Abstract
Personalized medicine has become a central focus of health and innovation policies in many countries. It is a complex policy field which, in the pursuit of both health and wealth, brings together technology, new data use, and medical care. The aim of this paper is to analyze how the notion of personalized medicine has evolved, and what publics are implied in the political mobilization of the concept. We answer these questions based on a document analysis of Danish strategy papers in the period 2014–2021 and expert interviews. We identify different strategy actors driving the process, shifts in topics during the strategy process, as well as different imaginaries of the public. We argue that each group of strategy actors act with a particular public in mind and that these influence how personalized medicine is envisioned. If the relationship between strategy development and the imagined publics remains unknown, it can pose a democratic problem.
Introduction
Across the world, personalized medicine has become a central policy focus during the last two decades (Reardon Citation2017; Tupasela Citation2021). With the aim of targeting diagnostics, prevention and treatment to individuals, personalized medicine strategies and policies concern, for example, the governance of genomics, biobanks, drug development and data security. Personalized medicine involves many actors from both private and public sectors and it relates to citizens in many ways – as patients, data sources, and taxpayers. In addition, it cuts across several policy arenas such as health, research, innovation and economic policy (Heta Tarkkala, Helén, and Snell Citation2019). What counts as personalized medicine is still debated and reframed both in the academic literature (Erikainen and Chan Citation2019; Prainsack Citation2017; Tutton Citation2012) and in the policy field (Australian Health Ministers’ Advisory Council Citation2017; General Secretariat of the Council Citation2015; Health Citation2016; Keogh Citation2015). Even the term personalized medicine has been debated, and there are other overlapping concepts such as stratified, precision and P4 medicine that are often used interchangeably although they have slightly different emphasis (Erikainen and Chan Citation2019). Our study is located in Denmark, and thus we use the most common term in this country, which is personalized medicine.
In the following, we set out to understand how the complex notion of personalized medicine has evolved over time in the Danish strategy process. In our investigation of policy documents, strategy papers and the policy processes of implementing personalized medicine in Denmark, we observed that some topics are very central at specific points in time and in specific documents and at other times they are ignored, forgotten, deemed irrelevant or perceived as subordinated (Jensen and Svendsen Citation2021). This spurred an interest in how to understand these fluctuations. All policy documents included in our study articulate the population as both a resource for personalized medicine and recipients of its products and services. In light of citizens central and dual role, we were intrigued by the way the actors behind the documents imagined and perceived these citizens. Therefore, the aim of this paper is to analyze how the notion of personalized medicine evolves over time through changes in topics and arguments, how the different policy actors imagine the citizens and the association between these two phenomena.
To analyze this, we found inspiration in the concept of imagined public introduced by scholars in environmental research, who use the concept to understand the different dynamics in a policy process (Barnett et al. Citation2010; Rodhouse et al. Citation2021; Walker et al. Citation2010). We show that different imagined publics influence which groups of citizens the policies address, and also which groups they do not address and who thereby are more or less excluded from taking part in the realization of personalized medicine. By making the imagined publics explicit, we are able to understand the evolution of the notion of personalized medicine, and to understand how the actions of the imagined publics may have consequences for the version of personalized medicine implemented in an actual healthcare system. We argue that if imagined publics remain unacknowledged, we fail to realize the main driver of the development of strategies and policies.
Imagined publics
In social science, life science policies – including policies on genetics, personalized medicine and health data governance – have often been investigated with discursive approaches (Erikainen and Chan Citation2019; Jones and Salter Citation2003; Martin and Turkmendag Citation2021; Webster Citation2005). This has also been the case in a Danish context where (Burau et al. Citation2021; Deleuran Terkildsen et al. Citation2020) studies show that discourses shape the direction of innovation and that competing discourses about technological futures and narratives sometimes overlap, sometimes in powerful discord with each other (Burau et al. Citation2021; Deleuran Terkildsen et al. Citation2020). The development of personalized medicine is, for example, described as “ … a process characterized by diverse sub-discourses which in combination make up a special version of personalized medicine” (Deleuran Terkildsen et al. Citation2020). In highlighting the performative aspect of expectations, the theoretical work within sociology of expectations e.g. (Brown and Michael Citation2003; Hoeyer Citation2019) and the theory of sociotechnical imaginaries e.g. (Jasanoff and Kim Citation2015; Jensen and Svendsen Citation2021; Heta Tarkkala, Helén, and Snell Citation2019) have uncovered how political visions not only articulate a possible future, but in themselves drive the technology development and pave its way into societal institutions. While these studies bring to the fore the coproduction of technology and political vision, they do not to any great extent pay attention to the particular notions of individual citizens or groups of citizens in political visions and policy processes.
Other scholars have investigated the imaginaries of publics in scientific practices and public engagement. Based on a UK study of imagined publics from the Second World War and onwards, Ian Welsh and Brian Wynne describe a development from a passive compliant imagined public to an imagined public who resists what is best for them due to their limited scientific understanding, ending with a public imagined to be a threat to science, as it does not comprehend the need for scientific supported commercial innovation in the global competition (Welsh and Wynne Citation2013). In a later study, Rommeteveit and Wynne point out that imagined publics are closely linked to political and economic agendas (Rommetveit and Wynne Citation2017). In the following, we take inspiration from this literature in combination with studies of biobanking and biomedicine, showing that certain imaginations of publics are utilized to recruit biobank participants, and to brand national research, infrastructures and the population itself (Busby and Martin Citation2006; Tarkkala and Tupasela Citation2018; Tupasela Citation2021; Citation2022). For example, Gottweis et al. point out that a public only exists when someone or a group of citizens are interested in something. Thus, biobanks start to imagine a public when they experience an interest from citizens in their work (Gottweis Citation2002).
In environmental research, the concept of “imagined publics” is used to describe, conceptualize and theorize the involvement of the public in atrategy processes and controversies. A common reference point for the concept of imagined publics is a paper by Maranta et al., where the authors outline the concept of the “Imagined Lay Person” (ILP), which is introduced to shed light on the implicit assumptions of the public described in literature within Public Understanding of Science (PUS) research (Maranta, Michael, and Pohl Citation2003). Maranta and colleagues make the point that ILPs act as functional constructions for experts in their knowledge production and that they are not a sociologically comprehensive representation of lay persons, but a way of ascribing epistemic and functional competences to lay persons. ILPs are often ascribed a limited number of competences, even though the collectives they represent feature all kinds of competences (Maranta, Michael, and Pohl Citation2003). Since Maranta and colleagues’ first article on the topic, ILP has evolved into the concept of imagined publics. Rodhous et al. define imagined publics as: “ … subjective social representations that build upon all sorts of assumptions and beliefs about the identities, abilities, knowledge, behaviors, and responsibilities of a particular group of people” (Rodhouse et al. Citation2021, 2). Imagined publics appear as fairly static knowledge schemes, which can be drawn upon whenever a representation for “the public” is needed. In this way, imagined publics are used to predict and counter the public reactions and positions on proposed politics and projects (Rodhouse et al. Citation2021). It is through the identification of different populations that regulatory interventions can be initiated (Ruppert Citation2011). Previous research has suggested that the imagined public is more significant for the development of a technology than the public it is supposed to represent (Rodhouse et al. Citation2021; Walker et al. Citation2010). Consequently, the imagined public becomes an actor with agency and political significance (Walker et al. Citation2010). In strategy processes, the public is always present in an abstract form, and influential on the development of a policy (Gisle Citation2018). Moreover, different imagined publics can co-exist, apparently representing the same group of people (Rodhouse et al. Citation2021).
In the present article, we apply the concept of imagined publics to the policy fields of personalized medicine. Where research in the environmental field has previously used the concept to analyze the involvement processes of the public in governance work and policy processes, we use it to contextualize the changes in argumentation and topics discussed in the different phases of the strategy process. “Imagined publics” as a concept helps us understand the changes in topics and argumentation and paves the way for uncovering how different strategy actors draw on different imagined publics, and as a consequence envision different versions of personalized medicine. Thereby the concept helps to understand how perceptions of publics are influential on policy and strategy outcome. In the Danish strategy papers, the imagined public is both understood as a passive research subject, a patient with the goal of receiving treatment, and an active citizen with the capacity to push back.
The Danish context
To set the scene for our analysis of the policy process, we will briefly introduce the Danish context. Denmark is a high-income country, with around 5.7 million inhabitants. Danish society is based on an all-embracing welfare state model, which co-exists with a free market economy. This means that the Danish healthcare system is primarily publicly funded through the redistribution of wealth through taxation, and is part of a welfare state offering all kinds of welfare services throughout the life of a Danish citizen. Denmark has five regions whose primary responsibility is to run hospitals and other healthcare services. The regions are governed by a democratically elected regional council, and they negotiate an annual budget with the national government. An umbrella organization called “Danish Regions” represents the five regions in political processes.
Like in other Nordic countries, there is a close relationship between the generation and collection of data and the development of welfare policies in Denmark. Every interaction with public institutions, including many private institutions, create data about the individual which become connected to the individual by a personal identification number. This means that in the welfare state, citizens’ interaction with state institutions produces massive amounts of data (Tupasela Citation2021), an outcome which has been framed as a natural part of state-citizen relationships: citizens fund healthcare services by paying taxes in exchange for access to these services. The data generated in this relationship comprise a collective good to be used for quality development of welfare services and for research (Bauer Citation2014; Hoeyer, Bauer, and Pickersgill Citation2019).
The development of personalized medicine in Denmark takes place in dialogue with similar developments in the Nordic Countries and the European Union. Crucial initiatives on the European scene are the visions of a European Health Data Space (https://www.european-health-data-space.com/) and the 1000,000 Genomes Project in the UK (https://www.genomicsengland.co.uk/initiatives/100000-genomes-project), which Danish stakeholders often highlight as an inspirational model for how to make genomics part of routine healthcare and enhance personalized medicine. Also, as a member of the International Consortium for Personalised Medicine (ICPerMed), Denmark supports research and implantation activities in Europe and internationally, with the aim of supporting and aligning research, funding and implementation of personalized medicine (https://www.icpermed.eu/index.php).
In tandem with these international initiatives, the Danish parliament decided, in 2018, to establish the National Genome Center as a key institution in a national infrastructure for the collection and storage of all information from genetic testing in the Danish healthcare system, thereby creating a huge database of genetic information. The proposal generated an intense public debate about privacy issues and the state’s intentions of collecting and storing all these data (Skovgaard and Hoeyer Citation2022). In the debate, the generation and collection of population health data appeared as a somewhat new – and worrying – endeavor in the welfare state (Svendsen and Navne Citation2022), despite data generation having always taken place since the establishment of welfare state institutions in the first half of the twentyish century. The debate gave voice to worried citizens questioning well-established data collection procedures, as these were coming to be seen as serving new purposes in a digitalized and data-intensive society.
Data collection and analysis process
To investigate the evolvement of Danish policy process in connection to personalized medicine, we have employed a qualitative study containing a document analysis and semi-structured interviews with policy actors. For the document analysis, we studied the relevant Danish policy documents and strategy papers from the first descriptions of a national initiative on personalized medicine (2014) to the latest updated national strategy on personalized medicine (2021). We have included all strategy documents specifically focusing on personalized medicine. Given our specific interest in the concept of personalized medicine, we have excluded health data and life sciences strategy documents which do not explicitly focus on personalized medicine. All the documents included in our study are available on public platforms. Interview participants were helpful in identifying relevant documents. For an overview of included documents see .
Table 1. The included strategy documents.
The document analysis was accomplished by applying a Thematic Analysis approach, where we read through and coded each document according to the topics and arguments put forward (Braun and Clarke Citation2006; Citation2019). We did this in an explorative way without in advance restricting ourselves to specific themes. The coded themes were then worked through by the first and last author to clarify the meanings of the themes, and some themes were collapsed because of overlapping content. The analysis process is inspired by what Coffey and Atkinson have named “the coding and retrieving strategy”. Using this strategy has three objectives: (1) to identify relevant phenomena, (2) to gather examples of the phenomena and (3) to analyse these phenomena so as to identify similarities, differences, patterns and structures (Coffey and Atkinson Citation1996, 29). Nvivo software was used to structure and arrange the coding process. The process resulted in 15 topics/arguments, which can be examined in .
Table 2. Overview of strategy topics according to time and actors.
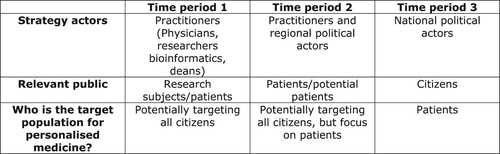
We divided the strategy process into three time periods, each period defined by the strategy actors driving the strategy process. This division is of course not clear-cut as all actors are involved in all periods, but the three time periods indicate a shift in which actors were the main drivers. Three groups of strategy actors were identified: (1) “Practitioners”, covering biomedical researchers and working physicians, bioinformatics researchers, and Deans from the health faculties; (2) Regional political actors, including Danish Regions, regional politicians and heads of corporate management in the five regions; and (3) National political actors, including national politicians and government officers from several departments.
The interview material in the present study is composed of 26 interviews with 28 interviewees. Interviewees represent research physicians at university hospitals (6), other researchers (4), Deans of health faculties from Danish universities (3), head of corporate management in the five regions (5), chairpersons from the five regional councils (5), employees from the Ministry of Health (2) and employees in Danish Regions (2). The interviews were conducted as part of an investigation of the implementation of personalized medicine in Denmark on a political administrative level. In the present article, interviews are used with a more specific purpose, namely, identifying statements about the public. The interviews were conducted in retrospect, meaning that in our conversations with strategy actors, they looked back on the strategy and policy process and reflected on the present initiatives. The persons interviewed had all been part of the strategy process even though some were more central than others. First, the first author coded the documents and interviews, looking for descriptions of “publics”. Second, the first and last author went through these codes to identify themes describing the different imagined publics. The imagined publics thus identified are described in the sections below.
To sum up, the document analysis revealed different topics and arguments emerging and disappearing through the three time periods. We then re-analyzed this material to uncover the representation of publics in relation to the identified topics and arguments. The interview material helped us understand the political context of the documents and see connections between specific groups of strategy actors and the publics they imagined.
Ethical approval
According to Danish legislation, research using questionnaires and interviews that do not involve human biological material (§14(2) of the Committee Act) interview studies are exempt from approval from the Committee on Health Research Ethics (https://en.nvk.dk/how-to-notify/what-to-notify). Informed oral consent was obtained and recorded prior to all interviews.
Imagined publics underlying official strategies on personalized medicine
In the following, we present our empirical analysis structured according to the three time periods. We describe the main discussion topics and arguments in each time period together with the identified imagined publics.
Time period 1: launching the idea of personalized medicine (2014–2015)
The key strategy actors in this first time period were researchers at universities and university hospitals, and the deans from health faculties at five Danish universities. For these actors, the main focus is to raise political awareness about personalized medicine as a research area which is to be developed in close connection to the public healthcare system and to attract funding for this endeavor. The end goal is to establish a research programme in personalized medicine for the benefit of future patients.
In 2014, researchers and deans at universities and researchers at university hospitals begin to draw up documents about introducing personalized medicine in Denmark. The faculties of health sciences at Danish universities have an ongoing dialogue with heads of corporate management in the regions to coordinate research and development at the hospitals and the universities.
As shows, deans and researchers emphasize the needs and importance of research when drawing the lines for a national initiative on personalized medicine. For them, it is important that the strategy enables well-functioning structures for conducting research in the field of personalized medicine. A strategy paper on a common initiative for personalized medicine from this time period states:
A project like this will support many Danish research areas, which connect knowledge about the genome to Danish population registers and clinical parameters. These activities will create extensive exposure for Danish research and contribute to securing Denmark's position in the knowledge society within a sector which is critical for [the] Danish economy (Personalized medicine and individualized treatment – proposal for a unified Danish effort 2015).
The infrastructure should enable 100,000 Danes to be offered the opportunity to be part of a national genome biobank in preparation for establishing a unique foundation for research in future prevention and treatment options (Personalized medicine and individualized treatment – proposal for a unified Danish effort 2015).
This development will have unprecedented commercial potential consisting of new medical products, which in the future will be priced according to their effectiveness in treatment. Knowledge from the massive amount of data generated across the population will lead to new types of companies at the interface of health science and IT (A national Danish initiative on precision medicine and individualized medicine – A 2014).
When you consider the amount of information we report to the Danish Customs and Tax Administration about marital status, our salary, et cetera, it's a lot of information we report to public institutions without being nervous about it. I'm in no way nervous about this (the collection of genetic data) or misuse of data (Researcher and physician 1).
If you look at patients’ and citizens’ motives to hand over data, they are very different. As a patient you say: Take samples. Do whatever you want with them. Find out what to do for me and the ones who have the same condition as me. As a citizen you think: What do you want with it (health data/genetic information)? What are you going to use it for? (Dean 2)
I understand that one could be worried, but I think information is important, to try to inform the public as much as possible, what all this is, and how are they going to be treated. I think that the National Genome Center is doing a very good job, putting all sorts of information on their website. And we’re trying to do the same. (Researcher 3)
Topics not mentioned in the documents from this time period are the issues of data security or privacy, the need to control and implement personalized medicine in the public healthcare system, and issues about public trust in public institutions as a critical parameter for the success of personalized medicine. The “missing” topics indicate that the researchers are not concerned about the issue of trust. A fair number of the researchers do not make explicit references to a public. This absence tells us that they take as self-evident the various publics’ willingness to participate. Although they know individual persons/patients who may be skeptical, they do not expect skepticism from the majority. They see citizens and patients as trusting researchers and health professionals and as being positive towards new treatment options.
Time period 2: enabling future treatment (2015–2018)
In the second time period, the key strategy actors were practitioners active in research from the university hospitals, politicians from the regional councils, heads of corporate management in the five regions, and members of staff from Danish Regions. In policy documents, these actors continue to focus on attracting funding to personalized medicine and generating interest in the field by involving national politicians. Personalized medicine is presented not so much as a research area, but as a new treatment paradigm. Personalized medicine as a new treatment paradigm is taken to be “the future”, and the task at hand is to convince the national politicians of this. Again, citizens are expected to – simultaneously – enable the realization of personalized medicine and benefit from it.
In the documents in this time period, we have observed a shift in focus which makes it different from the previous time period. Emphasis shifts from prevention and treatment to an almost exclusive focus on treatment. Accordingly, research and the mapping of a national reference genome play a less central role than in the previous time period. For the first time, documents mention the ethical dilemmas concerning the collection, storage and use of patient and citizen data.
Hence, it is important to safeguard the security, health, integrity and right to self-determination of both research subjects and patients, at the same time safeguarding the development of the healthcare system for the benefit of patients, including the development of personalized medicine (Reporting from the reference group on personalized medicine – an initial analysis 2016).
The development of personalized medicine is dependent on informing Danish patients and citizens about treatment and research. Transparency and dialogue with citizens are critical. Patients and citizens should be involved, and information, communication and involvement are critical activities (Personalized medicine for the benefit of patients 2016)
Even though the documents convey a strong focus on public institutions, including citizens’ trust in the collection, storage, and use of data in public institutions, they also acknowledge the benefits of public-private partnerships. For example, the national strategy on personalized medicine from 2017–2020 (Personalized medicine for the benefit of the patients 2016) says: “We see promising possibilities within public-private collaboration on new treatment options – and especially new medical products – for the benefit of the patients”.
The documents convey that regional politicians and heads of corporate management understand the imagined public as first and foremost a patient. The patient is imagined as finding it difficult to understand the consequences, pitfalls, and benefits; and in general, the information connected to the sequencing of the genome. Therefore, the imagined (patient) public are in need of guidance and assistance to navigate the difficult space of personalized medicine. This way of imagining the public places a great deal of responsibility on the strategy actors. They see it as their responsibility to guide patients in this paradigmatic change within healthcare services.
It can be difficult for a citizen to cope with the consequences of going through a genetic sequencing, and therefore I believe that as a public healthcare system we have a responsibility for giving thorough information to the patients before they go through a genetic sequencing (Head of Corporate Management in Region 5)
I'm not afraid of it (the use of genetic information). In fact, I'm convinced that the Danes really want to participate in it, because it will raise the quality of our healthcare system and we can all be treated for far more diseases with better quality in the future (Director of region 2)
Time period 3: citizen support is critical (2018–2021)
In the last period, the policy documents center on encouraging citizens to accept the idea of personalized medicine and support the National Genome Center as the infrastructure for the collection, storage, and use of data. The imagined public of the policy documents has changed from research subject (time period 1) and patient (time period 2) to citizen. This citizen is active, has the potential for active resistance, and takes an interest in debates about the use of private data, for example in connection with “big tech” companies and their use and misuse of health data. Thus, strategy actors are also concerned about debates on data misuse and its consequences for the implementation of personalized medicine.
The documents included from this time period have a strong focus on the ethical dilemmas related to collection, storage, and use of patient data. Therefore, they are also very much concerned about data security and data privacy, and keen to place the infrastructure of personalized medicine in public healthcare institutions. Citizens’ trust in public institutions is mentioned as strong, yet also as something which cannot be taken for granted. Thus, efforts are needed to retain public trust in order to make personalized medicine a success.
It is crucial for the trust in the Danish development of personalized medicine that the initiative rests on a widespread information effort as well as a solid ethical, legal and data security foundation. More knowledge must be created on an ongoing basis about ethical, legal and societal aspects connected to the commissioning of genome sequencing and personalized medicine in the healthcare system (Personalized medicine for the benefit of the patients 2020).
“How do we keep and ensure the trust of citizens and patients? It is important that we are transparent and inform citizens and patients sufficiently, when we introduce these new genomic technologies. It's to help the patients that we do this. It's to help the patients, which is also the focus in the strategy. It's not to go out there and map all Danes’ genomes with all kinds of different purposes.” (employee from the Danish Ministry of Health, 2019).
Similarly, to the previous time period, national strategy actors focus almost exclusively on personalized medicine in relation to treatment. Neither prevention nor research and the mapping of a national reference genome are giving much attention in the documents. Other topics not touched upon in the included documents are the possibility for public-private partnerships, the role of private actors in the field, the benefits and necessity of international collaboration, and the growth potential for private companies within the field of personalized medicine and genomics. The documents portray personalized medicine as an activity performed solely by public actors and located in public institutions.
Discussion
By analyzing Danish strategy papers and other central policy documents on personalized medicine. we have identified three time periods in the strategy- and policymaking process. In these three time periods, we have observed a pattern of different topics and arguments emerging and disappearing from the documents. Based on the documents included and the interviews of actors involved in the strategic work of personalized medicine, we have identified various different imagined publics, which together with various different aims of policy actors are shaping the observed pattern of topics. We have summarized these findings in .
Our analysis shows that each group of strategy actors reflects and addresses a particular imagined public and that these publics influence the notion of personalized medicine and thereby potentially also the version of personalized medicine implemented in the Danish healthcare system. In the first time period studied, the imagined public is a research subject or a patient with the main goal of being treated or facilitating future treatment. The person trusts the researcher or the physician. Personalized medicine is envisioned in multiple forms and as influencing the whole healthcare system from research to prevention to diagnostics and treatment. The focus is on creating the optimal conditions for research and development with a wish to investigate all imagined possibilities within personalized medicine, including all citizens in the creation of a national reference genome, prevention and treatment.
In the second time period studied, the imagined public is a patient undergoing treatment. The public consists of patients who trust the public institutions of the welfare state and also need guidance from public actors in order to navigate the complex field of personalized medicine. At the same time, citizens are also depicted as central actors in the realization of personalized medicine, and thus it becomes critical to signal how public institutions will handle ethical issues. One solution to the handling of ethical issues is to place all activities in public institutions, focusing less on research, and emphasizing public control over all collaborations.
In the third time period studied, the imagined public is a citizen. This citizen trusts public institutions, but may also come to question the trustworthiness of these institutions. The strategy actors see this mistrust as being influenced, among other things, by the behavior of large tech companies. To respond to this, public institutions must convince citizens as to the public institutions’ good intentions and capability of caring responsibly for the collection, storage, and use of genetic data. This orientation towards data security fosters an even more intense focus on ethical issues, especially the citizen’s privacy and the healthcare system’s secondary use of data. To soothe the citizens, policy documents and strategy actors emphasize the importance of establishing a strong relationship between research and patient treatment, and establishing an almost exclusive focus on patient treatment.
Imagined publics can either be explicitly constructed or implicitly implied in policy documents and statements from political actors. Either way, our analysis has shown that an imagined public can frame strategy development and consequently the implementation of personalized medicine. If the background for these changes in strategy focus remain unexamined or unacknowledged, this can pose a democratic problem in that not knowing the rationale behind the argumentation and framing of a problem makes it difficult to engage in a meaningful exchange of views. As we see it, strategies and policies are shaped to respond to the imagined public of specific strategy actor groups. Different strategy actors have varying aims and therefor also envisage different imagined publics. National political strategy actors often associate a concept like personalized medicine with international political currents like e.g. the notion of bioeconomy or the value of health data, while research strategy actors are more focused on clinical benefit and – effects. It is not so much that specific imagined publics are adjusted to serving specific aims, but more that specific aims turn attention towards specific publics.
Investigating the included documents, we identified that the perception of the imagined publics evolved throughout the strategy period. But analyzing the interview material, it became clear to us that the competing perceptions of the public – as research subject, patient, and citizen – continue to coexist between the different actor groups. The shift in the dominant imagined public in the three time periods is an expression of different actors having the power to establish the most relevant imagined public, at a particular time, in the strategy process. As Rodhouse points out, different imagined publics can be developed at the same time and thus co-exist, apparently representing the same group of people (Rodhouse et al. Citation2021). What we see in the Danish case is that various different policy actors drive the strategy process, each with a particular perception of the public and a particular aim of personalized medicine. The “imagined public” as concept helps to make visible different framings of complex problems and helps to uncover the argumentative work of policy documents addressing important societal issues. By using this concept, we show a diversified perception of the public: as source for the realization of personalized medicine, as beneficiaries of personalized medicine, as trusting citizens, as worried citizens, and as taxpayers.
The perception of a public in policy papers is not static. As we have shown, the imagined public has an impact on the strategy development and thereby potentially also on the version of personalized medicine implemented, but the imagined public is also formed in response to societal dynamics. As described earlier, the establishment of the National Genome Center induced an intense public debate about the intentions behind collecting, storing, and using genetic data. These discussions made “the citizen” a relevant and active actor in the strategy and policy process. The discussions introduced a new agenda in the argumentation process and the framing of problems. In particular, the national strategy actors were forced to incorporate this need for a new agenda in their argumentation for the implementation and development of personalized medicine, because they were the ones driving the strategy process in the last of the three time periods, and they are also the ones hosting the National Genome Center, as a national agency under the Danish Ministry of Health. From the policy documents and the interviews, we sense that what is at stake here is not only the future of personalized medicine, but the citizens’ trust in public institutions and in their handling of private information in general. The personal identification number in a welfare state and all the national registers connect citizen and state, individually and collectively, in a specific way: the personal identification number produces, on an ongoing basis, a growing archive of information about the interaction between citizen and state (Bauer Citation2014). Most Danish citizens find it unproblematic that this archived information is used for secondary use (Hoeyer, Bauer, and Pickersgill Citation2019), probably because people in the Nordic countries tend to perceive the welfare states as participatory and friendly (Bauer Citation2014). The downside of these information collection practices of the welfare states is the ease with which these practices can be turned into regimes of surveillance (Bauer Citation2014) or profit-making. Our case shows that work is needed in the welfare state in order to prove the friendly intentions of data collection, and the ways data collection will work for the common good.
Ethical and regulatory issues have been a central part of the political debate about genetics and personalized medicine, reflecting the historically close relationship between genetics and eugenics. Despite efforts to dispel this impression, for example in the Human Genome Project, by focusing on medical treatment, the fear connected to genetic research seems to lurk under the surface at any time (Reardon Citation2017). As we see in this analysis, the fear of data misuse seems to test the relationship between citizen and state. The solution of the Danish strategy actors in response to the concerns of their imagined publics, is strong public leadership and data control – a solution that would perhaps not be well received in other countries (Reardon Citation2017).
When looking at the pattern of disappearing and emerging topics and arguments during the three time periods, it seems as if the conditions for developing, implementing, and participating in personalized medicine are downplayed throughout the different strategy documents. Our analysis points out that the more critical the public is imagined to be, the more topics on the importance of public-private partnerships, international collaboration, data security, and investments in research disappear from the documents. We noticed that on the one hand national strategy actors emphasize the importance of transparency, and on the other hand parry concerns by downplaying the role of private actors and emphasizing public control and public institutions. This shows that the imagined public holds the power to shape and direct strategy and policy development and thereby also the power to shape the development of our society. Drawing the attention of the key actors’ different perceptions of the public, is crucial to uncover the positions we, as citizens, are offered in the public development of society.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Am, H., G. Solbu, and K. H. Sorensen. 2021. “The Imagined Scientist of Science Governance.” Social Studies of Science 51 (2): 277–297. https://doi.org/10.1177/0306312720962573.
- Australian Health Ministers’ Advisory Council. 2017. National Health Genomics Policy Framework 2018-2021 (https://www1.health.gov.au/internet/main/publishing.nsf/Content/FD973B58DE82BCFFCA2581CC007D4682/$File/National-Health-Genomics-Policy-Framework.pdf.
- Barnett, J., K. Burningham, G. Walker, and N. Cass. 2010. “Imagined Publics and Engagement Around Renewable Energy Technologies in the UK.” Public Understanding of Science 21 (1): 36–50. https://doi.org/10.1177/0963662510365663.
- Bauer, S. 2014. “From Administrative Infrastructure to Biomedical Resource: Danish Population Registries, the “Scandinavian Laboratory,” and the “Epidemiologist's Dream”.” Science in Context 27 (2): 187–213. https://doi.org/10.1017/S0269889714000040.
- Braun, V., and V. Clarke. 2006. “Using Thematic Analysis in Psychology.” Qualitative Research in Psychology 3 (2): 77–101. https://doi.org/10.1191/1478088706qp063oa.
- Braun, V., and V. Clarke. 2019. “Reflecting on Reflexive Thematic Analysis.” Qualitative Research in Sport, Exercise and Health 11 (4): 589–597. https://doi.org/10.1080/2159676X.2019.1628806.
- Brown, N., and M. Michael. 2003. “A Sociology of Expectations: Retrospecting Prospects and Prospecting Retrospects.” Technology Analysis & Strategic Management 15 (1): 3–18. https://doi.org/10.1080/0953732032000046024.
- Burau, V., N. Nissen, M. D. Terkildsen, and U. Vaeggemose. 2021. “Personalised Medicine and the State: A Political Discourse Analysis.” Health Policy 125 (1): 122–129. https://doi.org/10.1016/j.healthpol.2020.10.005.
- Busby, H., and P. Martin. 2006. “Biobanks, National Identity and Imagined Communities: The Case of UK Biobank.” Science as Culture 15 (3): 237–251. https://doi.org/10.1080/09505430600890693.
- Coffey, A., and P. Atkinson. 1996. Making Sense of Qualitative Data: Complementary Research Strategies. Sage.
- Deleuran Terkildsen, M., V. Burau, U. Væggemose, and N. Konstantin Nissen. 2020. “The Welfare State Driving “Me” and “We” Medicine – A Critical Discourse Analysis.” New Genetics and Society, https://doi.org/10.1080/14636778.2020.1755635.
- Erikainen, S., and S. Chan. 2019. “Contested Futures: Envisioning “Personalized,” “Stratified,” and “Precision” Medicine.” New Genetics and Society 38 (3): 308–330. https://doi.org/10.1080/14636778.2019.1637720.
- General Secretariat of the Council. 2015. Council conclusions on Personalised medicine for patients. http://data.consilium.europa.eu/doc/document/ST-15054-2015-INIT/en/pdf.
- Gisle, S. 2018. “The Physiology of Imagined Publics: From a Deficit to an Ambivalence Model.” Science & Technology Studies 31 (2).
- Gottweis, H. 2002. “The Governance of Genomics.” Critical Public Health 12 (3): 207–220. https://doi.org/10.1080/09581590210153344.
- Health, A.-T. F. N. A. f. L. S. a. 2016. GENOMIC MEDICINE FRANCE 2025 (https://solidarites-sante.gouv.fr/IMG/pdf/genomic_medicine_france_2025.pdf.
- Hoeyer, K. L. 2019. “Data as Promise – Reconfiguring Danish Public Health Through Personalized Medicine.” Social Studies of Science 49 (4): 531–555.
- Hoeyer, K., S. Bauer, and M. Pickersgill. 2019. “Datafication and Accountability in Public Health: Introduction to a Special Issue.” Social Studies of Science 49 (4): 459–475. https://doi.org/10.1177/0306312719860202.
- Jasanoff, S., & Kim, S.-H. (2015). Dreamscapes of Modernity: Sociotechnical Imaginaries and the Fabrication of Power. https://doi.org/10.7208/chicago/9780226276663.001.0001
- Jensen, L. G., and M. N. Svendsen. 2021. “Personalised Medicine in the Danish Welfare State: Political Visions for the Public Good.” Critical Public Health, 1–12. https://doi.org/10.1080/09581596.2021.1937524.
- Jones, M., and B. Salter. 2003. “The Governance of Human Genetics: Policy Discourse and Constructions of Public Trust.” New Genetics and Society 22 (1): 21–41. https://doi.org/10.1080/1463677032000069691.
- Keogh, B. 2015. Personalised Medicine Strategy. NHS England Board. (https://www.england.nhs.uk/wp-content/uploads/2015/09/item5-board-29-09-15.pdf.
- Maranta, A. G., Gisler Michael, and Christian Pohl. 2003. “The Reality of Experts and the Imagined Lay Person.” Acta Sociologica 46 (2).
- Martin, P. A., and I. Turkmendag. 2021. “Thinking the Unthinkable: How Did Human Germline Genome Editing Become Ethically Acceptable?” New Genetics and Society 40 (4): 384–405. https://doi.org/10.1080/14699915.2021.1932451.
- Prainsack, B. 2017. Personalized Medicine: Empowered Patients in the 21st Century. New York University Press.
- Reardon, J. 2017. The Postgenomic Condition: Ethics, Justice, and Knowledge after the Genome. University of Chicago Press. https://doi.org/10.7208/9780226345192
- Rodhouse, T. S. G. H., U. Pesch, E. H. W. J. Cuppen, and A. F. Correljé. 2021. “Public Agency and Responsibility in Energy Governance: A Q Study on Diverse Imagined Publics in the Dutch Heat Transition.” Energy Research & Social Science 77, https://doi.org/10.1016/j.erss.2021.102046.
- Rommetveit, K., and B. Wynne. 2017. “Technoscience, Imagined Publics and Public Imaginations.” Public Understanding of Science 26 (2): 133–147. https://doi.org/10.1177/0963662516663057.
- Ruppert, E. 2011. “Population Objects: Interpassive Subjects.” Sociology 45 (2): 218–233. https://doi.org/10.1177/0038038510394027.
- Skovgaard, L. L., and K. Hoeyer. 2022. “Data Authority: Public Debate About Personalized Medicine in Denmark.” Public Understanding of Science 31 (5): 590–607. https://doi.org/10.1177/09636625221080535.
- Svendsen, M. N., and L. E. Navne. 2022. “Citizen-Person: The “Me” in the “We” in Danish Precision Medicine.” Science, Technology, & Human Values, https://doi.org/10.1177/01622439221108535.
- Tarkkala, H., I. Helén, and K. Snell. 2019. “From Health to Wealth: The Future of Personalized Medicine in the Making.” Futures 109: 142–152. https://doi.org/10.1016/j.futures.2018.06.004.
- Tarkkala, H., and A. Tupasela. 2018. “Shortcut to Success? Negotiating Genetic Uniqueness in Global Biomedicine.” Social Studies of Science 48 (5): 740–761. https://doi.org/10.1177/0306312718801165.
- Tupasela, A. 2021. Population as Brands – Marketing National Resources for Global Data Markets. Cham: Palgrave Macmillan. https://doi.org/10.1007/978-3-030-78578-9
- Tupasela, A. 2022. “The Genetic Imagination: Imaging Populations and the Construction of Nationhood.” Finnishness, Whiteness and Coloniality, 19–40. https://doi.org/10.33134/hup-17-2.
- Tutton, R. 2012. “Personalizing Medicine: Futures Present and Past.” Social Science & Medicine 75 (10): 1721–1728. https://doi.org/10.1016/j.socscimed.2012.07.031.
- Walker, G., N. Cass, K. Burningham, and J. Barnett. 2010. “Renewable Energy and Sociotechnical Change: Imagined Subjectivities of ‘the Public’ and Their Implications.” Environment and Planning A: Economy and Space 42 (4): 931–947. https://doi.org/10.1068/a41400.
- Webster, A. 2005. “Social Science and a Post-Genomic Future: Alternative Readings of Genomic Agency.” New Genetics and Society 24 (2): 227–238. https://doi.org/10.1080/14636770500184834.
- Welsh, I., and B. Wynne. 2013. “Science, Scientism and Imaginaries of Publics in the UK: Passive Objects, Incipient Threats.” Science as Culture 22 (4): 540–566. https://doi.org/10.1080/14636778.2013.764072.