ABSTRACT
Background
Insufficient management of postoperative pain is a notable issue encountered by individuals after open-heart operations. The study aimed to evaluate the effect of ultrasound-guided pecto-intercostal fascial block (PIFB) and transversus thoracis muscle plane (TTB) on the analgesic efficacy in adult patients undergoing open-heart operations and the duration of mechanical ventilation (MV).
Methods
A randomized double-blind controlled trial was conducted on a cohort of 90 adult patients with elective open-heart surgery, namely valve replacement, with midline sternotomy. Patients were divided into three groups of similar size. The first group (control group) received conventional systemic analgesia alone, while the second group received bilateral TTB and the third group received bilateral PIFB, using ultra-sound guided technique.
Results
A significant reduction in NRS (Numeric Rating Scale) values was observed in both the TTB group and the PIFB group as compared to the control group at zero, three and 6-hour postoperative. The PIFB and TTB group exhibited an important delay in the initiation of first rescue analgesia, as well as a reduction in the overall intake of fentanyl for rescue purposes during a twenty-four-hour period. Additionally, the TTB group and the PIFB group demonstrated considerably shorter durations of mechanical ventilation as compared to the control group.
Conclusions
The utilization of ultrasound TTB and PIFB demonstrated efficacy in providing postoperative analgesia compared to the control group. This was evidenced by the less requirement for additional analgesic medication, reducing postoperative pain scores and a shorter duration of mechanical ventilation.
1. Introduction
Inadequate pain management may significantly impact the recovery process after surgery, resulting in various adverse outcomes such as pulmonary problems, heightened thromboembolic events, delayed wound healing and myocardial infarction [Citation1,Citation2]. These consequences subsequently contribute to prolonged stays in the intensive care unit (ICU) and hospital. In addition, it should be noted that the absence of appropriate treatment for acute pain has the potential to develop into chronic pain in a significant proportion, ranging from thirty to fifty percent of those who have had postcardiac surgical procedures [Citation3–5].
Traditional approaches to managing pain during the perioperative period often include the administration of opioids and nonsteroidal anti-inflammatory medications (NSAIDs). NSAIDs have been associated with the potential occurrence of bleeding, hemorrhagic complications and renal failure. On the other hand, opiates have been known to induce adverse effects such as, over sedation, nausea, vomiting, ileus, and respiratory depression [Citation6,Citation7].
Alternative treatments, as acetaminophen, ketamine and lidocaine patches, have not shown definitive efficacy [Citation8,Citation9]. Several regional treatments have been used for the thoracotomy pain management, including thoracic epidural, paravertebral nerve block, intercostal nerve block, and thoracic erector spinae plane block [Citation10,Citation11].
The Pecto-Intercostal Fascial Block (PIFB) is an innovative and less invasive approach for regional fascial plane block. The procedure known as PIFB specifically focuses on the anterior intercostal nerves, which traverse the fascial plane located between the external intercostal aponeurosis and the pectoralis major muscle, these neurons arise bilaterally across the sternum [Citation12].
The transversus thoracis muscle plane block (TTB) is an innovative regional anesthetic method that offers analgesic effects specifically targeting the anterior chest wall [Citation13,Citation14].
The TTB block refers to a nerve block technique that administers a local anesthetic into the transversus thoracis muscle plane, which is situated between the transversus thoracis and internal inter-costal muscles. In contrast to neuraxial blockade, both PIFB and TTB techniques do not exhibit an association with nerve damage, dural puncture, or epidural hemorrhage [Citation15].
The objective of this research was to assess and evaluate the impact of ultrasound-guided PIFB and TTB on pain scores as the major outcome, and secondary outcomes including 24-hour total opioid intake, duration of mechanical ventilation (MV), and incidence of complications in patients having elective open-heart operations.
2. Patients and methods
The present study was conducted on a sample of Ninety adult patients, including both females and males, aged between 21 and 60-years old. These patients were scheduled to have elective open-heart surgery, namely valve replacement, using midline sternotomy. The research design included blinding and randomization techniques to ensure control over any biases. The investigation was carried out between November 2021 and January 2023 subsequent to receiving clearance from the Ethical Committee of Tanta University Hospitals (approval number 21/2/34494) and registering on clinical trial.gov (ID: NCT05115357). All patients provided informed written consent.
The exclusion criteria encompassed several factors, such as chronic analgesic usage, cognitive impairment, a past record of drug abuse and a history of allergic reactions to local anesthetics, emergency or repeat surgeries, pre-existing important dysfunction of major organs including the liver or kidneys, pulmonary insufficiency, left ventricular ejection fraction (LVEF) below thirty%, known coagulation disorders, reliance on inotropes or intra-aortic balloon pump support, hemodynamic instability and an extended period of postoperative ventilatory support more than six hours.
The patients were randomly assigned to one of three groups of equal size. The first group, referred to as the control group, received just postoperative conventional systemic analgesia. The second group, referred to as the TTB group, received bilateral TTB along with an injection of 19 mL of 0.25% bupivacaine and one mL of 4-mg dexamethasone on each side. The third group, referred to as the PIFB group, received bilateral PIFB along with the same injection of bupivacaine and dexamethasone.
The process of randomization was conducted via the sealed opaque envelope method. The administration of the blocks was carried out by a single anesthesiologist, whilst the evaluation of outcome measures was conducted by another anesthesiologist who was unaware of the research groups.
The surgical and medical histories of the patient were assessed, followed by standard laboratory testing and clinical exams. The participants were instructed to observe an eight-hour fasting period for solid foods, a six-hour fasting period for semisolid foods, and a two-hour fasting period for clear fluids.
Upon entering the operating room, an IV line was established using an 18 G cannula. Routine monitoring, which consisted of electrocardiography (ECG), pulse oximetry (SPO2) and non-invasive arterial blood pressure measurement was then started for the patient. The administration of sedation was performed with midazolam at a dosage range of 0.01–0.05 mg/kg, arterial line was inserted under local anesthesia and invasive arterial blood pressure monitoring was started.
The administration of general anesthesia began by administering IV fentanyl at a dosage of five µg/kg. Subsequently, rocuronium was administered at a dosage range of 0.9–1.2 mg/kg to aid in the process of endotracheal intubation. A central venous catheter was successfully placed. The maintenance of anesthesia was achieved by administering a combination of intravenous fentanyl, bolus doses of rocuronium (0.1–0.2 mg/kg) and isoflurane in oxygen. Following the administration of sufficient heparin and the establishment of aortocaval cannulation, complete cardiopulmonary bypass was commenced. Following the administration of protamine and the completion of decisive surgery to reverse the effects of heparin until the activated clotting time returned to normal values, the sites where mediastinal drains were inserted were infiltrated with 2–3 ml of lidocaine 2%.
The administration of transversus abdominis plane blocks and femoral, guided by US was performed inside the operating theater after the closure of skin, before the patients were transferred to the critical care unit. The blocks were executed in a supine posture, with the chest area exposed, while maintaining strict aseptic conditions. The ultrasonic imaging was conducted using a Philips C×50machine equipped with a linear transducer operating at a high frequency range of seven-twelve MHz. The local anesthetic solutions were formulated inside twenty mL syringes, comprising nineteen mL of 0.25% bupivacaine combined with one mL of four mg dexamethasone.
3. PIFB
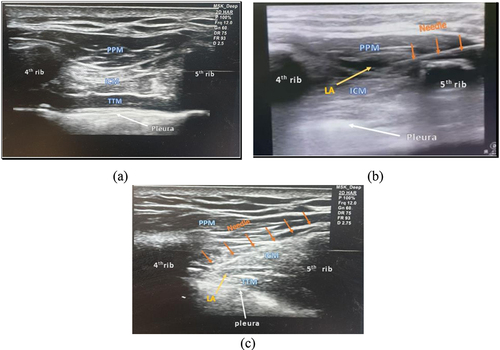
The transducer was positioned in a longitudinal manner, about 2 cm lateral to the sternal border, inside the fourth or fifth intercostal area. The parasternal sagittal view allowed for visualization of the pectoralis major muscle and the external intercostal muscles located between the fourth and fifth rib. Under the direction of ultrasonography, a needle measuring 22-gauge and 50 mm in length was placed in-plane. The needle was inserted into the pectoralis major muscle, and the local anesthetic solution was injected into the pecto-intercostal fascial plane, which is situated between the pectoralis major muscle and the external intercostal muscles, following a process of negative aspiration. The ultrasound imaging allowed for the observation of the separation of the fascial plane and the dispersion of the medication. To achieve bilateral blockage, the operation was repeated on the contralateral side [Citation16]. ()
4. TTB
The probe was positioned in the longitudinal plane, namely 1 cm laterally from the sternal boundary. The intercostal gap between the fourth and fifth ribs was detected using US imaging. The parasternal sagittal view allowed for visualization of the transversus thoracis muscle, and the internal intercostal muscle located between the fourth and fifth rib, positioned superior to the pleura. A needle with a diameter of 22-gauge and a length of 50 mm was put into the body in a specific direction until its tip reached the transversus thoracis muscle plane, which is situated between the transversus thoracis and internal intercostal muscles. Following the negative aspiration of air and blood, the administration of local anesthetic was carried out in aliquots of five mL, with intermittent aspiration. The procedure mentioned above was replicated on the contralateral side to achieve a bilateral blockage ().
4.1. Management of postoperative ICU
Following the completion of the PIFB and TTB procedures, patients were then moved to the ICU for ongoing medical attention. In this setting, patients received routine analgesic treatment in the form of IV administration of paracetamol at a dosage of 1 g every 6 hours, as well as tramadol at a dosage of 50 milligrams. The patients in the ICU were maintained under sedation until they met the necessary requirements for extubation.
Following extubation, all patients underwent pain assessment using the numeric rating scale (NRS) for pain, which encompasses a range from zero (indicating the absence of pain) to 10 (representing the most severe pain possible). In cases where the NRS score was equal to or greater than four rescue analgesia was administered intravenously in the form of fentanyl at a dosage of 0.5 µg/kg. The moment at which the first request for analgesia was made and the cumulative amount of fentanyl administered as rescue medication were recorded. The duration of mechanical ventilator (MV) in the ICU was documented as the period from the patient’s admission to the ICU to their successful weaning off MV. The research documented the occurrence of postoperative sequelae, including hematoma, pneumothorax, and local anesthetic toxicity, within 24 hours after the administration of blocks.
4.2. Sample size calculation
The main dependent variable in our research was the ratings measuring postoperative discomfort. The sample size of 27 patients was determined based on the findings of a prior investigation [Citation17]. This sample size was considered sufficient to identify a difference of 2.26 in the pain score, with a statistical power of 80% and an SD of 2.92, while maintaining an α error of 0.05. We enrolled a total of 30 individuals in each group, accounting for potential dropouts.
4.3. Statistical analysis
The statistical analysis was performed using SPSS v27 software (IBM©, Chicago, IL, USA). The assessment of the normality of the data distribution was conducted using the histograms and Shapiro–Wilks test. The research provided quantitative parametric data, namely in the form of average and SD. The data underwent statistical analysis using the analysis of variance (ANOVA) test, followed by a post hoc test (Tukey) to ascertain any significant disparities. The research used a quantitative non-parametric approach to analyze the data, with the results presented in terms of the inter-quartile range (IQR) and median. The statistical research included the use of the Kruskal–Wallis test, followed by the Mann Whitney-test, in order to compare the various groups. The qualitative variables were expressed in terms of percentage (%) and frequency and were analyzed using the chi-square test. A two-tailed p-value below 0.05 was considered statistically important.
5. Results
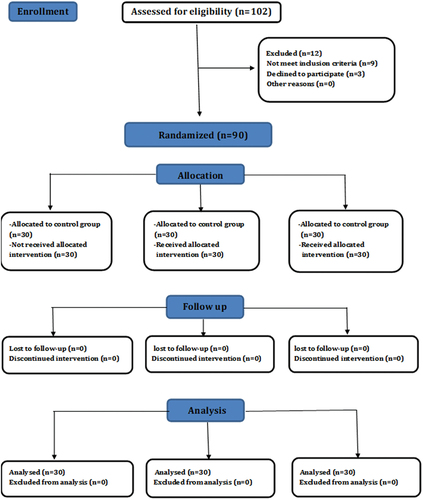
One hundred and two patients were evaluated for eligibility, nine patients did not meet the inclusion criteria (six patients on inotropic support, two patients had hemodynamic instability with left ventricular ejection fraction (LVEF) < thirty%, one patient had cognitive impairment) and three patients refused to participate in the study. The remaining 90 patients were randomly allocated in three groups (30 patients in each one). All the 90 patients were followed-up and their data were analyzed statistically ().
Figure 2. The CONSORT flow graphic illustrates the progression of participants at each stage of the randomized study.
There were no significant differences between the three groups as regards their duration of operations, demographic characteristics, type and intraoperative fentanyl consumption ().
Table 1. Demographic characteristics, type of operations, cross-clamping time, duration of operations, type and intraoperative fentanyl consumption in three studied groups.
The findings of this research indicate that there were lower values of NRS values in both the PIFB group and the TTB group when compared to the control group at zero 3 and 6 hours. (p = 0.002, <0.001, and <0.001, respectively). However, there were no significant differences observed among the three groups at 12 and 24 hours (p value = 0.068 and 0.053, respectively). No statistically significant differences were observed between the group receiving the PIFB intervention and the group receiving the TTB intervention at various measurement time points ().
Table 2. Comparison among the three studied groups according to (NRS).
There was an important delay in the onset of 1st analgesic request along with an important decline in the total 24-hour analgesic consumption in the PIFB group and TTB group as compared to control group (p value = 0.001 and <0.001 respectively). While no significant differences were observed between PIFB group and TTB group (p3 = 0.172 and p3 = 0.467 respectively). The duration of MV was significantly decreased in the PIFB group with average ± SD of 79.17 ± 26.13 hour and the TTB group with average ± SD of 66.07 ± 19.76 hour as compared to control group with average ± SD (134.0 ± 30.92) and (p < 0.001). There were no significant differences in the duration of MV between the PIFB group and the TTB group (P3 = 0.131). ().
Table 3. Comparison between the three studied groups according to time to postoperative analgesia, first analgesic request, and consumption of postoperative analgesia.
6. Discussion
The findings of this research revealed that the TTB and PIFB were associated with lower NRS and with decreased postoperative rescue analgesic consumption and delayed onset of 1st analgesic request as well as shorter duration of MV as compared to control group with variances observed among PIFB and TTB at all measurements.
Our research demonstrated that the use of ultrasound guided PIFB and TTB provided effective post operative analgesia in patients undergoing valve replacement surgery. PIFB and TTB were associated with reduced postoperative NRS at (zero, three, six hr) and declined post operative rescue fentanyl consumption as well delayed the onset of first rescue analgesia as compared to the control group with no significant differences between PIFB and TTB.
Our results were supported by Zhang et al.; [Citation18], Kumar et al.; [Citation19] and Hamed et al.; [Citation20] who concluded that bilateral PIFB provides effective analgesia in patients undergoing open cardiac surgery.
Moreover, Zhang et al. [Citation21] used continuous PIFB to provide effective analgesia in adult patients undergoing open cardiac surgery. The study concluded that bilateral continuous PIFB provided effective postoperative pain relief for 3 days.
Khera et al. [Citation22] found that patients receiving PIFB showed a statistically important reduction in visual analog scale scores. However, there was no difference in the -hour cumulative opioid (morphine) requirement.
Our outcomes were consistent with that of Aydin et al.; [Citation23] who studied the efficacy of ultrasound guided TTB on postoperative opioid consumption after cardiac surgery concluded that a single preoperative TTB provided effective analgesia and decreased opioid requirements in patients undergoing cardiac surgery.
Zhang et al.; [Citation24], Hamed et al.; [Citation25] and Deng et al.; [Citation26] concluded that bilateral TTB blocks can provide good perioperative analgesia for patients undergoing open cardiac surgery and promote postoperative recovery.
In contrast to the findings of our study, Fujii et al. [Citation27] reported that there was no significant difference in the 24-hour opioid requirement between patients who received the block and those who did not. The authors attributed their results to the absence of control over intraoperative and ICU opioid administration, which was used to manage sedate patients, hypertension, and alleviate non-surgical musculoskeletal discomfort caused by immobility. These factors may have influenced the overall opioid requirement.
Up to our knowledge only one pilot study of Kaya et al. [Citation28] indicate that there was no statistically important variation in the first 24-hour administration of morphine between the TTB and the PIFB groups. Additionally, no significant difference was observed in the NRS scores between the two groups. Moreover, both groups exhibited comparable needs for supplementary analgesia within the first 24 hours. However, in contrast to our research, they ascribed the cause for this disparity to the utilization of internal thoracic artery (ITA) harvesting in 85% of patients undergoing transversus TTB. This ITA harvesting procedure impacted the dispersion of LA along the transversus thoracic muscle, thereby impeding the injection from reaching the level of intended thoracic.
Our findings demonstrated that the duration of MV was significantly decreased in the PIFB group and the TTB group as compared to the control group. This may be due to minimal consumption of opioids in the ICU, to sedate patients, to maintain hemodynamic stability and to treat hypertension. High-dose opioid may cause prolonged ventilation, respiratory depression and delayed recovery.
Our results showed that the duration of MV was significantly decreased in the PIFB group and the TTB group as compared to the control group. This may be due to minimal consumption of opioids in the ICU to treat hypertension, to sedate patients and to maintain hemodynamic stability. High-dose opioid may cause respiratory depression, delayed recovery and prolonged ventilation.
Our results were in agreement with previous researches [Citation18,Citation21] which revealed that the time to extubation, the length of hospital stay and length of stay in the ICU were significantly decreased in the PIFB group.
The present results observed in this research mirror those of the previous research [Citation24,Citation29,Citation30] which revealed that the time to extubation were significantly shorter in the bilateral TTB blocks groups as compared to no nerve block groups. which might be attributed to the significantly lower postoperative opioid use in the TTB group than in the control group.
Cardinale et al.; [Citation31] It was determined that the use of a multimodal treatment approach, which included the use of a TTB, for patients having median sternotomy, led to a notable proportion of patients being extubated in the operating room, without any observed rise in the occurrence of postoperative re-intubations.
In contrast to our results, the studies of Deng et al.; [Citation26] and Hamed et al.; [Citation25] concluded that the reason was likely because extubation is not solely dependent on pain management; other parameters, such as hemodynamic stability and the neuromuscular blocker’s (NMB) complete reversibility, can influence the extubation time.
Our investigation has several limitations: it is important to note that providing good pain management after surgery has the potential to mitigate the onset of chronic pain. However, it is crucial to acknowledge that our research did not include a follow-up period beyond three to 6-month post-operation to assess the incidence of chronic pain. The catheter approach was not used in our study. However, it should be noted that continuous PIFB has the potential to provide sustained postoperative analgesia after heart surgery. Our study only focused on individuals who had valve replacement surgery. Consequently, more research is required to investigate the effects on patients following open-heart surgery.
7. Conclusion
The utilization of ultrasound TTB and PIFB demonstrated efficacy in providing postoperative analgesia compared to the control group. This was evidenced by the less requirement for additional analgesic medication, reducing postoperative pain scores and a shorter duration of mechanical ventilation.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Huang APS, Sakata RK. Dor após esternotomia – revisão. Rev Bras Anestesiol. 2016;66(4):395–401. doi: 10.1016/j.bjan.2014.09.003
- Gao L, Mu H, Lin Y, et al. Review of the Current situation of postoperative pain and causes of inadequate pain management in Africa. J Pain Res. 2023;16:1767–78. doi: 10.2147/JPR.S405574
- Beloeil H, Sulpice L. Peri-operative pain and its consequences. J Visc Surg. 2016;153(6):15–18. doi: 10.1016/j.jviscsurg.2016.09.004
- Weissman C. Pulmonary complications after cardiac surgery. Seminars in cardiothoracic and vascular anesthesia. Semin Cardiothorac Vasc Anesth. 2004;8(3):185–211. doi: 10.1177/108925320400800303
- Mittnacht AJ, Shariat A, Weiner MM, et al. Regional techniques for cardiac and cardiac-related procedures. J Cardiothorac Vasc Anesth. 2019;33(2):532–546. doi: 10.1053/j.jvca.2018.09.017
- de Souza Brito, F, Mehta RH, Lopes RD, et al. Nonsteroidal anti-inflammatory drugs and clinical outcomes in patients undergoing coronary artery bypass surgery. Am J Med. 2017;130(4):462–468. doi: 10.1016/j.amjmed.2016.10.023
- Sinatra R Causes and consequences of inadequate management of acute pain. Pain Med. 2010;11:1859–1871. 12 doi: 10.1111/j.1526-4637.2010.00983.x
- Vilīte B, Strīķe E, Rutka K, et al. Pain management in intensive care unit patients after cardiac surgery with sternotomy approach. Acta Med Litu. 2019;26(1):51–59. doi: 10.6001/actamedica.v26i1.3956
- Liu SS, Wu CL. Effect of postoperative analgesia on major postoperative complications: a systematic update of the evidence. Anesthesia & Analgesia. 2007;104(3):689–702. doi: 10.1213/01.ane.0000255040.71600.41
- Svircevic V, Nierich AP, Moons KG, et al. Thoracic epidural anesthesia for cardiac surgery: a randomized trial. ASA. 2011;114(2):262–270. doi: 10.1097/ALN.0b013e318201d2de
- Hamilton C, Alfille P, Mountjoy J, et al. Regional anesthesia and acute perioperative pain management in thoracic surgery: a narrative review. J Thorac Dis. 2022;14(6):2276–96. doi: 10.21037/jtd-21-1740
- Hong B, Yoon S-H, Youn AM, et al. Thoracic interfascial nerve block for breast surgery in a pregnant woman: a case report. Korean J Anesthesiol. 2017;70(2):209–12. doi: 10.4097/kjae.2017.70.2.209
- Ueshima H, Kitamura A. Clinical experiences of ultrasound-guided transversus thoracic muscle plane block: a clinical experience. J Clin Anesth. 2015;27(5):428–9. doi: 10.1016/j.jclinane.2015.03.040
- Zhong R, Zou Y, Bao S, et al. Analgesic efficacy of an ultrasound-guided transversus thoracis plane block combined with an intermediate cervical plexus block on postoperative pain relief after trans-areolar endoscopic thyroidectomy: A single center prospective randomized controlled study. J Pain Res. 2023;16:1059–1067. doi: 10.2147/JPR.S402902
- Nagaraja P, Ragavendran S, Singh NG, et al. Comparison of continuous thoracic epidural analgesia with bilateral erector spinae plane block for perioperative pain management in cardiac surgery. Ann Card Anaesth. 2018;21(3):323–25. doi: 10.4103/aca.ACA_16_18
- Wang L, Jiang L, Jiang B, et al. Effects of pecto-intercostal fascial block combined with rectus sheath block for postoperative pain management after cardiac surgery: a randomized controlled trial. BMC Anesthesiol. 2023;23(1):90. doi: 10.1186/s12871-023-02044-w
- Nagaraja PS, Ragavendran S, Singh NG, et al. Comparison of continuous thoracic epidural analgesia with bilateral erector spinae plane block for perioperative pain management in cardiac surgery. Ann Card Anaesth. 2018;21(3):323–7. doi: 10.4103/aca.ACA_16_18
- Zhang Y, Gong H, Zhan B, et al. Effects of bilateral pecto-intercostal fascial block for perioperative pain management in patients undergoing open cardiac surgery: a prospective randomized study. BMC Anesthesiol. 2021;21(1):1–8. doi: 10.1186/s12871-021-01391-w
- Kumar AK, Chauhan S, Bhoi D, et al. Pectointercostal fascial block (PIFB) as a novel technique for postoperative pain management in patients undergoing cardiac surgery. J Cardiothorac Vasc Anesth. 2021;35(1):116–122. doi: 10.1053/j.jvca.2020.07.074
- Hamed MA, Abdelhady MA, Hassan AA, et al. The analgesic effect of ultrasound-guided bilateral pectointercostal fascial plane block on sternal wound pain after open heart surgeries: a randomized controlled study. Clin J Pain. 2022;38(4):279–284. doi: 10.1097/AJP.0000000000001022
- Zhang Y, Min J, Chen S. Continuous pecto-intercostal fascial block provides effective analgesia in patients undergoing open cardiac surgery: a randomized controlled trial. Pain Med. 2022;23(3):440–7. doi: 10.1093/pm/pnab291
- Khera T, Murugappan KR, Leibowitz A, et al. Ultrasound-guided pecto-intercostal fascial block for postoperative pain management in cardiac surgery: a prospective, randomized, placebo-controlled trial. J Cardiothorac Vasc Anesth. 2021;35(3):896–903. doi: 10.1053/j.jvca.2020.07.058
- Aydin ME, Ahiskalioglu A, Ates I, et al. Efficacy of ultrasound-guided transversus thoracic muscle plane block on postoperative opioid consumption after cardiac surgery: a prospective, randomized, double-blind study. J Cardiothorac Vasc Anesth. 2020;34(11):2996–3003. doi: 10.1053/j.jvca.2020.06.044
- Zhang Y, Li X, Chen S. Bilateral transversus thoracis muscle plane block provides effective analgesia and enhances recovery after open cardiac surgery. J Card Surg. 2021;36(8):2818–23. doi: 10.1111/jocs.15666
- Hamed MA, Boules ML, Sobhy MM, et al. The analgesic efficacy of ultrasound-guided bilateral transversus thoracic muscle plane block after open-heart surgeries: a randomized controlled study. J Pain Res. 2022;15:675–679. doi: 10.2147/JPR.S355231
- Deng Q, Zheng C, Xia K. Transverse thoracic muscle plane block as a routine strategy for cardiac enhanced recovery after surgery in sternotomy: a retrospective analysis. J Med. 2022;101(11):5–9. doi: 10.1097/MD.0000000000029000
- Vadivelu N, Mitra S, Narayan D Recent advances in postoperative pain management. Yale J Biol Med. 2010;83:11–25.
- Kaya C, Dost B, Dokmeci O, et al. Comparison of ultrasound-guided pecto-intercostal fascial block and transversus thoracic muscle plane block for acute poststernotomy pain management after cardiac surgery: a prospective, randomized, double-blind pilot study. J Cardiothorac Vasc Anesth. 2022;36(8):2313–21. doi: 10.1053/j.jvca.2021.09.041
- Fujii S, Roche M, Jones PM, et al. Transversus thoracis muscle plane block in cardiac surgery: a pilot feasibility study. Reg Anesth Pain Med. 2019;44(5):556–60. doi: 10.1136/rapm-2018-100178
- Shokri H, Ali I, Kasem AA. Evaluation of the analgesic efficacy of bilateral ultrasound-guided transversus thoracic muscle plane block on post-sternotomy pain: a randomized controlled trial. Local Reg Anesthesia. 2021;14:145–149. doi: 10.2147/LRA.S338685
- Cardinale JP, Latimer R, Curtis C, et al. Incorporation of the transverse thoracic plane block into a multimodal early extubation protocol for cardiac surgical patients. Cardiothoracic And Vascular Anesthesia Is Semin. 2021;25(4):301–309. doi: 10.1177/1089253220957484