Abstract
Introduction
Non-suicidal self-injury disorder (NSSID) is a new diagnosis proposed in DSM-5 with a need of further study, especially in adolescent clinical populations where non-suicidal self-injury (NSSI) is particularly prevalent. We aimed to study characteristics of NSSID and estimate an optimal cutoff frequency level of NSSI behavior.
Methods
Data were collected from 103 outpatient adolescents (ages 12–18) with recurrent self-harm behavior.
Results
Adolescents with NSSID reported significantly more frequent NSSI behavior and suicide attempts than adolescents without NSSID. Frequency of NSSI, global functioning, depressive symptoms, number of self-harm methods and anxiety symptoms best discriminated between adolescents with and without NSSID. An optimal cutoff level for a diagnosis of NSSID was found to be ≥15 days with NSSI during the last year, which led to a reduction in the rate of adolescents diagnosed with NSSID from 54% to 46%.
Conclusion
This study shows that NSSID is a highly impairing disorder characterized by high risk of multiple NSSI and suicide attempts, decreased functioning and other associated psychiatric disorders. Clinical awareness of these risks are important to ensure early detection and treatment. Future prospective longitudinal studies are needed to further validate the characteristics of the NSSID diagnosis and its clinical utility.
INTRODUCTION
Non-suicidal self-injury (NSSI) has been defined as deliberate, self-inflicted destruction of body tissue without suicidal intent, and for purposes not socially sanctioned (Klonsky, Citation2007). Common self-injurious methods include cutting, burning and self-battery (Cipriano, Cella, & Cotrufo, Citation2017; Klonsky & Muehlenkamp, Citation2007), and most individuals who self-harm employ more than one method (Cipriano et al., Citation2017). Recurrent NSSI behavior is associated with high risk of future suicide attempts, poor mental health and low levels of global functioning (Bjureberg et al., Citation2019; Castellví et al., Citation2017; Glenn & Klonsky, Citation2013; Hawton, Saunders, & O'Connor, Citation2012). This led the American Psychiatric Association to propose Non-suicidal self-injury disorder (NSSID) as a disorder for further study in the DSM-5 (American Psychiatric Association, Citation2013). A diagnostic category such as this would potentially enable clinicians to more effectively identify high-risk individuals with severe NSSI behavior and target them for treatment. Furthermore, an NSSID diagnosis could stimulate research aiming to disentangle non-suicidal self-injury from suicide attempts, and, hopefully, lead to improved communication and conceptual clarity in clinical practice (Zetterqvist, Perini, Mayo, & Gustafsson, Citation2020). Several aspects of the NSSID proposal are, however, in need of clarification; such as the clinical characteristics and correlates of NSSID, and the suggested diagnostic criteria, (Muehlenkamp, Ertelt, Miller, & Claes, Citation2011; Zetterqvist et al., Citation2020).
In 2012, an early version of the official NSSID DSM-5 criteria were proposed by the DSM Task Force and work group, to urge new research and commentary from the field (In-Albon, Ruf, & Schmid, Citation2013). The official proposed DSM-5 diagnostic criteria of the NSSID were released in 2013 and contain the same criteria as the early version but with more detailed descriptions. The proposed diagnosis includes a presentation of deliberate self-inflicted damage to body tissue on five or more days within the past year, without the intent to suicide (Criterion A). The individual has expectations that the behavior will lead to relief from negative thoughts and emotions, induce a positive feeling state, or resolve interpersonal difficulty (Criterion B). The intentional behavior is associated with interpersonal difficulties, negative thoughts and emotions, and/or recurrent preoccupation of self-injury thoughts prior to the behavior (Criterion C). The behavior is not socially sanctioned (Criterion D), and cause clinically significant distress and interference in important areas of functioning (Criterion E). Finally, the behavior is not better explained by other mental disorder or medical condition (Criterion F) (American Psychiatric Association, Citation2013, p. 803).
Based on the current NSSID construct, the prevalence of the disorder varies between 5.6% and 7.6% in non-clinical adolescent samples, and rises to 74–78% in clinical samples of adolescents (Glenn & Klonsky, Citation2013; Washburn, Potthoff, Juzwin, & Styer, Citation2015), but is still only between 0.2% and 0.8% in young adults in the general population (Kiekens et al., Citation2018). Studies have shown that NSSID is frequently co-occurring with other mental disorders, such as depressive and anxiety disorders as well as borderline personality disorder and suicidal behavior (In-Albon et al., Citation2013; Selby, Bender, Gordon, Nock, & Joiner, Citation2012; Zetterqvist, Citation2015). However, it is less clear whether adolescents with NSSID have a higher number of suicide attempts compared to self-harming adolescents without NSSID, which would be important for clinicians to know when assessing the risk of suicidality. Furthermore, studies show that NSSID is associated with more severe psychopathology, lower psychosocial global functioning and increased self-injury method versatility (Castellví et al., Citation2017; Gratz, Dixon-Gordon, Chapman, & Tull, Citation2015; In-Albon et al., Citation2013; Kiekens et al., Citation2018; Selby et al., Citation2012; Washburn et al., Citation2015). Thus far, most studies of psychopathology and other features associated with NSSID have used data from adult samples and from the general population (Zetterqvist, Citation2015). This limits their capacity to inform clinicians working with self-harming adolescents where the need for this knowledge is greatest and where the prevalence of NSSID is highest (Muehlenkamp, Claes, Havertape, & Plener, Citation2012; Zetterqvist et al., Citation2020). Thus, there is a need for more studies in clinical adolescent populations to examine which clinical factors, such as level of global functioning, level of psychopathology and self-harm characteristics, have the strongest association with NSSID. More knowledge about these factors could enable clinicians to more effectively identify adolescents at high risk for severe NSSI and suicide attempts and to more precisely assess their treatment needs.
Several studies have examined the validity and utility of the proposed DSM-5 diagnostic criteria currently delineating NSSID (Brausch, Muehlenkamp, & Washburn, Citation2016; Zetterqvist et al., Citation2020), where the number of NSSI episodes needed to receive the diagnosis (Criterion A) seems so far, to have attracted the greatest interest (Muehlenkamp & Brausch, Citation2016; Selby, Kranzler, Fehling, & Panza, Citation2015; Wilkinson, Kelvin, Roberts, Dubicka, & Goodyer, Citation2011). Since this relatively low NSSI frequency cutoff level may increase the likelihood of over-diagnosing NSSID, several researchers have suggested to increase it (Ammerman, Jacobucci, & McCloskey, Citation2019; Buelens et al., Citation2020; Muehlenkamp & Brausch, Citation2016). Only a few studies have examined Criterion A in clinical adolescent populations. In a sample of female patients with conduct disorder and NSSID Szewczuk-Bogusławska et al. (Citation2018) found significant group differences in psychopathology and level of functioning when increasing the cutoff level of self-harm episodes to at least 8 “NSSI days last year.” Muehlenkamp, Brausch, and Washburn (Citation2017), examined the cutoff level of Criterion A in a sample of adolescent inpatients and found that a cutoff level of at least 25 days of NSSI last year was a good discriminator between degrees of psychopathology and functional impairment. These studies suggest that increasing the cutoff level of NSSI episodes would improve the discriminant validity of the diagnosis. However, these studies are not readily generalizable to other clinical settings, since they were based off of highly specialized adolescent samples. Based on a less highly selected sample of adolescents seen in child and adolescent mental health services, we, therefore, wanted to evaluate what would be a more optimal cutoff level of NSSI episodes to identify high-risk individuals with serious NSSI behavior.
Our aims were firstly to examine clinical characteristics in adolescents who meet the criteria for a DSM-5 diagnosis of Non-suicidal Self-Injury Disorder (NSSID) compared to adolescents who do not meet the criteria, in a clinical sample of adolescents with recurrent self-harming behavior. Secondly, we wanted to study which clinical factors best discriminate between adolescents with and without NSSID. Thirdly, we aimed to estimate what cutoff level (Criterion A) for the NSSID diagnosis would be associated with an optimal balance between sensitivity and specificity measured against significantly lowered global functioning. Based on this new cutoff threshold, we wanted to study the differences in level of psychopathology and self-harm characteristics in study subjects with and without NSSID, and examine whether this alternative cutoff level would lead to different discriminating factors.
METHOD
Participants and Procedures
Participants were 103 adolescents (ages 12–18) recruited from a child and adolescent psychiatric outpatient clinic at Oslo University Hospital, Norway. Adolescents were screened for self-harm behavior defined as “intentional poisoning or self-injury, regardless of intention to die” (Hawton, Citation2007), whereas Non-suicidal self-injury (NSSI) was defined as “the deliberate, self-inflicted destruction of body tissue without suicidal intent, and for purposes not socially sanctioned” (Klonsky, Citation2007). Finally, a suicide attempt was defined as “a potentially self-injurious act committed with at least some wish to die, as a result of the act” (Posner, Melvin, Stanley, Oquendo, & Gould, Citation2007). Inclusion criteria were recurrent self-harm behavior (two or more episodes) with the last episode having been within the past 6 months. Exclusion criteria were intellectual disability, or insufficient Norwegian language skills to understand or answer the interviews or questionnaires, as assessed through the recordings of anamnestic information (learning history, school information and school grades). Both adolescents and their parents signed a consent declaration to participate in the study, and the declaration was approved by the Regional Committee for Medical Research Ethics, South-East Norway. Interviewers have experienced clinicians and had received training and supervision in the use of the study instruments.
Measures
NSSID diagnosis was made through the use of the Clinician-Administered Non-suicidal Self-Injury Index (CANDI) (Gratz et al., Citation2015); a semi-structured interview originally developed for adults with good interrater reliability and adequate internal consistency (Gratz et al., Citation2015). The interview has also been used to assess NSSID in adolescent samples (Zetterqvist et al., Citation2020).
Borderline personality disorder was assessed with Childhood Interview for Borderline Personality Disorder (CI-BPD), Zanarini et al. (Citation2003); a semi-structured interview developed specifically for use with children and adolescents, with good psychometric properties (Sharp, Ha, Michonski, Venta, & Carbone, Citation2012).
Other DSM-5 diagnoses were assessed with Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version, 2013 (K-SADS-PL) (Kaufman et al., Citation1997).
The frequency of non-suicidal self-injury episodes (NSSI), suicide attempts and self-harm methods, age of self-harm onset and duration of self-harm behavior, was collected with the Suicide Attempt Self-Injury Interview (SASII); a comprehensive instrument with good psychometric properties (Borschmann, Hogg, Phillips, & Moran, Citation2012; Linehan, Comtois, Brown, Heard, & Wagner, Citation2006).
Global psychosocial functioning was assessed by the Children’s Global Assessment Scale (CGAS) (Shaffer et al., Citation1983), reflecting overall severity of disturbance (range 1–100) based on the most impaired level of functioning during the preceding month, where lower scores indicate lower functioning (Lundh et al., Citation2016; Shaffer et al., Citation1983).
Interviewer-rated level of depression was measured by the 10-item MADRS (Montgomery & Asberg, Citation1979).
Level of Borderline symptoms was assessed through the Borderline Symptom List (BSL-23), Bohus et al. (Citation2007), reflecting difficulties and problems commonly experienced by people with BPD.
Level of emotional dysregulation was measured with the self-report Difficulties in Emotion Regulation Scale (DERS), (Gratz & Roemer, Citation2004)—a 36-item measure good psychometric properties assessing multiple aspects of emotion dysregulation.
Level of Suicidal ideation was measured by the 15-item self-report Suicidal Ideation Questionnaire (SIQ-Jr), (Reynolds & Mazza, Citation1999), designed for use with adolescents.
Level of impulsivity was measured with the Barratt Impulsiveness Scale (BIS-15), (Meule, Michalek, Friederich, & Brockmeyer, Citation2020), an 8-item self-report instrument with good psychometric properties.
Finally, level of anxiety symptoms was evaluated through the anxiety subscale (SCL-6) (Heyerdahl, Kvernmo, & Wichstrøm, Citation2004) of the Hopkins Symptom Checklist (Derogatis, Lipman, Rickels, Uhlenhuth, & Covi, Citation1974).
All interviews were audiotaped, and subsets of (1) participants with NSSID (n = 14) and (2) participants with BPD (n = 13) were checked for interrater reliability (IRR) by an independent child and adolescent psychiatrist and a clinical psychologist expert in the relevant assessment instruments. IRR, measured by Kappa, was found to be 0.81 for NSSID, and 0.81 for BPD, which is considered to represent “substantial” agreement in the good range (Landis & Koch, Citation1977).
Data analysis
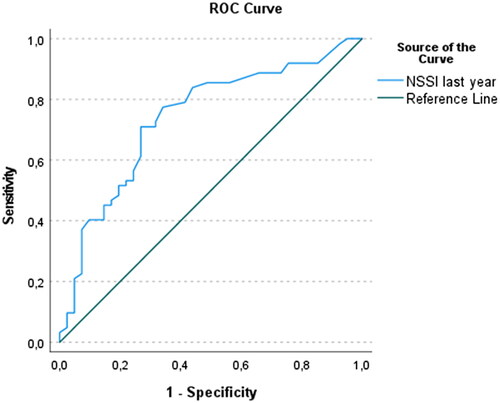
Means and standard deviations are given for normally distributed variables, while median and inter-quartile ranges are given for variables not meeting a normal distribution. Differences between the groups were tested using chi-square for categorical variables and independent-sample t-tests for continuous variables. The significant results from the sample’s t-test, was followed up using discriminant functional analysis, to explore which of these continuous variables could most strongly discriminate between participants with and without NSSID (Tabachnick & Fidell, Citation2018). Based on the results of the discriminant function analysis, an alternative cutoff threshold for NSSID Criterion A was explored. A Receiver Operating Characteristic (ROC) analysis was performed to examine the sensitivity and specificity of the different numbers of days with NSSI last year against level of global function (CGAS), (, Table in supplementary materials), (Kirkwood & Sterne, Citation2003). Since the current study was sampled on recurrent self-harm behavior in a psychiatric outpatient setting, the CGAS cutoff score was set at ≤56, based on the results of a recent Norwegian study with a similar clinical sample of adolescents with recurrent self-harm behavior (Mehlum et al., Citation2014).
FIGURE 1. A Receiver Operating Characteristic (ROC) analysis. Sensitivity and specificity of the different numbers of days with NSSI last year against level of global function (CGAS).
All statistical analyses were performed using SPSS 27.0, and significance level was set to .05.
RESULTS
Sample characteristics, psychopathology and self-harm
A total of 103 adolescents with a mean age of 15.9 years (SD = 1.47), the majority identifying as female (86.4%), participated in the study. Participants received a mean number of 3.2, (range = 0–8), DSM-5 diagnoses with mood disorders and anxiety disorders being the most prevalent. Cutting was the most commonly reported NSSI method (93.2%), followed by self-battery (41.7%), and stabbing (16.3%). Mean number of self-harm methods was 2.7 (range 1–10) and mean level of global functioning (CGAS) was 53.3 (range 31–85, SD = 9.2). For details on sample characteristics, see and .
TABLE 1. Diagnostic and clinical characteristics of adolescents with repetitive self-harm behavior (NSSI and suicide attempts) (N = 103) with current DSM-5 cutoff threshold Criterion A ≥ 5 NSSI episodes last year.
TABLE 2. Self-harm characteristics (NSSI and suicidal behavior) and psychopathology, in a clinical sample of adolescents (N = 103) with recurrent self-harm behavior and NSSID based on DSM-5 cutoff threshold Criterion A ≥ 5 NSSI episodes last year.
Based on the current DSM-5 threshold Criterion A being at least 5 days of NSSI last year, adolescents with NSSID (n = 56) were more likely to have a mood disorder, anxiety disorder or borderline personality disorder (), but not a higher number of DSM-5 diagnoses, compared to adolescents without NSSID (n = 47). Adolescents with NSSID reported significantly higher frequencies of NSSI episodes, and they had used a significantly higher number of self-harm methods. There were no significant differences between the groups with respect to reporting at least one suicide attempt, but adolescents with NSSID reported a significantly higher number of suicide attempts ().
Factors discriminating between participants with and without NSSID
Based on the current threshold NSSID Criterion A (at least 5 days with NSSI last year), the significant variables from the t-test were followed up in a discriminant function analysis showing that all 8 predictor variables (number of days with NSSI last year, level of global functioning, age of self-harm onset, number of self-harm methods, level of emotion regulation difficulties, level of suicide ideation, levels of depression and anxiety symptoms) contributed significantly to the variance (53.1%, canonical r2 = 0.74), between the two groups (). Structure Matrix, which holds the correlations (loadings) between the predictor variables and the discriminant function, showed that number of days of NSSI last year (r = 0.86) and level of global functioning (r = −0.42) were the strongest predictors for an NSSID diagnosis. Next, we examined which of the variables that would best discriminate between participants with and without NSSID when we excluded the variable “number of days with NSSI last year” from the analysis. Structure Matrix showed that level of global functioning was now the strongest discriminating variable, followed by level of depressive symptoms, number of self-harm methods and level of anxiety symptoms ().
TABLE 3. Summary of interpretive measures for discriminant function analysis in a clinical sample of adolescents (N = 103) with recurrent self-harm behavior and NSSID based on DSM-5 cutoff threshold Criterion A ≥ 5 NSSI episodes last year.
Sensitivity and specificity of threshold Criterion A
The results from the ROC analysis, which was based on a CGAS cutoff score at ≤56, showed that the area under the curve (AUC), which reflects the overall accuracy of the threshold Criterion A in differentiating between participants with and without NSSID (Kirkwood & Sterne, Citation2003), was 0.74 (95% CI: 0.64–0.82; p = 0.000), (). A frequency of 14.5 (≈ 15) NSSI episodes were associated with acceptable sensitivity (0.74) and specificity (0.73). (The coordinates of the ROC curve are presented in supplementary material).
Factors discriminating between participants with and without NSSID using the optimal cutoff value
Based on the results from the ROC-analysis and using the optimal cutoff level of 15 days with NSSI last year as a diagnostic threshold criterion, all analyses were rerun. Results now showed that 46.6% (n = 48) of the participants met full criteria for NSSID (full presentation of results in supplementary material). A new discriminant function analysis was conducted with the new set of significant predictor variables (number of days with NSSI episodes last year, level of global functioning, number of self-harm methods, level of emotion regulation difficulties, level of depression symptoms, level of anxiety symptoms and level of borderline symptoms). Together, the predictor variables explained 54.3% of the variance between the groups (canonical r2 = 0.74). Structure Matrix showed that number of days with NSSI last year and level of global functioning were the strongest predictors, while level of borderline symptoms predicted the least (r = 0.19).
When the predictor variable “number of NSSI episodes last year” was excluded from the discriminant analysis, the strongest predictors were level of global functioning, level of depressive symptoms, number of self-harm methods and level of anxiety, whereas level of borderline symptoms still predicted the least. In an additional analysis (not shown), we switched the variable “borderline symptoms (BSL)” with the variable “sum of borderline personality disorder (BPD) criteria» and found similar results.
DISCUSSION
In this study of 103 adolescents with recurrent self-harm behavior, we examined the proposed DSM-5 disorder, Non-suicidal Self-injury Disorder (NSSID), and studied the characteristics of the disorder as well as whether the current cutoff of NSSI frequency used to diagnose the disorder is appropriate.
Our main findings were that participants who met the criteria for NSSID reported significantly more frequent NSSI behavior and suicide attempts, higher levels of psychopathology and lower global functioning than participants who did not meet these criteria. Adolescents with and without NSSID were best discriminated by the number of days with NSSI last year, level of global functioning, level of depressive symptoms, number of self-harm methods and level of anxiety symptoms. Furthermore, our analyses indicated that 15 days with NSSI last year was the optimal cutoff level for a diagnosis of NSSID and applying this as an alternative Criterion A led to a reduction in the rate of adolescents diagnosed with NSSID from 54% (with current DSM-5 Criterion A cutoff level), to 46%.
Firstly, our novel finding that adolescents with NSSID had a significantly higher number of suicide attempts than adolescents who self-harm without this disorder, suggests that adolescents with recurrent NSSI in general, and NSSID in particular, may be more at risk than previously known. This indicates that strategies of early assessment and treatment for this group of adolescents are particularly important to reduce current and future suicidal behavior (Mehlum et al., Citation2014). It also suggests that clinicians must be careful not to underestimate the severity of NSSI due to its “non-suicidal” intention since such recurrent non-suicidal behavior increases the risk of suicide attempts (Chesin et al., Citation2017; Griep & MacKinnon, Citation2022).
Our findings that the number of days with NSSI last year, number of self-harm methods, and level of psychopathology were significantly higher in adolescents with NSSID, corresponds well with previous studies (In-Albon et al., Citation2013; Muehlenkamp et al., Citation2017; Whitlock et al., Citation2013), which suggests that adolescents with NSSID are at risk of a more severe trajectory, compared to self-harming adolescents without NSSID. However, studies with more diverse adolescent samples are needed to examine NSSID over time, for further validation of the NSSID and to study the prospective trajectory of this diagnosis.
Secondly, our results clearly show that NSSI is strongly associated with reduced global functioning, even though the behavior may give short-term subjective relief from distress and suffering. The capacity of NSSI to reduce negative emotion and discomfort is precisely at the core of this recurrent behavior, but the relief is short-lived and often associated with the development of tolerance (leading to increasing frequency and severity of the NSSI behavior) and dependence (can’t do without it), (American Psychiatric Association, Citation2013, p. 804). One of the diagnostic criteria in the NSSID, Criterion E, requires the NSSI behavior or its consequences to cause significant distress and interfere with important areas of functioning, such as interpersonal or academic areas (American Psychiatric Association, Citation2013). This criterion is, however, very challenging to assess, since many adolescents report that their self-harm actually reduces suffering, at least for a short period of time (Cipriano et al., Citation2017; Zetterqvist et al., Citation2020). Although the current study did not investigate this topic specifically, we noticed that it was difficult for the teenagers to know what the exact consequences of their self-harm really were, which corresponds well with the findings of Zetterqvist et al. (Citation2020) where adolescents not meeting the criterion E attributed their impairment to other diagnoses or problems unrelated to NSSI. It may be that the criterion E, as currently formulated in DSM-5, is defined too narrowly, and that further instructions on how this criterion should be operationalized seem warranted in order not to falsely exclude individuals. Our finding that level of global assessment of functioning differentiated well between self-harming adolescents with, and without NSSID, could imply that to use some form of global function measure in the diagnostic assessment could increase the validity of the criterion E.
Thirdly, when we increased the NSSI cutoff level from 5 to 15 days, the rate of NSSID was reduced from 54% to 46%. However, this altered cutoff level was still associated with mostly the same variables predicting a diagnosis of NSSID (number of days with NSSI last year, number of self-harm methods, and level of psychopathology). These clinical variables seem, therefore, relatively robust at discriminating between those with or without NSSID, in this sample. On the other hand, it may be that in clinical samples, where frequency of NSSI is high, minor changes in the cutoff level will not be enough to significantly differentiate between groups or clinical variables. However, if the cutoff level increases too much to better distinguish between clinical groups, there is a potential risk that NSSID sub-threshold individuals who also struggle with NSSI and who could benefit from treatment, will not be detected.
Finally, it is important to mention that although we found that BSL (and BPD) were significantly associated with NSSID, the discriminant analyses showed that these factors discriminated the least between those with and without NSSID, even when excluding the number of NSSI episodes last year from the analysis. The results may suggest that NSSID and BPD are closely related but distinct clinical phenomena, and are thus in support of other studies (Glenn & Klonsky, Citation2013; In-Albon et al., Citation2013) finding that NSSID and BPD overlap, but that the overlap is no greater than that between other DSM-5 disorders.
Strengths and Limitations
Our findings should be interpreted in the light of some methodological limitations, primarily that the cross-sectional design adopted precludes any longitudinal or causal conclusions, such as predicting risk based on the NSSID diagnosis. Also, as with most similar previous studies, the limited number of males (13.6%) in this sample prevents us from generalizing findings to males in clinical populations. Also, the limited sample size precluded analyses of some smaller subgroups. Among the strengths of this study are that it was based on a clinical sample of adolescents and that structured interviews were used, with good interrater reliability, to assess all the proposed DSM-5 diagnostic NSSID criteria and other clinical diagnoses enabling reliable comparisons with other studies. Future studies with more diverse samples and more males and with a longitudinal design with repeated measurements are needed to establish the predictive validity of the NSSID diagnosis as well as increase generalizability of findings to a broader clinical population.
CONCLUSIONS
This study examined the suggested DSM-5 disorder, Non-suicidal Self-injury Disorder (NSSID), in adolescents with recurrent self-harm behavior, and studied the characteristics of the disorder as well as whether the current cutoff of NSSI frequency used to diagnose the disorder is appropriate. Our findings, that NSSID is a highly impairing disorder should merit considerable interest and attention from clinicians as well as researchers, and underlines the importance of early detection and treatment. According to our results, clinical factors that could aid such detection should focus on number of days with NSSI last year, number of self-harm methods used by adolescents, their level of symptoms of anxiety and depression and their global functioning. To avoid over-diagnosing of NSSID, it may be useful to adopt a more conservative cutoff level for number of days with NSSI last year; our findings suggest at least 15 days with NSSI behavior as a more optimal level leading to a reduction in the rate of adolescents diagnosed with NSSID from 54% (with current DSM-5 Criterion A threshold) to 46%. Future prospective longitudinal studies with diverse adolescent samples are needed to further validate the psychometric properties of the NSSID diagnosis and its clinical utility.
ETHICAL APPROVAL
The study was approved by the Regional Committee for Medical Research Ethics, South-East Norway. All methods were carried out in accordance with relevant guidelines and regulations.
CONSENT FORM
Adolescents and their parents provided written informed consent prior to inclusion.
AUTHOR NOTES
Anne Brager-Larsen and Pål Zeiner, Division of Mental Health and Addiction, Department of Research and Innovation, Child and Adolescent Mental Health Research Unit, Oslo University Hospital, Norway. Lars Mehlum, National Centre for Suicide Research and Prevention, Institute of Clinical Medicine, University of Oslo, Norway.
Supplemental Material
Download MS Word (14.4 KB)ACKNOWLEDGEMENTS
The authors wish to thank the patients, clinicians and leaders at the participating clinics.
DISCLOSURE STATEMENT
No potential conflict of interest was reported by the author(s).
DATA AVAILABILITY STATEMENT
The datasets analyzed during the current study are available from the corresponding author on reasonable request. We have only used standard questionnaires and interviews that have been previously published elsewhere, and in according to guidelines.
Additional information
Funding
REFERENCES
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5 (5th ed. ed.). Washington, DC: American Psychiatric Association.
- Ammerman, B. A., Jacobucci, R., & McCloskey, M. S. (2019). Reconsidering important outcomes of the nonsuicidal self-injury disorder diagnostic criterion A. Journal of Clinical Psychology, 75(6), 1084–1097. doi:10.1002/jclp.22754
- Bjureberg, J., Ohlis, A., Ljótsson, B., D'Onofrio, B. M., Hedman-Lagerlöf, E., Jokinen, J., … Hellner, C. (2019). Adolescent self-harm with and without suicidality: Cross-sectional and longitudinal analyses of a Swedish regional register. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 60(3), 295–304. doi:10.1111/jcpp.12967
- Bohus, M., Limberger, M. F., Frank, U., Chapman, A. L., Kühler, T., & Stieglitz, R.-D. (2007). Psychometric properties of the Borderline Symptom List (BSL). Psychopathology, 40(2), 126–132. doi:10.1159/000098493 17215599
- Borschmann, R., Hogg, J., Phillips, R., & Moran, P. (2012). Measuring self-harm in adults: a systematic review. European Psychiatry : The Journal of the Association of European Psychiatrists, 27(3), 176–180. doi:10.1016/j.eurpsy.2011.04.005 21696926
- Brausch, A. M., Muehlenkamp, J. J., & Washburn, J. J. (2016). Nonsuicidal self-injury disorder: Does Criterion B add diagnostic utility? Psychiatry Research, 244, 179–184. doi:10.1016/j.psychres.2016.07.025
- Buelens, T., Luyckx, K., Kiekens, G., Gandhi, A., Muehlenkamp, J. J., & Claes, L. (2020). Investigating the DSM-5 criteria for non-suicidal self-injury disorder in a community sample of adolescents. Journal of Affective Disorders, 260, 314–322. doi:10.1016/j.jad.2019.09.009
- Castellví, P., Lucas-Romero, E., Miranda-Mendizábal, A., Parés-Badell, O., Almenara, J., Alonso, I., … Alonso, J. (2017). Longitudinal association between self-injurious thoughts and behaviors and suicidal behavior in adolescents and young adults: A systematic review with meta-analysis. Journal of Affective Disorders, 215, 37–48. doi:10.1016/j.jad.2017.03.035
- Chesin, M. S., Galfavy, H., Sonmez, C. C., Wong, A., Oquendo, M. A., Mann, J. J., & Stanley, B. (2017). Nonsuicidal self-injury is predictive of suicide attempts among individuals with mood disorders. Suicide & Life-Threatening Behavior, 47(5), 567–579. doi:10.1111/sltb.12331
- Cipriano, A., Cella, S., & Cotrufo, P. (2017). Nonsuicidal self-injury: A systematic review. Frontiers in Psychology, 8, 1946. doi:10.3389/fpsyg.2017.01946
- Derogatis, L. R., Lipman, R. S., Rickels, K., Uhlenhuth, E. H., & Covi, L. (1974). The Hopkins Symptom Checklist (HSCL): A self-report symptom inventory. Behavioral Science, 19(1), 1–15. doi:10.1002/bs.3830190102
- Glenn, C. R., & Klonsky, E. D. (2013). Nonsuicidal self-injury disorder: An empirical investigation in adolescent psychiatric patients. Journal of Clinical Child and Adolescent Psychology, 42(4), 496–507. doi:10.1080/15374416.2013.794699
- Gratz, K. L., & Roemer, L. (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment, 26(1), 41–54. doi:10.1023/B:JOBA.0000007455.08539.94
- Gratz, K. L., Dixon-Gordon, K. L., Chapman, A. L., & Tull, M. T. (2015). Diagnosis and characterization of DSM-5 nonsuicidal self-injury disorder using the clinician-administered nonsuicidal self-injury disorder index. Assessment, 22(5), 527–539. doi:10.1177/1073191114565878
- Griep, S. K., & MacKinnon, D. F. (2022). Does Nonsuicidal Self-Injury Predict Later Suicidal Attempts? A Review of Studies. Archives of Suicide Research : official Journal of the International Academy for Suicide Research, 26(2), 428–446. doi:10.1080/13811118.2020.1822244 32985383
- Hawton, K. (2007). Psychiatric assessment and management of deliberate self-poisoning patients. Medicine, 35(10), 565–569. doi:10.1016/j.mpmed.2007.07.015
- Hawton, K., Saunders, K. E., & O'Connor, R. C. (2012). Self-harm and suicide in adolescents. Lancet (London, England), 379(9834), 2373–2382. doi:10.1016/s0140-6736(12)60322-5
- Heyerdahl, S., Kvernmo, S., & Wichstrøm, L. (2004). Self-reported behavioural/emotionalproblems in Norwegian adolescents from multiethnicareas. European Child & Adolescent Psychiatry, 13(2), 64–72. doi:10.1007/s00787-004-0359-1
- In-Albon, T., Ruf, C., & Schmid, M. (2013). Proposed diagnostic criteria for the DSM-5 of nonsuicidal self-injury in female adolescents: Diagnostic and clinical correlates. Psychiatry Journal, 2013, 159208. doi:10.1155/2013/159208
- Kaufman, J., Birmaher, B., Brent, D., Rao, U., Flynn, C., Moreci, P., … Ryan, N. (1997). Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry, 36(7), 980–988. doi:10.1097/00004583-199707000-00021
- Kiekens, G., Hasking, P., Claes, L., Mortier, P., Auerbach, R. P., Boyes, M., … Bruffaerts, R. (2018). The DSM-5 nonsuicidal self-injury disorder among incoming college students: Prevalence and associations with 12-month mental disorders and suicidal thoughts and behaviors. Depression and Anxiety, 35(7), 629–637. doi:10.1002/da.22754
- Kirkwood, B. R., & Sterne, J. A. C. (2003). Essential medical statistics (2nd ed.). Malden: Blackwell.
- Klonsky, E. D. (2007). The functions of deliberate self-injury: A review of the evidence. Clinical Psychology Review, 27(2), 226–239. doi:10.1016/j.cpr.2006.08.002
- Klonsky, E. D., & Muehlenkamp, J. J. (2007). Self-injury: A research review for the practitioner. Journal of Clinical Psychology, 63(11), 1045–1056. doi:10.1002/jclp.20412
- Landis, J. R., & Koch, G. G. (1977). The measurement of observer agreement for categorical data. Biometrics, 33(1), 159–174. doi:10.2307/2529310
- Linehan, M. M., Comtois, K. A., Brown, M. Z., Heard, H. L., & Wagner, A. (2006). Suicide Attempt Self-Injury Interview (SASII): development, reliability, and validity of a scale to assess suicide attempts and intentional self-injury. Psychological Assessment, 18(3), 303–312. doi:10.1037/1040-3590.18.3.303 16953733
- Lundh, A., Forsman, M., Serlachius, E., Långström, N., Lichtenstein, P., & Landén, M. (2016). Psychosocial functioning in adolescent patients assessed with Children’s Global Assessment Scale (CGAS) predicts negative outcomes from age 18: A cohort study. Psychiatry Research, 242, 295–301. doi:10.1016/j.psychres.2016.04.050
- Mehlum, L., Tørmoen, A. J., Ramberg, M., Haga, E., Diep, L. M., Laberg, S., … Grøholt, B. (2014). Dialectical behavior therapy for adolescents with repeated suicidal and self-harming behavior: A randomized trial. Journal of the American Academy of Child and Adolescent Psychiatry, 53(10), 1082–1091. doi:10.1016/j.jaac.2014.07.003
- Meule, A., Michalek, S., Friederich, H. C., & Brockmeyer, T. (2020). Confirmatory factor analysis of the Barratt Impulsiveness Scale-short form (BIS-15) in patients with mental disorders. Psychiatry Research, 284, 112665. doi:10.1016/j.psychres.2019.112665
- Montgomery, S. A., & Asberg, M. (1979). A new depression scale designed to be sensitive to change. The British Journal of Psychiatry, 134, 382–389. doi:10.1192/bjp.134.4.382
- Muehlenkamp, J. J., & Brausch, A. M. (2016). Reconsidering criterion A for the diagnosis of non-suicidal self-injury disorder. Journal of Psychopathology and Behavioral Assessment, 38(4), 547–558. doi:10.1007/s10862-016-9543-0
- Muehlenkamp, J. J., Brausch, A. M., & Washburn, J. J. (2017). How much is enough? Examining frequency criteria for NSSI disorder in adolescent inpatients. Journal of Consulting and Clinical Psychology, 85(6), 611–619. doi:10.1037/ccp0000209
- Muehlenkamp, J. J., Claes, L., Havertape, L., & Plener, P. L. (2012). International prevalence of adolescent non-suicidal self-injury and deliberate self-harm. Child and Adolescent Psychiatry and Mental Health, 6, 10. doi:10.1186/1753-2000-6-10
- Muehlenkamp, J. J., Ertelt, T. W., Miller, A. L., & Claes, L. (2011). Borderline personality symptoms differentiate non-suicidal and suicidal self-injury in ethnically diverse adolescent outpatients. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 52(2), 148–155. doi:10.1111/j.1469-7610.2010.02305.x
- Posner, K., Melvin, G. A., Stanley, B., Oquendo, M. A., & Gould, M. (2007). Factors in the assessment of suicidality in youth. CNS Spectrums, 12(2), 156–162. doi:10.1017/s1092852900020678
- Reynolds, W. M., & Mazza, J. J. (1999). Assessment of suicidal ideation in innercity children and young adolescents: Reliability and validity of the suicidal ideation questionnaire–JR. School Psychology Review, 28(1), 17–30. doi:10.1080/02796015.1999.12085945
- Selby, E. A., Bender, T. W., Gordon, K. H., Nock, M. K., & Joiner, T. E. Jr. (2012). Non-suicidal self-injury (NSSI) disorder: A preliminary study. Personality Disorders, 3(2), 167–175. doi:10.1037/a0024405
- Selby, E. A., Kranzler, A., Fehling, K. B., & Panza, E. (2015). Nonsuicidal self-injury disorder: The path to diagnostic validity and final obstacles. Clinical Psychology Review, 38, 79–91. doi:10.1016/j.cpr.2015.03.003
- Shaffer, D., Gould, M. S., Brasic, J., Ambrosini, P., Fisher, P., Bird, H., & Aluwahlia, S. (1983). A Children’s Global Assessment Scale (CGAS). Archives of General Psychiatry, 40(11), 1228–1231. doi:10.1001/archpsyc.1983.01790100074010
- Sharp, C., Ha, C., Michonski, J., Venta, A., & Carbone, C. (2012). Borderline personality disorder in adolescents: evidence in support of the Childhood Interview for DSM-IV Borderline Personality Disorder in a sample of adolescent inpatients. Comprehensive Psychiatry, 53(6), 765–774. doi:10.1016/j.comppsych.2011.12.003 22300904
- Szewczuk-Bogusławska, M., Kaczmarek-Fojtar, M., Moustafa, A. A., Mahlberg, J., Frydecka, D., Oleszkowicz, A., … Misiak, B. (2018). Assessment of the frequency criterion for the diagnosis of non-suicidal self-injury disorder in female adolescents with conduct disorder. Psychiatry Research, 267, 333–339. doi:10.1016/j.psychres.2018.05.054
- Tabachnick, B. G., & Fidell, L. S. (2018). Using multivariate statistics (7th ed.). Upper Saddle River: Pearson.
- Washburn, J. J., Potthoff, L. M., Juzwin, K. R., & Styer, D. M. (2015). Assessing DSM-5 nonsuicidal self-injury disorder in a clinical sample. Psychological Assessment, 27(1), 31–41. doi:10.1037/pas0000021
- Whitlock, J., Muehlenkamp, J., Eckenrode, J., Purington, A., Baral Abrams, G., Barreira, P., & Kress, V. (2013). Nonsuicidal self-injury as a gateway to suicide in young adults. The Journal of Adolescent Health, 52(4), 486–492. doi:10.1016/j.jadohealth.2012.09.010
- Wilkinson, P., Kelvin, R., Roberts, C., Dubicka, B., & Goodyer, I. (2011). Clinical and psychosocial predictors of suicide attempts and nonsuicidal self-injury in the Adolescent Depression Antidepressants and Psychotherapy Trial (ADAPT). The American Journal of Psychiatry, 168(5), 495–501. doi:10.1176/appi.ajp.2010.10050718
- Zanarini, M. C., Vujanovic, A. A., Parachini, E. A., Boulanger, J. L., Frankenburg, F. R., & Hennen, J. (2003). Zanarini Rating Scale for Borderline Personality Disorder (ZAN-BPD): A continuous measure of DSM-IV borderline psychopathology. Journal of Personality Disorders, 17(3), 233–242. doi:10.1521/pedi.17.3.233.22147
- Zetterqvist, M. (2015). The DSM-5 diagnosis of nonsuicidal self-injury disorder: A review of the empirical literature. Child and Adolescent Psychiatry and Mental Health, 9, 31. doi:10.1186/s13034-015-0062-7
- Zetterqvist, M., Perini, I., Mayo, L. M., & Gustafsson, P. A. (2020). Nonsuicidal self-injury disorder in adolescents: Clinical utility of the diagnosis using the clinical assessment of nonsuicidal self-injury disorder index. Frontiers in Psychiatry, 11, 8. doi:10.3389/fpsyt.2020.00008

