ABSTRACT
Introduction
Patients with fractured hips almost always have marked pain that results in unfavorable positioning for the central neuraxial block. It was revealed that regional block approaches, including suprainguinal fascia-iliaca compartment block (S-FICB) and pericapsular nerve group (PENG) block, might effectively alleviate pain in patients with hip fractures. This research aimed to evaluate the influence of S-FICB and PENG block on patients positioning during central neuraxial block and compare their analgesic efficacy.
Methods
This randomized double-blinded trial included 60 cases aged ≥ 40 years old and ASA I-III with hip fracture with persistent pain and scheduled for surgery under spinal anesthesia (SA). Cases were randomized equally into two groups. Group I (S-FICB) received ultrasound (US) guided S-FICB, and group II (PENG group) received US guided PENG. Both blocks were performed by the same operator using 23 ml of ropivacaine 0.25% + 2 ml (8 mg) of dexamethasone.
Results
The ease of spinal positioning (EOSP) score was significantly better in the PENG group than the S-FICB group (p < 0.001). Twenty minutes after blocks, the numeric rating scale (NRS) reduced significantly in PENG than in SFICB groups at rest (p < 0.015) and movement (p < 0.010). The first request for analgesia, NRS in the first 24-hour period postoperatively, and the number of tramadol doses were similar between both groups (p = 0.552) and (p < 0.370), respectively.
Conclusions
Although each block provides comparable duration of postoperative analgesia, PENG block achieved more analgesic effect and easier positioning than S-FICB for SA in patients who had hip fractures surgery.
1. Introduction
Hip fractures are a typical orthopedic emergency that should be operated on within 72 hours for a better outcome [Citation1]. It mainly occurs among older people or as a result of high-impact trauma and is correlated with substantial mortality and morbidity [Citation2,Citation3]. Pain in hip fracture patients, either preoperative or postoperative, is more pronounced, especially when the joint is immobile.
Neuraxial anesthesia is a widely accepted method for reducing perioperative adverse effects in elderly individuals either with low-dose local anesthetic or in combination with different adjuvants [Citation4]. Also, spinal anesthesia (SA) is the method of choice in orthopedic surgery due to its rapid onset of analgesia, anesthesia, and economic issues [Citation5].
Severe hip fracture pain usually results in difficulty while attempting to assume an SA position, hence a problem accessing the subarachnoid space [Citation6]. Insufficient surgical analgesia may impede limb mobility, impeding healing and leading to opioid overuse [Citation7].
In these populations, a successful perioperative analgesic that lowers the need for opioids and their side effects is critical [Citation8].
To provide analgesia for hip fractures, anesthesiologists frequently employ the fascia iliaca compartment block (FICB), which targets the femoral nerve (FN), obturator nerve (ON), and lateral femoral cutaneous nerve (LFCN) to achieve immediate and postoperative analgesia for hip fractures [Citation9]. Also, the pericapsular nerve group (PENG) block, which explicitly affects the articular branches of the FN, ON, and perhaps accessory obturator nerve (AON), was recently reported [Citation10]. Hence diminishing reliance on opioids and augmenting patients comfort [Citation9,Citation11].
Nevertheless, there is a shortage of comparative research comparing FICB and PENG regarding the simplicity of positioning during neuraxial anesthesia. To our knowledge, there is limited data in the literature that evaluated the effectiveness of adding dexamethasone to ropivacaine in both PENG and S-FICB.
As a result, we decided to conduct a prospective randomised double-blind trial to assess the analgesic efficacy of S-FICB block and PENG in patients with hip fractures with respect to facilitate the optimal sitting position for SA.
2. Methods
This randomized prospective double-blinded trial included 60 cases aged ≥40 years old and ASA I-III with hip fracture and scheduled for surgical procedure under SA. The trial was done from March 2023 to December 2023. The trial was conducted at Benha University Hospitals.
Each patient supplied informed written consent. The study was carried out with the Benha University Hospitals Ethical Committee (approval (RC 11 March 2023), and registration of clinicaltrials.gov (ID: NCT05987254).
Patients who declined to participate, any contraindications to SA or peripheral nerve blocks, chronic opiates use, and patients with considerable cognitive impairment were excluded. Patients who experienced mild pain when sitting independently numeric rating scale (NRS) at rest less than 4 without assistance were also excluded from the study.
3. Randomization and blindness
Computer‐generated randomization numbers were used to assign 60 cases equally into two groups. Group I (S-FICB group) received ultrasound (US) guided S-FICB, and group II (PENG group) received US-guided PENG. A nurse not involved in the study utilized opaque, sequentially numbered, and hermetically sealed envelopes to ensure a random assignment. The allocation ratio was 1:1 in a parallel manner. Patients and outcome evaluators were blinded to the study groups.
4. Preoperative
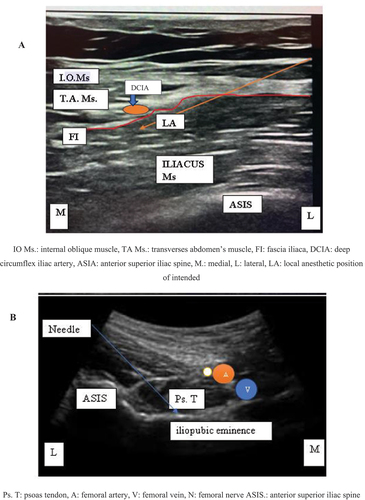
Before the SA, all patients were transported to the operating room, where essential monitoring such as noninvasive blood pressure, pulse oximetry and electrocardiograms were applied. NRS was utilized to document pre-procedure discomfort during rest and movement (15° passive elevation) of the afflicted limb [10 = the worst suffering possible; 0 = zero pain]. The blocks were done while the cases were supine by the same operator, adhering to rigorous sterile protocols. After coating the area to be blocked with a solution of 5% povidone-iodine and 70% ethyl alcohol, it was draped. A high-frequency linear US probe (5–10 MHz) for S-FICB and a curvilinear probe (3–5 MHz) for PENG block was positioned transversely over the anterior superior iliac spine (ASIS) before being aligned to determine the locations of the subsequent landmarks:
Group S-FICB: received ropivacaine 0.25% 23 ml +2 ml of 8 mg dexamethasone. Landmarks included Fascia lata, fascia iliaca, internal oblique muscle, sartorius muscle, iliacus muscle, and bone. Injection was performed at the interface of the fascia iliaca and iliacus muscle.
Group PENG: received 23 ml of ropivacaine 0.25% + 2 ml of dexamethasone 8 mg. The anterior inferior iliac spine, pubic ramus, psoas muscle and tendon, and femoral artery were all landmarks. The injection site was located between the pubic ramus and the psoas tendon in the fascial plane .
Analgesia was assessed using NRS at rest and during passive limb elevation, twenty minutes after the blocks. It was determined that if a patient’s NRS were greater than five, 50 mg of tramadol would be administered intravenously (IV) until the NRS equal or below four; only then they would be permitted to assume a seated position for subarachnoid block using 12.5 mg bupivacaine 0.5% in addition to 20 µg fentanyl.
In case NRS did not reach four or less after 50 mg of IV tramadol, patients were excluded from our trial and shifted to general anesthesia.
On a scale from zero to three, the ease of spinal positioning (EOSP) was evaluated as follows: zero indicated immobility, one suggested the patient required assistance for positioning due to pain-induced abnormal posturing, two showed mild discomfort, but no support was needed for positioning, and three indicated an ideal condition in which the patient could position himself painlessly. NRS scores, scores for EOSP, the time to first analgesic request and the number of tramadol doses used were recorded post-block. Patient satisfaction was measured after 24 hours utilizing a Likert scale with five points: “very dissatisfied,” “dissatisfied,” “unsure,” “satisfied,” and “very satisfied”.
The primary outcome was EOSP 20 minutes after the block. Twenty minutes following block, NRS during both rest and movement, postoperative NRS for 24 hours, the time to first analgesic request, number of tramadol dosage, patient satisfaction, and complications associated with block were considered secondary outcomes.
5. Sample size calculation
The sample size calculation was done by G*Power 3.1.9.2 (Universitat Kiel, Germany). According to a previous study [Citation12], the mean ± SD of EOSP (the primary outcome) was 2.348 ± 0.504 in the PENG group and 1.754 ± 0.95 in the S-FICB group. The sample size was based on the following considerations: 0.781 effect size, 95% confidence limit, 80% power of the study, and three cases were added to each group to overcome dropout. Therefore, we recruited 30 patients in each group.
6. Statistical analysis
Statistical analysis was conducted using SPSS v28, developed by IBM and located in Armonk, NY, USA. The Shapiro-Wilks test and histograms were employed to determine if the data was normally distributed. The quantitative parametric data was examined using an unpaired student t-test and was provided as mean and standard deviation (SD). The median and interquartile range (IQR) were used to present quantitative non-parametric data, which were examined using the Mann Test. For qualitative variables, we used Chi-square or Fisher’s exact tests as needed and displayed the results as percentages and frequencies. Significant statistical analysis was defined as a two-tailed p value ≤ 0.05.
7. Results
In this study, eligibility was dedicated to 102 participants; 31 participants did not match the eligibility requirements, and 11 patients chose not to participate in the research. The remaining 60 cases were randomly assigned to two groups of equal size (30 cases per group). Every assigned case was observed and statistically evaluated.
Age, ASA physical status, sex, weight, height, and BMI were matched between the two groups.
Table 1. Demographic data of the studied groups.
NRS was significantly lower in the PENG group both at rest and movement 20 min post-block compared to S-FICB (p-value ≤0.05), whereas the number of patients who required tramadol (post-block) was comparable between both groups (p-value >0.05). The EOSP had a mean value (± SD) of 1.4 (± 0.68) in the S-FICB group and had a mean value (± SD) of 2.2 (± 0.82) in the PENG group with a mean difference (95%CI) of −0.8 (−1.19: −0.41). The EOSP in the PENG group was significantly greater than in the S-FICB group (p-value <0.001).
Table 2. Comparison of NRS at rest in the S-FICB and PENG group patients preoperatively and at various time points postoperatively.
Although NRS postoperatively was significantly lower in PENG at 8 h, it was statistically insignificant between both groups at PACU, 2 h, 4 h,12, and 24 h postoperatively (p-value >0.05).
Figure 3. Comparison of NRS at various time points postoperatively in patients assigned to the S-FICB and PENG groups.
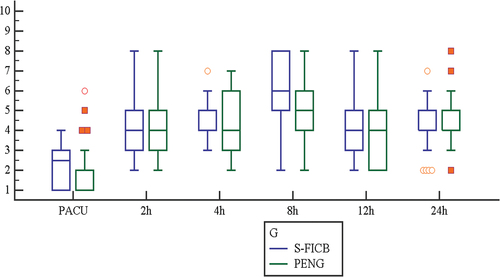
The time to first analgesic request was a mean value (± SD) of 8.58 (± 2.34) h in the S-FICB group and with a mean value (± SD) of 8.93 (± 2.19) h in the PENG group. The time for the first analgesic request was insignificantly different between groups (p-Value 0.552). The number of tramadol doses had a mean value (± SD) of 2.73 (± 2.02) in the S-FICB group and with a mean value (± SD) of 2. 3 (± 1.35) in the PENG group. The number of tramadol doses was comparable between both groups (p-value 0.37).
Table 3. Time to first analgesic request and number of tramadol doses in the studied groups.
There were 22 (73.33%) satisfied and 8 (26.67%) unsatisfied in the S-FICB group. There were 27 (90%) satisfied and 3(10%) unsatisfied in the PENG group. Patients’ satisfaction was insignificantly differed between the two groups (P = 0.181).
8. Discussion
Hip fractures are common orthopedic problems after high-impact trauma [Citation13]. Fixation of these fractures as rapidly as possible is required to decrease the incidence of fat embolism and other complications. Regional anesthesia sub arachidonic block (SAB) is most commonly used for providing anesthesia to repair these fractures as part of adequate perioperative analgesia and enhanced functional recovery after hip surgery [Citation14].
The advance of the PENG block or S-IFICB and their combination were used in many studies because the anterior and superolateral hip joint capsule is rich with nociceptive fibers and mechanoreceptors in the posterior capsule [Citation15]. That causes discomfort during movement and at rest in patients with hip fractures.
Positioning for SAB is essential for successful spinal anesthesia. Pain in hip fracture patients leads to improper positioning for spinal anesthesia, which makes SAB more difficult. The addition of peripheral nerve blocks is being advised by the National Institute for Health and Care Excellence (NICE) when paracetamol and opioids are not adequate for pain relief, which in turn decreases opioid use and its adverse effects [Citation16].
Regional techniques, like FN block and 3-in-1 FN block, decreased pain and improved patient comfort and proper positioning for SAB [Citation16–18]. However, analgesia from these blocks is Partially satisfactory for patients and surgeons [Citation19,Citation20]; furthermore, existing literature indicates that the articular branches of these nerves are blocked inconsistently [Citation21,Citation22].
According to earlier anatomic investigations, the anterior hip capsule is innervated by articular branches of the FN, ON, and the AON. These nerves can be inhibited by a PENG block [Citation9].
FICB and PENG block are widely employed regional procedures for spinal positioning analgesia and postoperative pain reduction. For patient comfort, both the PENG and FICB procedures offer adequate analgesia; however, most of the data about the PENG block is presented in the form of case series [Citation22–24].
S-FICB is an emerging methodology, and the available comparative data cannot provide a definitive conclusion. S-FICB reliably inhibits the three nerves in comparison to the infrainguinal method [Citation25,Citation26]. Kumar et al. [Citation27] reported that S-FICB exhibits enhanced postoperative analgesic efficacy in contrast to the intra-operative technique of FICB while also requiring a much-reduced amount of morphine during the initial twenty-four hours.
In the infra-inguinal method, large amounts of LA (40–60 ml) have been utilised to achieve a successful compartmental block with the FICB [Citation28]. However, research on the S-FICB method has shown contradictory findings about the optimal/effective volume. Based on dissection and computed tomography (CT) scan results from a cadaveric investigation of FICB, it was hypothesized that 40 ml of injectate might reach the FN, ON, and LFCN [Citation29].
Yamada et al. [Citation30] investigated the minimal adequate volume of LA in SFICB. 15.01 ml and 26.99 ml were determined to be the EV50 and EV95 of ropivacaine 0.25% for S-FICB, respectively.
In their comparative analysis of S-FICB and PENG block, Bhattacharya et al. [Citation31] determined that 20 ml of 0.25% levobupivacaine administered to both groups was efficacious.
The PENG block, recently documented as a regional analgesic method, administers a single injection to the articular branches supplying the anterior hip joint. This technique was inspired by a cadaveric study that demonstrated that the accessory obturator nerve and the femoral and obturator nerves significantly contribute to the innervation of the anterior hip joint. Consequently, it is designed to conserve motor resources; this is its primary distinction from FICB. Since its initial description, a considerable body of literature has been devoted to publishing case reports and series that emphasize PENG block’s remarkable analgesic benefits for perioperative pain management during hip surgery [Citation23,Citation24,Citation32].
Ropivacaine, a long-acting local anesthetic with a lower incidence of cardiotoxicity and more sensory block compared to bupivacaine, leads to early mobilization and prevents complications of prolonged recumbency, especially postoperative pulmonary complications and venous thromboembolism. This has made ropivacaine a commonly used local anesthetic in peripheral nerve blockade [Citation33] with the addition of local anesthetic adjuvant like dexamethasone, which was studied in PNB and found to improve the quality and effectiveness of PNB [Citation23].
To our knowledge, this is the first study that evaluated the effectiveness of adding dexamethasone to ropivacaine in both PENG and S-FICB.
In this study, both blocks were performed using 23 ml of ropivacaine 0.25% + 2 ml of 8 mg dexamethasone. It highlighted the positive outcomes of peripheral nerve blocks with dexamethasone in maintaining optimal management of postoperative pain, faster motor recovery, and reduction in opioid usage [Citation34].
In our study, we observed that PENG block provides superior analgesia than S-FIB in both rest (p-value 0.015*) and dynamic hip movement 20 min after block (p-value 0.010*) and EOSP for spinal anesthesia (p-value <0.001*). We observed that the time for the requirement of rescue analgesia was insignificantly different in both the PENG and S-FIB block groups. Although NRS postoperatively was lower in the PENG group, it was statistically insignificant. Also, the number of analgesic doses [tramadol 50 mg] required was insignificantly different between both groups in the PENG group (2.3 ± 1.35) compared to (2.7 ± 2.02) in the S-FICB group in 1st 24 h postoperative period.
The time until the initial request for analgesics was utilized to determine the duration of analgesia in our study. The duration was comparable between the PENG and SFICB groups.
An additional double-blinded randomized comparison research conducted by Shankar et al. [Citation12] found that the S-FICB and PENG had equal durations of the block (7.85 and 8.16 hours, respectively)
Jadon et al. [Citation9] also compare S-FICB versus pericapsular PENG for EOSP during spinal anesthesia.
Contrary to our result, patients have more prolonged postoperative analgesia, and the time for first rescue analgesia was after 12, and this may be due to the residual effect of using dexmedetomidine infusion during surgery in their study.
Girón-Arango et al. [Citation33] performed PENG block on 5 patients having hip fractures. Their study showed reduced pain scores without quadriceps weakness in all patients.
Regarding our results in this study of 30 patients of each group, we recommend using USG PENG block for perioperative analgesia in patients with hip fractures as it provides better analgesia and EOSP for central neuraxial block than S-FICB.
9. Limitation of our study
Assessment of the VAS score is subjective and will depend on patient understanding. The duration of the hospital stay was not recorded. A small sample size, sensory pattern, and nerve blockade were better assessed more objectively.
10. Conclusions
Although each block provides comparable duration of postoperative analgesia, PENG block achieved more analgesic effect and easier positioning than S-FICB for SA in patients who had hip fractures surgery.
Author contributions
All authors participated in preparing this clinical trial and approved of the work as it is being submitted. All authors read and approved the final manuscript.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Clinical trial registration
The research was conducted after the approval of the Ethical Committee Benha University Hospitals (approval code: RC 11 March 2023) and registration of clinicaltrials.gov (ID: NCT05987254).
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki. Each patient supplied informed written consent. The study was carried out with the approval of the Benha University Hospitals Ethical Committee (approval code: RC 11 March 2023), registration of clinicaltrials.gov (ID: NCT05987254).
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Allahabadi S, Roostan M, Roddy E, et al. Operative management of hip fractures within 24 hours in the elderly is achievable and associated with reduced opiate use. Geriatr Orthop Surg Rehabil. 2022;13:21514593221116331. doi: 10.1177/21514593221116331
- Schnell S, Friedman SM, Mendelson DA, et al. The 1-year mortality of patients treated in a hip fracture program for elders. Geriatr Orthop Surg Rehabil. 2010;1(1):6–14. doi: 10.1177/2151458510378105
- Lloyd R, Baker G, MacDonald J, et al. Co-morbidities in patients with a hip fracture. Ulster Med J. 2019;88(3):162–166.
- Sivevski AG, Karadjova D, Ivanov E, et al. Neuraxial anesthesia in the geriatric patient. Front Med. 2018;5:254. doi: 10.3389/fmed.2018.00254
- Capdevila X, Aveline C, Delaunay L, et al. Factors determining the choice of spinal versus general anesthesia in patients undergoing ambulatory surgery: results of a multicenter observational study. Adv Ther. 2020;37(1):527–40. doi: 10.1007/s12325-019-01171-6
- Diakomi M, Papaioannou M, Mela A, et al. Preoperative fascia iliaca compartment block for positioning patients with hip fractures for central nervous blockade: a randomized trial. Reg Anesth Pain Med. 2014;39(5):394–8. doi: 10.1097/AAP.0000000000000133
- Gan TJ. Poorly controlled postoperative pain: prevalence, consequences, and prevention. J Pain Res. 2017;10:2287–98. doi: 10.2147/JPR.S144066
- Kaye AD, Urman RD, Rappaport Y, et al. Multimodal analgesia as an essential part of enhanced recovery protocols in the ambulatory settings. J Anaesthesiol Clin Pharmacol. 2019;35(5):S40–s5. doi: 10.4103/joacp.JOACP_51_18
- Jadon A, Mohsin K, Sahoo RK, et al. Comparison of supra-inguinal fascia iliaca versus pericapsular nerve block for ease of positioning during spinal anaesthesia: a randomised double-blinded trial. Indian J Anaesth. 2021;65(8):572–8. doi: 10.4103/ija.IJA_417_21
- Vamshi C, Sinha C, Kumar A, et al. Comparison of the efficacy of pericapsular nerve group block (PENG) block versus suprainguinal fascia iliaca block (SFIB) in total hip arthroplasty: a randomized control trial. Indian J Anaesth. 2023;67(4):364–9. doi: 10.4103/ija.ija_311_22
- Mariem K, Mohamed AM, Ameur A, et al. Pericapsular nerve group block versus fascia iliaca block for perioperative analgesia in hip fracture surgery: a prospective randomized trial. Pan Afr Med J. 2023;46. doi: 10.11604/pamj.2023.46.93.41117
- Shankar KSR, Ashwin AB, Nandini U, et al. Comparative study of ultrasound guided PENG [pericapsular nerve group] block andFIB [fascia iliaca block] for positioning and postoperative analgesia prior to spinal anaesthesia for hip surgeries: prospective randomised comparative clinical study. Indian J Anesth Analg. 2020;7(3):798–803. doi: 10.21088/ijaa.2349.8471.7320.22
- Brauer CA, Coca-Perraillon M, Cutler DM, et al. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302(14):1573–1579. doi: 10.1001/jama.2009.1462
- Sandby-Thomas M, Sullivan G, Hall JE. A national survey into the peri-operative anaesthetic management of patients presenting for surgical correction of a fractured neck of femur. Anaesthesia. 2008;63(3):250–8. doi: 10.1111/j.1365-2044.2007.05328.x
- Mosaffa F, Taheri M, Manafi Rasi A, et al. Comparison of pericapsular nerve group (PENG) block with fascia iliaca compartment block (FICB) for pain control in hip fractures: a double-blind prospective randomized controlled clinical trial. Orthop Traumatol Surg Res. 2022;108(1):103135. doi: 10.1016/j.otsr.2021.103135
- Freeman N, Clarke J. Perioperative pain management for hip fracture patients. Orthop Trauma. 2016;30(2):145–52. doi: 10.1016/j.mporth.2016.03.012
- Haines L, Dickman E, Ayvazyan S, et al. Ultrasound-guided fascia iliaca compartment block for hip fractures in the emergency department. J Emerg Med. 2012;43(4):692–7. doi: 10.1016/j.jemermed.2012.01.050
- Unneby A, Svensson O, Gustafson Y, et al. Femoral nerve block in a representative sample of elderly people with hip fracture: a randomised controlled trial. Injury. 2017;48(7):1542–9. doi: 10.1016/j.injury.2017.04.043
- Beaudoin FL, Haran JP, Liebmann O, et al. A comparison of ultrasound-guided three-in-one femoral nerve block versus parenteral opioids alone for analgesia in emergency department patients with hip fractures: a randomized controlled trial. Acad Emerg Med. 2013;20(6):584–91. doi: 10.1111/acem.12154
- Guay J, Parker MJ, Griffiths R, et al. Peripheral nerve blocks for hip fractures. Cochrane Database Syst Rev. 2017;5:Cd001159. doi: 10.1002/14651858.CD001159.pub2
- Birnbaum K, Prescher A, Hessler S, et al. L’innervation sensitive de l’art. coxofémorale- Étude anatomique. Surg Radiol Anat. 1997;19(6):371–375. doi: 10.1007/BF01628504
- Gerhardt M, Johnson K, Atkinson R, et al. Characterisation and classification of the neural anatomy in the human hip joint. Hip Int. 2012;22(1):75–81. doi: 10.5301/HIP.2012.9042
- Acharya U, Lamsal R. Pericapsular nerve group block: an excellent option for analgesia for positional pain in hip fractures. Case Rep Anesthesiol. 2020;2020:1830136. doi: 10.1155/2020/1830136
- Morrison C, Brown B, Lin DY, et al. Analgesia and anesthesia using the pericapsular nerve group block in hip surgery and hip fracture: a scoping review. Reg Anesth Pain Med. 2021;46(2):169–75. doi: 10.1136/rapm-2020-101826
- Brown B, Lin D, Saies A, et al. The pericapsular nerve group block for hip fracture surgery: a prospective case series. J Anesth Clin Res. 2021;12:999.
- Vermeylen K, Desmet M, Leunen I, et al. Supra-inguinal injection for fascia iliaca compartment block results in more consistent spread towards the lumbar plexus than an infra-inguinal injection: a volunteer study. Reg Anesth Pain Med. 2019;44(4):483–491. doi: 10.1136/rapm-2018-100092
- Kumar K, Pandey RK, Bhalla AP, et al. Comparison of conventional infrainguinal versus modified proximal suprainguinal approach of fascia iliaca compartment block for postoperative analgesia in total hip arthroplasty. A prospective randomized study. Acta Anaesthesiol Belg. 2015;66(3):95–100.
- Dulaney-Cripe E, Hadaway S, Bauman R, et al. A continuous infusion fascia iliaca compartment block in hip fracture patients: a pilot study. J Clin Med Res. 2012;4:45–48. doi: 10.4021/jocmr724w
- Vermeylen K, Soetens F, Leunen I, et al. The effect of the volume of supra-inguinal injected solution on the spread of the injectate under the fascia iliaca: a preliminary study. J Anesth. 2018;32(6):908–13. doi: 10.1007/s00540-018-2558-9
- Yamada K, Inomata S, Saito S. Minimum effective volume of ropivacaine for ultrasound-guided supra-inguinal fascia iliaca compartment block. Sci Rep. 2020;10(1):21859. doi: 10.1038/s41598-020-79059-7
- Bhattacharya A, Bhatti T, Haldar M. ESRA19-0539 pericapsular nerve group block–is it better than the rest for pain relief in fracture neck of femur? Reg Anesth Pain Med. 2019;44:A116–A.
- Rocha‐Romero A, Arias‐Mejia K, Salas‐Ruiz A, et al. Pericapsular nerve group (PENG) block for hip fracture in the emergency department: a case series. Anaesthesia Rep. 2021;9(1):97–100. doi: 10.1002/anr3.12118
- Girón-Arango L, Peng PWH, Chin KJ, et al. Pericapsular Nerve Group (PENG) block for hip fracture. Reg Anesth Pain Med. 2018;43:859–863. doi: 10.1097/AAP.0000000000000847
- Albrecht E, Kern C, Kirkham KR. A systematic review and meta-analysis of perineural dexamethasone for peripheral nerve blocks. Anaesthesia. 2015;70(1):71–83. doi: 10.1111/anae.12823