Abstract
Aim
Given that patients with cancer may commit suicide due to physical and mental problems, the present study objectives were to identify particular risk factors of different subgroup of patients including type of cancer, gender, age, type and time of suicide, and geographical region to facilitate early care and psychosocial support.
Methods
A comprehensive review of databases including Embase, Scopus, PubMed, and Web of Science was conducted for original articles published in English from January 2000 to March 2022. It is based on the PRISMA checklist.
Results
After reviewing 69 articles selected from 15 countries, the total prevalence rate of suicide among 34,157,856 patients with cancer was estimated 67,169, at 0.013 (95% CI, 0.008–0.021). The highest suicide prevalence was related to gastrointestinal cancer, estimated at 0.204 (95% CI, 0.161–0.255). A gender-based meta-analysis showed that the prevalence of suicide/suicidal ideation was higher among men, estimated at 0.013 (95% CI, 0.008–0.023) compared with women, at 0.006 (95% CI, 0.002–0.017).
Conclusion
Based on study results, suicide-prevention strategies should be aimed at patients younger than 40 years of age to effectively resolve their mental health disorders and promote their self-efficacy in successful management of the disease.
INTRODUCTION
Cancer represents the second leading cause of death worldwide, with an estimated 17 million deaths in 2030, accounting for approximately one in six deaths (Ribas et al., Citation2018). It is predicted that the total number of new cases will quickly increase to 29.4 million in the proceeding 20 years, reaching nearly 2 million deaths (Park et al., Citation2016). In addition, a cancer diagnosis can cause negative emotional feelings to patients, including pain, anxiety, stress, and depression during the treatment process. Thus, having both cancer and a psychological disorder is associated with decreased quality of life, increased risk of mortality particularly by suicide, poor adherence to medication, and diminished health outcomes (Klonsky, May, & Saffer, Citation2016; Sinyor, Tse, & Pirkis, Citation2017). Patients with cancer have a high prevalence of depression, which limits patients’ ability to suppress the disease. Furthermore, it reduces patients’ acceptance of their medication and leads to prolonged length of hospital stay (Amiri & Behnezhad, Citation2020). This negative emotion substantially increases the odds of future suicide attempts (Chochinov, Citation2001). Accordingly, literature has shown that individuals with cancer are at twice the risk of committing suicide compared to the general population (Ahn et al., Citation2015; Kye & Park, Citation2017; Yamauchi et al., Citation2014). During the years 2000 to 2016, Liu et al. found an increasing trend in suicide risk among patients with cancer which drew the attention of health professionals to this issue as preventable deaths (Liu et al., Citation2022). Higher suicide rates among patients with cancer were mainly mentioned to be associated with individuals with poor prognoses, such as those with stomach and pancreatic cancers, feelings of depression, lack of social support, vulnerability, interpersonal dysfunction, and prolonged unmanageable pain along with particular demographic characteristics such as age, gender, and specific cancer types (McFarland, Walsh, Napolitano, Morita, & Jaiswal, Citation2019).
Failure to mitigate risk of death by suicide among patients with cancer may lead to more morbidity and mortality. To obtain data in regard to suicide risk factors, it might be helpful to identify patients with cancer who are at the highest risk of suicide (Senf, Bender, & Fettel, Citation2022). Findings of related studies conducted between 1973 and 2002 revealed that the greatest suicide risks were found in patients with cancers of the head and neck (Kam et al., Citation2015). Development of study results until 2011 also confirmed that head and neck cancers were associated with the highest suicide rates, with three times more frequent suicides than in the general United States population (Zaorsky et al., Citation2019). Other studies reported the highest prevalence of suicide among patients with cancers of the respiratory system, followed by those with affected pharynx or cancer of plasma cells, bones and joints, the digestive system, and the nervous system (Zhang, Sun, Peng, Ma, & Tang, Citation2021). Male gender and age were also mentioned as risk factors for suicide among patients with cancer (Misono, Weiss, Fann, Redman, & Yueh, Citation2008; Spicer & Miller, Citation2000). The high prevalence of suicide in patients with cancer compared with the general population might be due to either patients’ willingness and attitude toward self-autonomy and self-control or severe depressive symptoms (Filiberti et al., Citation2001). Thus, all-inclusive cancer care should incorporate appropriate psychiatric intervention along with pain management with the purpose of minimizing suicidal ideation (Akechi, Okamura, Nishiwaki, & Uchitomi, Citation2002).
Despite the importance of the issue, only few meta-analyses have examined the prevalence of suicide and its associated risk factors among patients with cancer through a comprehensive literature search. The present study objectives were to identify particular risk factors of different subgroup of patients including type of cancer, gender, age, type and time of suicide, and geographical region to facilitate early care and psychosocial support.
METHODS
Registration and Reporting
The systematic review was registered with PROSPERO 2022, CRD42022333866 (available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022333866). The related methods are in line with the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (Page et al., Citation2021).
Databases and Search Terms
A comprehensive review of databases including Embase, Scopus, PubMed, and Web of Science was conducted for original articles published in English from January 2000 to March 2022 with the following search terms: (Suicide[MeSH Terms]) AND (((((((((((((Tumor[Title]) OR (Neoplasm[Title])) OR (Tumors[Title])) OR (Neoplasia[Title])) OR (Neoplasias[Title])) OR (Cancer[Title])) OR (Cancers[Title])) OR (Malignant Neoplasm[Title])) OR (Malignancy[Title])) OR (Malignancies[Title])) OR (Malignant Neoplasms[Title])) OR (Benign Neoplasms[Title])) OR (Benign Neoplasm[Title])).
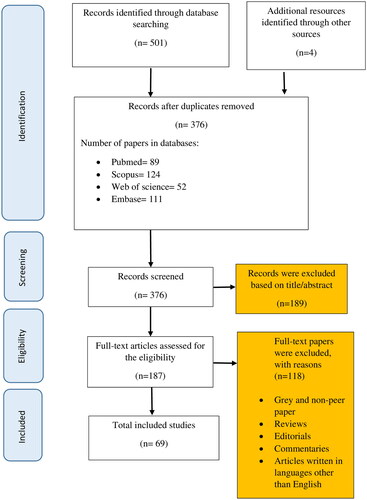
From the initial search of different electronic databases, a total of 505 articles were retrieved. After removing the duplicates, 376 articles remained for further review. To check the data relevancy, two independent researchers reviewed the titles and abstracts independently, leading to 187 articles. In the next step, the full texts of articles were deeply reviewed to collect all associated evidence that meets the eligibility criteria for the review. As a result, studies that incorporated data on the prevalence of suicide in patients with cancer or its determinants were considered for further review. Conference abstracts were also searched and the references of included articles were examined to be included as additional references. Finally, applying inclusion/exclusion criteria resulted in 69 studies which were included in the final review ().
Inclusion and Exclusion Criteria
Studies with quantitative data on prevalence among patients with cancer and its determinants were included to find a set of articles based on the research keywords. Different types of observational studies containing cross-sectional, case-study, case-series, prospective, and cohort were involved. Additionally articles published in English between January 2000 and March 2021 were considered in the review.
Exclusion criteria were other types of studies including interventional studies, case-control, reviews, letter to the editor, books, reports, and commentaries published in languages other than English. Furthermore, studies with inadequate data on research questions and those focusing on diagnosis approaches, therapeutic methods, and medication therapies were not included in the review.
Quality Assessment
To assess the risk of bias of included studies, the Newcastle-Ottawa Scale (NOS) was used. This checklist is a standard evaluating tool to assess the quality of studies based on dimensions including case definition, selection of controls, comparability of cases and controls, and exposure/outcome in three main sections of exposure/outcome ascertainment, selection of study groups, and their comparability. To assess risk of bias, each study was evaluated by two independent researchers; in case of any discrepancy, consensus was reached by consulting with a third party. The lowest and highest NOS scores for each of the evaluated articles could be in a range between 0 and 10, so that an article with score below 4 was mentioned to have a low level of quality (Wells et al., Citation2000).
Data Extraction
A data extraction form was used to enter the data of included studies by two independent investigators. The form included requisite information including first author’s name, publication date and country, data gathering tool, study design, study population, sampling method, region based on World Health Organization (WHO) classification, type of cancer, gender, age, time of suicide, risk of bias, and outcome measures such as the prevalence of suicide and its associated factors.
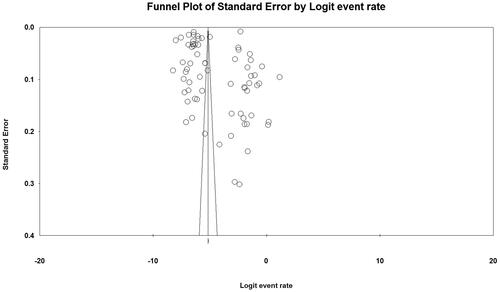
Statistical Analysis
The prevalence of depression was evaluated by random-effects model. In addition, subgroup analysis was used to determine heterogeneity based on different study settings and patients’ sociodemographic characteristics. Meta-analysis was performed using Comprehensive Meta-Analysis and R software. Finally, to examine the heterogeneity of preliminary studies, I2 test was used.
Patient and Public Involvement
No patients were involved.
RESULTS
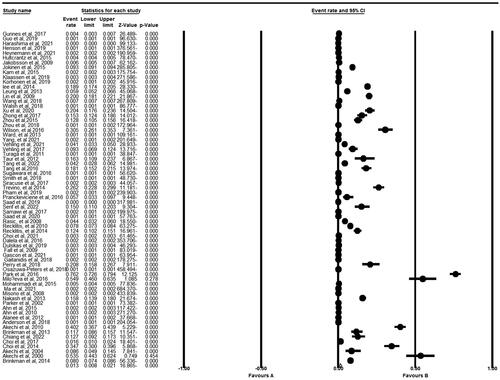
To report the findings of this review, PRISMA guidelines were employed. After reviewing 69 articles published from January 2000 to March 2021 in 15 countries, the total prevalence rate of suicide among 34,157,856 patients with cancer was estimated to be 67,169, at 0.013 (95% CI, 0.008–0.021) ().
Meta-Analysis Based on Countries, Continents, and WHO Regions
Based on meta-analysis, 15 countries were identified among 69 studies. Among these countries, Greece and Israel had the highest prevalence of suicide in patients with cancer, at 0.549 (95% CI, 0.46–0.635) and 0.158 (95% CI, 0.139–0.179), respectively. Furthermore, Australia and the United Kingdom were reported to have the lowest prevalence of suicide among these patients. Results based on continents revealed that Asia had the highest prevalence of suicide estimated at 0.067 (95% CI, 0.025–0.165) ().
TABLE 1. Subgroup analysis based on country, continent, and World Health Organization (WHO) region.
Meta-analysis based on different WHO regions also revealed that the Region of the Americas (AMR) had the lowest suicide rate at 0.006 (95% CI, 0.004–0.008). On the other hand, no studies were found to be conducted in Eastern Mediterranean region (EMR), Regional Office for Africa (AFRO), and South-East Asia regions (SEAR) ().
Meta-Analysis Based on Type of Cancer
According to the results based on cancer type, findings indicated that the highest suicide prevalence was related to gastrointestinal cancer, estimated at 0.204 (95% CI, 0.161–0.255), followed by breast cancer at 0.131 (95% CI, 0.080–0.176) and thoracic cancer at 0.116 (95% CI, 0.096–0.140), respectively ().
TABLE 2. Subgroup analysis based on type of cancer.
Meta-Analysis Based on Type and Time of Suicide
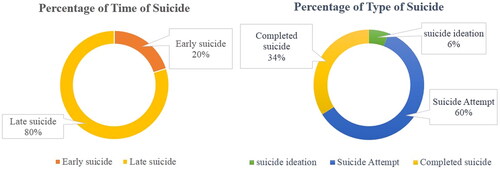
Study findings showed that out of 67,169 patients, 6% (n = 4,030) had suicidal ideation, 60% (n = 40,300) had unsuccessful suicide, and 34% (n = 22,839) had completed suicide (). Furthermore, 20% of patients had suicidal ideation during the first year after cancer diagnosis, and the rest experienced suicidal tendencies a year after being diagnosed with the disease ().
Meta-Analysis Based on Gender
A gender-based meta-analysis showed that the prevalence of suicide/suicidal ideation was higher among men estimated at 0.013 (95% CI, 0.008–0.023) compared with women at 0.006 (95% CI, 0.002–0.017) ().
TABLE 3. Meta-analysis based on gender.
Meta-Regression Based on Age and Year of Publication
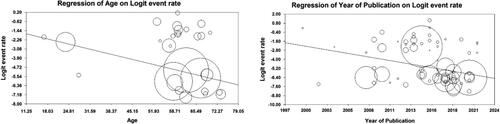
A meta-analysis affirmed a significant indirect relationship between suicide prevalence in cancer patients and year of study publication (p < .05), so that a unit of increase in the study year led to a decreased rate in suicide prevalence. Furthermore, an inverse relationship between patient’s age and suicide prevalence was observed based on the meta-analysis ().
Meta-Regression for Quality Assessment
In case of study quality assessment, more than half of the included studies (n = 47) had high quality, while 16 studies were of medium quality and the other 6 studies were of low quality ().
TABLE 4. Meta-regression based on quality assessment tool.
DISCUSSION
Overview
Our meta-analysis of 69 studies revealed that the total prevalence rate of suicide among 34,157,856 patients with cancer was estimated at 0.013. Several factors associated with suicide among study patients were found, including age, gender, place of residence, type of cancer, and year of study publication. Knowing more about suicide in the patients with diagnosed cancer is necessary both for healthcare providers and caregivers due to being familiar with associated risk factors as well as for health authorities to organize and implement preventive measures. The average total score of suicide among patients with cancer in our review was reported to be 0.013, which was lower than the rate estimated in Denmark for both male and female patients, at 1.7 and 1.4, respectively (Yousaf, Christensen, Engholm, & Storm, Citation2005). Furthermore, the higher prevalence of suicide among patients with cancer was observed in studies conducted by Hem et al. and Björkenstam et al., with corresponding mortality ratio of 1.55 and 2.5 (Björkenstam, Edberg, Ayoubi, & Rosén, Citation2005; Zaorsky et al., Citation2017). In another study by Zaorsky et al., an extremely high mortality rate of 4.44 was estimated, which highlighted a more than fourfold increase in suicide risk among patients with cancer (Zaorsky et al., Citation2017). These inconsistencies with our study findings might be due to the differences in the baseline risks of comparison groups or as a result of different characteristics of included patients with multiple primary tumors, which could threaten the validity of study results.
Gender
Our review also revealed that a greater suicide risk was correlated with male gender. Research data obtained by Kendal et al. in the United States affirmed this finding and added that the suicide prevalence was higher in men, equating to 19 deaths per 10,000 male patients compared to 4 deaths per 10,000 women (Kendal, Citation2007). In addition, our review affirmed a significant association between risk of suicide and cancer sites/organ system.
Cancer Type
The greatest suicide rate was found in patients with gastrointestinal cancer, followed by those with breast cancer and thoracic/lung cancers. However, the anatomic sites associated with increased suicide rates differed in various literatures. For example, a study by Misono et al. found that the highest suicide rates were associated with lung, gastrointestinal system, and head and neck cancers (Misono et al., Citation2008). Similar to our meta-analysis findings, the elevated suicide rates in patients with lung and gastric cancer were related to emotional distress and lower quality of life in patients (Carlsen, Jensen, Jacobsen, Krasnik, & Johansen, Citation2005; Nordin & Glimelius, Citation1997; Sarna et al., Citation2002). Therefore, our analysis suggests that healthcare providers should pay more attention to patients’ psychological experiences as patients with cancer encounter high levels of mental distress and psychosocial challenges.
Age
Our review revealed a high rate of suicide among adolescent and young adults with cancer. In fact, as these groups of patients are at an early stage of education, occupation, and family life, they are subjected to more psychological pressures which rapidly deteriorate their physical and mental condition. Young adult patients with cancer encounter several challenges after diagnosis, such as diminished chance to continue their job and educational growth or even maintain their family life balance (Pang et al., Citation2008). In addition, cancer incidence among adolescents and young adults has been proven to be considerably more common than older population (Langeveld et al., Citation2003; Trama, Botta, & Steliarova-Foucher, Citation2018). A study by Yang et al. highlighted that patients aged 20 to 24 years old had the highest rates of suicide (Yang et al., Citation2019). Another study also found that younger patients were more likely to have poorer survival outcomes and advanced disease at diagnosis than were older patients (Wu et al., Citation2017; Xiao, Cao, Qiu, Wang, & Wang, Citation2013).
Territory
Analyzing suicide rates among people with cancer in different countries showed higher rates in the United States, Greece, and Israel than in Europe, Asia, or Australia (Yang et al., Citation2019). The type of financing system in the health systems of mentioned countries together with economic costs of chronic diseases such as cancer might result in greater probability of therapy withdrawal, particularly among individuals from lower socioeconomic levels, which may bring them disappointment and a desire to end their lives or attempt suicide. On the other hand, most European countries have universal health coverage and easy access to healthcare services, which facilitate cancer therapy without imposing financial burden to citizens (Jones & Kantarjian, Citation2019). Studies conducted in England and the United States have asserted that urgent health promotion strategies among patients with cancer should be implemented with logical costs to eliminate depression and associated risk of suicide (Guo et al., Citation2019).
LIMITATION
Our study has some limitations. First, our review has been restricted to studies published in English, which might exclude relevant researches. Second, lack of data for some of the countries including EMRO, AFRO, and SEAR restricted the generalizability of our findings. Third, we were incapable of evaluating the potential confounding role of comorbidities such as medical or psychological disorders on the prevalence of suicide among patients with cancer. Furthermore, we did not mention the role of unhealthy lifestyle or harmful behaviors such as tobacco and alcohol use as associated factors for increased risk of suicide.
CONCLUSION
This systematic review identified several risk factors that affect the prevalence of suicide among patients with cancer worldwide. Based on study results, suicide-prevention strategies should be aimed at patients younger than 40 years of age to effectively address their mental health disorders and promote their self-efficacy in successful management of the disease.
AUTHORS’ CONTRIBUTIONS
Conception and design of study: Samira Raoofi, Ahmad Ghashghaee, Fatemeh Pashazadeh Kan. Acquisition of data: Farzaneh Bagheribayati, Fatemeh Pashazadeh Kan, Samira Raoofi, Akbar Javan Biparva, Zahra Noorani Mejareh, Mohaddeseh Sanaei, Yasamin Dolati, Bahare Abdollahi. Analysis and/or interpretation of data: Samira Raoofi, Ahmad Ghashghaee, Fatemeh Pashazadeh Kan. Drafting the manuscript: Sima Rafiei, Ahmad Ghashghaee. Revising the manuscript critically for important intellectual content: Sima Rafiei, Ahmad Ghashghaee. Approval of the version of the manuscript to be published: Samira Raoofi, Ahmad Ghashghaee, Sima Rafiei, Elaheh Parnian
DISCLOSURE STATEMENT
The authors declare that they have no competing interests
Additional information
Notes on contributors
Sima Rafiei
Sima Rafiei, Social Determinants of Health Research Center, Research Institute for Prevention of Non-Communicable Diseases, Qazvin University of Medical Sciences, Qazvin, Iran.
Fatemeh Pashazadeh Kan
Fatemeh Pashazadeh Kan, Student Research Committee, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran.
Samira Raoofi
Samira Raoofi and Farnoosh Shafiee, Department of Health Services Management, School of Health Management and Information Sciences, Iran University of Medical Sciences, Tehran, Iran.
Farnoosh Shafiee
Samira Raoofi and Farnoosh Shafiee, Department of Health Services Management, School of Health Management and Information Sciences, Iran University of Medical Sciences, Tehran, Iran.
Maryam Masoumi
Maryam Masoumi, Clinical Research and Development Center, Qom University of Medical Sciences, Qom, Iran.
Farzaneh Bagheribayati
Farzaneh Bagheribayati, Cellular and Molecular Biology, University of Zanjan, Zanjan, Iran.
Akbar Javan Biparva
Akbar Javan Biparva, Student Research Committee, School of Health Management and Medical Informatics, Iranian Center of Excellence in Health Management, Tabriz University of Medical Sciences, Tabriz, Iran.
Zahra Noorani Mejareh
Zahra Noorani Mejareh, Student Research Committee, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
Mohaddeseh Sanaei
Mohaddeseh Sanaei, Student Research Committee, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran.
Yasamin Dolati
Yasamin Dolati, Student Research Committee, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran.
Bahare Abdollahi
Bahare Abdollahi, Student Research Committee, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
Saghar Khani
Saghar Khani, Student Research Committee, School of Medicine, Iran University of Medical Sciences, Tehran, Iran.
Elaheh Parnian
Elaheh Parnian, Department of Health Services Management, School of Health Management and Information Sciences, Iran University of Medical Sciences, Tehran, Iran.
Elmira Nosrati Sanjabad
Elmira Nosrati Sanjabad, Student Research Committee, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran.
Ahmad Ghashghaee
Ahmad Ghashghaee, The School of Medicine, Dentistry & Nursing, University of Glasgow, Glasgow, UK.
REFERENCES
- Ahn, M. H., Park, S., Lee, H. B., Ramsey, C. M., Na, R., Kim, S. O., … Hong, J. P. (2015). Suicide in cancer patients within the first year of diagnosis. Psycho-Oncology, 24(5), 601–607. doi:10.1002/pon.3705.
- Akechi, T., Okamura, H., Nishiwaki, Y., & Uchitomi, Y. (2002). Predictive factors for suicidal ideation in patients with unresectable lung carcinoma: A 6‐month follow‐up study. Cancer, 95(5), 1085–1093. doi:10.1002/cncr.10769.
- Amiri, S., & Behnezhad, S. (2020). Cancer diagnosis and suicide mortality: A systematic review and meta-analysis. Archives of Suicide Research: Official Journal of the International Academy for Suicide Research, 24(sup2), S94–S112. doi:10.1080/13811118.2019.1596182.
- Björkenstam, C., Edberg, A., Ayoubi, S., & Rosén, M. (2005). Are cancer patients at higher suicide risk than the general population? Scandinavian Journal of Public Health, 33(3), 208–214. doi:10.1080/14034940410019226.
- Carlsen, K., Jensen, A. B., Jacobsen, E., Krasnik, M., & Johansen, C. (2005). Psychosocial aspects of lung cancer. Lung Cancer (Amsterdam, Netherlands), 47(3), 293–300. doi:10.1016/j.lungcan.2004.08.002.
- Chochinov, H. M. (2001). Depression in cancer patients. The Lancet Oncology, 2(8), 499–505. doi:10.1016/S1470-2045(01)00456-9.
- Filiberti, A., Ripamonti, C., Totis, A., Ventafridda, V., De Conno, F., Contiero, P., & Tamburini, M. (2001). Characteristics of terminal cancer patients who committed suicide during a home palliative care program. Journal of Pain and Symptom Management, 22(1), 544–553. doi:10.1016/s0885-3924(01)00295-0.
- Guo, C., Zheng, W., Zhu, W., Yu, S., Ding, Y., Wu, Q., … Lu, C. (2019). Risk factors associated with suicide among kidney cancer patients: A surveillance, epidemiology, and end results analysis. Cancer Medicine, 8(11), 5386–5396. doi:10.1002/cam4.2400.
- Jones, G., & Kantarjian, H. (2019). The many roads to universal health care in the USA. The Lancet. Oncology, 20(10), e601–e605. doi:10.1016/S1470-2045(19)30517-0.
- Kam, D., Salib, A., Gorgy, G., Patel, T. D., Carniol, E. T., Eloy, J. A., … Park, R. C. W. (2015). Incidence of suicide in patients with head and neck cancer. JAMA Otolaryngology- Head & Neck Surgery, 141(12), 1075–1081. doi:10.1001/jamaoto.2015.2480.
- Kendal, W. S. (2007). Suicide and cancer: A gender-comparative study. Annals of Oncology: Official Journal of the European Society for Medical Oncology, 18(2), 381–387. doi:10.1093/annonc/mdl385.
- Klonsky, E. D., May, A. M., & Saffer, B. Y. (2016). Suicide, suicide attempts, and suicidal ideation. Annual Review of Clinical Psychology, 12(1), 307–330. doi:10.1146/annurev-clinpsy-021815-093204.
- Kye, S.-Y., & Park, K. (2017). Suicidal ideation and suicidal attempts among adults with chronic diseases: A cross-sectional study. Comprehensive Psychiatry, 73, 160–167. doi:10.1016/j.comppsych.2016.12.001.
- Langeveld, N. E., Ubbink, M. C., Last, B. F., Grootenhuis, M. A., Voute, P. A., & De Haan, R. J. (2003). Educational achievement, employment and living situation in long‐term young adult survivors of childhood cancer in the Netherlands. Psycho-Oncology, 12(3), 213–225. doi:10.1002/pon.628.
- Liu, Q., Wang, X., Kong, X., Wang, Z., Zhu, M., Ren, Y., … Wang, J. (2022). Subsequent risk of suicide among 9,300,812 cancer survivors in US: A population-based cohort study covering 40 years of data. EClinicalMedicine, 44, 101295. doi:10.1016/j.eclinm.2022.101295.
- McFarland, D. C., Walsh, L., Napolitano, S., Morita, J., & Jaiswal, R. (2019). Suicide in patients with cancer: Identifying the risk factors. Oncology, 19;33(6), 221–226.
- Misono, S., Weiss, N. S., Fann, J. R., Redman, M., & Yueh, B. (2008). Incidence of suicide in persons with cancer. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology, 26(29), 4731–4738. doi:10.1200/JCO.2007.13.8941.
- Nordin, K., & Glimelius, B. (1997). Psychological reactions in newly diagnosed gastrointestinal cancer patients. Acta Oncologica (Stockholm, Sweden), 36(8), 803–810. doi:10.3109/02841869709001361.
- Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. International Journal of Surgery (London, England), 88, 105906. doi:10.1016/j.ijsu.2021.105906.
- Pang, J. W., Friedman, D. L., Whitton, J. A., Stovall, M., Mertens, A. C., Robison, L. L., & Weiss, N. S. (2008). Employment status among adult survivors in the Childhood Cancer Survivor Study. Pediatric Blood & Cancer, 50(1), 104–110. doi:10.1002/pbc.21226.
- Park, H.-M., Woo, H., Jung, S. J., Jung, K.-W., Shin, H.-R., & Shin, A. (2016). Colorectal cancer incidence in 5 Asian countries by subsite: An analysis of cancer incidence in five continents (1998–2007). Cancer Epidemiology, 45, 65–70. doi:10.1016/j.canep.2016.09.012.
- Ribas, J. J., Martins, J. T., Scholze, A. R., Galdino, M. J. Q., Santos, G. C., Oliveira, A. A., & Ribeiro, R. P. (2018). Causas da aposentadoria por invalidez de servidores públicos. Journal of Nursing and Health, 7(3), 20–55.
- Sarna, L., Padilla, G., Holmes, C., Tashkin, D., Brecht, M. L., & Evangelista, L. (2002). Quality of life of long-term survivors of non–small-cell lung cancer. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology, 20(13), 2920–2929. doi:10.1200/JCO.2002.09.045.
- Senf, B., Bender, B., & Fettel, J. (2022). Suicidal ideation, distress, and related factors in a population of cancer patients treated in a general acute hospital. Supportive Care in Cancer: Official Journal of the Multinational Association of Supportive Care in Cancer, 30(1), 487–496. doi:doi:10.1007/s00520-021-06429-w
- Sinyor, M., Tse, R., & Pirkis, J. (2017). Global trends in suicide epidemiology. Current Opinion in Psychiatry, 30(1), 1–6. doi:10.1097/YCO.0000000000000296.
- Spicer, R. S., & Miller, T. R. (2000). Suicide acts in 8 states: Incidence and case fatality rates by demographics and method. American Journal of Public Health, 90(12), 1885.
- Trama, A., Botta, L., & Steliarova-Foucher, E. (2018). Cancer burden in adolescents and young adults: A review of epidemiological evidence. Cancer Journal (Sudbury, Mass.), 24(6), 256–266. doi:10.1097/PPO.0000000000000346.
- Wells, G. A., Shea, B., O’Connell, D., Peterson, J., Welch, V., Losos, M., & Tugwell, P. (2000). The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses: Oxford.
- Wu, S.-G., Liao, X.-L., He, Z.-Y., Tang, L.-Y., Chen, X.-T., Wang, Y., & Lin, Q. (2017). Demographic and clinicopathological characteristics of nasopharyngeal carcinoma and survival outcomes according to age at diagnosis: A population-based analysis. Oral Oncology, 73, 83–87. doi:10.1016/j.oraloncology.2017.08.006.
- Xiao, G., Cao, Y., Qiu, X., Wang, W., & Wang, Y. (2013). Influence of gender and age on the survival of patients with nasopharyngeal carcinoma. BMC Cancer, 13(1), 226. doi:10.1186/1471-2407-13-226.
- Yamauchi, T., Inagaki, M., Yonemoto, N., Iwasaki, M., Inoue, M., Akechi, T., … Tsugane, S. (2014). Death by suicide and other externally caused injuries after stroke in Japan (1990–2010): The Japan public health center–based prospective study. Psychosomatic Medicine, 76(6), 452–459. doi:10.1097/PSY.0000000000000079.
- Yang, J., He, G., Chen, S., Pan, Z., Zhang, J., Li, Y., & Lyu, J. (2019). Incidence and risk factors for suicide death in male patients with genital-system cancer in the United States. European Journal of Surgical Oncology: The Journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology, 45(10), 1969–1976. doi:10.1016/j.ejso.2019.03.022.
- Yousaf, U., Christensen, M.-L. M., Engholm, G., & Storm, H. H. (2005). Suicides among Danish cancer patients 1971–1999. British Journal of Cancer, 92(6), 995–1000. doi:10.1038/sj.bjc.6602424.
- Zaorsky, N. G., Churilla, T. M., Egleston, B. L., Fisher, S. G., Ridge, J. A., Horwitz, E. M., & Meyer, J. E. (2017). Causes of death among cancer patients. Annals of Oncology: Official Journal of the European Society for Medical Oncology, 28(2), 400–407. doi:10.1093/annonc/mdw604.
- Zaorsky, N. G., Zhang, Y., Tuanquin, L., Bluethmann, S. M., Park, H. S., & Chinchilli, V. M. (2019). Suicide among cancer patients. Nature Communications, 10(1), 207. doi:10.1038/s41467-018-08170-1.
- Zhang, X., Sun, S., Peng, P., Ma, F., & Tang, F. (2021). Prediction of risk of suicide death among lung cancer patients after the cancer diagnosis. Journal of Affective Disorders, 292, 448–453. doi:doi:10.1016/j.jad.2021.05.123