ABSTRACT
Background
Cataract surgery is one of the infrequent ocular surgeries. The adequate ocular position with central alignment is the main prerequisite for good surgical technique. Propofol and sevoflurane are the common anesthetics drugs used during pediatric anesthesia. BIS monitor is one of the common intraoperative awareness monitors used.
Aim
To assess the efficacy of the bispectral index monitor in quantifying the depth of anesthesia and its correlation with ocular alignment during juvenile cataract surgery. Specifically, we will compare the use of sevoflurane anaesthesia with total intravenous anesthesia using a midazolam bolus and propofol infusion.
Methods
This study included 100 children scheduled for cataract surgery. The children were divided into two groups: group (S) included 50 children who were anesthetized using sevoflurane maintenance only and group (P) included 50 children who were anesthetized using continuous intravenous anesthesia (midazolam bolus plus propofol infusion) as maintenance after induction with sevoflurane anesthesia 8%. The bispectral index was recorded immediately after induction and after intubation and every 5 min later on until end of surgery.
Results
The eye position showed statistically significant central position among the propofol group with p value 0.02. An eye position-BIS value association was found statistically significant negative correlation in sevoflurane group while no statistically significant link was found in the propofol group.
Conclusion
Use of BIS monitor for making correlation between depth of anesthesia for prediction of ocular alignment was significant in sevoflurane group, but not in propofol group in pediatric patients and even with adequate depth of general anesthesia.
1. Introduction
Pediatric cataract remains an infrequent but a significant disease with vision threatening consequences. It is the main treatable cause of visual disability. Improper treatment of pediatric cataract may lead to lifetime blindness [Citation1]. General anesthesia is often used in children because it is nearly impossible to apply local anesthesia especially in the ages younger than 10 years. However, its main disadvantage is slightly elevated and divergent positions of the eyes during surgery. These eccentric eye position makes the surgical access more difficult which increase the incidence of intraoperative complications [Citation2].
The bispectral index (BIS) is an electroencephalographic measurement that quantifies the hypnotic impact of various anesthetic medications in pediatric patients [Citation3]. BIS values were considered as an accepted measure of the depth of anaesthesia in many studies [Citation4].
The most commonly used anesthetic agents in pediatric patients are sevoflurane and propofol. Because of many merits like rapid induction, smooth maintenance and rapid recovery, however, the main drawback of sevoflurane is agitation during recovery [Citation5]. Many studies have evaluated the correlation between the end-tidal sevoflurane and BIS values [Citation6–8], but this issue was not investigated using propofol [Citation9].
This study asses the effect of propofol-midazolam versus sevoflurane on the depth of anesthesia using BIS monitoring and their correlation with eye position in pediatric cataract surgery.
We hypothesized that propofol-midazolam might be comparable to sevoflurane anesthesia in maintaining central eye position throughout the surgery.
2. Patients & methods
2.1. Study design
This prospective, randomized, single-center trial with two equal parallel arms was conducted at Mansoura Ophthalmology Center from June 2021 to November 2023. The planned protocol was approved on 13 April 2021 by Mansoura University Institutional Research Board ID (MD21.03.449); after that, it was registered at clinical trials.gov on (date 2/3/2022) with registry ID: NTC05262205.
This study included 100 children of both genders, who had a first class ASA physical status and were scheduled for unilateral cataract surgery. The age range of the participants was between 3 and 10 years. Participation in the trial was restricted to exclude children with neurological illnesses, eye movement impairments, certain syndromes (such as Cohen, Dubowetz, and Degos disease), those using antipsychotic medication, and those with a history of drug allergies.
2.2. Anesthetic management
Pre-operative evaluation of the enrolled children included history, physical examination, and laboratory investigations. Before the child’s legal guardians signed an informed consent form during the pre-operative appointment, they were given a thorough description of the study protocol. There was no premedication with sedatives.
In the pre-anesthetic unit, pupils were dilated with the instillation five drops of phenylephrine eye drops 2.5% in the surgical eye, then waited for 10 min. Upon transferring the child to the operating room with parent attendance, basic monitors were attached to them (electrocardiography, pulse oximeter, and noninvasive blood pressure using appropriate cuff size). Basic values were recorded. The BIS monitor and its pediatric sensor were used to monitor the depth of anesthesia. At first, the skin was cleansed with 70% ethanol, and then the electrode of BIS was placed front-laterally on the patient’s forehead according to the manufacturer’s recommendations. The signal quality index was 95%.
Induction of anesthesia was standardized for all patients by mask inhalation of sevoflurane with oxygen% 100. After intravenous cannulation, a single dose of atracurium 0.25 mg/kg to facilitate endotracheal insertion and paracetamol 15 mg/kg were given slowly. Volume-controlled mode was the set mode for both groups with tidal volume 6–8 ml/kg and respiratory rate 18–20. Capnography kept between 35 and 40 mm Hg. Patients were connected to a standard pediatric circle system for children and an anesthesia machine. Fresh gas flow was maintained at 2 l/min using an oxygen/air mixture (4:6). Then, the maintenance of anesthesia was followed by the group’s allocation. With the use of a computer-generated table of randomization and the Statistical Package for the Social Sciences (SPSS) version 22 for Windows (IBM SPSS, IL, USA), the enrolled youngsters were divided into two equal groups at random (1:1). The same team of surgeons operated on each patient. Before anesthesia was administered, the group assignment was supplied and opened from an opaque, sealed envelope.
Group Sevoflurane S (n = 50); the maintenance of anesthesia was done by end – tidal sevoflurane 2%.
Group Propofol P (n = 50): the maintenance of anesthesia was done by midazolam at a bolus dose 0.05 mg/kg propofol at bolus dose 1 mg/kg and this is according to MacFarlan regimen [Citation10] as follows:
0–10 min: 15 mg/kg/h
10–15 min: 15 mg/kg/h
15–20 mis: 13 mg/kg/h
20–30 min: 13 mg/kg/h
30–40 min: 11 mg/kg/h
40–50 min: 11 mg/kg/h
50–60 min: 11 mg/kg/h
2.3. Data collection and post-operative management
Pupillary dilatation was assessed using the pupil ruler. If the pupil size is equal or more than 5 mm, it was considered adequately dilated. While if less than 5 mm, it was considered not dilated and recorded at 10 min and 20 min after speculum insertion.
An examiner who was blind to the BIS data videotaped and assessed eye position immediately during induction, after intubation, and at 5-min intervals. At the same recording times, the position of the surgical eye was recorded whether central or not.
Heart rate and mean arterial blood pressure were recorded at baseline, throughout induction, during intubation, and every 5 min until the end of the procedure.
Following extubation, the child was sent to the pediatric post-anesthetic care unit (PACU), where hemodynamics and post-operative emerging agitation were monitored. The latter was measured using the five-step WATCHA Scale [Citation11] and recorded after extubation and 30 min later. Any vomiting or nausea episode was noted. When it occurred, ondansetron was administered intravenously (IV) at a dose of 0.1 ml/kg slowly over 2 to 5 min for children under 40 kg and 4 mg slowly over 2 to 5 min for children over 40 kg.
2.4. Sample size calculation and statistical analysis
Our primary discovery for calculating the sample size was the correlation between the globe’s position throughout the injection of propofol and sevoflurane, and the depth of anesthesia as evaluated by BIS. The data were obtained from a pilot research that consisted of 10 instances in each group. The sample size for the study was determined using the G power software version 3.1.9.7, with a two-tailed test, an alpha error of 0.05, and a power of 80.0%. The minimum sample size required for each group was determined to be 50 instances, based on an effect size of 0.569 observed in the BIS score (45.3 ± 9.80 for the S group and 50.2 ± 7.2 for the P group).
SPSS (version 22) for windows was used to code, process, and analyze the data that had been gathered. The test of Shapiro–Wilk was used to check if the distribution of numerical data was normal. The mean plus standard deviation of continuous data with a normal distribution was used for comparison with an unpaired student’s t-test. Data that were not normally distributed were compared using the Mann–Whitney U-test and shown as the median (range). The Chi-square test was used to compare the numerical (%) form of the categorical data. The spearman correlation coefficient was correlated between continuous data for non-parametric distribution. p values of less than 0.05 were used to classify data as significant.
3. Results
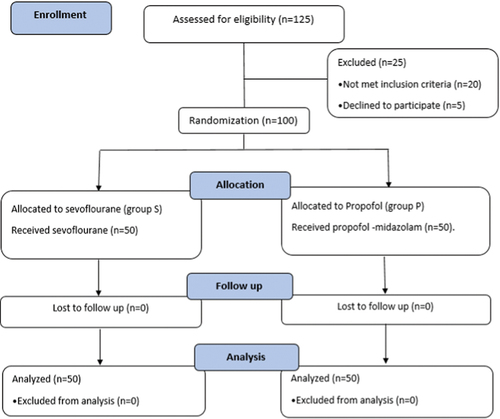
One hundred and twenty-five children who had cataract surgery scheduled between 1 June 2021, and the last of November, 2023, had their eligibility evaluated. Five patients declined to participate, and 20 patients did not match the inclusion criteria ().
indicates that the demographic data were comparable in the two studied groups.
Table 1. Patient characteristics, duration of surgery and anesthesia.
Mean blood pressure and HR were comparable in the two studied groups at all study times. Additionally, there was no statistically significant difference between the two groups regarding intraoperative BIS index monitoring (). which displayed the WATCHA score after surgery demonstrated statistical significance higher scores among the propofol group at both time points (after extubation and 30 min later), with a p value of 0.01.
Figure 2. (a) showing BIS using clustered column chart. (b) WATCHA score was represented with numbers and %.
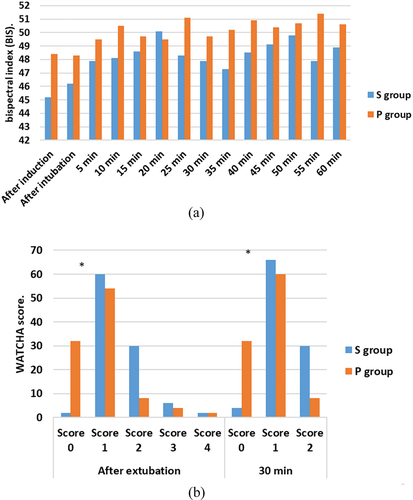
In the propofol group, as compared to the sevoflurane group, the eye position exhibited a statistically significant central position at 10 min (96% vs 82%), 20 min (100% vs 90%), and 30 min (100% vs 90%) with a p-value of 0.02. There was no significant difference in pupil dilation between the two groups, as indicated by the lack of statistical significance ().
Table 2. Eye position throughout the surgery and pupillary dilatation.
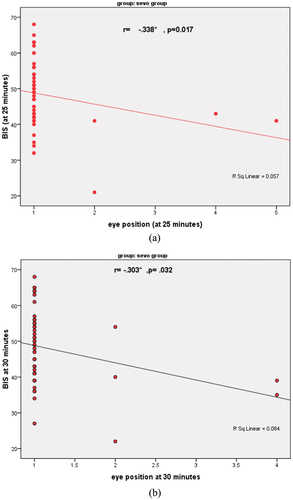
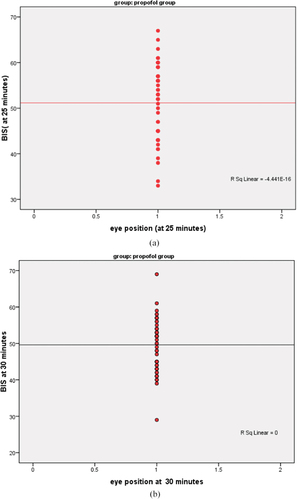
An eye position BIS value association was found statistically significant negative correlation in sevoflurane group (). However at the same follow-up, no statistically significant link was found between eye position and BIS, in the propofol group ().
4. Discussion
In this randomized study, there was a significant negative correlation between globe position and increasing depth of anesthesia in sevoflurane group, but this relationship was not demonstrated in the propofol group. Furthermore, the Propofol group’s Watcha score demonstrated a statistically significant improvement.
It is crucial to use a BIS monitor since there is a negative link between eye positions and BIS when sevoflurane is being administered. Because it might help keep the eye’s center place. There was a strong correlation between the position of the globe and the depth of anesthesia because the BIS values linked to the central globe were within the range of 40–65, which is the range for an adequate level of anesthesia. Increasing or decreasing the depth of anesthesia would be associated with a reciprocal change in the globe.
Kook et al. corroborated our discovery by demonstrating a substantial inverse relationship between pediatric BIS readings and the level of anesthesia under sevoflurane anesthesia. They proposed a correlation between the lower depth of anesthesia and the elevated eye position [Citation12].
Our findings were consistent with a study conducted by Ganish and his colleagues on BIS monitoring in pediatric anesthesia. They concluded that although bispectral index values may vary with equipotent doses of different agents, its scores were found to strongly correlate with sedation scores during conscious or deep sedation in pediatric patients, as well as with end-tidal concentrations of inhalation agents in children. The findings of this study provided evidence for the effectiveness of BIS in children who were administered inhalational anesthetics during sedation. BIS helped to decrease the dosage of anesthetic medications used [Citation13]. The findings confirmed the effectiveness of BIS in children undergoing sedation with inhalational anesthetics. This led to a reduction in the dosage of anesthetic medications. However, the study did not examine the correlation between BIS and eye position.
Rodriguez and his colleagues found that subjects’ BIS values overlapped between multiple levels of anesthesia, leading to significant inter-individual variability. This contradicts our findings regarding the ability of BIS to predict depth of inhalational anesthesia in children during induction and arousal [Citation14]. In 2020, Sullivan and associates also presented data that were in opposition to ours, claiming that BIS had little use in tracking anesthesia patients between the ages of 2 and 12 for reducing volatile anesthetic exposure [Citation15].
These results showed that using the BIS monitor to adjust the globe position during intravenous propofol anesthesia is ineffective. Rather, this suggests that propofol has a distinct effect on the globe position, which may be related to its muscle relaxant effect on the eye muscle rather than the depth of anesthesia itself. In juvenile cataract surgery, propofol may be a good substitute for sevoflurane in order to maintain the globe’s central position without requiring the use of a BIS monitor to track the depth of anesthetic.
Our results related to TIVA group (propofol and midazolam bolus then maintenance propofol infusion) showed that usage BIS for maintaining central eye position did not correlate with depth of anesthesia in children during cataract surgery although having more central eye position during surgery in relation to sevo group. In 2008, Avidan and his colleagues had published results that supported our findings as he reported the unusefulness of BIS as a measure of awareness of anesthesia in 2000 patients undergoing surgery. Its use did not lower the administration of volatile anesthetic concentration where anesthesia awareness occurred even when BIS was used. Minimum alveolar concentration was monitored [Citation16]. Our findings for the TIVA group (propofol and midazolam bolus followed by maintenance propofol infusion) indicated that, although the TIVA group had more central eye position during surgery, there was no relationship between the depth of anesthesia in children receiving BIS for central eye position maintenance during cataract surgery. The unreliability of BIS as a measure of anesthesia awareness in 2000 surgical patients was reported by Avidan and colleagues in 2008; furthermore, its use did not reduce the administration of volatile anesthetic concentration, where anesthesia awareness occurred even when BIS was used and minimum alveolar concentration was monitored [Citation16]. These results corroborated our findings.
In another study done on patients who had hystroscopic procedures under sedation with propofol, Li and his colleagues compared using BIS versus BISpro by TCI, and they proved for both devices to be reliable in sedation under propofol. This may be related to the age of patients in the study as they were adult females, but our patients were children aged 3 to 10 years [Citation17].
In a previous study on BIS with propofol anesthesia in children aged 1 to 12 years, BIS showed variation with different age groups but was similar in same nine time points determined to evaluate BIS after propofol injection. This was related to the fact that the pediatric nervous system differs from that of adults in that it is characterized by rapid development; hereafter, typical pediatric EEGs are more variable than adult EEGs [Citation18].
For maintenance of pupillary dilatation with sevoflurane and propofol, we found no statistically significant difference between both anesthetics allover surgery with TIVA group having 100% pupillary dilatation in 10 min and 20 min measurement versus sevo group having 98% in 1st 10 min and 96% in next 20 min.
Shirozu and his colleagues studied the effect of different anesthetics on pupillary function during general anesthesia using an infrared automated pupillometer. They divided patients into four groups, comparing them with using propofol, remifentanyl, sevoflurane, recuronium, and desflurane. They found that propofol, sevoflurane, desflurane, and fentanyl decreased the pupillary size but not the latency of pupillary reflex. The neurologic pupillary index was slower in sevogroup than propofol group that may be explained by deeper plain of anesthesia in volatile anesthetic group than intravenous group or that there are anesthetic-dependent differences in their effects on brain activity. He concluded also that the neurologic pupillary index did not correlate with BIS [Citation19].
Another evidence supporting the suggestion that depth of anesthesia may be related to pupillary diameter changes was the study done by Sabourdin and her colleagues when they studied the effect of increasing doses of intravenous infusion of propofol using TCI on the pupillary diameter guided by BIS allover surgery. They found that propofol has a dose-dependent effect on pupillary diameter and BIS has a positive correlation to pupillary diameter within propofol concentration used (from 1 to 3 micrograms plasma concentration) [Citation20].
Another important outcome was emergence agitation. In a prospective cohort study done by Haile and colleagues on 90 patients anesthetized with propofol 1 mg/kg before the end of ENT surgery, the incidence of emergence after recovery was lower in children exposed to propofol than non-exposed [Citation21]. Ramlan and colleagues used lower dose of propofol (0.5 mg/kg) in children undergoing general anesthesia under sevoflurane before end of surgery. They reached the same results of that propofol decreases emergence agitation of general anesthesia [Citation22] and both studies agreed with our findings.
5. Conclusion
Use of BIS monitor for correlation between depths of anesthesia and prediction of ocular alignment was reliable for children anesthetized with sevoflurane but weak in pediatric patients anesthetized with propofol infusion. Even with adequate depth of general anesthesia, eye could move up or down as eye gaze has its already saccadic movement that has complex neural pathway and perhaps there are other factors interfering with anesthesia making eye move.
5.1. Limitations of the study
Firstly, we did not divide the children to different age groups as age range was from 3 to 10 years. And hemodynamics may differ among different ages. Secondly, we did not have statistics for rescue medication during eccentric eye position as propofol for the p group or concentration of sevoflurane in the S group.
Clinical trial registration number
The study protocol was registered at clinical trials.gov on (date 2/3/2022) with unique ID NTC05262205.
IRB number
The Institutional Research Board, Faculty of Medicine, Mansoura University approved the study protocol on 13 April 2021 (IRB code: MD21.03.449).
First page reem.docx
Download MS Word (13.2 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/11101849.2024.2344747
References
- Gilbert C. Worldwide causes of blindness in children. In: Wilson ME, Trivedi RH Saunders RA, editors. Pediatric ophthalmology: current thought and a practical guide. Berlin Heidelberg: Springer; 2009.p. 47–60.
- Donahue SP. Binocular vision and ocular motility, 6th edition. J Neuroophthalmol. 2003;23(1):99. doi: 10.1097/00041327-200303000-00051
- Davidson A, Huang G, Rebmann C, et al. Performance of entropy and Bispectral Index as measures of anaesthesia effect in children of different ages. British Journal of Anaesthesia. 2005;95(5):674–679. doi: 10.1093/bja/aei247
- Davidson AJ, McCann M, Devavaram P, et al. The differences in the bispectral index between infants and children during emergence from anesthesia after circumcision surgery. Anesthesia & Analgesia. 2001;93(2):326–330. doi: 10.1213/00000539-200108000-00017
- Pieters BJ, Penn E, Nicklaus P, et al. Emergence delirium and postoperative pain in children undergoing adenotonsillectomy: a comparison of propofol vs sevoflurane anesthesia. Pediatric Anaesth. 2010;20(10):944–950. doi: 10.1111/j.1460-9592.2010.03394.x
- McCann ME, Bacsik J, Davidson A, et al. The correlation of bispectral index with end-tidal sevoflurane concentration and haemodynamic parameters in preschoolers. Pediatr Anesthesia. 2002;12(6):519–525. doi:10.1046/j.1460-9592.2002.00886.x
- Denman WT, Swanson EL, Rosow D, et al. Pediatric evaluation of the bispectral index (BIS) monitor and correlation of BIS with end-tidal sevoflurane concentration in infants and children. Anesthesia & Analgesia. 2000;90(4):872–877. doi: 10.1213/00000539-200004000-00018
- Bannister CF, Brosius KK, Sigl JC, et al. The effect of bispectral index monitoring on anesthetic use and recovery in children anesthetized with sevoflurane in nitrous oxide. Anesthesia & Analgesia. 2001;92(4):877–881. doi: 10.1097/00000539-200104000-00015
- Jeleazcov C, Ihmsen H, Schmidt J, et al. Pharmacodynamic modelling of the bispectral index response to propofol-based anaesthesia during general surgery in children. Br J Anaesth. 2008;100(4):509–516. doi: 10.1093/bja/aem408
- McFarlan CS, Anderson BJ, Short TGJPA. The use of propofol infusions in paediatric anaesthesia: a practical guide. Pediatric Anaesth. 1999;9(3):209–216. doi: 10.1046/j.1460-9592.1999.00364.x
- Bajwa SA, Costi D, Cyna AMJPA. A comparison of emergence delirium scales following general anesthesia in children. Pediatric Anesthesia. 2010;20(8):704–711. doi: 10.1111/j.1460-9592.2010.03328.x
- Kook KH, Chung SA, Park S, et al. Use of the bispectral index to predict eye position of children during general anesthesia. Korean J Ophthalmol. 2018;32(3):234–240. doi: 10.3341/kjo.2017.0104
- Ganesh A, Watcha, MFJCOIA. Bispectral index monitoring in pediatric anesthesia. Curr Opin Anaesth. 2004;17(3):229–234. doi: 10.1097/00001503-200406000-00006
- Rodriguez RA, Hall LE, Duggan S, et al. The bispectral index does not correlate with clinical signs of inhalational anesthesia during sevoflurane induction and arousal in children. Can J Anaesth. 2004;51(5):472. doi: 10.1007/BF03018310
- Sullivan CA, Egbuta C, Park RS, et al. The use of bispectral index monitoring does not change intraoperative exposure to volatile anesthetics in children. JCM. 2020;9(8):2437. doi: 10.3390/jcm9082437
- Avidan MS, Zhang L, Burnside BA, et al. Anesthesia awareness and the bispectral index. N Engl J Med. 2008;358(11):1097–1108. doi: 10.1056/NEJMoa0707361
- Lin YJ, Wang YC, Huang HH, et al. Target-controlled propofol infusion with or without bispectral index monitoring of sedation during advanced gastrointestinal endoscopy. J Gastro Hepatol. 2020;35(7):1189–1195. doi: 10.1111/jgh.14943
- Wang F, Zhang J, Yu J, et al. Variation of bispectral index in children aged 1–12 years under propofol anesthesia: an observational study. BMC Anesthesiol. 2019;19(1):145. doi: 10.1186/s12871-019-0815-6
- Shirozu K, Setoguchi H, Tokuda K, et al. The effects of anesthetic agents on pupillary function during general anesthesia using the automated infrared quantitative pupillometer. J Clin Monit Comput. 2017;31(2):291–296. doi: 10.1007/s10877-016-9839-3
- Sabourdin N, Diarra C, Wolk R, et al. Pupillary pain index changes after a standardized bolus of alfentanil under sevoflurane anesthesia: first evaluation of a New Pupillometric index to assess the level of analgesia during general anesthesia. Anesth Analg. 2019;128(3):467–474. doi: 10.1213/ANE.0000000000003681
- Haile S, Girma T, Akalu L. Effectiveness of propofol on incidence and severity of emergence agitation on pediatric patients undergo ENT and ophthalmic surgery: Prospective cohort study design. Ann Med Surg. 2021;69:102765. doi: 10.1016/j.amsu.2021.102765
- Ramlan AAW, Pardede DKB, Marsaban A, et al. Efficacy of 0.5 mg/kg of propofol at the end of anesthesia to reduce the incidence of emergence agitation in children undergoing general anesthesia with sevoflurane. J Anaesthesiol Clin Pharmacol. 2020;36(2):177–181. doi: 10.4103/joacp.JOACP_257_19