per individual. So far, research focused on fatigue trajectories with predicting, perpetuating and precipitating factors of CRF, often investigated in patients with quantitative measures (Abrahams et al., Citation2016; Andrykowski et al., Citation2005; Bootsma et al., Citation2020; Bower et al., Citation2018; Kuhnt et al., Citation2019; Puigpinós-Riera et al., Citation2020; Schmidt et al., Citation2018). Quantitative measures only describe the measured construct but lack information about which aspects are important to measure the construct. Qualitative research has been conducted, but either represented quantitatively (Curt et al., Citation2000) or lack aspects such as coping (Penner et al., Citation2020). Schellekens et al. (Citation2019) used a multivariate network approach because of the interplay between patients’ symptoms and protective factors. Several reviews have been conducted, however, they summarise findings from studies assessing single factors in details or concepts instead of using a holistic approach (Abrahams et al., Citation2016; Bootsma et al., Citation2020; Bower, Citation2014; Fagundes et al., Citation2015; Joly et al., Citation2019; Lashbrook et al., Citation2018; Mitchell, Citation2010). Also, a multifactorial approach to CRF is simply not the same as a holistic approach as the latter recognises the person as a whole whereas multifactorial, so multiple factors, not necessarily concerns the whole person. The holistic approach provides the relevant information that must be known about an individual which can be operationalized into a holistic patient profile. Profiles regarding coping have been developed but not to investigate CRF and its perpetuating factors (Cheng et al., Citation2019; Li et al., Citation2017). This emphasises the need for a holistic patient profile of the experience and impact of CRF for the individual patient.
Next to CRF being multidimensional, treatments are highly preference sensitive, and therefore a personal approach with individually tailored treatment plans for CRF seems to be the most promising (Mitchell, Citation2010). If CRF continues for more than three months after cancer treatment, it is unlikely that CRF will decrease without treatment (Goedendorp et al., Citation2013). Treatments are effective in general but do not result in clinically relevant improvement for everyone (Abrahams et al., Citation2017; Buffart et al., Citation2014). Recently, Beenhakker et al. (Citation2022) provided an overview of existing eHealth treatments for breast cancer patients with CRF and the preference sensitive attributes that can be used to align a treatment to the patient’s preferences. Previous research by Wasmann et al. (Citation2019) indicates that participants are less likely to participate if the treatment does not match their preference. As improved patient outcomes are related to treatment adherence (Cillessen et al., Citation2020), we expect that matching the treatment recommendation to patient preferences increases the adherence and thereby patient’s outcomes. Buffart et al. (Citation2014) emphasises the necessity to move from one-size fits all to tailoring as well as including preferences of individual patients but also the patients’ characteristics, needs, and capabilities. Regarding the capabilities, patients whose fatigue might be perpetuated by dysfunctional cognitions could benefit more from cognitive-behavioural therapy (Bower, Citation2014). Therefore, early and personalized advice and treatment recommendations based on holistic overview of the patient are the future in reducing the impact of CRF on the QoL in individuals and societal impact of serious fatigue after breast cancer.
So, a holistic approach is missing in CRF literature to tailor treatment on patients’ characteristics, needs, capabilities, preferences, and their possible influence on each other. The needed information to tailor treatment can be combined in a holistic patient profile that gives an overview of their experience with CRF and the impact on their life. Therefore, the aim of this study was to determine the content that can be used to develop a holistic patient profile for CRF for women with breast cancer. This profile can subsequently be used for personalized treatment recommendation and monitoring of CRF over time.
Method
This study included semi-structured focus groups with breast cancer patients and semi-structured interviews with health care professionals (HCPs). While patients and HCPs are considered relevant stakeholders to develop a holistic patient profile, research often only includes patients’ experiences as for example Bootsma et al. (Citation2020). Breast cancer patients can describe their experience and HCPs working in the field of breast cancer and CRF treatment can be supplemented with their knowledge to get a complete holistic profile of CRF (Kip et al., Citation2018).
For reporting, the consolidated criteria for reporting qualitative research (COREQ) (Tong et al., Citation2007) guideline was used where possible.
Ethical approval of the study was given from all relevant bodies: Committee on Research involving human subjects (CMO, in Dutch ‘Commissie Mensgebonden Onderzoek’) Arnhem-Nijmegen, the clinical institutes who provided the participants (University Medical Center Groningen [UMCG], ‘Ziekenhuisgroep Twente’ [ZGT] hospital, Helen Dowling Institute [HDI] and Roessingh Rehabilitation Centre), and the University of Twente (Faculty of Electrical Engineering, Mathematics and Computer Science). Informed consent was obtained from all participants. The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Focus groups with patients
Patients were recruited from the above mentioned four clinical institutes, either during an outpatient clinic visit or by telephone. Thereafter, the first author (KW) informed the patients about the study. Inclusion criteria used for patients were being 1) female, 2) diagnosed with breast cancer and treated with a curative intent irrespective of the year of diagnosis, 3) at least 18 years of age, 4) under treatment or follow-up in the participating institutes, 5) able to read and write in the Dutch language, 6) able and willing to participate in the focus group, and 7) able to provide informed consent. Patients were excluded if they 1) were also diagnosed with a different cancer than breast cancer, 2) had a relapse or metastases.
In total, 27 patients participated in four online group interviews between April and September 2021. Focus groups were formed with the aim to have different treatments and illness phases per group. Therefore, two focus groups consisted of patients from hospital ZGT: Group 1 with breast cancer patients during active treatment (n = 9) and Group 2 with women who had finished active treatment (n = 6). Ongoing hormonal treatment was allowed in Group 2. For clarity, hereafter, women in both groups will be referred to as patients. Group 3 consisted of UMCG hospital patients recruited after surgery. Group 4 consisted of HDI (a centre providing psychological care to cancer patients and their close others) and Roessingh (rehabilitation centre) patients due to limited number of available patients (n[Roessingh] = 4 and n[HDI] = 3), as ideally a focus group is held with six to ten patients (Evers, Citation2015).
Of the initially approached patients, 53% participated. Patients did not participate because of scheduling of the meetings (n = 24), preference for a physical meeting (n = 1) and not wanting to participate in a group setting (n = 1). During the focus group, patients (n = 2) dropped out due to time limitations or technical issues. Regarding the exclusion criteria, during the focus groups three patients appeared to have had another cancer (kidney and cervical, or secondary primary breast cancer). These three patients were not removed from analysis as there were no differences noticed in the comments which is addressed further in the discussion. The four focus groups had a mean duration of 1:42 h (standard deviation [SD] = 3 min). shows the patient characteristics with a mean age of 54.5 years (SD = 7.6 years). For most patients, the diagnosis of breast cancer was over a year ago (74%, up to 8.5 years).
Table 1. Characteristics of breast cancer patients, with n the number of patients.
Interviews with health care professionals (HCPs)
Team members of the four clinical institutes either approached HCPs themselves or provided contact details of HCPs to contact for the interview. The HCPs work in the field of breast cancer treatment (ZGT and UMCG) or psychological treatment of CRF (HDI) and rehabilitation trajectory (Roessingh). KW informed the HCPs about the interviews via email with the information letter. In total, KW interviewed fourteen HCPs between January and June 2021 with different professions providing information from multiple disciplines. The online interviews had a mean duration of 55 min (SD = 7 min). The HCPs characteristics are shown in . HCPs were on average 47.8 years (SD = 10.8 years) with a mean work experience of 14.9 years (SD = 8.5 years).
Table 2. Characteristics of HCPs.
Data collection
KW conducted the interviews and the focus groups. During the focus groups LB was present as an observer to ensure that everyone participated actively and to keep an eye on completeness of the topics discussed. Supplementary Material 1 contains the semi-structured interview scheme that was used. To get to know the participants, the first question concerned participants’ general experience with breast cancer which is only included in the analysis if it concerned fatigue. Thereafter, information about the individual’s perception of experienced CRF and influence on the patients’ lives was addressed by asking about their direct experience, coping with CRF, and emotions, thoughts, and behaviour regarding CRF. For the HCP, the questions regarded the patient’s life and the diversity of patient’s the HCP treats. LB (MSc) and KW (MSc) are both PhD candidates. The whole research team is female. KW is a Technical Physician and followed a 2-day interviewing course. Due to COVID-19, the four focus groups and fourteen interviews were held online and were audio-recorded for transcription. The participants had no prior knowledge about the researchers. Transcripts were not returned to the participants for comment or correction, nor did participants provide feedback on the findings.
Analysis
Several qualitative methods were considered. Thematic analysis (TA) was most suitable as analysis involves theoretical assumptions and choices whereas Qualitative Content Analysis is atheoretical (Braun & Clarke, Citation2021a). However, a theoretical framework was not found and therefore interpretative phenomenological analysis would be inappropriate. Data is segmented for analysis when using grounded theory whereas coding in reflexive TA can be as fine grained or as coarse as required to address the research goal. Pattern-based discourse analysis was not preferred as this approach focusses on micro details of language practice. On the TA continuum, reflexive TA is most suitable as themes are analytic output from the creative labour of coding whereas coding reliability and codebook approaches have an early theme development (Braun & Clarke, Citation2021a). The data was analysed using the six phases process reflexive TA approach as described by Braun and Clarke (Citation2021d). Concerning data familiarisation, all interviews and focus groups were transcribed verbatim by KW in Dutch and thereafter read while taking notes. During the first analysis, new codes were added until no new codes were used during analysis of new data, resulting in the concept coding scheme. As the coding process was data-driven but the code names are inspired by theory, coding was a combination of inductive and deductive coding. The interview data was coded using Atlas.ti 7. As the holistic patient profile can subsequently be used for personalized treatment recommendation and monitoring of CRF, this requires operationalisation and therefore semantic codes are considered more appropriate compared to latent codes (Braun & Clarke, Citation2021c). To allow for operationalisation into a holistic questionnaire, data was analysed with a realist (post)positivism approach (Braun & Clarke, Citation2021b). Next, constructs were listed in conceptual themes overarching the codes (generating initial themes from coded and collated data). Hereafter, all interviews were re-analysed using the concept coding scheme and re-coded if necessary. After coding all interviews, the developed themes were reviewed. Saturation was considered as no new information was gathered in the last interview and focus group (Braun & Clarke, Citation2021e). Although reflexive TA is about the reflective and thoughtful engagement of the researcher with the data, saturation of the collected information is necessary as this information will be used to determine what should be known of the individual (Braun & Clarke, Citation2019, Citation2021e). The interviews and focus groups were coded by one researcher (KW), and a subset of 10% was also coded by a second researcher (LB) using the concept coding scheme. The level of agreement between the two coders ranged between 83 and 100%. In coding reliability approaches, the researcher subjectivity is seen as a potential threat to coding reliability which can be objectified with measuring the level of ‘agreement’ between multiple coders (Braun & Clarke, Citation2021a). Although the level of agreement is part of the coding reliability approaches on the TA continuum, it is also important with regard to our goal to use the holistic profile to inspire the information needed for personalized treatment recommendations. During the coding process, the researchers (KW, LB, AW, SS, MV and CB) discussed the concept coding scheme several times and adjusted it until agreement was reached about the scheme covering the relevant aspects of the verbal data. The final coding scheme was developed based on comparing and discussing the categorisations. Subsequently, the themes and codes of the concept coding scheme were defined and named. Quotes were translated by KW.
Results
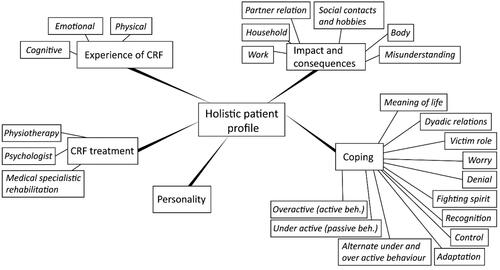
This study aimed to determine the content of a holistic patient profile for CRF in breast cancer patients. TA resulted in the same five major themes for breast cancer patients and HCPs incorporating: 1. Experience of CRF, 2. Impact and consequences, 3. Coping, 4. Personality and 5. CRF treatment. An overview of the themes is illustrated in , see Supplementary Material 2 for the descriptions of (sub)themes. The themes and their subthemes are described below for both focus groups and interviews including the differences between patients and HCPs.
Figure 1. Themes of the holistic patient profile for CRF in breast cancer patients. beh.: behaviour.
1. Experience of CRF
Both HCPs and patients reported that CRF worsened during initial breast cancer treatment. With consecutive treatments, recovery duration increased and the level of energy decreased. During breast cancer treatment, CRF is acknowledged by patients and their social network (friends, family and work), probably because of the patient’s hair loss and fatigue being a side effect of ongoing treatment. However, after successful treatment, the network expected the patient to continue their lives as before diagnosis. Sometimes, patients also expected to continue their lives, but CRF is incomprehensible, described as sudden, and even more intense after treatment. Reintegrating in society made patients aware of their CRF and coping with CRF is a lifelong challenge for some patients. Patients’ activities were not associated to CRF in the same manner in all situations, neither did resting resolve or diminish CRF. Both patients and HCPs described aspects of CRF which are summarised below as cognitive, emotional, and physical fatigue.
Cognitive CRF
Aspects mentioned most by both HCPs and patients considered as cognitive CRF were concentration and memory problems such as forgetfulness and being more sensitive to stimuli or being overstimulated more quickly. Some patients also indicated a full head and less space for processing personal information shared by close others as illustrated by a patient
Concentration and memory are still an issue. Too many stimuli, especially sound, I have to say the influence becomes less. Previously, we could gather around the table with friends, sounds came from everywhere, everyone was talking, and I became quieter, as I did not process the sounds any longer, I turned within myself as my head was full.
(Pt1, 52 years) *All patients are female
So, I think multitasking, is one of which I believe, plays a key role. Processing multiple stimuli from various levels, is a mental aspect you often hear of.
(HCP1, 38-year female)
Emotional CRF
Aspects of emotional CRF were only mentioned by a few patients, but by all HCPs. Both described feelings of fear (of recurrence), uncertainty, frustration, and irritability. HCPs described mood problems and fewer energy to handle emotions. Illustrated by a patient as
[…] then you are so tired, you can only cry and I find that so terrible. The last few weeks, I have been crying more than during the treatment trajectory because I am so tired. I find that confronting for myself as well as for those around me.
(Pt2, 65 years)
[…] but also joy if they get a feeling of regaining control […]
(HCP2, 50-year male)
Physical CRF
Physical CRF is described by most patients and HCPs as reduced fitness, loss of strength or energy and increased energy expenditure. An HCP also mentioned patients having less desire in being active. This form of CRF experience is illustrated by a patient and HCP
I experience just physical fatigue. I do not know, I feel my legs becoming heavier and energy draining my body. […] I cannot remember ever having experienced that in my life. Feeling draining energy, you know.
(Pt3, 50 years)
Yes, perhaps also low energy, less motivation to do things, less desire to take initiative. And sometimes less physical condition, so able to do things for shorter periods of time with regard to taking a walk or sports.
(HCP3, 62-year female)
2. Impact and consequences
This theme reflects the impact and consequences of fatigue on the lives of patients. Several patients indicated that their life changed from being energetic and employed, to being low in energy and needing to recover with ups and downs. Some patients resumed work shortly after treatment, however, after two weeks up to a year the low energy forced them to return to sick leave. This is recognised by several HCPs, reporting that many patients were not able to participate in social activities and role fulfilment as before. Work and family roles that were previously performed automatically have become energy consuming. In addition, an HCP also mentioned financial problems since incomes decreased because of sick leave and expenses increased due to medication costs, travel and parking expenses for hospital appointments, and needing household help. The impact and consequences on the subthemes of work, family, partner relation, social contact and hobbies, body and misunderstanding are discussed below in detail.
Work
Work includes aspects related to work resumption and employability. Patients needed to find a new work-life balance. Some patients were unable to work, others had to reduce work and indicated limitations, or changed their career. For example, entrepreneurs needed to work during treatment, otherwise they had to rebuild their network afterwards or because they were without disability insurance. Patients experienced their inability to work differently, namely grief for losing their independence, unexpected happiness for becoming a housewife, or becoming aware of the importance of work in society as illustrated by
[…] I noticed how important work is in society. If you introduce yourself, you say your name and your profession. I grieved because of my situation, but in the meantime I am satisfied with how I introduce myself. I never realized how it can impact people if they work or not, when you make the choice not to work. […]
(Pt4, 58 years)
Household
Household comprises the influence of CRF on family life within their household and social role fulfilment. Various patients mentioned that CRF affected their children, especially for single parents. In general, children were willing to help, but asking for intergenerational help appeared especially difficult. Patients also indicated being too tired, frustrated, or irritable to give attention to their children. A patient appreciated that role changes were accepted by their family which corresponds to HCPs reporting that roles within families can alter. These role changes are not always desired as indicated by
[…] I just remember a case of a woman with young children of three and one years old. The youngest had her first haircut which was something the mother treasured. However, she was not able to at the moment. So, her mother (the child’s grandmother) took over which she found horrible. These are things that people like to be in control of. […]
(HCP4, 32-year female)
Partner relation
The subtheme partner relation describes how CRF can affect the relationship between patient and her partner. Multiple HCPs indicated that fatigue could put pressure on relationships, resulting in misunderstanding, fatigue changing the relation, or even relationship breaks but partners can also have a stimulating role illustrated by
When you lived life to the fullest and everything was possible, and you become a fatigued person who needs to schedule her day, must rest and are also irritable. Yes, that affects the relationship.
(HCP5, 32-year female)
[…] the worries he has, yes I do forget a lot. Therefore, now and then I need to check. So, the equal relationship we had, is still equal but is also changed at the same time. For example, our talk with the employment expert he was very sad to say what changed. […]
(Pt4, 58 years)
Physical changes occurred between a patient and partner, but the cause might be menopause or fatigue. This might relate to an HCP mentioning that physical problems can limit intimacy.
Social contact and hobbies
Social contact and hobbies cover the social aspects in the patient’s life and the influence of their social support system. Several patients mentioned they realised who their real friends are, and some were unexpected. Patients preferred to have social conversations not limited to cancer with them, or just small talk. Many patients indicated that their social life changed because of limited energy, illustrated by
[…] when meeting friends, previously from 7 pm which could go on all night. This is impossible now. The meetings are shorter, but I think more intense in contact. Just as someone else said, the small talk, I do not enjoy it anymore. The people that are close, with whom spending time is nice and yes sometimes intense conversations.
(Pt1, 52 years)
It affects their social life, as they wonder “Oh that party, do I have to?”. While she would have enjoyed it
(HCP6, 48-year female)
Body
The subtheme ‘Body’ describes the effects of CRF and treatment of breast cancer on the body. The loss of their hair was the most mentioned aspect by patients. Hair loss is very confronting and therefore consumes lots of energy as illustrated by
[…] if you are bald, then you are really ill. So, I can imagine that it consumes lots of energy when looking in the mirror. […]
(Pt4, 50 years)
Several patients improved their appearance by tattooing their eyebrows, wearing a wig, or other scalp covering. Various patients indicated earlier menopause which drains their energy due to hot flushes and sleep disturbances. HCPs indicated body changes following breast surgery affected sensitivity of the breast and femineity. Several HCPs and patients mentioned loss of confidence in the body.
Misunderstanding
Misunderstanding refers to the failure to understand CRF and its limitations by patients and their environment. Several patients mentioned being misunderstood by others post treatment as everybody expects the patient returning to their pre-cancer lifestyle. HCPs call this period ‘the black hole’ which is a tough period for patients. This results in a discrepancy between patient’s desires or expectations and the expectations of the environment. Also being unable to fulfil social roles can lead to misunderstanding as illustrated by
It is really confronting, every time. I have been doing things in a particular way for quite some time. I must do it differently now, I am already seven years since diagnosis. It remains a thing, every time. Previously, everything went so easy, something here, something there. Doing this, also this. Now, after doing for example two things, there is no energy left. That is quite different now.
(Pt5, 53 years)
But also, lots of thoughts about their environment, as they do not understand it and it is invisible.
(HCP2, 50-year male)
Patients also mentioned feeling guilty (e.g. to be fatigued again), or put it down to ageing. In addition, living in a small community where involvement of everyone is expected but no longer possible as limited energy is challenging.
3. Coping
Many coping strategies to deal with CRF were mentioned by both patients and HCPs and will be discussed below, see for an overview of the twelve strategies. Several HCP acknowledged different groups of patients: a small group that has a very active attitude and handles fatigue independently and another small group showing passive behaviour without initiatives to manage CRF. Most patients need some encouragement and information to be able to deal with fatigue. An HCP compared this with the variation in the general population in how people manage health and life, but this difference becomes more pronounced and crucial if diagnosed with cancer.
Overactive or active behaviour
Active behaviour or being overactive is about keeping going and exceeding personal physical, cognitive, and emotional limits, hereafter referred to as personal limits. Patients and several HCPs indicated that preventing exceeding personal limits is a challenge. To signal her personal limits, a patient gets help from her husband
I notice, I am the type that just keeps going. Sometimes I exceed my personal limits which is indicated by my husband as “It is enough”. Then, you notice it immediately, that you are exhausted.
(Pt6, 52 years)
Underactive or passive behaviour
Passive or underactive behaviour is about not taking initiative. Patients did not describe this reaction. Most HCPs described a group of patients who are afraid of becoming fatigued and therefore avoid being active. As a result, their physical condition declines and they become fatigued more easily.
People that out of fear or because they do not know how to do it differently, just lie on the couch because they are tired. [….]
(HCP7, 65-year female)
Alternating between overactive and underactive behaviour
Alternating concerns changing between active and passive behaviour. One patient for example schedules a rest day in advance after a (too) full weekend. Patients exploit good moments as it is so precious to be as active as before breast cancer illustrated by
Sometimes, I schedule days of rest. [….] For example, I have a nice weekend during which I chose to ignore my tiredness and doing everything knowing that I have to pay. So, I reserve the whole Monday to stay on the couch and do nothing. [….]
(Pt7, 52 years)
Adaptation
Adaptations means adjusting to CRF by changing daily-life, accordingly, illustrated by
Take what you can get, within your limits of comfort and respect for yourself.
(HCP8, 52-year male)
Control
Control is about the degree of control patients can or want to execute. Several patients indicated the desire to control their agenda with limited scheduled appointments. In addition, some HCPs mentioned being in control is an essential part of being human and that patients who especially need high levels of control, will become troubled if they have less control. Some patients presented complaining of fatigue, asking the HCP for a solution wherein the patient adopted a submissive role. Various HCPs indicated that patients who realise they have impact on their own CRF experience, are better capable of coping with fatigue. Patients experienced difficulties with social activities because of personal limits, for example
Going for a walk, can sometimes be one hour and other times it can be half an hour. Both are fine, but it can be challenging if you go with a friend who is determined to walk one and a half hours. This can result in crossing your personal limits which you regret afterwards. As a consequence, I prefer to plan my own activities.
(Pt8, 50 years)
Recognition
Recognition is about accepting CRF and about recognition by others. Various patients indicated that the focus group provided peer support, resulting in lots of recognition, and understanding. Several HCPs indicated the importance of recognition by others. Many patients mentioned accepting CRF is needed, illustrated by
Acceptance seems to be particularly important. I always think, you are who you are now, with the fun and less pleasant things. That is one of the hardest things in my opinion.
(Pt4, 58 years)
Fighting spirit
Fighting spirit includes a positive attitude, being strong, and having a survival or fighting mode. Patients mentioned that communicating about personal limits is hard, as participation is desired but not possible if the mind and emotions are not aligned. At the same time, they were aware of their progress
But we are back, we are still here and we are doing really well. So, I keep reminding myself every instance, look at where we came from and what we are all capable of now
(Pt5, 53 years)
Denial
Denial concerns CRF being ignored or not taken seriously. A patient denied her CRF, as CRF was invisible for others it was possible to chat away a lot, by distracting herself and others from CRF in conversation. Several HCPs mentioned this as denial, communicating in a way to hide CRF, keeping going and denying your problems. Nine out of ten patients do not take CRF serious enough in the beginning and CRF is not always recognised by patients as illustrated by
Do not always recognise fatigue, so not recognising feeling emotionally worse or being angrier as symptoms of fatigue. They blame themselves for feeling bad and not being nice for the people around them. They will step up and overload even more.
(HCP9, 53-year female)
Worry
Worry is about pessimistic thinking, negative thoughts and worrying. Several patients doubted their perceptions and feelings. This is also acknowledged by various HCPs as thoughts and feelings of insufficiency. HCPs also indicated that patients are more anxious and worrisome. A patient reported agitation as she experienced failure illustrated by
Failure, disappointment, and doubt. With fatigue I get the feeling I failed; I cannot do it all. That disappoints me, resulting in doubts such as: will I succeed? Now, I am fighting hard to return, at least till I am halfway. If I am only halfway… But even that does not work, then you start to doubt. Should I work twelve hours a week, sixteen or eighteen? That results in turmoil. And where should I draw the line to regain rest?
(Pt6, 52 years)
Victim role
Victim role includes self-pity, lingering in CRF and all that is not possible anymore illustrated by a patient as
I can get really frustrated wondering why, why, why. I have the impression I will never get back to pre-cancer level [….]
(Pt9, 44 years)
Dyadic relations
Dyadic relations entail that breast cancer and CRF is not only experienced and dealt with by the patient but also involves others to cope with CRF. Patients mentioned seeking social support by calling a friend when feeling down or motivation by their partner. HCPs indicated the partner or network can be stimulating as well as discouraging.
Often towards partners, children, or family, it can sometimes give battles. The patient is too tired, and the partner thinks we should walk around the block because that is beneficial for you. And we should do this and that. It is important to inform that it is not unwillingness of the patient but can result from the treatment. That can clear the air between people. One has good intentions, but the other cannot do it at the moment. You can wonder, because some patients need stimuli, but if it causes friction than it can help to give relief, give recognition.
(HCP10, 32-year female)
Meaning of life
Meaning of life concerns personal values, making other choices, self-development, and appreciation of life. Several patients and HCPs indicated living more aware such as finding happiness in small things and using energy just for desired activities. Patients also mentioned having a positive mindset, being resilient and being grateful to be able to do a lot. Several patients experienced personal growth as being slowed down instead of juggling many balls or switching career and rethinking the way of living illustrated by
You notice that other things in your life become important. So, for me it meant reassessment of what I still want, what I am able to, what is important, who is important, etcetera.
(Pt10, age unknown)
In the next section, aspects that are embedded into the patients’ personalities and how patients and HCPs view the influence of character traits are discussed.
4. Personality
Personality is about the influence of character traits on CRF and alterations in character traits due to CRF. Patients indicated changes of their personality, such as being a less happy person or busy bees becoming more introvert as illustrated with the quote,
It is not who I am, naturally I like the unexpected. If someone rings the doorbell for teatime, I always enjoyed it, however I have difficulties with scheduled appointments. No matter how nice these moments are, even a dinner or something else. At the moment, this is difficult but normally, nowadays I am really having a tough time with that.
(Pt5, 53 years)
I think, in particular the tools people possess, you know one character is not the other. You have some kind of innate tools to deal with disappointment and setbacks. You see differences in that. People that experience every bump in the road as “the Mount Everest”, suffer more than people saying it is a bump, but we are going to take it (not as “the Mount Everest”).
(HCP6, 48-year female)
The above-mentioned themes in 1. Experience of CRF, 2. Impact and consequences, 3. Coping, and 4. Personality sections are relevant to obtain insight into the patient’s experience of CRF, and impact of CRF on their life to come towards personalized treatment advice. The patients who underwent treatment for CRF and the HCPs working in the field of breast cancer treatment or CRF treatments, also provided information about CRF treatment.
5. CRF treatment
Only a few patients mentioned treatments for CRF, namely blood transfusion for low Hb, oncology physiotherapy, haptotherapy, mindfulness, yoga and peer support. An illustration of the effect of certain treatments is
Mindfulness and yoga help me a lot. It really relaxes me, thereby accepting it much better.
(Pt11, 56 years)
In summary, the relevant content for the holistic patient profile as compiled from the analysis of the focus group and interviews is provided in .
Discussion
The aim of this study was to develop a holistic patient profile for CRF for breast cancer patients which can be used to systematically assess the patient and to serve as a basis for personalized treatment advice and monitoring of CRF over time. The holistic approach resulted in the identification of five themes consisting of the experience of CRF, impact and consequences, coping, personality, and CRF treatment. Regarding the experience of CRF, both patients and HCPs mentioned aspects of cognitive, emotional, and physical fatigue, supporting the multidimensionality of CRF (NCCN, Citation2022). The impact and consequences of CRF are enormous and affect work, the patient’s body and relationships with family, partner, as well as social participation. The patients must find a balance between on the one hand not doing or wanting too much, but on the other hand also not expecting too much or too little of themselves. Also misunderstanding regarding CRF was an important aspect of the findings. For coping, both adaptive and maladaptive coping strategies were mentioned. With regard to personality, one has innate tools to deal with disappointment and setbacks which can be helpful or unhelpful in dealing with CRF. Concerning CRF treatment, several treatments were mentioned consisting of different aspects to handle CRF. As the individual perception, risk factors and perpetuating factors vary, an overview of the experience and impact of CRF on the individual was developed based on qualitative data from patients and HCPs. The ability to answer the research question, justifies the chosen data-analysis method and our assumptions. The (sub)themes in the results play an essential role in the development of personalized treatments advice based on the holistic patient profile.
In our research, focus groups and interviews allowed the participants to inform us how patients experience CRF in their daily lives. With the involved stakeholders, we assured that HCPs and patients were included from a peripheral and academic hospital as well as consulting participants from tertiary line of care institutes that offer CRF treatments. In this way, we could check if the patients were a good representation of the heterogeneity of the population at stake and collect information from multiple HCP disciplines. This is a strength of this study since other research has often only included patients, not HCPs (Bootsma et al., Citation2020). Although CRF is one of the most commonly reported health problems, less than half of the patients visit a health care professional for CRF, as indicated by de Ligt, Heins, Verloop, Smorenburg, et al. (Citation2019). This highlights the importance of both patients and HCPs as stakeholders. Another important strength of the study is the high concordance between themes that arose from the interviews with professionals and focus groups with patients, which can be interpreted as a sign of validity for the holistic patient profile. Validity is important as this allows the profile to serve as a basis for personalized treatment advice and monitoring of CRF over time. The most interesting difference between HCPs and patients in our results is that patients did not mention underactive coping, but HCPs observed this in their patient population. This corresponds to a recent review by Schaab et al. (Citation2023) summarising that passive management strategies such as avoidance and fatalism worsen CRF. This could be explained by the underrepresentation of passive patients in the study because they are less likely to participate in focus groups or that this coping strategy is less recognised by patients themselves. Another explanation might be unawareness of the patients of their behaviour, but more research is needed to confirm this. Also, all HCP mentioned emotional fatigue, compared to few of the patients. It could be that not all patients recognise emotional fatigue in all its aspects as also being part of CRF.
Using a holistic approach, all relevant information was collected to gain understanding of the importance of subthemes and the relation between subthemes, themes, and CRF illustrated in . This is an advantage of the holistic approach compared to reviews or combining existing literature, as Bootsma et al. (Citation2020) indicated that not for all themes there were responses from all individuals. Furthermore, CRF prediction models, such as the one of Chartogne et al. (Citation2021) only explained 56% but lacks, for example coping strategies which was identified as relevant by both patients and HCPs and is one of the themes in our holistic patient profile. Additionally, Lashbrook et al. (Citation2018) described coping strategies while Fagundes et al. (Citation2015) used a biobehavioural approach. However, without a holistic approach it is not possible to determine the relation with CRF of different factors or concepts. Since the holistic patient profile is developed based on the information provided by a sample of relevant stakeholders, validation is needed as it could be different when other types of HCPs are recruited or patients from other regions of the Netherlands or other countries were recruited.
Despite the strengths of this study, it is important to acknowledge its limitations. Our proposed methodology was to alternate between interviews and focus groups, which would have enabled the validation of the obtained information. However, due to COVID-19, the focus groups were postponed hoping to conduct them physically and the interviews were conducted first. A second limitation was the need to switch to telephone conversations as opposed to video calls during two interviews and technical problem for two patients during the focus group. As a consequence, information on non-verbal communication was lacking for this small proportion of participants. Two patients dropped out during the focus group and as a result part of their input is missing. Another limitation is that collecting data via focus groups means that findings may not reflect the individual views of participants as they may conform to the perspectives of others in the group (Sim, Citation1998). The researchers did make efforts to ensure that everyone had ample opportunities to express their perspective and four focus groups were held to verify that views co-occurred in the separate focus groups.
The holistic patient profile has been developed based on qualitative information of breast cancer patients and survivors, and HCPs involved in breast cancer related CRF. However, three of the 27 patients appeared to have experienced multiple cancers or had a relapse, and it was expected it would be harder for them to distinguish these situations. However, their comments did not seem to differ from the others. Yet, other patients indicated finding it difficult to distinguish fatigue symptoms from natural ageing, menopause or other complaints. Whether the information the profile is specific for breast cancer or could be extrapolated to other cancer types is an important question for future studies. Lashbrook et al. (Citation2018) indicated that colorectal, prostate, and breast cancer survivors seem to use different coping strategies. In addition, as indicated in the subtheme body, breast cancer can affect femininity. The bodily changes of cancer treatment might be experienced differently by men and also depends on the type of cancer. Taking the above into consideration, the (sub)themes found in this study can be used as a framework but further research is needed to adjust it to other types of cancer and to research contextual differences. This also relates to (post)positivism as the used data-analysis approach. Although different stakeholders were involved, a limitation of the (post)positivism approach is that the results are interpreted as the reality but are contextual depended.
As a first step for future research, the parameters that capture the content of the holistic patient profile should be determined. Consequently, questionnaires, wearables or health apps can be assessed to develop a toolkit that can operationalise these parameters. To allow the toolkit to be used for personalized treatment recommendation and monitoring of CRF over time one needs to keep in mind if the information of the five themes is also informative for the personalized treatment advice. For example, as the NCCN guideline sections about interventions for CRF for patients on active breast cancer or post-treatment lacks treatments focused on personality changes, this could imply that personality will not be operationalized into a holistic questionnaire for the personalized treatment advice (NCCN, Citation2022). In addition, it could be interesting to personalize the holistic patient profile by only showing the relevant themes for the individual patient at that point in time in perpetuating their CRF which could be targeted during treatment for CRF.
Conclusion
A first holistic patient profile was presented for CRF after breast cancer using qualitative data of patients and HCPs. This holistic patient profile consists of the themes experience of CRF, impact and consequences, coping, personality and CRF treatment. In future research, this holistic patient profile can be operationalized to collect the relevant information needed for a personalized treatment recommendation for CRF and monitoring of CRF over time. This has the potential to increase awareness on CRF and reduce the impact of it on the QoL in individuals and the societal impact of fatigue after cancer, by tailoring treatment to patients’ characteristics, needs, capabilities, and preferences.
Ethical approval
Ethical approvals of the study have been given from all relevant bodies: CMO Arnhem-Nijmegen, clinical institutes (University Medical Center Groningen [UMCG], ‘Ziekenhuisgroep Twente’ [ZGT], Helen Dowling Institute [HDI] and Roessingh Rehabilitation Centre), and the University of Twente (Faculty of Electrical Engineering, Mathematics and Computer Science). The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent
Informed consent was obtained from all participants included in the study.
Author contribution
The study was conceptualised by KW, LB, AW, SS, MV and CB and approved by all authors. Participants were approached by ES, CJ, CG, and MS, and included by KW. Interviews were conducted by KW, during focus groups LB assisted. Data analysis was performed by KW, with 10% coding by LB and the coding scheme was discussed with KW, LB, AW, SS, MV and CB. KW drafted and improved the manuscript as all authors critically reviewed the manuscript. Finally, all authors approved the final version of the manuscript.
Supplemental Material
Download Zip (29.5 KB)Acknowledgements
The authors would like to thank everyone who participated in the focus groups and interviews for their input. This research is supported by KWF Kankerbestrijding and NWO Domain AES, as part of their joint strategic research programme: Technology for Oncology ll. The collaboration project is co-funded by the PPP Allowance made available by Health ∼ Holland, Top Sector Life Sciences and Health, to stimulate public-private partnerships.
Disclosure statement
The authors report there are no relevant competing interests to declare.
Data availability
Coding of the focus groups and interviews is available in Dutch and can be requested from the corresponding author.
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Abrahams, H. J. G., Gielissen, M. F. M., Donders, R. R. T., Goedendorp, M. M., van der Wouw, A. J., Verhagen, C. A. H. H. V. M., & Knoop, H. (2017). The efficacy of Internet-based cognitive behavioral therapy for severely fatigued survivors of breast cancer compared with care as usual: A randomized controlled trial. Cancer, 123(19), 3825–3834. https://doi.org/10.1002/cncr.30815
- Abrahams, H. J. G., Gielissen, M. F. M., Schmits, I. C., Verhagen, C. A. H. H. V. M., Rovers, M. M., & Knoop, H. (2016). Risk factors, prevalence, and course of severe fatigue after breast cancer treatment: A meta-analysis involving 12 327 breast cancer survivors. Annals of Oncology, 27(6), 965–974. https://doi.org/10.1093/annonc/mdw099
- Abrahams, H. J. G., Gielissen, M. F. M., Verhagen, C. A. H. H. V. M., & Knoop, H. (2018). The relationship of fatigue in breast cancer survivors with quality of life and factors to address in psychological interventions: A systematic review. Clinical Psychology Review, 63, 1–11. https://doi.org/10.1016/j.cpr.2018.05.004
- Andrykowski, M. A., Schmidt, J. E., Salsman, J. M., Beacham, A. O., & Jacobsen, P. B. (2005). Use of a case definition approach to identify cancer-related fatigue in women undergoing adjuvant therapy for breast cancer. Journal of Clinical Oncology, 23(27), 6613–6622. https://doi.org/10.1200/JCO.2005.07.024
- Beenhakker, L., Witteveen, A., Wijlens, K. A. E., Siemerink, E. J. M., van der Lee, M. L., Bode, C., Siesling, S., & Vollenbroek-Hutten, M. M. R. (2022). Patient preference attributes in eHealth interventions for cancer-related fatigue: A scoping review. European Journal of Cancer Care, 31(6), e13754. https://doi.org/10.1111/ecc.13754
- Bootsma, T. I., Schellekens, M. P. J., Woezik, R. A. M., Lee, M. L., & Slatman, J. (2020). Experiencing and responding to chronic cancer-related fatigue: A meta-ethnography of qualitative research. Psycho-oncology, 29(2), 241–250. https://doi.org/10.1002/pon.5213
- Bower, J. E. (2014). Cancer-related fatigue—mechanisms, risk factors, and treatments. Nature Reviews. Clinical Oncology, 11(10), 597–609. https://doi.org/10.1038/nrclinonc.2014.127
- Bower, J. E., & Ganz, P. A. (2015). Symptoms: Fatigue and cognitive dysfunction. Improving outcomes for breast cancer survivors (pp. 53–75). Breast Cancer Research Foundation 2015. https://doi.org/10.1007/978-3-319-16366-6_5
- Bower, J. E., Wiley, J., Petersen, L., Irwin, M. R., Cole, S. W., & Ganz, P. A. (2018). Fatigue after breast cancer treatment: Biobehavioral predictors of fatigue trajectories. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association, 37(11), 1025–1034. https://doi.org/10.1037/hea0000652
- Braun, V., & Clarke, V. (2019). Reflecting on reflexive thematic analysis. Qualitative Research in Sport, Exercise and Health, 11(4), 589–597. https://doi.org/10.1080/2159676X.2019.1628806
- Braun, V., & Clarke, V. (2021a). Can I use TA? Should I use TA? Should I not use TA? Comparing reflexive thematic analysis and other pattern-based qualitative analytic approaches. Counselling and Psychotherapy Research, 21(1), 37–47. https://doi.org/10.1002/capr.12360
- Braun, V., & Clarke, V. (2021b). Conceptually locating reflexive thematic analysis. Thematic analysis. A Practical Guide.
- Braun, V., & Clarke, V. (2021c). Exploring this world in detail: Doing coding. Thematic analysis. A Practical Guide.
- Braun, V., & Clarke, V. (2021d). One size fits all? What counts as quality practice in (reflexive) thematic analysis? Qualitative Research in Psychology, 18(3), 328–352. https://doi.org/10.1080/14780887.2020.1769238
- Braun, V., & Clarke, V. (2021e). To saturate or not to saturate? Questioning data saturation as a useful concept for thematic analysis and sample-size rationales. Qualitative Research in Sport, Exercise and Health, 13(2), 201–216. https://doi.org/10.1080/2159676X.2019.1704846
- Broeckel, J. A., Jacobsen, P. B., Horton, J., Balducci, L., & Lyman, G. H. (1998). Characteristics and correlates of fatigue after adjuvant chemotherapy for breast cancer. Journal of Clinical Oncology, 16(5), 1689–1696. https://doi.org/10.1200/JCO.1998.16.5.1689
- Buffart, L. M., Galvão, D. A., Brug, J., Chinapaw, M. J. M., & Newton, R. U. (2014). Evidence-based physical activity guidelines for cancer survivors: Current guidelines, knowledge gaps and future research directions. Cancer Treatment Reviews, 40(2), 327–340. https://doi.org/10.1016/j.ctrv.2013.06.007
- Chartogne, M., Rahmani, A., Landry, S., Bourgeois, H., Peyrot, N., & Morel, B. (2021). Neuromuscular, psychological, and sleep predictors of cancer-related fatigue in cancer patients. Clinical Breast Cancer, 21(5), 425–432. https://doi.org/10.1016/j.clbc.2020.12.002
- Cheng, C. T., Ho, S. M. Y., Liu, W. K., Hou, Y. C., Lim, L. C., Gao, S. Y., Chang, W. Y., & Wang, G. L. (2019). Cancer-coping profile predicts long-term psychological functions and quality of life in cancer survivors. Supportive Care in Cancer, 27(3), 933–941. https://doi.org/10.1007/s00520-018-4382-z
- Cillessen, L., van de Ven, M. O., Compen, F. R., Bisseling, E. M., van der Lee, M. L., & Speckens, A. E. (2020). Predictors and effects of usage of an online mindfulness intervention for distressed cancer patients: Usability study. Journal of Medical Internet Research, 22(10), e17526. https://doi.org/10.2196/17526
- Curt, G. A., Breitbart, W., Cella, D., Groopman, J. E., Horning, S. J., Itri, L. M., Johnson, D. H., Miaskowski, C., Scherr, S. L., Portenoy, R. K., & Vogelzang, N. J. (2000). Impact of cancer-related fatigue on the lives of patients: New findings from the fatigue coalition. The Oncologist, 5(5), 353–360. https://doi.org/10.1634/theoncologist.5-5-353
- de Ligt, K. M., Heins, M., Verloop, J., Ezendam, N. P. M., Smorenburg, C. H., Korevaar, J. C., & Siesling, S. (2019). The impact of health symptoms on health-related quality of life in early-stage breast cancer survivors. Breast Cancer Research and Treatment, 178(3), 703–711. https://doi.org/10.1007/s10549-019-05433-3
- de Ligt, K. M., Heins, M., Verloop, J., Smorenburg, C. H., Korevaar, J. C., & Siesling, S. (2019). Patient-reported health problems and healthcare use after treatment for early-stage breast cancer. Breast (Edinburgh, Scotland), 46, 4–11. https://doi.org/10.1016/j.breast.2019.03.010
- Evers, J. (2015). Kwalitatief interviewen: Kunst én kunde (2nd ed.). Boom Lemma.
- Fagundes, C., LeRoy, A., & Karuga, M. (2015). Behavioral symptoms after breast cancer treatment: A biobehavioral approach. Journal of Personalized Medicine, 5(3), 280–295. https://doi.org/10.3390/jpm5030280
- Gielissen, M. F. M., Verhagen, S., Witjes, F., & Bleijenberg, G. (2006). Effects of cognitive behavior therapy in severely fatigued disease-free cancer patients compared with patients waiting for cognitive behavior therapy: A randomized controlled trial. Journal of Clinical Oncology, 24(30), 4882–4887. https://doi.org/10.1200/JCO.2006.06.8270
- Glaus, A., Crow, R., & Hammond, S. (1996). A qualitative study to explore the concept of fatigue/tiredness in cancer patients and in healthy individuals. Supportive Care in Cancer, 4(2), 82–96. https://doi.org/10.1007/BF01845757
- Goedendorp, M. M., Gielissen, M. F. M., Verhagen, C. A. H. H. V. M., & Bleijenberg, G. (2013). Development of fatigue in cancer survivors: A prospective follow-up study from diagnosis into the year after treatment. Journal of Pain and Symptom Management, 45(2), 213–222. https://doi.org/10.1016/j.jpainsymman.2012.02.009
- Heins, M. J., de Ligt, K. M., Verloop, J., Siesling, S., Korevaar, J. C., Berendsen, A., Brandenbarg, D., Dassen, A., Jager, A., Hugtenburg, J., & Weele, G. V D, PSCCR group. (2022). Adverse health effects after breast cancer up to 14 years after diagnosis. Breast (Edinburgh, Scotland), 61, 22–28. https://doi.org/10.1016/j.breast.2021.12.001
- Huber, M., Knottnerus, J. A., Green, L., Horst, H. V D., Jadad, A. R., Kromhout, D., Leonard, B., Lorig, K., Loureiro, M. I., Meer, J. W. M. V D., Schnabel, P., Smith, R., Weel, C. V., & Smid, H. (2011). How should we define health? BMJ, 343(2), d4163–d4163. https://doi.org/10.1136/bmj.d4163
- Joly, F., Lange, M., Dos Santos, M., Vaz-Luis, I., & Di Meglio, A. (2019). Long-term fatigue and cognitive disorders in breast cancer survivors. Cancers, 11(12), 1896. https://doi.org/10.3390/cancers11121896
- Kip, H., Kelders, S. M., Sanderman, R., & van Gemert-Pijnen, L. (2018). eHealth research theory and development. Routledge
- Kuhnt, S., Friedrich, M., Schulte, T., Esser, P., & Hinz, A. (2019). Predictors of fatigue in cancer patients: A longitudinal study. Supportive Care in Cancer, 27(9), 3463–3471. https://doi.org/10.1007/s00520-019-4660-4
- Lashbrook, M. P., Valery, P. C., Knott, V., Kirshbaum, M. N., & Bernardes, C. M. (2018). Coping strategies used by breast, prostate, and colorectal cancer survivors. Cancer Nursing, 41(5), E23–E39. https://doi.org/10.1097/NCC.0000000000000528
- Li, L., Li, S., Wang, Y., Yi, J., Yang, Y., He, J., & Zhu, X. (2017). Coping profiles differentiate psychological adjustment in Chinese women newly diagnosed with breast cancer. Integrative Cancer Therapies, 16(2), 196–204. https://doi.org/10.1177/1534735416646854
- Mitchell, S. A. (2010). Cancer-related fatigue: State of the science. PM & R: The Journal of Injury, Function, and Rehabilitation, 2(5), 364–383. https://doi.org/10.1016/j.pmrj.2010.03.024
- National Comprehensive Cancer Network (NCCN). (2022). Cancer-related fatigue guideline version 1.2022. National Comprehensive Cancer Network (NCCN).
- Netherlands Comprehensive Cancer Organisation (IKNL). (2019). Cancer care in the picture: On living after cancer (Kankerzorg in beeld: Over leven met en na kanker). https://iknl.nl/getmedia/a5d364d2-7b5b-40d2-9e0d-2ffb8efd2590/kankerzorg-in-beeld-over-leven-met-en-na-kanker-verdiepende-informatie.pdf
- Paalman, C. H., van Leeuwen, F. E., Aaronson, N. K., de Boer, A. G. E. M., van de Poll-Franse, L., Oldenburg, H. S. A., & Schaapveld, M. (2016). Employment and social benefits up to 10 years after breast cancer diagnosis: A population-based study. British Journal of Cancer, 114(1), 81–87. https://doi.org/10.1038/bjc.2015.431
- Penner, C., Zimmerman, C., Conboy, L., Kaptchuk, T., & Kerr, C. (2020). “Honorable toward your whole self”: Experiences of the body in fatigued breast cancer survivors. Frontiers in Psychology, 11, 1502. https://doi.org/10.3389/fpsyg.2020.01502
- Person, H., Guillemin, F., Conroy, T., Velten, M., & Rotonda, C. (2020). Factors of the evolution of fatigue dimensions in patients with breast cancer during the 2 years after surgery. International Journal of Cancer, 146(7), 1827–1835. https://doi.org/10.1002/ijc.32527
- Prue, G., Rankin, J., Allen, J., Gracey, J., & Cramp, F. (2006). Cancer-related fatigue: A critical appraisal. European Journal of Cancer (Oxford, England: 1990), 42(7), 846–863. https://doi.org/10.1016/j.ejca.2005.11.026
- Puigpinós-Riera, R., Serral, G., Sala, M., Bargalló, X., Quintana, M. J., Espinosa, M., Manzanera, R., Doménech, M., Macià, F., Grau, J., & Vidal, E. (2020). Cancer-related fatigue and its determinants in a cohort of women with breast cancer: The DAMA Cohort. Supportive Care in Cancer, 28(11), 5213–5221. https://doi.org/10.1007/s00520-020-05337-9
- Schaab, M., Wijlens, K. A. E., & Bode, C. (2023). Psychological coping factors associated with breast cancer-related fatigue: A systematic review of recent evidence for stages 0 to III. Clinical Breast Cancer, 23(7), e401–e411. https://doi.org/10.1016/j.clbc.2023.06.005
- Schellekens, M. P. J., Wolvers, M. D. J., Schroevers, M. J., Bootsma, T. I., Cramer, A. O. J., & van der Lee, M. L. (2019). Exploring the interconnectedness of fatigue, depression, anxiety and potential risk and protective factors in cancer patients: A network approach. Journal of Behavioral Medicine, 43(4), 553–563. https://doi.org/10.1007/s10865-019-00084-7
- Schmidt, M. E., Chang-Claude, J., Vrieling, A., Heinz, J., Flesch-Janys, D., & Steindorf, K. (2012). Fatigue and quality of life in breast cancer survivors: Temporal courses and long-term pattern. Journal of Cancer Survivorship: Research and Practice, 6(1), 11–19. https://doi.org/10.1007/s11764-011-0197-3
- Schmidt, M. E., Wiskemann, J., Schneeweiss, A., Potthoff, K., Ulrich, C. M., & Steindorf, K. (2018). Determinants of physical, affective, and cognitive fatigue during breast cancer therapy and 12 months follow-up. International Journal of Cancer, 142(6), 1148–1157. https://doi.org/10.1002/ijc.31138
- Servaes, P., Verhagen, C., & Bleijenberg, G. (2002a). Fatigue in cancer patients during and after treatment. European Journal of Cancer (Oxford, England: 1990), 38(1), 27–43. https://doi.org/10.1016/S0959-8049(01)00332-X
- Servaes, P., Verhagen, S., & Bleijenberg, G. (2002b). Determinants of chronic fatigue in disease-free breast cancer patients: A cross-sectional study. Annals of Oncology, 13(4), 589–598. https://doi.org/10.1093/annonc/mdf082
- Sim, J. (1998). Collecting and analysing qualitative data: Issues raised by the focus group. Journal of Advanced Nursing, 28(2), 345–352. https://doi.org/10.1046/j.1365-2648.1998.00692.x
- Thong, M. S. Y., van Noorden, C. J. F., Steindorf, K., & Arndt, V. (2020). Cancer-related fatigue: Causes and current treatment options. Current Treatment Options in Oncology, 21(2), 17. https://doi.org/10.1007/s11864-020-0707-5
- Tong, A., Sainsbury, P., & Craig, J. (2007). Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care: Journal of the International Society for Quality in Health Care, 19(6), 349–357. https://doi.org/10.1093/intqhc/mzm042
- Wasmann, K. A., Wijsman, P., van Dieren, S., Bemelman, W., & Buskens, C. (2019). Partially randomised patient preference trials as an alternative design to randomised controlled trials: Systematic review and meta-analyses. BMJ Open, 9(10), e031151. https://doi.org/10.1136/bmjopen-2019-031151
- Young, K. E., & White, C. A. (2006). The prevalence and moderators of fatigue in people who have been successfully treated for cancer. Journal of Psychosomatic Research, 60(1), 29–38. https://doi.org/10.1016/j.jpsychores.2005.03.011
- Zamanzadeh, V., Jasemi, M., Valizadeh, L., Keogh, B., & Taleghani, F. (2015). Effective factors in providing holistic care: A qualitative study. Indian Journal of Palliative Care, 21(2), 214. https://doi.org/10.4103/0973-1075.156506

