ABSTRACT
Background
Improper management and late detection of complications, especially peri-operative acute kidney injury (AKI), could result in higher morbidity and mortality rates. This work was aimed at confirming the tidal volume challenge (TVC) test’s predictability while performing laparoscopic abdominal surgery for early postoperative AKI and intra-operative hypotension.
Methods
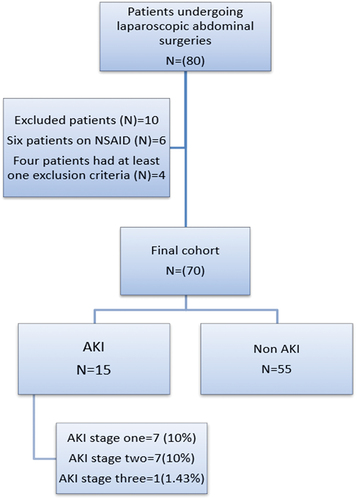
Our prospective observational study involved 70 cases whose age ranged between 18 and 65 years, American Society of Anesthesiologists (ASA) I and ASA II going through general anesthesia (GA) for laparoscopic abdominal elective surgery. Patients went through a categorization into AKI or Non-AKI according to the worst Kidney Disease: Improving Global Outcomes (KDIGO) classification according to serum creatinine and urine output that are measured at 0, 24 and 48h.
Results
TVC exhibited significant correlation with the AKI development with the OR of 2.3, 95% CI, p = 0.052, while the exposure index was deemed to be an AKI development risk factor with the OR of 1.0, 95% CI, p = 0.034. However, baseline neutrophil gelatinase-associated lipocalin in urine (UNGAL) showed insignificant association with the AKI development with the OR 1.04 and p = 0.366. The relationship between TVC and hypotension frequency was estimated using linear regression. The regression showed that there exists a positive significant relation between these two parameters; as hypotension frequency increases, TVC increases as well with a coefficient estimate of 0.5.
Conclusions
AKI represents complication after laparoscopic abdominal surgery. To avoid peri-operative renal impairment, the limiting exposure index should be considered. Our work introduces the TVC test for AKI prediction in laparoscopic abdominal surgeries.
1. Introduction
The scope of laparoscopic surgeries is increasing. Recently, we can almost operate on any abdominal organ using laparoscopy. Laparoscopy has many potential risks and complications which require early detection and prevention. Patients’ extreme position for long period, carbon dioxide (CO2) insufflation consequences and unexpected organ tissue damage should all be monitored and considered by a vigilant anaesthesiologist [Citation1].
The laparoscopic insufflation with CO2 can cause cardiovascular depression, causing hypotension and bradycardia up to cardiac arrest through several mechanisms, including vagal-mediated cardiovascular reflex, preload decrease, as well as venous return due to pneumoperitoneum (PP) [Citation2].
Acute kidney injury (AKI) incidence following laparoscopic abdominal surgical procedure is 35.9% as shown in a previous study, and this is attributed to the PP, resulting in renal insufficiency through hypercapnia, increased intra-abdominal pressure and renin-angiotensin-aldosterone system [Citation3].
The low volume status exhibits a substantial impact on AKI following the surgical procedure. However, multiple theories have emerged to explain the higher AKI occurrence rates among cases that undergo laparoscopic surgical procedures, addressing that an increased intra-abdominal pressure could result in an elevated renal resistive index [Citation4].
Several indicators could be utilized to assess the intra-operative volume status, involving inferior vena cava, stroke volume variation (SVV) as well as pulse pressure variation (PPV). Although they could exhibit reliability, they are linked to some disadvantages, involving complexity as well as prolonged time. Moreover, they need skilled clinicians along with advanced equipment [Citation5].
The tidal volume challenge (TVC) test represents a recently developed tool utilized to assess the volume status. It has been validated as a dependable tool specifically for cases that undergo neurosurgery. Nevertheless, to the best of our knowledge, it has not been utilized for hypotension as well as AKI prediction in laparoscopic procedures. We propose that simulating the impact of elevated intra-abdominal pressure by transiently utilizing the TVC test may assist in identifying individuals possessing greater chances for post-operative AKI [Citation6].
The TVC test/abdominal insufflation negative events could be primarily attributed to decreased venous compliance in certain cases, resulting in blood mobilization towards the peripheral venous system along with a decrease in venous elasticity. As a result, the passive blood recoil to the heart, which is crucial for preserving hemodynamic stability as well as organ perfusion, is reduced. This exacerbates the impact of elevated intra-abdominal or intra-thoracic pressure. Such a mechanism has been investigated in orthostatic hypotension [Citation7].
This work was aimed at confirming the TVC test’s predictability while performing laparoscopic abdominal surgery for early postoperative AKI as well as intra-operative hypotension.
2. Materials and methods
Our prospective observational study involved 70 consecutive cases whose ages ranged between 18 and 65 years old, both genders, American Society of Anesthesiologists (ASA) I and II undergoing general anesthesia (GA) for laparoscopic abdominal elective surgery. The study was done from October 2020 to March 2023 after the approval from the Ethical Committee Cairo University Hospitals, Cairo, Egypt (approval code: MD-302-2021). All participants were asked to fill in an informed consent.
We excluded patients with cardiovascular diseases such as permanent atrial fibrillation as well as valvular heart disease, cardiac arrhythmias and right ventricular failure; we also excluded those with pulmonary diseases such as chronic obstructive pulmonary disease, airway asthma or a prolonged smoking history, and also those with kidney impairment, intracranial hypertension, and cases consuming non-steroidal anti-inflammatory drug (NSAID) for a week before the surgical procedure.
All participants went through a comprehensive medical history and clinical examinations.
Venous along with arterial accesses was established to monitor continuous invasive blood pressure after reaching the operating room as well as prior to anesthesia induction. The general Electric (GE) monitor was used to monitor non-invasive blood pressure, invasive radial arterial blood pressure, pulse oximetry, heart rate (HR), electrocardiogram, maximum airway pressure, plateau pressure (Ppl) and driving pressure (Ppl – positive end expiratory pressure [PEEP]) and the partial pressure of carbon dioxide in the end-tidal gas (PETCO2). PPV was recorded with invasive arterial pressure (IAP) monitor. Following the zeroing of arterial transducer, a flush test was conducted to make sure that the arterial pressure measurement system was properly damped. Monitoring the arterial pulse pressure wave was simultaneously done through the patient monitor (GE Healthcare). Stroke volume was measured using electrical cardiometry ICON, which is OSYPKA medical USA made portable, noninvasive handheld device for the continuous measurement of different hemodynamic parameters using four skin sensors placed on upper neck(A), root of the neck(B) and the left thorax (C and D) which permits continuous measurement of changes in the thoracic electrical bioimpedance. The application of advanced filtering techniques, Electrical Cardiometry™ (EC™), is isolating the impedance changes corresponding to varying blood flow.
The patients received Ringer solution at a dosage of 5 to 7 ml/kg/h for fluid maintenance by the blinded anaesthesiologist, and GA was induced after pre-oxygenation for 2 min by intravenous (IV) midazolam (0.03 mg/kg), fentanyl (1 µg/kg), atracurium (0.5 mg/kg) and propofol (2 mg/kg). After reaching appropriate muscle relaxation, Tracheal intubation was performed, and the GE anaesthesia machine was connected for mechanical ventilation with pressure-controlled ventilation-volume guaranteed (PCV-VG) mode with these settings: tidal volume (Vt) of 6 ml/kg PBW; PETCO2 remain within the 35–45 mmHg range with an inspired oxygen fraction 0.5 and a fresh gas flow 2 L/min of oxygen and air; PEEP to be maintained between three to five cmH2O and SpO2 to be kept above 95%. Anesthesia maintenance was performed utilizing fentanyl (1–5 µg/kg/hr), atracurium (0.12–0.9 mg/kg/hr) as well as isoflurane (1–2%). Anesthetic depth was maintained during the operation via adjusting the end-tidal isoflurane concentration.
Simultaneously, the adequate vaso-active drugs’ administration (atropine as well as nor-adrenaline) had been for maintaining HR as well as MAP at around 20% of the base value. We recorded PPV, SVV, MAP, HR, and maximum airway pressure after intravenous anesthesia induction. Before starting the operation in supine or Trendelenburg or reverse Trendelenburg position with angle incline between 15° and 30° and before abdominal gas insufflation with pressure ranging between 12 mmHg and 16 mmHg in the supine position, the patient was ventilated with PCV-VG with Vt 6 ml/kg PBW, a maximum airway pressure of 30 mmH2O and PEEP 3 to 5 cmH2O for 1 min. We recorded baseline measurements (T0) involving PPV (PPV6) as well as stroke volume (SV) (SV6). We performed TVC by temporarily raising Vt (from 6 to 8 ml/kg PBW for a minute) then recorded another PPV (PPV 8) and SV (SV8) measurement after 1 min (T1). The PPV value change (ΔPPV6–8) as well as the change in stroke volume (SV6–8) was also calculated. Vt rose again to 10 ml/kg PBW, as well as another measurement value of PPV (PPV 10), SV (SV10), SVV (SV8–10) and (ΔPPV8–10) was documented after another 1 min (T2). After completing TVC, the tidal volume was lowered to 6 ml/kg PBW again, and another measurement of PPV (PPVT3) and (SVT3) was recorded after another 1 min (T3).
From the beginning of the operation, collecting three consecutive blood and urine samples was accomplished at 0, 24, as well as 48 h to determine serum creatinine and UNGAL. We also collected urine output every 30 min throughout surgery and for 3 h and collected and measured urine volume every 3 h for 24 h after surgery.
Kidney Disease: Improving Global Outcomes (KDIGO) was utilized for diagnosing AKI [Citation7]. For AKI staging, cases underwent classification according to the worst KDIGO based on serum creatinine or UO. Since UO was only available within 24 h of the day, the following changes were made to the UO standard: ≥0.5 ml/kg/h, there is no AKI; 0.3–0.5 ml/kg/h is (stage 2); < 0.3 ml/kg/h (stage 3). Therefore, AKI will be defined as UO below 0.5 ml/kg/hr or as > or = 1.5 times increase of serum creatinine or > 0.3 mg/dl increase of baseline serum creatinine.
The primary outcome was the prediction of the tidal volume challenge (TVC) tests for early postoperative AKI and intra-operative hypotension, while secondary outcomes were UNGAL and exposure index.
3. Sample size calculation
The sample size was calculated using MedCalc software version 14 (MedCalc Software bvba, Ostend, Belgium) to detect the area under the receiver operating characteristic curve (AUC) of 0.75, setting the null hypothesis AUC at 0.50 and taking into consideration that the incidence of post-operative AKI after laparoscopic surgeries was 35% (1), and we calculated a minimum number of 61 patients which would be increased to 70 cases to compensate for possible dropouts for study power 90% and an alpha error of 0.05.
4. Statistical analysis
The data went through a statistical analysis utilizing SPSS v26 (IBM Inc., Chicago, IL, USA). The quantitative variables were displayed as mean as well as standard deviation (SD) then compared among the two groups utilizing unpaired Student’s t-test. The qualitative variables were displayed as frequency as well as percentage (%) then went through analysis of the chi-square or Fisher’s exact test when appropriate. A two-tailed p value of less than 0.05 was deemed to exhibit a statistical significance.
5. Results
Sex, ASA classification and type of operation (upper and lower abdominal surgeries) exhibited significant variations among AKI as well as non-AKI groups. However, the remaining patient demographic or clinical characteristics did not exhibit significant variations among the AKI as well as non-AKI groups. The patients’ age within the AKI along with non-AKI groups did not exhibit significant variations. Baseline serum creatinine, co-morbid conditions and baseline vital signs exhibited comparable values within both groups.
Table 1. Patients characteristics, clinical characteristics, comorbid conditions, and type of operation.
The serum creatinine returned to baseline at 48 h within the two groups. The median UNGAL level of AKI patients exhibited an increase from 10 ng/mL at time 0 to 39 ng/mL at 48 h following the surgical procedure. The median UNGAL level exhibited greater values within the AKI group as opposed to the non-AKI group at 48 h: median 39 (13.0, 65.0) vs. 11.6 (4.0, 28.0) ng/mL.
TVC exhibited a marginally significant correlation with the AKI development with the OR of 2.3, 95% CI, p = 0.052, while the exposure index which is the product of inflation time and intra-abdominal pressure (inflation time x IAP) was a risk factor of AKI development with the OR of 1.0, 95% CI, p = 0.034. However, baseline UNGAL showed insignificant association with AKI development with OR 1.04 and p = 0.366.
Table 2. Analysis of intra-operative predictors.
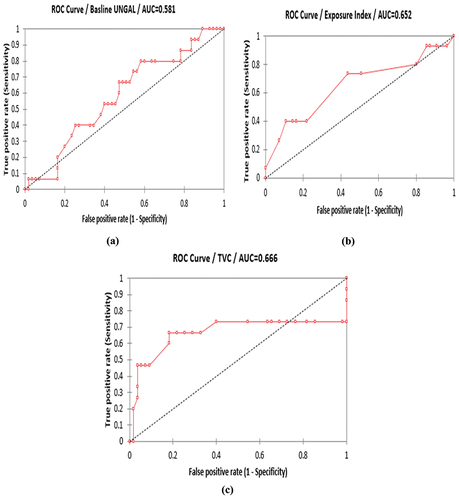
Regarding baseline UNGAL, AUC was 0.581; 95% CI (−0.076 to 0.238), 80% sensitivity [53.9, 93.5] and 41.8% specificity [29.8, 55] with cut-off value (> or = 7.0) with PPV 27.3% and NPV 88.5%. Regarding exposure index, AUC was 0.651; 95% CI (−0.023 to 0.327), 73.3% sensitivity [47.5, 89.3] and 56.4% specificity [43.3, 86.6] with cut-off value (> or = 1800) with PPV 31.4% and NPV 88.6%. Regarding TVC, AUC was 0.66; 95% CI (−0.052 to 0.384), 66.7% sensitivity [41.5, 84.8] and 81.8% specificity [69.4, 89.9] with cut-off value (> or = 3.8) with PPV 45.5% and NPV 89.6%.
Figure 2. The AUC for (a) baseline neutrophil gelatinase-associated lipocalin in urine (UNGAL), (b) exposure index, (c) tidal volume challenge (TVC).
The relationship between TVC and hypotension frequency was estimated using linear regression. The regression showed that there exists a positive significant relation between these two parameters; as hypotension frequency increases, TVC increases as well with a coefficient estimate of 0.5. Further correlation between TVC and hypotension was found to be rather weak with a value of 0.3. (
Table 3. Relationship between TVC and hypotension frequency.
6. Discussion
This study addressed the TVC predictability for both AKI and intra-operative hypotension; it also showed the correlation between baseline UNGAL as well as exposure index with AKI after laparoscopic abdominal surgical procedure. Our findings also addressed that both TVC and high exposure index are significant predictors for AKI and high TVC values are associated with high frequency of hypotension intra-operatively. The AKI occurrence within our research exhibited 21.4% which is higher than in previous studies. For example, Sharma et al. [Citation8] found that the incidence of AKI following laparoscopic bariatric surgery in morbidly obese patients ranged from 2.3 to 2.9%.
Nevertheless, this study did not utilize urine output as diagnostic criteria. We utilized standard KDIGO criteria, involving serum creatinine as well as urine output criteria that possibly enabled broader AKI identification.
Our research introduced a recent test “TVC” that was aimed at predicting the occurrence of oliguria and AKI. The previous studies proposed cut-off value of 3.5% for TVC to be a positive test in peri-operative fluid responsiveness assessment as supposed by Myatra et al. [Citation9] and Messina et al. [Citation6] found that TVC is a good predictive test to early post-operative AKI with cut-off value > or = 3.8% a higher value than proposed previously by Myatra et al. [Citation9] While it was not a good test in predicting hypotension which can be attributed to the good fluid management done by blinded anesthesiologist or the conservative local protocol of increasing IAP and limiting it to less than 16 mmHg. The previous studies focused on inflation time and intra-abdominal pressure separately proposing that each increases the risk of AKI development [Citation8].
We tested a relatively new parameter called exposure index which is the result of multiplying the inflation time and the IAP. We reached a cut-off value of > or = 1800 which is slightly lower than that proposed by Nattachai Srisawat et al. [Citation10]. Our research highlights the need of surgeons as well as ASA, minimizing the prolonged exposure index to mitigate the perioperative AKI incidence. Multiple research have been conducted to explain the impact of elevated (IAP) on the (AKI) progression [Citation11]. Several various mechanisms exist that involve the direct chemical effect of hypercarbia and the mechanical effect as a result of elevated IAP [Citation12,Citation13]. A previous study which was done on animals proposed that IAP of 20 mmHg can lead to renal dysfunction due to vessel compression and subsequent renal hypoperfusion [Citation14]. Such a mechanism could not give an explanation regarding our research’s findings, since all cases exhibited a mean IAP at 15 mmHg. Previous studies involving laparoscopic abdominal surgeries considered pneumoperitoneum with IAP ranging between 12 and 16 mmHg as standard normal pressure laparoscopic surgeries [Citation15].
We utilized UNGAL, an innovative biomarker for AKI diagnosis which did not have standard cut-off level based on previous studies. Additionally, most AKI cases exhibited UNGAL levels less than 70 ng/mL, indicating that most AKI patients may have a non-severe form of renal insult. We have also found UNGAL level doubles every 24 h in AKI patients, while serum creatinine returns to baseline at 48 h [Citation16,Citation17]. However, baseline UNGAL was of no predictive value for AKI which can be attributed to the marker itself being new with no absolute cut-off value, and in addition, the value of baseline UNGAL expresses a patient before our test TVC and before laparoscopic insufflation. Overall, in our study, we found that the two intra-operative parameters TVC and the exposure index can both be of early predictive value of postoperative AKI especially when combined.
Our study has several strengths. First, multiple intra-operative parameters were explored while predicting laparoscopic abdominal surgery associated with AKI. Secondly, urine output was added to serum creatinine level for AKI diagnosis, and unlike previous studies used only serum creatinine levels, we also used a novel biomarker NGAL in urine to both diagnose and confirm the diagnosis of early post-operative AKI which made us able to obtain more AKI cases as opposed to previous research. Third, we excluded cases with chronic kidney diseases and those who might have renal affection by NSAID to isolate the effect of PP on AKI development.
Limitations: A relatively modest sample size as well as a prospective observational single-centered study, making us unable to generalize the findings unless they are validated in a larger study.
7. Conclusions
AKI represents a frequently seen complication that occurs temporarily after laparoscopic abdominal surgery. To avoid peri-operative renal impairment, limiting exposure index should be considered. Our work introduces the TVC test as a new tool for (AKI) prediction in laparoscopic abdominal surgeries. Nevertheless, more RCTs are required to support this hypothesis.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Pisano CW. Laparoscopy. Anesthesiology. 2017;247–253 doi: 10.1007/978-3-319-50141-3_32
- Jiang R, Sun Y, Wang H, et al. Effect of different carbon dioxide (CO2) insufflation for laparoscopic colorectal surgery in elderly patients: a randomized controlled trial. Medicine. 2019;98(41):180–196. doi: 10.1097/MD.0000000000017520
- Srisawat N, Kongwibulwut M, Laoveeravat P, et al. The role of intraoperative parameters on predicting laparoscopic abdominal surgery associated acute kidney injury. BMC Nephrol. 2018;19(1):289–295. doi: 10.1186/s12882-018-1081-4
- Dreischulte T, Morales DR, Bell S, et al. Combined use of nonsteroidal anti-inflammatory drugs with diuretics and/or renin–angiotensin system inhibitors in the community increases the risk of acute kidney injury. Kidney Int. 2015;88(2):396–403. doi: 10.1038/ki.2015.101
- Malo R. Plethysmography Variation Index (PVI) utility in guiding goal-directed fluid therapy during major abdominal surgery. Kidney Int. 2023;77:70–77.
- Messina A, Montagnini C, Cammarota G, et al. Tidal volume challenge to predict fluid responsiveness in the operating room: an observational study. Eur J Anaesthesiol. 2019;36(8):583–591. doi: 10.1097/eja.0000000000000998
- Skoog J, Lindenberger M, Ekman M, et al. Reduced venous compliance: an important determinant for orthostatic intolerance in women with vasovagal syncope. Am J Physiol Regul Integr Comp Physiol. 2016;310(3):253–261. doi: 10.1152/ajpregu.00362.2015
- Sharma KC, Brandstetter RD, Brensilver JM, et al. Cardiopulmonary physiology and pathophysiology as a consequence of laparoscopic surgery. Chest. 1996;110(3):810–815. doi: 10.1378/chest.110.3.810
- Myatra SN, Prabu NR, Divatia JV, et al. The changes in pulse pressure variation or stroke volume variation after a “tidal volume challenge” reliably predict fluid responsiveness during low tidal volume ventilation. Crit Care Med. 2017;45(3):415–421. doi: 10.1097/ccm.0000000000002183
- Srisawat N, Kongwibulwut M, Laoveeravat P, et al. The role of intraoperative parameters on predicting laparoscopic abdominal surgery associated acute kidney injury. BMC Nephrol. 2018;19(1):200–215. doi: 10.1186/s12882-018-1081-4
- Kirsch AJ, Hensle TW, Chang DT, et al. Renal effects of CO2 insufflation: oliguria and acute renal dysfunction in a rat pneumoperitoneum model. Urol. 1994;43(4):453–459. doi: 10.1016/0090-4295(94)90230-5
- Srivastava A, Niranjan A. Secrets of safe laparoscopic surgery: Anaesthetic and surgical considerations. J Minim Access Surg. 2010;6(4):91–94. doi: 10.4103/0972-9941.72593
- Seigneux de, S, Klopfenstein CE, Iselin C, et al. The risk of acute kidney injury following laparoscopic surgery in a chronic kidney disease patient. NDT Plus. 2011;4(5):339–341. doi: 10.1093/ndtplus/sfr071
- Shuto K, Kitano S, Yoshida T, et al. Hemodynamic and arterial blood gas changes during carbon dioxide and helium pneumoperitoneum in pigs. Surg Endosc. 1995;9(11):1173–1178. doi: 10.1007/bf00210922
- Sandhu T, Yamada S, Ariyakachon V, et al. Low-pressure pneumoperitoneum versus standard pneumoperitoneum in laparoscopic cholecystectomy, a prospective randomized clinical trial. Surg Endosc. 2009;23(5):1044–1047. doi: 10.1007/s00464-008-0119-2
- Haase M, Bellomo R, Devarajan P, et al. Accuracy of neutrophil gelatinase-associated lipocalin (NGAL) in diagnosis and prognosis in acute kidney injury: a systematic review and meta-analysis. Am J Kidney Dis. 2009;54(6):1012–1024. doi: 10.1053/j.ajkd.2009.07.020
- Singer E, Elger A, Elitok S, et al. Urinary neutrophil gelatinase-associated lipocalin distinguishes pre-renal from intrinsic renal failure and predicts outcomes. Kidney Int. 2011;80(4):405–414. doi: 10.1038/ki.2011.41