Abstract
Objective
To define the natural course and complications, and develop a model for predicting persistency when low-lying placenta (LLP) is detected early in pregnancy.
Methods
This retrospective cohort study included women with LLP detected during an early anatomic scan performed at 13–16 weeks gestation. Additional transvaginal ultrasound exams were assessed for resolution at 22–24 weeks and 36–39 weeks. Patients were categorized as: Group 1–LLP resolved by the second-trimester scan, Group 2–LLP resolved by the third trimester, or Group 3–LLP persisted to delivery. Clinical and laboratory parameters, as well as maternal and neonatal complications, were compared. A linear support vector machine classification was used to define a prediction model for persistent LLP.
Results
Among 236 pregnancies with LLP, 189 (80%) resolved by 22–24 weeks, 25 (10.5%) resolved by 36–39 weeks and 22 (9.5%) persisted until delivery. Second trimester hCG levels were higher the longer the LLP persisted (0.8 ± 0.7MoM vs. 1.13 + 0.4 MoM vs. 1.7 ± 1.5 MoM, adjusted p = .03, respectively) and cervical length (mm) was shorter (first trimester: 4.3 ± 0.7 vs. 4.1 ± 0.5 vs. 3.6 ± 1; adjusted p = .008; Second trimester: 4.4 ± 0.1 vs. 4.1 ± 1.2 vs. 3.8 ± 0.8; adjusted p = .02). The predictive accuracy of the linear support vector machine classification model, calculated based on these parameters, was 90.3%.
Conclusions
Persistent LLP has unique clinical characteristics and more complications compared to cases that resolved. Persistency can be predicted with 90.3% accuracy, as early as the beginning of the second trimester by using a linear support vector machine classification model.
Introduction
The location of the placenta is relative to the internal cervical os: previa, low-lying, or distant from the cervical canal, may be determined as early as the beginning of the second trimester, usually during the early anatomic scan. Low-lying placenta (LLP) is diagnosed when the inferior placental edge is within 2 cm of the internal cervical os but does not overlie it [Citation1–3]. Resolution of low placentation, when diagnosed in the mid-trimester, occurs in 66% to 98% of cases and is more likely if it is low-lying rather than placenta previa [Citation1,Citation2]. Management of pregnancies with LLP is based on data published regarding placenta previa. Information regarding the natural course, clinical and laboratory parameters, outcomes and complications of isolated LLP has not been published. LLP and placenta previa may be associated with antepartum hemorrhage and are indications for cesarean delivery if persistent into the third trimester. However, these complications are also based on extrapolation from studies that investigated placenta previa and LLP as a single group [Citation1–5]. Moreover, data regarding differences between LLP that resolved early, versus those that resolved later or persisted until delivery are lacking.
The primary aim of this study was to define the natural course and complications of pregnancies with LLP diagnosed at 13–16 weeks of gestation and to compare demographics, mode of delivery, obstetrical history, and maternal and neonatal outcomes and complications between cases in which LLP resolved during pregnancy and cases where it persisted until delivery. The secondary aim was to create a clinical model that would predict persistent LLP, based on clinical and laboratory parameters among pregnant women with very early diagnosis of LLP.
Material and methods
This retrospective cohort study included all patients with a diagnosis of LLP detected during early ultrasound anatomic scan, performed at 13–16 weeks of gestation, at a tertiary academic institution, from 2010 through 2019. In Israel, an ultrasound anatomic scan at 13–16 weeks of gestation is routinely performed during pregnancy.
Patients were excluded if the pregnancy was terminated or ended in delivery or fetal loss before 24 weeks of gestation. Multiple pregnancies, pregnancies with placenta previa, placenta accreta spectrum (PAS, when placental villi invade beyond the decidua basalis, leading to placenta accreta, increta, or percreta) [Citation6], whether a prenatal diagnosis of PAS or a diagnosis during cesarean section and pathology, or other placental anomalies such as abnormal cord insertion, accessory lobes, and patients with prior uterine surgeries including myomectomy or previous cesarean delivery were excluded, as well.
Placental location was evaluated using transvaginal ultrasound (TVS). After bladder emptying, a TVS probe (9 MHz GE Voluson E8, Milwaukee, WI) was inserted into the anterior vaginal fornix, with the patient in the dorsal lithotomy position. All measurements were performed by the same certified sonographer. The cervix was visualized in the sagittal plane. The distance between the placental edge and the internal os was measured. According to the American Institute of Ultrasound in Medicine (AIUM) criteria, LLP is defined when this distance is 0 to 20 mm [Citation7]. Measurements collected before the AIUM classification was published, were categorized retrospectively according to these criteria.
Resolution of LLP was defined as >20 mm in subsequent examinations. Follow-up TVS were performed to assess for resolution during the second-trimester scan at 21–24 weeks of gestation and before delivery at 36–39 weeks of gestation. Patients were divided into three groups. Group 1 included those with a resolution of LLP by the second-trimester scan. Group 2 included patients with persistent LLP in the second trimester that resolved in the third trimester, as diagnosed by ultrasound at 36–39 weeks, and Group 3 were women with persistent LLP at delivery.
Data regarding demographics, obstetrical history, clinical and laboratory parameters during pregnancy, mode of delivery and maternal and neonatal outcomes and complications, were abstracted from electronic medical records. Postpartum anemia was defined as Hb <10 mg/dl. We defined Fetal growth restriction (FGR)/small for Gestational age (SGA) as the estimated fetal weight (EFW) below the 10th centile [Citation8]. We did not have the Doppler measurements of these fetuses. Our clinical approach is to deliver women with <10 mm between the placental edge and the internal os by an elective cesarean section [Citation9].
Statistical analysis
Post-hoc power sample size analysis was calculated based on an α error of 0.05 and a power of 80%. An absolute difference of 25% in parameters between low-lying placentas that resolved or persisted (with an enrollment ratio of 1:5) would have a clinical impact on counseling a patient who has low-lying placenta at the end of the first trimester. A sample size of 26 in the study group and 130 in the control group was found to be sufficient for statistical significance.
Data were analyzed using SPSS-25 (IBM Corp., Armonk, NY, USA). Statistical significance between the two groups was calculated using the Chi-square test or Fisher’s exact test for differences in quantitative variables and t-test or Mann–Whitney for continuous variables, each when appropriate. adjusted p < .05 was set as the level of statistical difference because of the performance of multiple comparisons. In order to evaluate the clinical predictors for persistency, we performed a multivariate logistic regression analysis.
Using these data, classification models can be produced by different classifiers. To define a predictive model for persistent LLP in this study, we chose a Linear Support Vector Machine (LSVM) classification using the MATLAB Classification Learner software. The LSVM is a classical machine learning approach widely used in supervised learning to find a line with the largest margin that separates different classes of data points. Validation of the model was performed using 5-fold cross-validation which is preferable in this case of relatively small data sets.
Ethical approval
The study was approved by Meir Medical Center Institutional Ethics Committee, affiliated with Tel Aviv University. Informed consent was waived due to the retrospective nature of the study.
Results
A total of 246 pregnancies with low placentation were detected at 13 to 16 weeks of gestation during the study period. Five were excluded due to the diagnosis of placenta previa, 4 were excluded because of multiple gestations and in the case of placenta accreta. 236 cases of LLP were included in this study. On subsequent sonographic examinations, 189 (80%) had resolved by 21–24 weeks of gestation, 25 (10.5%) by 36–39 weeks, and 22 (9.5%) cases persisted until delivery 236.
Women with persistent LLP (Group 3) were older than women in Group 2 and were older than women in Group 1 (34.9 ± 4.5 vs. 31 ± 3.9 vs. 30 ± 4.9 years, respectively; adjusted p = .001; ). There were no significant differences in gravidity, parity or BMI among the groups. No woman reported cigarette smoking while pregnant. Only two women (group 1) were diagnosed with FGR/SGA [2 (1.05%) vs. 0 vs 0, adjusted p = .8]. Second-trimester hCG levels, taken as part of second-trimester prenatal genetic screening, were higher the longer the LLP persisted (0.8 ± 0.7 vs. 1.13 ± 0.4 vs. 1.7 ± 1.5 MoM, respectively; adjusted p = .03). Other second-trimester markers were within the normal range, without significant differences between groups. Gestation was shorter the longer the LLP persisted (39 ± 1.3 vs. 38.5 ± 1.5 vs. 37.7 ± 1.8 weeks, respectively; adjusted p = .001).
Table 1. Maternal characteristics.
Cervical lengths measured during both anomaly scans were shorter in Group 3 compared to Group 2 (4.1 ± 0.5 vs. 4.3 ± 0.7 mm respectively; adjusted p = .008), and in Group 2 compared with Group 1 (3.6 ± 1 vs. 4.1 ± 0.5 mm, adjusted p = .02). Intrapartum maternal bleeding was significantly higher in the persistent LLP group, who delivered vaginally, as compared to Groups 1 and 2 ().
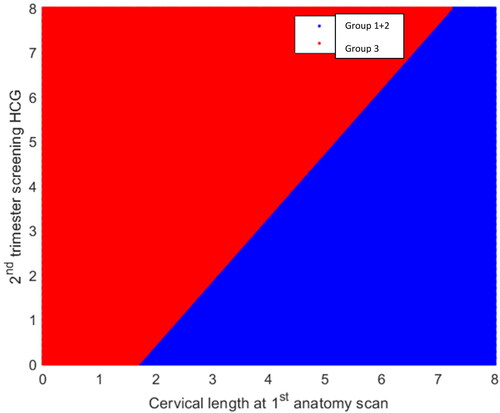
Logistic regression of these two parameters was statistically significant (). Odds ratio (OR) for cervical length in the first trimester was 0.14 (95% CI 0.052–0.38, adjusted p < .001) and hCG level OR 2.9 (95%CI 1.3–5.3, adjusted p < .001). Receiver operating characteristic curve for the interaction of these two parameters was statistically significant (area under the curve of 0.681, adjusted p = .006; ).
Figure 1. The receiver operating characteristic curve for the interaction of the parameters (cervical length in the first trimester and second trimester hCG level) was statistically significant (area under the curve of 0.681, p = .006).
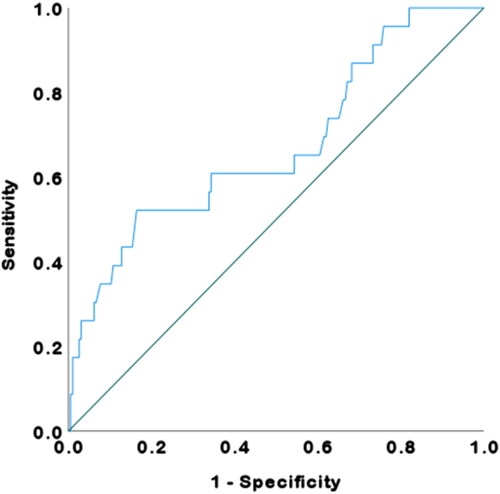
Table 2. Multivariate logistic regression analysis.
The rate of postpartum anemia, defined as Hb <10 mg/dl, was significantly higher in Group 3 than in Groups 1 and 2 (20% vs. 9.7% vs. 6.7%, respectively, adjusted p = .04). Neonatal complications are shown in . No significant differences were found between the groups regarding birth weight, Apgar scores or umbilical cord blood pH.
Table 3. Neonatal characteristics.
Women with <10 mm between the placental edge and the internal os (30% of Group 3) were delivered by elective cesarean section. The rate of cesarean section was 37.5% in the rest of Group 3 women with 10-20 mm between the placental edge and the internal os. The cesarean section rate was 16% in Group 2 and 36.3% in Group 3 (adjusted p = .001). The chance of having a cesarean section if LLP was diagnosed at 13–16 weeks of gestation was 9.3%. However, if it persisted to the second anatomic scan at 22–24 weeks, the chance of having a cesarean section was 46%. Evaluation of these results produced a model for predicting persistent LLP, detected at 13–16 weeks of gestation, based on cervical length at the first anatomic scan and second-trimester screening hCG level.
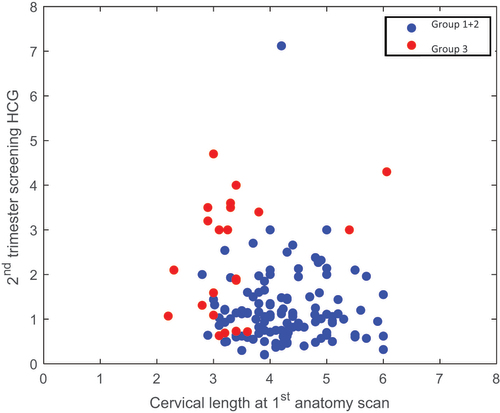
The data include 121 Group 1 + 2 points and 23 Group 3 points (patients), where each point is characterized by two features. Feature A is the cervical length at the first anatomical scan and feature b is the second trimester hCG level. This is depicted in , where the x and y axes correspond to features a and b, respectively. A clear difference is observed between Groups 1 + 2 and 3.
Figure 2. Visualization of the data: each point corresponds to a woman in Group 1 or 2 and is characterized by features a and b, where feature a is the cervical length at the first anatomical scan and feature b is the second trimester hCG level. Clear separation between Groups 1 + 2 and 3 is observed. A Linear Support Vector Machine (LSVM) classification using the MATLAB Classification Learner software was used. The LSVM is a classical machine learning approach widely used in supervised learning to find a line with the largest margin that separates different class data points. Since the available data sets were limited in size, validation of the model was performed using 5-fold cross-validation.
The prediction accuracy of this model, based on cervical length at the early anatomic scan and second trimester hCG level was found to be 90.3%. The classification surfaces of this model are visualized in .
Discussion
The current study describes the natural course, clinical data and maternal and neonatal complications of LLP diagnosed early in pregnancy, and suggests a new model for predicting persistent cases. To the best of our knowledge, this is the first report regarding a cohort that includes solely women with LLP and not a mixed population of LLP and placenta previa. The executive summary of the joint Fetal Imaging Workshop recommended ultrasound evaluation at 16 weeks of gestation to rule out placenta previa. In cases of LLP, a follow‐up ultrasound is recommended at 32 weeks of gestation [Citation9]. The routine practice of fetal anomaly surveys in Israel includes an early anatomic scan at 13–16 weeks of gestation and second-trimester anomaly scan at 21–24 weeks. This provides a window of opportunity to investigate the clinical behavior and natural course of different types of placentation over a range of gestational ages, as described in this study.
According to our results, we can define phases of resolution that divide pregnancies with LLP into three categories, with different clinical characteristics. The small group with persistent LLP had unique characteristics and complications compared to the other two groups. These included significantly older maternal age, earlier gestational age at delivery, higher second-trimester hCG levels, shorter cervical lengths measured during first and second-trimester anatomic scans and a higher rate of peripartum complications. The combination of these findings defines pregnancies with persistent LLP as high-risk, in contrast to cases of LLP that resolve during pregnancy.
Therefore, the challenge of managing LLP diagnosed early in pregnancy is early detection with a focus on cases that will persist until delivery. To meet this challenge, we present a novel predictive model for persistent LLP that uses two statistically significant clinical parameters: early second-trimester cervical length and second-trimester hCG. By utilizing this LSVM classification, the predictive accuracy of the model was 90.3% (5-fold cross-validation was used). The parameters of cervical length and hCG measurements used in this model are easily detected as part of routine pregnancy follow-up.
As more complex predictive models and algorithms are presented in the field of prenatal care, the rationale and benefit of this model are as follows: LLP is a common obstetrical finding with potentially serious complications for the mother and the fetus. In addition, it is associated with a financial burden as well as emotional stress for the pregnant woman.
Regarding justification of the prediction, using logistic regression, we found that the variables that affected the prediction accuracy most were cervical length measured by ultrasound at 13–16 weeks and second trimester hCG levels.
The more complicated the prediction model, the more data are needed for validation. Since the available data sets were limited in size, validation of the model was performed using 5-fold cross-validation. Splitting the data into training and validation sets may be biased for small data sets; therefore, 5-fold cross-validation is preferable. We speculate that the higher the hCG levels and/or the shorter the cervical length, the better the prediction accuracy.
The clinical implications of this novel model may enable us to detect a high-risk population of women with persistent low-lying placenta diagnosed as early as 16–17 weeks of gestation by using the first anatomic scan and second trimester hCG level. Early detection will improve the follow-up and management of these women, will provide further tools to identify high-risk cases and will reduce stress and uncertainty among all women with LLP. Early detection will also decrease unnecessary costs related to following guideline precautions and follow-up exams for all women with LLP.
Regarding the natural course of LLP detected early in pregnancy, we found that most cases were resolved by 21–24 weeks of gestation. About half of the remaining cases were resolved in the third trimester and only 9.5% persisted until delivery.
Previous studies reported that placenta previa diagnosed in the mid-trimester resolved in 66% to 98% of cases and that resolution is more likely with LLP [Citation4,Citation10]. The process of resolution is termed migration. Among the various hypotheses considering the etiology of migration is trophotropism, the process of atrophy of thin placental margins due to a poor vascular supply in the lower uterine segment [Citation1,Citation11]. Another theory is dynamic placentation, in which it is hypothesized that the anterior uterine wall expands more than the posterior wall. This can relate to a possibly higher migration rate of the anterior placentas because the lower uterine segment will lengthen due to elongation and hypertrophy during pregnancy, causing the uterus to enlarge on the anterior side [Citation1]. The migration process might explain our results. In cases of migration failure, LLP will persist.
Earlier studies that tried to approach this subject were heterogenous and included cases of LLP and complete placenta previa in the same study group [Citation1–4,Citation10,Citation12]. Durst et al. reported 91.9% resolution of LLP or placenta previa among 1663 pregnant women at the mid-trimester anatomic survey [Citation1]. The median time to resolution was 10 weeks. The probability of resolution was inversely proportional to the distance from the internal os. However, this finding is limited because the distance of the placenta from the internal cervical os was known in only 51% of women. Our findings in a population with LLP are consistent with these results.
Using 1 cm from the internal cervical os as a cutoff value, Alouini et al. [Citation2] found that complete placenta previa and most placentas less than 1 cm from the internal cervical os did not migrate. In most cases with placentas located more than 1 cm away, migrated three to four weeks later.
The trend toward shorter cervix and earlier delivery in Group 3 may reflect the negative effects of persistent LLP on the cervix. This might be explained by abnormal vascular changes due to the lower placentation.
Pathological placentation is a term used to describe an abnormal location of the placenta, abnormal invasion of the placenta into the uterine wall, or both [Citation13]. Increased levels of biological markers, such as hCG in maternal serum are thought to result from early placental vascular damage and may be due to their greater absorption into maternal blood flow [Citation13]. Berezowsky et al. found that second-trimester hCG levels were significantly higher among cases of pathological placentation, such as those in the spectrum of placenta previa and placenta accreta [Citation14]. We also found higher levels of hCG the longer the LLP persisted. This can be due to abnormal placentation and is used as a marker in our suggested model.
Peripartum maternal bleeding is another well-known complication of low placentation. Our results revealed that persistent LLP is a risk-factor for heavier bleeding and lower postpartum hemoglobin levels. Therefore, labor involving persistent LLP should be managed carefully, blood products should be appropriately prepared and careful intra- and postpartum clinical surveillance should be performed.
The main limitation of the current study lies in its retrospective design. Nevertheless, it has several important strengths. First, data were collected from a single center with uniform management protocols and all measurements were performed by the same sonographer. Moreover, the relatively large sample of patients with LLP without placenta previa is unique.
In conclusion, the clinical course of pregnancies with LLP and a new model for detecting persistent LLP is presented in this study. Most cases of LLP diagnosed at early anomaly scan resolve before delivery. Persistence versus resolution of LLP may represent two different clinical entities and not a resolution spectrum of the same clinical condition. The longer LLP persists, the less likely it will resolve. LLP that persisted until delivery was associated with unique clinical characteristics and risks, including shorter cervical length, high second-trimester hCG level and maternal complications, which may be explained in part by different pathophysiology of the placentation process. These characteristics can be recognized as soon as the low placentation is diagnosed and may serve as a predictive factor for non-resolution, with an accuracy of 90.3%, as seen in the predictive model. This can increase physician awareness regarding the need for closer surveillance. These findings are very important for obstetricians managing LLP during pregnancy and in the delivery room, as well as while consulting with patients and making shared decisions throughout the pregnancy.
Author contributions
S.F.G, O.M: study design, planning, data analysis, manuscript writing. H.G, M.S.W, G.S.M, H.S, O.W, T.B.S: data analysis and interpretation, revised manuscript. All authors agree with the version to be submitted.
Disclosure statement
The authors report no conflict of interest.
Data availability statement
Data is available upon request.
Additional information
Funding
References
- Durst JK, Tuuli MG, Temming LA, et al. Resolution of a low-lying placenta and placenta previa diagnosed at the midtrimester anatomy scan. J Ultrasound Med. 2018;37(8):2011–2019.
- Alouini S, Megier P, Fauconnier A, et al. Diagnosis and management of placenta previa and low placental implantation. J Matern Neonatal Med. 2020;33(19):3221–3226.
- Lauria S, Smith MR, Treadwell RS, et al. The use of second-trimester transvaginal sonography to predict placenta previa, ultrasound. Ultrasound Obstet Gynecol. 1996;8(5):337–340.
- Rosati P, Guariglia L. Clinical significance of placenta previa detected at early routine transvaginal scan. J Ultrasound Med. 2000;19(8):581–585.
- Dashe D, McIntire JS, Ramus DD, et al. Persistence of placenta previa according to gestational age at ultrasound detection. Obstet Gynecol. 2002;99(5 Pt 1):692–697.
- Oğlak SC, Ölmez F, Tunç Ş. Evaluation of antepartum factors for predicting the risk of emergency cesarean delivery in pregnancies complicated with placenta previa. Ochsner J. 2022;22(2):146–153.
- Reddy UM, Abuhamad AZ, Levine D, et al. Current commentary fetal imaging executive summary of a joint eunice kennedy shriver national institute of child health and human development, society for maternal-fetal medicine, American institute of ultrasound in medicine. Obstet Gynecol. 2014;123(5):1070–1082.
- Oğlak SC, Bademkıran MH, Obut M. Predictor variables in the success of slow-release dinoprostone used for cervical ripening in intrauterine growth restriction pregnancies. J Gynecology Obstetrics Human Reproduction. 2020;49(6):101739.
- Jansen C, de Mooij YM, Blomaard CM, et al. Vaginal delivery in women with a low-lying placenta: a systematic review and meta-analysis. BJOG. 2019;126(9):1118.
- Blouin D, Rioux C. Routine third trimester control ultrasound examination for low-lying or marginal placentas diagnosed at mid-pregnancy: is this indicated? J Obstet Gynaecol Can. 2012;34(5):425–428.
- Herring A, Wolfe HM. Clinical factors associated with its resolution. Am J Perinatol. 2011;28:735–740.
- Smith S, Lauria RS, Comstock MR, et al. Transvaginal ultrasonography for all placentas that appear to be low-lying or over the internal cervical os. Ultrasound Obstet Gynecol. 1997;9(1):22–24.
- Tikkanen V, Hämäläinen M, Nuutila E, et al. Elevated maternal second-trimester serum alpha-fetoprotein as a risk factor for placental abruption. Prenat Diagn. 2007;27(3):240–243.
- Berezowsky A, Pardo J, Ben-Zion M, et al. Second trimester biochemical markers as possible predictors of pathological placentation: a retrospective case-control study, fetal. Fetal Diagn Ther. 2019;46(3):187–192.