ABSTRACT
Background
The effect of an intervention based on Mediterranean diet on reducing recurrence risk or subsyndromal depressive symptoms in recovered depressed patients has not been explored.
Methods
The PREDIDEP study was a two-year randomized trial designed to assess the effect of the Mediterranean Diet enriched with extra virgin olive oil on depression recurrence. At baseline and at four, eight, 16, 20, and 24 months of follow-up, depressive symptoms were evaluated through the Beck Depression inventory. Cox regression analysis was fitted to assess the role of dietary intervention on the risk of depression recurrence. Mixed effects linear models were used to assess changes in depressive subsyndromal symptoms according to the intervention.
Results:
After two years of intervention, the dietary intervention group (n = 103) compared to the control group (n = 93) showed no differences regarding depression recurrence risk as main outcome. As secondary outcomes, an improvement of depressive symptoms was yielded at four (−2.15; 95% CI = −4.00 to −0.29) and eight months (−2.42; 95% CI = −4.17 to −0.67) in the intervention group, with no changes in control group. Moreover, at 20 months, significant differences were found between groups (−3.35; 95% CI = −6.08 to −0.61).
Conclusions:
An intervention with Mediterranean diet in patients with previous depressive episodes might contribute to the reduction of depressive subsyndromal symptoms.
Introduction
Unipolar depression is a growing global Public Health challenge. It is a common worldwide mental disorder which could appear at short ages (even in three-year-old children) [Citation1]. Depression prevalence is estimated at five percent, this value is even higher when evaluating subcases. Lifetime prevalence is around 17% [Citation2], with some differences between countries in Europe (ranging from 8.8 to 23.6%). Depression is one of the leading global causes of quality of life impairment measured in disability-adjusted life years (DALYs) and Years Lived with Disability (YLD) [Citation3].
Mediterranean diet is currently considered one of the healthiest dietary models worldwide [Citation4]. This dietary pattern is a modifiable lifestyle factor which might influence the onset, development, and prognosis of depression. In fact, several observational studies have described a relationship between high adherence to Mediterranean diet and a lower depression risk [Citation5–11]. Moreover, short-term field trials have also showed similar results for depression treatment [Citation12–15].
Preventing depression recurrence is one of the main objectives in the management of patients with unipolar depression. Moreover, as the number of relapses is higher, the recurrence rate increases, ranging from a percentage of 40–60% in patients who have suffered a single episode to values up to 90% for those with three previous episodes. In addition to the number of previous episodes, depressive residual or subsyndromal symptoms that persist after remission are another important predictor of relapse. In this context, to our knowledge, the role of a dietary intervention based on Mediterranean diet in the risk of depression recurrence or in changes in subsyndromal symptoms in patients recovered from depression has not been evaluated yet. Only a prospective cohort study, not a randomized clinical trial, has reported that long-term adherence to a healthy diet defined by Alternative Healthy Eating Index-2010, but not Mediterranean diet, could confer protection against recurrent depressive symptoms [Citation16].
The principal objective of this study was to assess the effect of two-year intervention with Mediterranean diet enriched with extravirgin olive oil (EVOO), in addition to usual care, on reducing the risk of recurrence and improving depressive subsyndromal symptoms in recovered depressed patients.
Material and methods
Study population
The PREDIDEP study was a multicentre, randomized, controlled, single-blind trial. The study design and methodology have been described previously in detail elsewhere [Citation17]. Briefly, the aim of the PREDIDEP study was to analyse the effect of a Mediterranean diet intervention enriched with EVOO in addition to usual care, compared to usual care without nutritional intervention (control group) in the prevention of recurrence of depression. Study participants were randomly assigned to one of two groups (Mediterranean diet or control) once their data were included in a centralized data management system by the specialists. Various stratification factors were considered for the randomization, sex, age group (<65 years or ≥65 years), and recruitment centre. At baseline, psychiatrists and clinical psychologists were blinded to the allocation of the participants, following the CONSORT guidelines for randomized trials to prevent selection biases. Originally, the trial included another arm with a Mediterranean intervention supplemented with tree nuts that finally was not considered because of a budget adjustment.
The PREDIDEP study included 52 men and 144 women between 18 and 86 years old who had suffered at least one depression episode within the last five years and who were in a stage of total or partial clinical remission in the last six months, based on DSM-5 criteria. We excluded participants with the presence of comorbid psychiatric disorders or severe medical conditions as well as participants with a history of food allergies. Moreover, institutionalized patients or without autonomy were excluded from the trial. Four centres across Spain participated in recruiting participants: Hospital Dr Negrín (Las Palmas de Gran Canaria), Clínica Universidad de Navarra (Pamplona), Hospital Universitario (Vitoria), and Clinica Dr Chiclana (Madrid).
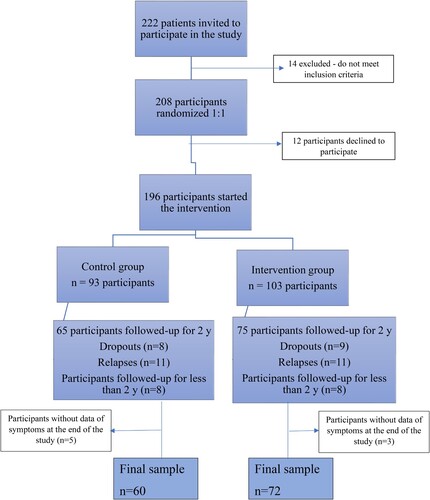
The flowchart () shows participants who completed two-year follow-up. Between March 2017 and December 2020, 222 patients were invited to participate in the study. Of them, although 208 patients were recruited and randomized, 196 started the intervention. The number of dropouts was 17. Thus, the retention rate was 91.3% after 2 years of follow-up (179/196), similar for both groups.
The main analysis of this trial included 196 participants who started the intervention to analyse the effect of the Mediterranean Diet enriched with extra virgin olive oil on depression recurrence. In a secondary analysis, we included all participants who had already been followed up for at least two years and had successfully fulfilled the overall information about depressive symptoms collected in Beck depression inventories at four, eight, 16, 20, and 24 months (n = 91) ().
All procedures contributing to this work complied with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. The Research Ethics Committees at each recruitment centre approved the protocol (date 06/21/2016). All participants provided written informed consent after they received the information sheet and an additional verbal explanation of the study characteristics.
Exposure assessment
The aim of the nutritional intervention of the PREDIDEP study was to analyse the effect of a Mediterranean diet intervention enriched with EVOO in addition to usual care, compared to usual care without nutritional intervention (control group) in the prevention of recurrence of depression. In the PREDIDEP study, we used a remote nutritional intervention rather than an in-person approach. This remote intervention was conducted by a team of registered dietitians by phone and on the internet, and participants had access to web-based information on a website and printed materials. Beyond usual clinical care and dietary intervention, each participant in the intervention group also received EVOO for free (1 litre per week). Participants in the control group received usual clinical care. The nutritional intervention has been described previously in detail elsewhere [Citation17].
Adherence to the traditional Mediterranean diet was also appraised by a validated 14-item MEDAS questionnaire at baseline and every three months in the intervention group and yearly in the control group. The MEDAS questionnaire is a Spanish-validated questionnaire that consists of 14 items that include 12 questions about the frequency of food intake (olive oil, vegetables, fruit, red meat, animal fats, carbonated beverages, red wine, fish/seafood, nuts, commercial food, and sofrito) (a traditional condiment with tomato sauce, garlic, onion, etc.) and two questions about the preferred cooking fat used and meat consumed. Each item is scored as zero or one, and the final score is the sum of each (0–14). The MEDAS scores were categorized as low adherence (<9) and high adherence to the Mediterranean dietary pattern (≥9) [Citation18,Citation19].
Finally, changes in Mediterranean diet adherence through the first year of follow-up were measured as low-maintained adherence, increased adherence (from low to high by MEDAS), decreased adherence (from high to low) and high-maintained adherence after one year of follow-up.
Outcome assessment
Depression recurrence was assessed by psychiatrists and clinical psychologists through clinical evaluations (semi-structured clinical interviews: Spanish SCID-I).
The subsyndromal depressive symptoms are described as presence of moderate affective symptoms but without meeting diagnostic criteria for major depression. Although the Montgomery-Asberg Depression Rating Scale (MADRS) was originally proposed to assess changes in subsyndromal symptoms, finally MADRS was not used because this scale is affected by inter-evaluator differences. As this study is a multicentre clinical trial based on participants from different regions in Spain and in order to avoid a differential misclassification bias in outcome assessment carried out by the psychiatrists, we decided to use BDI and not MADRS to assess depressive symptoms. Thus, subsyndromal depressive symptoms were evaluated at baseline and every four months by phone with the validated Spanish version of The Beck Depression Inventory (BDI) [Citation20].
The BDI is a 21-item, multiple-choice self-report inventory. Respondents are asked to rate each item based on four response choices according to the severity of the symptoms, ranging from the absence of a symptom to an intense level during the past week. The 21 symptoms and attitudes contained in the BDI reflect the intensity of depression; items receive a rating of zero to three to reflect their intensity and are summed linearly to create a score which ranges from zero to 63. The BDI is interpreted using cut-off points: scores from zero through 9 indicate none or minimal depression; scores from 10 through 18 indicate mild to moderate depression; scores from 19 through 29 indicate moderate to severe depression; and scores from 30 through 63 indicate severe depression.
Baseline and yearly depressive symptoms were evaluated by psychiatrists and psychologists through the BDI and a clinical interview. At baseline, eight individuals showed BDI scores >18, but they were included in the trial after the specialists ruled out any current depressive episode. It is important to mention that many of the participants were not evaluated by specialists after 12 months of intervention because this period temporally coincided with COVID-19 lockdown in Spain. For that reason, in this paper, we solely analysed changes in depressive symptoms after four, eight, 16, 20, and 24 months of follow-up.
If any suspicion of depression was detected through the BDI (score BDI > 18), or the subject him/herself communicated it, the participant was examined by care providers to confirm or rule out the diagnosis of recurrence.
Other covariate assessment
At baseline, the dietitians also collected information about sociodemographic characteristics, such as educational level (secondary or less/University or more), civil status (single/married/others), and working status (working/retired/others); smoking habits (smoker/non-smoker); and anthropometric measurements (self-reported weight and height). During this phone call, information about physical activity was also collected with a physical activity questionnaire validated for the Spanish population [Citation21]. Health-related quality of life was also ascertained through the validated Spanish version of the SF-36 Health Survey [Citation22].
Sample size and statistical analysis
To detect a mean two-year difference of 3 points in the Beck Inventory with a standard deviation equal to 6 in each group considering a five percent significance level and 80% power, a sample size of 126 participants was necessary. Considering an attrition of 15%, the final number of required participants was 150.
Quantitative variables were expressed as means and standard deviations (SDs), whereas categorical variables were described as numbers and percentages (n [%]). Student t-test for continuous variables and chi-square test for categorical variables were applied to test differences in baseline characteristics according to the intervention groups.
For each participant, we computed person-months of follow-up from the date of inclusion in the study to the date of depression recurrence, the date of dropping out from the study, or the date of returning the last BDI completed by the participant, whichever came first.
Cox proportional hazards regression models were fitted to assess the relationship between the dietary intervention with Mediterranean diet and the risk of depression recurrence. Hazard Ratio (HR) and its 95% CI were calculated considering the control group as the reference category.
For the analysis of changes in depressive symptoms, we included all randomized participants with baseline data, regardless of whether they had incomplete information at follow-up visits, with multiple imputation procedures for missing data (intention-to-treat analysis). Multiple imputation method used an iterative Markov chain Monte Carlo method (STATA ‘mi’ command) was applied. We generated 20 imputations for each missing measurement. Imputed missing values were used for follow-up data but not for baseline data. The imputation models included sex, age, smoking status, body mass index, civil status, educational level, total energy intake, physical activity, intervention group, and the baseline value of the variable that was imputed as a predictor.
Furthermore, we analysed only participants with complete/available information for the overall follow-up visits (completers only). Secondly, different analyses were carried out to assess the role of the intervention in depressive symptom changes at different time periods.
Finally, the association between adherence to the Mediterranean diet (and yearly adherence change) and changes in depressive symptoms at several time periods was analysed according to an observational design.
Mixed effects linear models were used to assess the effect of the nutritional intervention on changes in depressive symptoms from baseline to four, eight, 16, 20, and 24-month follow-up visits in all randomized participants and in completers only. A two-level mixed linear model with random intercepts at the recruitment centre and participants was fitted.
Finally, mixed effects linear models were also used to assess the relationship between baseline adherence to the Mediterranean diet and joint exposure to both baseline adherence to the Mediterranean diet and adherence change after one-year follow-up and changes in BDI scores at different periods of time.
The analyses were performed using STATA (v 12.0, StataCorp LP). The significance level (two-tailed) was set at p-values lower than 0.05.
Results
Baseline characteristics
Among the 196 patients who started the intervention, 73.5% were women with a mean age of 51.1 years (SD 14.2). Participants’ age range was between 18 and 86 years old. shows the demographic, anthropometric, and lifestyle baseline characteristics of participants according to the randomized groups. No significant differences between groups were found.
Table 1. Baseline characteristics of PREDIDEP participants.
Primary outcomes
Risk of depression recurrence by intervention group
During a total of 4256 person-months of follow-up, we found 22 cases of depression recurrence. We did not find any significant association between the dietary intervention and the risk of depression recurrence with HR = 0.91 and 95% CI = 0.39–2.13.
Depressive symptoms changes by intervention groups
The effects of dietary intervention on depressive symptom changes in all randomized and completer-only participants are shown in .
Table 2. Effect of an intervention based on Mediterranean diet enriched with EVOO on changes in depressive symptoms in PREDIDEP study.
After two years of intervention, the Mediterranean Diet intervention group compared to the control group showed no differences regarding the primary outcome (recurrence of depression). Intervention group showed a depressive symptom reduction after four months [−2.15 (−4.00 to −0.29)] and eight months [−2.42 (−4.17 to −0.67)], with no changes in the control group when analysing all randomized participants. In addition, significant differences between groups were observed at 4 months (between-group difference: −3.10; 95% CI −5.72 to −0.47, p = 0.021).
After 20 months of intervention, depressive symptoms increased in the control group and descended in the intervention group, with significant differences between groups (between-group difference: −3.35; 95% CI −6.08 to −0.61, p = 0.017).
Results obtained from the completers-only analysis did not differ from the main analysis.
A sensitivity analysis was made excluding participants with baseline BDI values >18 (n = 8). The results did not change from the main estimation (data not shown).
Secondary outcomes
Depressive symptoms changes at every independent temporal period by intervention groups
The effects of dietary intervention on depressive symptom changes at every independent temporal evaluation in completers-only participants are shown in .
Table 3. The effects of dietary intervention on depressive symptoms changes at every independent temporal evaluation in completers-only participants in PREDIDEP study.
Consistent with the results observed in the previous analysis, participants in the intervention group showed a reduction in depressive symptoms at 4 months [−2.14 (−3.71 to −0.58)] (between-group difference: −3.05; 95% CI −5.59 to −0.51, p = 0.018); and after 8 months [−2.62 (−4.11 to −1.13)] (between-group difference: −2.24; 95% CI −4.33 to −0.14, p = 0.036), with no changes in control group.
In addition, depressive symptoms reduction in intervention group at 20 months [−1.91 (−3.52 to −0.30)] (between-group difference: −3.57; 95% CI −6.12 to −1.01, p = 0.006) was confirmed. Although participants in the intervention group showed a significant reduction in depressive symptoms after 24 months in the study [−1.86 (−3.65 to −0.09)], the difference between the groups was not statistically significant.
Changes in depressive symptoms at short-medium term according to baseline adherence to Mediterranean Diet
Mean changes in depressive symptoms after four and eight months of follow-up according to baseline Mediterranean Diet adherence are presented in .
Table 4. Mean changes in depressive symptoms after 4 and 8 months of follow-up according to baseline Mediterranean Diet adherence in the PREDIDEP study (n = 151).
After 8 months of follow-up, participants with high baseline adherence to the Mediterranean diet (MEDAS score > 9) showed a significant reduction in depressive symptoms [−2.06 (−4.05 to −0.08)], with no changes in those participants with baseline low adherence to this pattern. However, the difference between categories did not reach statistical significance.
Change in depressive symptoms at long term according to changes in adherence to Mediterranean Diet after one year of intervention
Mean changes in depressive symptoms after 16, 20, and 24 months of follow-up according to the annual change in Mediterranean Diet adherence are presented in .
Table 5. Mean change and 95% confidence interval in depressive symptoms after 16, 20, and 24 months of follow-up according to annual change in the adherence to the Mediterranean Diet in the PREDIDEP study (n = 95).
Participants who maintained high adherence to the Mediterranean diet after one year of follow-up showed a considerable reduction of depressive symptoms [−4.67 (−7.18 to −2.17)]. However, the differences between groups were not statistically significant.
Discussion
This trial is, to our knowledge, the first multiprofessional intervention study which has evaluated the effect of a remote dietary intervention based on the Mediterranean diet enriched with EVOO on reducing the risk of depression recurrence and on decreasing subsyndromal depressive symptoms in recovered depressed patients. Although we did not find any significant effect of the dietary intervention on the reduction of recurrence risk, our results showed, in general, an important reduction of depressive symptoms at short-medium term (four and eight months of follow-up) among participants in the intervention group. Besides, participants who maintained a high adherence to the Mediterranean diet after one year of intervention, showed a significant reduction in depressive symptoms after 24 months of follow-up.
There are several observational studies with a large sample size that have supported the relationship between high adherence to Mediterranean diet and low risk of depression. Sánchez-Villegas et al. [Citation5, Citation9], Hodge et al. [Citation6], Rienks et al. [Citation7], Skarupski et al. [Citation8], and Adjibade et al. [Citation10] found a significant inverse association linking high adherence to the Mediterranean diet with decreased depressive symptoms. These results have been collected in several systematic reviews and meta-analyses reporting conflicting results. For example, a systematic review published in 2019 was unable to conclude a significant association between adherence to the Mediterranean Diet and depression when analysing cohort studies, although the authors found significant associations in cross-sectional studies [Citation23]. However, Lassale et al. confirmed a beneficial effect of Mediterranean diet in prospective observational studies [Citation24]. The most recent evidence was published as an umbrella review of meta-analyses of observational studies and intervention trials and found that, although the strength of the evidence was generally weak, convincing or suggestive evidence was found for an inverse relationship between Mediterranean diet and depression [Citation25].
On the other hand, there are only four small randomized controlled trials which have evaluated the effects of dietary interventions based on a Mediterranean dietary pattern on depression [Citation12–15]. Firstly, the SMILES study, a 12-week randomized controlled trial with a total of 67 participants, found a positive relationship between improvements in diet and depression [Citation12]. Secondly, the HELFIMED study, a 6-month randomized controlled trial with a total of 85 participants, showed a positive relationship between a specific Mediterranean diet intervention supplemented with fish oil and depression [Citation13]. Finally, a three-week controlled trial in young adults with a total of 76 participants, found similar results than previous studies [Citation14]. SMILES and HELFIMED studies were face-to-face interventions that focused on adherence to the Mediterranean diet pattern while the last trial was an internet video guided intervention based on Australian Guide to Healthy Eating with additional recommendations to increase concordance with Mediterranean-style diets. Recently, a 12-wk, randomized controlled trial based on young males with moderate/severe depression (n = 72) found significant decreases in BDI-II scores after a dietary intervention with Mediterranean diet [Citation15].
As these previous trials, the present study showed a positive effect of a Mediterranean diet intervention on depression at short-medium term. It is important to highlight the studies duration. While the maximum follow-up period in these previous clinical trials was six months, the present study maintained the intervention and follow-up for two years.
Strengths and limitations
There are several strengths and limitations of this study that should be considered when interpreting the results. The main strength of this study is that, as far as we know, this is the first multiprofessional intervention study which has assessed the effect of a Mediterranean diet intervention enriched with EVOO combined with usual treatment on the reduction of subsyndromal symptoms of depression in patients recovered from this disease using personalized nutritional information through different remote access routes, in coordination with the face-to-face intervention conducted by psychiatrists and psychologists. To our knowledge, this is the first trial including such a high number of participants and that has evaluated the effect of a dietary intervention for a large period of time, up to two years. That long duration has allowed us to accurately evaluate the medium-long-term effects of adherence to the Mediterranean diet on subsyndromal depressive symptoms. Moreover, depressive symptoms and adherence to Mediterranean diet were evaluated by BDI and MEDAS questionnaire, respectively, which were assessed at baseline and during the intervention. Thereby, the precision of the analyses and temporal consistency of the results are guaranteed.
Likewise, to evaluate low/high adherence to the Mediterranean diet according to MEDAS, we have used a widely used reference point for Spanish population [Citation19] which allows us to obtain comparable results with other populations. Finally, some analyses have been adjusted for a wide range of baseline characteristics that could have interfered with the results.
The free provision of EVOO, which could be a strength of our study, could also represent a barrier for a generalized recommendation because of the high cost of this product.
The lack of effect of the dietary intervention for preventing the risk of depression recurrence could be probably explained by the small number of recurrences observed (only 22 cases) after a median follow-up of 24.3 months. The primary objective of the trial was to assess the role of the intervention with Mediterranean diet on depression recurrence. The sample size required to respond to this aim was of 500 participants, 250 participants in each group. Medical characteristics of the participants (most of them with residual depressive symptoms) and the irruption of COVID pandemic caused that we were not able to include and follow the overall sample. Finally, only 196 participants could be analysed so we could not obtain significant results for the main objective due to lack of statistical power. However, the inclusion of this number of participants was sufficient to assess the secondary objective of the trial, which was to compare changes in depressive symptoms during the follow-up according to the nutritional intervention.
Unfortunately, we do not present results for one-year visit to the psychiatrist although it was included in the study protocol. This visit coincided in most cases with the beginning of the COVID-19 outbreak and lockdown in Spain, and specialists could not carry out it due to health requirements derived from the epidemic situation. Furthermore, COVID-19 pandemic caused a significant impact on population mental health with an increase in depression rates, which could have also interfered with the 16-month follow-up results [Citation26,Citation27].
Another possible limitation of this study is that, although validated instruments, MEDAS and BDI questionnaires are self-reported measures, which are susceptible to information bias. It is possible that participants exert a tendency to report exposure and outcomes as more favourable than they are (social desirability bias). Likewise, if there had been an information bias, this would have been a nondifferential one biasing the results towards null (lack of effectiveness). Therefore, it would expect that the difference obtained would be even greater than that observed. Given that the blinding of patients was not possible in this nutritional intervention, the influence of a placebo effect on the self-report of depressive symptoms in the intervention group cannot be ruled out. Moreover, we need to underline that participants in the intervention group could have felt more supported and this fact could partly explain the protective effect observed in this group.
Finally, it should be highlighted that part of the intervention was made during COVID-19 pandemic (especially, between 12 and 16 months of follow-up), including the lockdown period in Spain. Evidence suggests a significant increase in the risk of depressive episodes has been observed during this period [Citation26,Citation27]. Moreover, adoption of healthier dietary habits and higher adherence to the Mediterranean diet was also observed during COVID-19 outbreak beginning and lockdown in Spain [Citation28]. All these factors could have interfered with our results. However, study retention rates were sustained over time. Moreover, adherence to the Mediterranean diet pattern was significantly greater for intervention group than for control group during the development of the trial, as we have already found [Citation29]. Finally, our results are consistent, showing similar figures between intention-to-treat and per protocol analysis.
Conclusions
Our results indicate that a Mediterranean diet–based nutritional intervention enriched with EVOO in addition to usual treatment, compared with usual care without nutritional intervention did not show efficacy regarding relapse prevention but might to a greater extent, significantly reduce subsyndromal depressive symptoms in patients with remitted major depression.
As far as we know, no previous studies have assessed the effect of a Mediterranean diet personalized intervention added to usual care on reducing subsyndromal symptoms of patients recovered from depression. Moreover, worldwide it is the first time that a long-term evaluation of a dietary intervention (follow-up and intervention period of two years) has been carried out in this type of patients. In this sense, we observed that the efficacy of the Mediterranean diet intervention on subsyndromal symptoms of depression was maintained over time.
For that reason, Mediterranean Diet nutritional interventions, which are safe and inexpensive interventions, seem to be a great tool for secondary depression prevention if its preventive properties are confirmed in future clinical trials in major depressive disorder.
Acknowledgements
The authors are grateful to all PREDIDEP study participants.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Funding
This study is externally funded by the Spanish Ministry of Economy and Competitiveness (ISCIII), grant no. PI16/01274. The Interprofesional del Aceite de Oliva-Aceites de Oliva de España (Madrid, Spain) donated the olive oil used in the study.
None of the funding sources played a role in the design, collection, analysis, or interpretation of the data or in the decision to submit the manuscript for publication.
Data availability statement
The data that support the findings of this study are available from the corresponding author [ASV], upon reasonable request.
Trial registration number: ClinicalTrials.gov NCT03081065.
Additional information
Notes on contributors
Beatriz M. Cabrera-Suárez
Beatriz Cabrera-Suárez, MD, PhD. Psychiatrist. Hospital Dr. Negrín, Las Palmas de Gran Canaria (Spain).
Jose L. Hernández-Fleta
Jose L Hernández-Fleta, MD, PhD. Associate Prof. of Psychiatry. Universidad de Las Palmas de Gran Canaria. Director of the Department of Psychiatry. Hospital Dr. Negrín, Las Palmas de Gran Canaria (Spain).
Patricio Molero
Patricio Molero, MD, PhD. Psychiatrist. Clínica Universidad de Navarra (Spain).
Ana González-Pinto
Ana González-Pinto, Professor of Psychiatry. Universidad del País Vasco. Director of the Department of Psychiatry. Scientific Director of the CIBERSAM. Hospital Universitario de Alava. Vitoria, Spain.
Francisca Lahortiga
Francisca Lahortiga Ramos, PhD. Associate Prof. of Psychology. Director of the Department of Clinical Psychology at Clinica Universidad de Navarra (Spain) (retired).
Claudio Cabrera
Claudio Cabrera, MD. PhD. Associate Prof. of Psychiatry. Universidad de Las Palmas de Gran Canaria. Psychiatrist. Hospital Dr. Negrín, Las Palmas de Gran Canaria (Spain).
Carlos Chiclana-Actis
Carlos Ciclana, MD. PhD. Psychiatrist. Psychotherapist. Medical Director at “Consulta Dr. Carlos Chiclana”. Researcher at the International University of La Rioja (Spain).
Almudena Sánchez-Villegas
Almudena Sánchez-Villegas, BPharm, PhD. Professor of Preventive Medicine and Public Health. Universidad Pública de Navarra, Pamplona, Spain.
References
- Ferrari AJ, Somerville AJ, Baxter AJ, et al. Global variation in the prevalence and incidence of major depressive disorder: a systematic review of the epidemiological literature. Psycho Med. 2013;43:471–81. doi:10.1017/S0033291712001511
- Thase M, Jindal R, Howland R. Biological aspects of depression. In: Gotlib I, Hammen C, eds. Handbook of depression. Nueva York: The Guilford Press; 2002.
- GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. 2022;9(2):137-50.
- Morris L, Bhatnagar D. The Mediterranean diet. Curr Opin Lipidol. 2016;27(1):89–91. doi:10.1097/MOL.0000000000000266
- Sanchez-Villegas A, Delgado-Rodriguez M, Alonso A, et al. Association of the Mediterranean dietary pattern with the incidence of depression: the Seguimiento Universidad de Navarra/ University of Navarra follow-up (SUN) cohort. Arch Gen Psychiatry 2009;66(10):1090–8. doi:10.1001/archgenpsychiatry.2009.129
- Hodge A, Almeida OP, English DR, Giles GG, Flicker L. Patterns of dietary intake and psychological distress in older Australians: benefits not just from a Mediterranean diet. Int Psychogeriatr. 2013;25(3):456–66. doi:10.1017/S1041610212001986
- Rienks J, Dobson AJ, Mishra GD. Mediterranean dietary pattern and prevalence and incidence of depressive symptoms in mid-aged women: results from a large community-based prospective study. Eur J Clin Nutr. 2013;67(1):75–82. doi:10.1038/ejcn.2012.193
- Skarupski KA, Tangney CC, Li H, Evans DA, Morris MC. Mediterranean diet and depressive symptoms among older adults over time. J Nutr Health Aging. 2013;17(5):441–5. doi:10.1007/s12603-012-0437-x
- Sánchez-Villegas A, Henríquez-Sánchez P, Ruiz-Canela M, et al. A longitudinal analysis of diet quality scores and the risk of incident depression in the SUN project. BMC Med. 2015;13:197. doi:10.1186/s12916-015-0428-y
- Adjibade M, Assmann KE, Andreeva VA, et al. Prospective association between adherence to the Mediterranean diet and risk of depressive symptoms in the French SU.VI.MAX cohort. Eur J Nutr. 2018;57(3):1225–35. doi:10.1007/s00394-017-1405-3
- Mamalaki E, Ntanasi E, Hatzimanolis A, Basta M, Kosmidis M, Dardiotis E, et al. The association of adherence to the Mediterranean diet with depression in older adults longitudinally taking into account cognitive status: results from the HELIAD study. Nutrients. 2023;15(2):359. doi:10.3390/nu15020359
- Jacka FN, O’Neil A, Opie R, et al. A randomised controlled trial of dietary improvement for adults with major depression (the ‘SMILES’ trial). BMC Med. 2017;15(1):23. Erratum in: BMC Med 2018;16(1):236. doi:10.1186/s12916-017-0791-y
- Parletta N, Zarnowiecki D, Cho J, et al. A Mediterranean-style dietary intervention supplemented with fish oil improves diet quality and mental health in people with depression: a randomized controlled trial (HELFIMED). Nutr Neurosci. 2019;22(7):474–87. doi:10.1080/1028415X.2017.1411320
- Francis HM, Stevenson RJ, Chambers JR, Gupta D, Newey B, Lim CK. A brief diet intervention can reduce symptoms of depression in young adults – a randomised controlled trial. PLoS One. 2019;14(10):e0222768. doi:10.1371/journal.pone.0222768
- Bayes J, Schloss J, Sibbritt D. The effect of a Mediterranean diet on the symptoms of depression in young males (the ‘AMMEND: A Mediterranean diet in MEN with depression’ study): a randomized controlled trial. Am J Clin Nutr. 2022;116(2):572–80. doi:10.1093/ajcn/nqac106
- Recchia D, Baghdadli A, Lassale C, Brunner E, Verdier JM, Kivimäki M, Akbaraly T. Associations between long-term adherence to healthy diet and recurrent depressive symptoms in Whitehall II Study. Eur J Nutr. 2020;59(3):1031–41. doi:10.1007/s00394-019-01964-z
- Sánchez-Villegas A, Cabrera-Suárez B, Molero P, et al. Preventing the recurrence of depression with a Mediterranean diet supplemented with extra-virgin olive oil. The PREDI-DEP trial: study protocol. BMC Psychiatry. 2019;19(1):63. doi:10.1186/s12888-019-2036-4
- Schröeder H, Fitó M, Estruch R, et al. Screener is valid for assessing Mediterranean diet adherence among older Spanish men and women. J Nutr. 2011;141:1140–5. doi:10.3945/jn.110.135566
- García-Conesa MT, Philippou E, Pafilas C, et al. Exploring the validity of the 14-item Mediterranean diet adherence screener (MEDAS): a Cross-National Study in Seven European Countries around the Mediterranean Region. Nutrients. 2020;12(10):2960. doi:10.3390/nu12102960
- Sanz J, Navarro ME, Vázquez C. Adaptación española para el Inventario de Depresión de Beck-II (BDI-II). Propiedades psicométricas en estudiantes universitarios. Análisis y Modificación de Conducta. 2003;29:239–88. article in Spanish.
- Martínez-González MA, López-Fontana C, Varo JJ, Sánchez-Villegas A, Martinez JA. Validation of the Spanish version of the physical activity questionnaire used in the nurses’ health study and the health professionals’ follow-up study. Public Health Nutr. 2005;8(7):920–7. doi:10.1079/PHN2005745
- Alonso J, Regidor E, Barrio G, et al. Population reference values of the Spanish version of the Health Questionnaire SF-36. Med Clin (Barc). 1998;111(11):410–6.
- Shafiei F, Salari-Moghaddam A, Larijani B, Esmaillzadeh A. Adherence to the Mediterranean diet and risk of depression: a systematic review and updated meta-analysis of observational studies. Nutr Rev. 2019;77(4):230-9. Erratum in: Nutr Rev 2019;77(6):454. doi:10.1093/nutrit/nuy070
- Lassale C, Batty GD, Baghdadli A, et al. Healthy dietary indices and risk of depressive outcomes: a systematic review and meta-analysis of observational studies. Mol Psychiatry. 2019;24(7):965–86. doi:10.1038/s41380-018-0237-8
- Gianfredi V, Dinu M, Nucci D, Eussen SJPM, Amerio A, Schram MT, Schaper N, Odone A. Association between dietary patterns and depression: an umbrella review of meta-analyses of observational studies and intervention trials. Nutr Rev. 2023;81(3):346–59. doi:10.1093/nutrit/nuac058. Online ahead of print.
- Salari N, Hosseinian-Far A, Jalali R, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Global Health. 2020;16(1):57. doi:10.1186/s12992-020-00589-w
- Luo M, Guo L, Yu M, Jiang W, Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public – a systematic review and meta-analysis. Psychiatry Res. 2020;291:113190. doi:10.1016/j.psychres.2020.113190
- Rodríguez-Pérez C, Molina-Montes E, Verardo V, et al. Changes in dietary behaviours during the COVID-19 outbreak confinement in the Spanish COVIDiet study. Nutrients. 2020;12(6):1730. doi:10.3390/nu12061730
- Cabrera-Suárez BM, Pla J, González-Pinto A, et al. Effectiveness of a remote nutritional intervention to increase the adherence to the Mediterranean diet among recovered depression patients. Nutr Neuroscience. 2023;26(8):696–705. doi:10.1080/1028415X.2022.2081448. Online ahead of print.