ABSTRACT
With the popularization of percutaneous coronary intervention technology in clinical applications, the mortality rate of acute myocardial infarction has been significantly reduced. However, ventricular remodeling following myocardial infarction (MI) has attracted extensive attention for that it can cause malignant arrhythmia, heart failure, and even death. We aimed to investigate the effects of ginsenoside Rg2 on cardiac function and myocardial fibrosis after MI and its potential mechanism. The results demonstrated that ginsenoside Rg2 improved cardiac function and inhibited collagen deposition in mice after MI. In addition, ginsenoside Rg2 reduced the levels of fibrosis-associated genes Collagen I (Col 1), Collagen III (Col 3), and alpha-smooth muscle actin (α-SMA) by activating phosphorylated AKT in angiotensin II–induced cardiac fibroblasts. Taken together, ginsenoside Rg2 improves cardiac function and attenuates cardiac fibrosis via the AKT pathway, suggesting that ginsenoside Rg2 may be a promising drug for the prevention of ventricular remodeling after MI.
Abbreviations: MI: myocardial infarction; AMI: acute myocardial infarction; LAD: left anterior descending; ECM: extracellular matrix; Col 1: collagen I; Col 3: collagen III; α-SMA: alpha-smooth muscle actin; ROS: reactive oxygen species; SOD: superoxide dismutase; GSH: glutathione; HO-1: heme oxygenase-1; WST8: water-soluble tetrazolium salt 8.
Graphical abstract
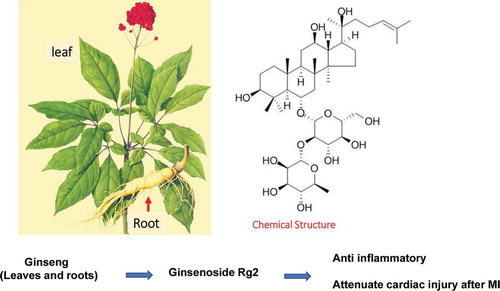
Rg2 is the main active component extracted from the leaves and roots of ginseng, which can attenuate the heart injury and improve the cardiac repair after MI.
Coronary heart disease, particularly acute myocardial infarction (AMI), is one of the leading causes of mortality worldwide, and its incidence has been increasing in recent years [Citation1]. The replacement of necrotic myocardium with scar tissue after myocardial infarction (MI), an increase in fibroblast proliferation after MI, a disorder in extracellular matrix (ECM) secretion, and numerous other factors can cause ventricular remodeling, which eventually develops into malignant arrhythmia, heart failure, and even death [Citation2,Citation3]. Therefore, inhibiting ventricular remodeling following MI, preventing or reducing infarct size, and delaying the occurrence of heart failure are keys to improve the survival rate and quality of life of patients [Citation4]. Although there have been a number of studies on the mechanism of ventricular remodeling after MI, the molecular mechanism remains unclear, and further research and the development of effective new drugs are required.
Ventricular remodeling involves a variety of factors, among which changes in the content and composition of cardiac ECM are an important cause of ventricular remodeling [Citation5,Citation6]. After MI, myocardial interstitial fibroblasts proliferate significantly in the infarcted and marginal areas, and the secretion of Col 1, Col 3, and α-SMA increases markedly, which can cause excessive collagen deposition and aggravate myocardial fibrosis [Citation6,Citation7]. Therefore, how to successfully regulate the proliferation and differentiation of myocardial fibroblasts and maintain the balance of ECM to inhibit the process of myocardial fibrosis has become a critical factor to improve the prognosis of MI.
Ginseng saponins, such as panax ginseng and panax notoginseng, are the main active ingredients of acanthopanaceae plants [Citation8]. According to the different chemical structures, ginseng saponins are divided into different species, and it has been reported that different components have differential effects on the body [Citation9]. At present, the compound preparation of ginseng has been widely used in the treatment of heart diseases in China [Citation10]. Rg2, as one of the main components of ginsenoside, has shown obvious antiapoptotic and anti-inflammatory effects in numerous diseases [Citation11,Citation12]. In addition, previous studies have demonstrated that Rg2 can regulate the AKT and mitogen-activated protein kinase (MAPK) pathways [Citation13,Citation14]. However, the role of Rg2 in cardiac function and ventricular remodeling following MI and its underlying mechanism remain unclear.
The present study constructed a mouse model of MI to study the effect of Rg2 on fibrosis and cardiac function after acute MI and investigated its potential mechanism, providing a potential new treatment for preventing ventricular remodeling after MI.
Materials and methods
Reagents
Rg2 standards (purity >95%) were purchased from Chengdu Sikehua Biotechnology Co., Ltd., and were dissolved in 50% aqueous methanol to obtain a stock solution for further investigations.
Cell isolation and culture
Neonatal rat cardiac fibroblasts (NRCFs) were isolated from 1–2-day-old Sprague-Dawley rats purchased from Cavens Lab Animal (Changzhou, China) (age, 1–3 days; weight, 5–6 g) and prepared as previously described [Citation15]. NRCFs were cultured in Dulbecco’s modified Eagle’s medium (DMEM; Gibco, USA) supplemented with 10% fetal bovine serum (Sciencell Research Laboratories, USA) and 1% penicillin–streptomycin at 37°C with 5% CO2.
Hypoxia treatment
Prior to hypoxia treatment, NRCFs were cultured with serum-free no-glucose DMEM (Gibco) in an airtight chamber with a humidified hypoxic atmosphere containing 5% CO2 and 95% N2 at 37°C. Twelve hours later, NRCFs were exposed to further experiments.
Cell treatment
To determine an effective concentration of Rg2, NRCFs were exposed to different concentrations (1, 2, 5, 10, 20, 50, 100, and 200 μM) of Rg2 for 24 h, followed by hypoxia treatment for 12 h. To investigate if Rg2 could perform a beneficial effect on inhibiting cardiac fibrosis, NRCFs were exposed to Ang II stimulation (10−7 mol/L) in the presence or absence of Rg2 (10 μM) treatment. To confirm how Rg2 exhibited its effect, AKT inhibitor MK2206 (1 μM) (Selleck, USA) was exposed to NRCFs together with Rg2 treatment.
Animal experiments
All animal care and experimental procedures were in accordance with the Guidelines for the Care and Use of Laboratory Animals (US National Institutes of Health). Protocols were approved by the Committee on Animal Care of Affiliated Hospital of Guizhou Medical University (Guiyang, China). Totally, 37 male mice (aged, 8 weeks) were purchased from Beijing Vital River Laboratory Animal Technology Co., Ltd. Mice were randomly divided into three groups: (i) Sham group (n = 7); (ii) MI group (n = 15); and (iii) MI+Rg2 group (n = 15). MI surgery was performed using left anterior descending (LAD) ligation, and the sham operation involved the same procedure except that a suture was passed under the LAD coronary artery without ligation. Rg2 or saline was given to mice once a day via intragastric administration at a dose of 0.5 g/(kg. d) for 4 weeks from day 1 after MI surgery. The mice were then exposed to associated examination.
Echocardiography
A total of 4 days after the operation, 2% isoflurane was used to induce anesthetization, and an echocardiography was performed using Vevo2100 (Visual Sonics) to examine the cardiac function of mice, including the ejection fraction, fractional shortening, left ventricular internal dimension (LVID) diastolic, and LVID systolic.
2,3,5-Triphenyltetrazolium chloride (TTC) staining
To investigate if Rg2 has a beneficial effect on attenuating infarct size, TTC staining was used to measure infarct size at 24 h after MI surgery. Evans blue (1%) was slowly injected into the left ventricle and the hearts were stained with TTC. The area at risk/left ventricle weight ratio and the infarct size/area at risk ratio were determined to evaluate the homogeneity of surgery and the severity of cardiac MI injury, respectively.
Masson staining
After mice were sacrificed, Masson staining was used to evaluate cardiac fibrosis as previously described [Citation16]. Briefly, the hearts were harvested at the end of the experiment, fixed in 4% paraformaldehyde, and cut into parasternal short-axis sections (thickness, 4 μm). The sections were then stained with Masson Trichrome kit (Sigma-Aldrich, Darmstadt, Germany) according to the manufacturer’s instructions. Images of the slides were captured and analyzed with a Carl Zeiss Axioskop microscope (Carl Zeiss AG, Germany). The area of cardiac fibrosis (blue collagen staining for scar tissue) was expressed as a percentage of the left ventricular surface area.
Cell Counting Kit-8 (CCK8) assay
Cell viability was detected using a CCK8 assay. Briefly, NRCFs were cultured in a 96-well plate and cultured in an incubator at 37°C, with 5% CO2. CCK8 assay solution (10 µL) contained water-soluble tetrazolium salt (WST-8) was then added to each well following Rg2 treatment and the cells were incubated for 2 h. The optical density of each well was measured using a microplate reader (Thermo Fisher Scientific, Inc.) at 450 nm.
Reverse transcription-quantitative polymerase chain reaction (RT-qPCR) analysis
Total RNA was extracted using TRIzol (Invitrogen, USA). cDNA was synthesized by RT from 400 ng total RNA using the Oligo(dT) priming method (Takara, Japan) according to the manufacturer’s protocol. qPCR was then performed using SYBR Green qPCR Master mix (Bio-Rad, USA). The mRNA expression was normalized to GAPDH. The 2−ΔΔCT method was used to determine the relative expression levels. Primers used inexperiments were showed in .
Table 1. List of primers used for qRT-PCR.
Western blot analysis
Total protein was extracted and quantified. The protein (30 µg/lane) was then separated by 12% Sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) gels and transferred to Polyvinylidene fluoride (PVDF) membranes. Primary antibodies against Col 1, Col 3, α-SMA, AKT, p-AKT473, p-AKT308, p-ERK, ERK, p-P38, P38, p-JNK, and JNK were used in the experiment, and GAPDH was used as a loading control.
Statistical analysis
All data are presented as the mean ± standard deviation. One-way Analysis of Variance (ANOVA) followed by Bonferroni’s post-hoc test was used for multiple comparisons using GraphPad Prism 7.0 (GraphPad Prism, Inc.). P < 0.05 was considered to indicate a statistically significant difference.
Results
Selection of the hypoxia time point and optimal Rg2 concentration for the in vitro model
Hypoxia exposure induced significant cell death in a time-dependent manner (), and 12 h was selected as the time point to stimulate cardiac fibroblast death. The effect of Rg2 on cell viability is presented in ; CCK8 assay results demonstrated that Rg2 exhibited no significant cytotoxic effect at concentrations up to 20 μM after 24 h of treatment. Furthermore, NRCFs were treated with different concentrations of Rg2, followed by hypoxia for 12 h. It was identified that 10 μM Rg2 significantly improved cardiomyocyte cell viability induced by hypoxia (). Based on these results, 10 μM was selected as the experimental concentration for in vitro experiments.
Figure 1. Rg2 decreases hypoxia-induced cardiac fibroblast death. (a) As hypoxia prolonged, cell viability decreased more seriously (n = 6). (b) Cardiac fibroblast was treated with Rg2 with different concentrations, and Rg2 over 10 μM induced cell death (n = 6). (c) Rg2 at 10 μM decreased hypoxia-induced cell death (n = 6). *P < 0.05; **P < 0.01; ***P < 0.001 versus respective control.

Rg2 downregulates fibrosis-associated genes and increases p-AKT expression in Ang II–induced cardiac fibroblasts
RT-qPCR and Western blot analyses were conducted to investigate the effect of Rg2 on the expression of fibrosis-related genes Col-1, Col-3, and α-SMA. It was identified that the expression levels of Col-1, Col-3, and α-SMA were markedly increased in Ang II–induced NRCFs and were inhibited by treatment with Rg2 (-). To further investigate the potential pathways involved in the inhibitory role of Rg2 on Ang II–induced fibrosis, the AKT and MAPK pathways were investigated, which are widely involved in the process of MI injury (-). The Western blot analysis demonstrated that Ang II could significantly reduce the expression of p-AKT, which was inhibited by treatment with Rg2. By contrast, Rg2 had no significant effect on the Ang II–induced MAPK pathway.
Figure 2. Rg2 downregulates Ang II–induced fibrosis-related genes in cardiac fibroblasts. (a) RT-PCR analysis indicated Rg2 decreased expression of fibrosis-related genes in mRNA level (n = 6). (b) Western blot analysis proved Rg2 decreased expression of fibrosis-related genes in protein level (n = 3). *P < 0.05; **P < 0.01 versus respective control.

Rg2 inhibits Ang II–induced expression of collagen-related genes by activating the AKT pathway
To confirm whether the AKT pathway regulates the inhibitory role of Rg2 on Ang II–induced fibrosis, the AKT inhibitor of MK2206 was first used to reduce the expression of p-AKT473 and p-AKT308 (). Subsequently, RT-qPCR and Western blotting demonstrated that the suppressive role of Rg2 on Ang II–induced collagen-related genes of Col I, Col 3, and a-SMA expression in NRCFs was partially reversed by p-AKT inhibitor (-c). The present results demonstrated that Ang II–induced fibrosis gene expression in NRCFs was attenuated by Rg2 via the AKT pathway.
Figure 4. AKT inhibitor MK2206 abrogates effect of Rg2 in cardiac fibroblasts. (a) MK2206 inhibited phosphorylation of AKT activated by Rg2 (n = 3). (b–c) MK2206 eliminated protective effect of Rg2 on inhibiting fibrosis-related genes in mRNA level (n = 6) and in protein level (n = 3). *P < 0.05; **P < 0.01; ***P < 0.001 versus respective control.

Rg2 improves cardiac function and inhibits cardiac fibrosis in mice after MI
The present study first investigated the role of Rg2 on cardiac function and myocardial fibrosis in mice after MI. Compared with the sham group, the left ventricle ejection fraction and fractional shortening in MI mice were significantly impaired. However, Rg2 significantly protected cardiac functions of MI-induced mice (). However, it demonstrated no effect on infarct size at 24 h after MI injury (). This suggests that Rg2 may not exhibit an effect at the acute injury stage. We also found that compared with the mice in the MI group, the survival rate of mice in the Rg2 treatment group was significantly improved (). In addition, the Masson staining assay revealed that Rg2 markedly reduced MI-induced cardiac fibrosis in mice (). Western blot analysis also demonstrated that Rg2 decreased MI-induced collagen deposition in mice (). Apart from cardiac fibrosis, Rg2 also exhibited beneficial effects on attenuating inflammation and reactive oxygen species (ROS) activation (-c). Since previous studies have shown that Rg2 can regulate AKT expression [Citation13], the present study demonstrated that Rg2 could increase AKT (Ser473 and Thr308) phosphorylation, which was inhibited by MI in vivo (). These data indicate that Rg2 improves the cardiac function and decreases the myocardial fibrosis of MI-induced mice.
Figure 5. Rg2 suppresses cardiac function and myocardial fibrosis in mice after MI surgery. (a) Echocardiography indicated Rg2 increased cardiac function of mice (n = 6). (b) Rg2 had no effect on infarct size at 24 h after MI (n = 6). (c) Rg2 improved survival rate of MI mice during treatment stage. (d) Masson staining indicated Rg2 decreased MI-induced fibrosis (n = 6), scale bar = 20 μm. AAR: area at risk; INF: infarct size. *P < 0.05; **P < 0.01; ***P < 0.001 versus respective control.

Figure 6. Rg2 inhibits MI-induced collagen deposition and inflammation and improves ROS activation. (a) Rg2 attenuated MI-induced collagen deposition via RT-PCR analysis (n = 6) and Western blot analysis (n = 3). (b–c) RT-PCR analysis indicated Rg2 attenuated MI-induced inflammation and improved ROS activation (n = 6). (d) Rg2 activated AKT signaling pathway in vivo (n = 3). *P < 0.05; **P < 0.01; ***P < 0.001 versus respective control.

Discussion
In recent years, with the wide application of percutaneous coronary intervention technology in AMI, the mortality rate of AMI has decreased significantly [Citation17]. However, the long-term malignant events caused by ventricular remodeling following MI are particularly prominent. Ventricular remodeling involves numerous factors, including cardiomyocyte hypertrophy, apoptosis, and changes in ECM volume and composition [Citation18]. In particular, changes in ECM can initiate ventricular remodeling that leads to myocardial fibrosis and an imbalance of collagen ratios, which will eventually lead to heart failure, directly affecting the quality of life and prognosis of patients [Citation18,Citation19]. A number of studies worldwide are investigating how to better inhibit myocardial fibrosis after MI and prevent the occurrence of heart failure following ventricular remodeling [Citation4].
Ginsenoside is the most active pharmacological ingredient extracted from ginseng rhizome, which is used in a number of clinical diseases [Citation20]. The monomer components of ginsenosides have attracted attention from numerous researchers, particularly in regards to their antiapoptotic, anti-oxidative stress and anti-inflammatory effects [Citation21]. In addition, using in vivo and in vitro models of MI, previous studies have identified that ginsenosides can significantly reduce the damage to myocardial cells induced by MI [Citation12]. A previous study also confirmed that ginsenoside Rg2 can alleviate oxygen–glucose deprivation and reperfusion-induced injury of the nervous system [Citation11]. The present study identified that ginsenoside Rg2 can significantly improve the recovery of cardiac function following MI in mice and reduce the occurrence of myocardial fibrosis. Although Rg2 improved MI-induced cardiac injury and increased the survival rate after MI, the sample size of our in vivo experiments is limited, so it is necessary to expand the sample size to further investigate if Rg2 could beneficially decrease death rate in vivo. In addition, both in vivo and in vitro experiments revealed that Rg2 could significantly inhibit AMI-induced expression of Col 1, Col 3, and α-SMA. These results indicate that ginsenoside Rg2 has an obvious effect on inhibiting cardiac fibrosis after MI.
Previous studies have reported that the AKT and MAPK pathways are involved in the development of MI. The AKT pathway, including phosphorylation of Ser473 and Thr308 sites, was significantly inhibited and the MAPK pathway was significantly activated after MI [Citation22]. Studies have also demonstrated that ginsenoside Rg2 can regulate the AKT and MAPK pathways in other disease models [Citation13]. The present study identified that ginsenoside Rg2 could significantly increase the level of p-AKT (Ser437 and Thr308) inhibited by MI but had no effect on the AMI-induced MAPK pathway. After further use of AKT inhibitors, the effect of Rg2 on the MI-induced expression levels of ECM-associated molecules was partially blocked. In our study, we found that Rg2 could reduce MI-induced cardiac injury by increasing the expression of AKT 473 and 308 phosphorylation sites. It is not clear which other genes of the Akt pathway are involved in the process of Rg2 inhibiting MI injury. Therefore, it is necessary to explore the potential genes of AKT upstream and downstream which mediated in the role of Rg2 on MI injury in future.
In conclusion, the present study confirmed that Rg2 can alleviate myocardial fibrosis and promote the recovery of cardiac function in mice after MI by activating the AKT pathway. However, whether Rg2 can inhibit MI-induced fibrosis by regulating signaling pathways other than the AKT pathway remains unknown. This will be further investigated in future studies.
Author contribution
X.L. performed the in vitro experiments, analyze the data, and wrote the manuscript. N.X. performed the in vivo experiments. Z.W. (corresponding authors) conceived and supervised the study and performed manuscript editing.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Verma SK. Updated cardiac concerns with rituximab use: a growing challenge. Indian Heart J. 2016;68(Suppl 2):S246–S248.
- Christia P, Frangogiannis NG. Targeting inflammatory pathways in myocardial infarction. Eur J Clin Invest. 2013;43:986–995.
- Galvez-Monton C, Prat-Vidal C, Roura S, et al. Post-infarction scar coverage using a pericardial-derived vascular adipose flap. Pre-clinical results. Int J Cardiol. 2013;166:469–474.
- Chistiakov DA, Orekhov AN, Bobryshev YV. The role of cardiac fibroblasts in post-myocardial heart tissue repair. Exp Mol Pathol. 2016;101:231–240.
- Suncion VY, Schulman IH, Hare JM. Concise review: the role of clinical trials in deciphering mechanisms of action of cardiac cell-based therapy. Stem Cells Transl Med. 2012;1:29–35.
- Kurabayashi M. [Inhibitor of left ventricular remodeling]. Nihon Rinsho. 2011;69(Suppl 9):246–251.
- Sano M, Fukuda K. [Metabolic remodeling in the ischemic and non-ischemic failing heart]. Nihon Rinsho. 2011;69(Suppl 7):60–68.
- Yuan CS, Wang CZ, Wicks SM, et al. chemical and pharmacological studies of saponins with a focus on American ginseng. J Ginseng Res. 2010;34:160–167.
- Li XD, Wang JS, Chang B, et al. Panax notoginseng saponins promotes proliferation and osteogenic differentiation of rat bone marrow stromal cells. J Ethnopharmacol. 2011;134:268–274.
- Zeng P, Li J, Chen Y. The structures and biological functions of polysaccharides from traditional Chinese herbs. Prog Mol Biol Transl Sci. 2019;163:423–444.
- Pi MS, Ru Q, Gong XK, et al. [Effect of ginsenoside Rg2 and its stereoisomers on oxygen-glucose deprivation and reperfusion induced cortical neuronal injury model]. Zhongguo Zhong Xi Yi Jie He Za Zhi. 2016;36:333–338.
- Fu W, Sui D, Yu X, et al. Protective effects of ginsenoside Rg2 against H2O2-induced injury and apoptosis in H9c2 cells. Int J Clin Exp Med. 2015;8:19938–19947.
- Cui J, Wang J, Zheng M, et al. Ginsenoside Rg2 protects PC12 cells against beta-amyloid25-35-induced apoptosis via the phosphoinositide 3-kinase/Akt pathway. Chem Biol Interact. 2017;275:152–161.
- Cho YS, Kim CH, Ha TS, et al. Ginsenoside rg2 inhibits lipopolysaccharide-induced adhesion molecule expression in human umbilical vein endothelial cell. Korean J Physiol Pharmacol. 2013;17:133–137.
- Song J, Zhu Y, Li J, et al. Pellino1-mediated TGF-beta1 synthesis contributes to mechanical stress induced cardiac fibroblast activation. J Mol Cell Cardiol. 2015;79:145–156.
- Issa ZF. My approach to the patient with ventricular arrhythmia and no structural heart disease. Trends Cardiovasc Med. 2019;29:190.
- Yang HY, Ahn MJ, Jeong MH, et al. Korea acute myocardial infarction registry I: predictors of in-hospital mortality in Korean patients with acute myocardial infarction. Chonnam Med J. 2019;55:40–46.
- Gorman RC, Jackson BM. The potential role of ventricular compressive therapy. Surg Clin North Am. 2004;84:45–59.
- Riaz S, Zeidan A. Myocardial proteases and cardiac remodeling. J Cell Physiol. 2017;232:3244–3250.
- Nabavi SF, Sureda A, Habtemariam S. Ginsenoside Rd and ischemic stroke; a short review of literatures. J Ginseng Res. 2015;39:299–303.
- Liu JF, Yan XD, Qi LS, et al. Ginsenoside Rd attenuates Abeta25-35-induced oxidative stress and apoptosis in primary cultured hippocampal neurons. Chem Biol Interact. 2015;239:12–18.
- Simonis G, Wiedemann S, Joachim D, et al. Stimulation of adenosine A2b receptors blocks apoptosis in the non-infarcted myocardium even when administered after the onset of infarction. Mol Cell Biochem. 2009;328:119–126.

