Abstract
Objective
To develop a conceptual framework around the factors that influence audiologists in the clinical uptake of remote follow-up hearing aid support services.
Design
A purposive sample of 42 audiologists, stratified according to client-focus of either paediatric or adult, were recruited from professional associations in Ontario, Canada, as members of the six-step, participatory-based concept mapping process. Analyses included multidimensional scaling and hierarchical cluster analysis.
Results
Six main themes emerged from this research according to overall level of importance: (1) technology and infrastructure; (2) audiologist-centred considerations; (3) hearing healthcare regulations; (4) client-centred considerations; (5) clinical implementation considerations; and (6) financial considerations. Subthemes were identified at the group-level and by subgroup. These highlight the importance of TECH factors (accessible Technology, Easy to use, robust Connection, and Help available), as well as the multi-faceted nature of the perceived attitudes/aptitudes across stakeholders.
Conclusion
Findings can be utilised in tailored planning and development efforts to support future research, knowledge dissemination, best-practice protocol/guideline development, and related training to assist in the clinical uptake of remote follow-up hearing aid support services, across variable practice contexts.
Introduction
The increasing global prevalence of hearing loss, paired with a demand for improved access to service provision due to low patient-provider ratios (World Health Organization Citation2019), has created demand for non-traditional service delivery models. In Canada, the speech-language pathology and/or audiology patient-provider ratio is estimated at 6:100,000 (Speech-Language and Audiology Canada Citation2019). Non-traditional service delivery models, outside of a face-to-face model, are generally focussed on the delivery of services at a distance (herein referred to as remote services). Remote service delivery relies on information and communication technology to connect all stakeholders involved in the care process. For example, remote services can be used to connect a hearing healthcare professional, situated in a clinic, with their client at home. The connected health model is described as a conceptual model for the delivery and management of health, where devices, services, or interventions are designed around the patient’s needs; connecting all stakeholders in the sharing of information through smarter use of data, devices, communication platforms and people (Caulfield and Donnelly Citation2013). The term “connected hearing healthcare” is starting to emerge in audiology literature and has been proposed as an umbrella term, encompassing terms like “telepractice in audiology”, “tele-audiology”, “eAudiology” and other remote/virtual service delivery options (Davies-Venn and Glista Citation2019). The connected health model highlights a dynamic model of service provision that recognises the changing health care needs and contexts in society, with patient empowerment being an important component.
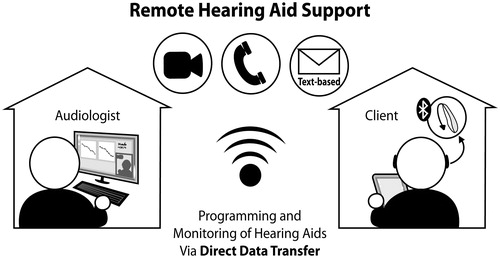
The upsurge of technology-driven applications in audiology, designed to enable remote service delivery, calls attention to the need for a connected hearing healthcare model of care that encapsulates tele-audiology and other related terms. Audiological services can now be delivered remotely during screening, diagnosis and intervention appointments (Swanepoel and Hall Citation2010); this is mainly due to the significant advancements in technology over the past decade, including wireless and digital chip technology, driven by trends such as connectivity and individualisation (Edwards Citation2007). When considering intervention advancements, remote hearing aid (HA) support is an example of an application gaining considerable interest in audiology. An example of current remote HA technology includes the use of Bluetooth connectivity, to transfer data from a HA to an app on a smart device, and wireless connectivity, to transfer the data from the smart device to a laptop computer with HA fitting software. illustrates an example of remote HA support as part of a follow-up appointment, including an audiologist positioned in their clinic and a HA user in their home. Studies have begun to demonstrate that remote service delivery can provide greater access to a family-centred care model. Muñoz et al. (Citation2017) discuss the benefits of connected hearing healthcare in the management of paediatric HA fittings to include greater flexibility and convenience, along with the potential to include multiple family members in the care process. The benefits of remote services related to HA management are also discussed in the adult literature, suggesting greater efficiency and timeliness related to HA counselling services, when compared to face-to-face appointments. When considering best-practice requirements for initial hearing aid fitting appointments, greater time may be needed to perform technical procedures such as HA verification involving a probe microphone system; current examples in the literature include the use of client-site facilitator(s) and remote use of specialised equipment (Campos and Ferrari Citation2012; Ferrari and Bernardez-Braga Citation2009). Depending on the support needed, remote follow-up hearing aid appointments may also require the use of verification procedures. In some telepractice delivery scenarios, a facilitator and often a team-based approach can be beneficial (Novak et al. Citation2016); for example, a caregiver, other healthcare professionals, or healthcare students could assist in the delivery of services, benefitting the patient, the training model and interprofessional relationships.
Figure 1. Illustration of a remote hearing aid support application - connecting an audiologist at a clinic-site to a patient at home.
Over the past decade, researchers have started to explore the potential of remote service delivery from an implementation science perspective. A recent systematic review on the barriers of adopting telemedicine worldwide (across health fields) site the top barriers as technology-specific and likely overcome by training, change-management strategies, and through better patient-to-provider interaction (Kruse et al. Citation2018). Specific to the field of audiology, the literature points to the major barriers to uptake being related to infrastructure, reimbursement, and licensure (Ravi et al. Citation2018). In general, HAs that possess the ability to connect to smart technologies are thought to influence the provider, patient, and patient-provider experience, specifically when considering the candidacy profile of the user and the nature and time spent during interactions; the authors of this work conclude that more research and clinical consideration is needed to support uptake (Ng et al. Citation2017).
Various surveys have suggested that the attitude of the service provider is not likely a significant barrier, with most audiologists possessing a positive attitude towards remote service delivery, especially when considering adult-focussed services related to follow-up clinical appointments (Eikelboom and Swanepoel Citation2016; Singh et al. Citation2014; Swanepoel and Hall Citation2010). Furthermore, the American Speech-Language-Hearing Association (ASHA Citation2002, Citation2016) reports growing use patterns around services related to counselling and follow-up care, especially when focussed on areas related to HA(s), hearing disorder(s) and aural rehabilitation. A less-positive attitude towards remote service delivery has been reported when considering vulnerable populations (e.g. paediatric patients), when performing clinical tasks with low perceived suitability to tele-audiology and/or with patients for whom rapport was newly developing (e.g. those requiring tactile information, initial fittings, and new patients and assessments) (Singh et al. Citation2014). Therefore, it is likely that clinical uptake will differ according to the type of care being delivered and/or the patient group receiving care.
Overall, current literature suggests a strong capacity for, but an underutilisation of, remote care within current adult hearing services (Meyer et al. Citation2019). These findings align with those reported in a recent survey exploring Canadian audiologists’ readiness to adopt a connected model of care during HA management; while approximately half of the respondents reported engaging in some form of connected audiological care, significantly fewer, approximately a quarter of the respondents, had engaged in the delivery of remote HA support services (Perez et al. Citation2020). Further research is therefore needed to explore factors related to the low clinical uptake of remote services in hearing healthcare and especially those related to HA support and management. A review of concept mapping (CM), a useful methodology in implementation science research (Joukes et al. Citation2016), is provided below. CM is a participatory research method, with stakeholder involvement spanning the entire process. Specifically, group CM is a structured process focussed on a topic or construct of interest, involving input from multiple participants, that produces an interpretable pictorial view of ideas and concepts and how they are interrelated (Trochim Citation1989). Traditionally, this involves a six-step mixed-methods process, described by Trochim and McLinden (Citation2017) to include:
Preparation: the study focus, rating scales, participant selection criteria/descriptive data and study logistics are outlined. The study focus is operationalised into a focus prompt that is phrased as an open-ended imperative statement to encompass the desired content for the map and guide the participants during the statement generation step. Participant sampling should include a diverse group of participants, while still using opportunistic sampling to ensure that the study focus is represented closely.
Generation: participants perform a brainstorming activity to create a rich and varied set of statements corresponding to a defined study focus. This step often includes editing and synthesising of the original list(s) to remove poorly worded or redundant statements.
Structuring: the collection of descriptive data (enabling subgroup analyses), as well as the sorting and rating of the statements. Rating tasks generally include five-point Likert-type scales.
Representation: data analysis techniques and pictorial representation of the data in the form of a map. More commonly used CM software options include multidimensional scaling to yield a two-dimensional configuration of the set of statements (represented on a point map), and hierarchical cluster analysis to create a non-overlapping cluster solution map. The final cluster solution should both preserve detail and yield interpretable statement clusters. Other useful analyses often incorporated into the representation stage include pattern matches and go-zone plots, which allows for the comparison of datasets based on importance-level.
Interpretation: usually a joint participatory collaborative process involving the researchers and participants in the final labelling of clusters and the resulting map.
Utilisation: an ongoing process that can assist with planning and development of frameworks to use in a future programme(s), planning and/or evaluation(s).
In this study, the primary research objective was to use CM to develop a conceptual framework developed from audiologists’ experiences, perceptions, thoughts, and ideas around the factors influencing the clinical adoption of remote HA support services during a follow-up appointment. A secondary research objective was to explore whether these factors differed across the subgroups of paediatric-audiologists compared with audiologists who primarily worked with adult patients.
Materials and methods
Participants
Participants included audiologists that were recruited by email or telephone from the College of Audiologists and Speech-Language Pathologists of Ontario public registrar of members and through researcher-engaged professional networks. Participants were screened for eligibility via the telephone or by email using the following inclusion criteria: (a) currently employed in the province of Ontario; (b) providing services around HA fitting, including follow-up HA support services; (c) having access to a computer and the internet; and (d) is English-speaking. Purposive sampling was used to identify participants that self-identified themselves as belonging to one of the two following subgroups:
Paediatric-focussed audiologists (herein referred to as paediatric-audiologists): hold the technical expertise and desire to provide services to paediatric clients aged 0–17 years and provide services to a larger proportion of children than adults; and
Adult-focussed audiologists (herein referred to as adult-audiologists): hold the technical expertise and desire to provide clinical services to adult clients aged 18 years of older and provide services to a larger proportion of adults than children.
outlines the participant characteristics collected at the beginning of each group session, from a paper-and-pencil questionnaire, and provides a breakdown of the characteristics according to subgroup. Overall, the research team strived to include a heterogeneous sample of audiologists that was stratified according to client-focus (adult versus paediatric). The final group of 42 audiologists was largely comprised of experienced clinicians (62%) from a variety of practice settings. While 54% of the participants were between 30 and 49 years of age, a larger proportion of paediatric-audiologists were above 55 years of age (33%), compared to adult-audiologists (2%). Almost all adult-audiologists practiced in private-practice settings (93%), while the paediatric-audiologists were mostly split between private practice (39%) and hospital-based (43%) settings. The overall group reported providing services across all age groups similarly. The subgroups were consistently defined through self-identification and questionnaire results, with the questionnaire results indicating 100% service provision to clients aged 18−65+ years for adult-audiologists and 96% service provision to children aged 0−17 for paediatric-audiologists. Almost all owned a smartphone (98%) and a laptop computer (90%), and the majority owned a tablet (71%) and a desktop computer (52%). Adult-audiologists reported a higher overall skill level (mostly “advanced”), when compared to paediatric-audiologists (mostly “average”) when using computer, smartphones, and tablets. Most audiologists reported having access to workplace IT support (88%) and few currently offer tele-audiology services (12%).
Table 1. Participant characteristics for the overall group (N) and for participant-identified groups based on patient focus (n).
Procedures
The Health Sciences Research Ethics Board of The University of Western Ontario granted ethical approval for this study. CM integrates qualitative (group process, brainstorming, unstructured sorting, and interpretation) and quantitative (multidimensional scaling and hierarchical cluster analysis) research methods to enable stakeholders to articulate and graphically depict a coherent conceptual model of the topic of interest (Trochim and McLinden Citation2017). Procedures in this study followed the six-step process, as described by Trochim and McLinden. All participants provided written consent to participate in one face-to-face group session, as well as several follow-up web-based tasks using a personal computer. Participants completed web-based tasks, including sorting and rating, using The Concept System® Global Max© Software by Concept Systems (2017) (herein referred to as Global Max software). To enable web-based tasks, participants were invited via email, in which a web-link to the Global Max software was provided. A paper record of a unique login and password was provided to each participant during the group sessions.
Preparation
The focus of this study was to investigate the range of factors that practising audiologists felt would influence their use of tele-audiology when performing remote HA support services in a follow-up appointment. This study did not focus on the use of alternate delivery models during initial hearing aid appointments, nor did it focus on incorporating additional healthcare professionals to operate specialised equipment at the remote client-site. As part of the preparation step, the core research team, together with 3 external experts on the topics of CM and/or tele-audiology, developed a “prompt” or focus statement to be used in the brainstorming step. The core research team was composed of a group of clinician-scientists specialising in both clinical and research-focussed audiology practices. The research team and external experts came to consensus on the following focus statement “One thing that may influence my use of tele-audiology for remote follow-up hearing aid support is…” Also included in the preparation step was the development of all project tools which included an introductory PowerPoint presentation describing tele-audiology, remote HA support services, and the difference between initial versus follow-up appointments for participants. Remote HA support was described to include all types of HA troubleshooting, adjustments, and management. This description did not include the use of remote probe microphone measurement to verify fittings remotely or the need for a facilitator to operate specialised equipment in the remote location. Discussion around the use of optional parent and/or caregiver roles to aid in facilitating home-based appointments were included (e.g. technology set-up). An importance rating scale using a 5-point Likert scale (1 = relatively unimportant; 2 = somewhat important; 3 = moderately important; 4 = very important; 5 = extremely important) was also developed during the preparation step.
Brainstorming and idea synthesis
Face-to-face group brainstorming was completed using five sessions of non-overlapping participant groups (M = 8.8 participants/group, Min = 7, Max = 12). The group sessions lasted between 2 and 3 hours and were held in small conference rooms. The location of each session was determined by an accessible central location for each group of clinicians. For some participants, the group session was held in the same building as their place of practice and/or was attended by colleagues. All groups were moderated consistently and in a way that encouraged equal participation from all attending audiologists, resulting in an open discussion platform at each session. A total of 42 audiologists completed the brainstorming (100% of recruited participants): 15 adult-audiologists and 27 paediatric-audiologists. Each session began with a brief prepared presentation, followed by a paper and pencil questionnaire outlining key participant characteristics (); this data was later entered into web-based software by the researchers. Statement generation was guided using the focus statement in a complete-the-sentence instruction format. The researchers compiled the five statement sets into one large set of all statements (n = 401). This was edited and synthesised, by the research team, to eliminate redundancies and refine statements to ensure clarity and comprehension; statements that were unrelated to the prompt were removed, statements were also merged or split to ensure that each statement had one clear meaning; methods followed those previously sighted in the CM literature (Bennett et al. Citation2018; Wutzke et al. Citation2017). The statement synthesis steps were recorded to create an audit trail. On average, each group session resulted in 80 statements (Min = 67 and Max = 90). The final set included 106 unique statements related to the focus statement.
Structuring
Web-based data structuring, using Global Max software, included two phases: sorting and rating. All structuring tasks were completed by the participants, at their convenience, within a one-month period. The total sample for all structuring tasks well-exceeded the recommended sample size of 15 (Rosas and Kane Citation2012). A total of 40 participants completed the sorting step (95% of total sample): 14 adult-audiologists (7% dropout rate) and 26 paediatric-audiologists (4% dropout rate). Dropout rates for all structuring tasks were calculated according to the original sample size. Participants were provided with the following instructions when completing statement sorting: (a) group similar statements together into piles, (b) give each pile a name that captures the meaning of the content of the pile, (c) do not create piles according to priority or value (e.g. importance), (d) do not create miscellaneous or “other” piles, (e) statements can be put alone in a pile if unrelated to all other statements, and (f) do not leave any statements unsorted. On average, the audiologists sorted the statements into 10.5 piles (Min = 4, Max = 33 and SD = 5.4).
A total of 38 participants completed the rating step (91% of total sample): 14 adult-audiologists (7% dropout rate) and 24 paediatric-audiologists (11% dropout rate). Participants were asked to rate the importance of each statement using the 5-point Likert scale, indicating the relative importance of each statement in influencing the use of tele-audiology in remote HA support services. The average rating value for the participant group was 3.5. Individually, 31 participants used the full range of the scale when rating statements (i.e. values ranged from 1−5); the remaining seven participants used values between 2 and 5 to complete ratings.
Results
The representation of CM results was enabled using the Global Max software and two types of analyses: multidimensional scaling and hierarchical cluster analysis. Details pertaining to the production of the final concept map and accompanying pattern match are described in the representation section.
Representation
Multidimensional scaling was used to locate each statement in a two-dimensional space to display on a point map, using the following steps (Kane and Trochim Citation2007):
A similarity matrix, using a similarity cut-off of 3 to filter out spurious relationships between statements, was generated by pairing the 106 statements with one another and assigning a numerical value indicating the number of people who put that pair of statements in the same pile.
A two-dimensional solution was used to produce X-Y coordinates for each statement, following a bivariate distribution.
These steps resulted in the generation of a point map with a cluster solution shown as . Each point on the point map represents one statement. Statements that were sorted together more often by the participants appear as points closer together, statements that were less often sorted together appear further apart (Trochim and McLinden Citation2017). Stress is a statistic routinely generated and reported in multidimensional scaling analyses, indicating how well the statement configuration matches the data (Rosas and Kane Citation2012). The final stress value of 0.28, which falls within the normal and acceptable range for CM research (Kane and Trochim Citation2007; Kaplan et al. Citation2016), indicates that the map appropriately represents the sorting data.
Figure 2. Six-cluster map, of the 106 statement point map, of factors influencing the use of tele-audiology for remote hearing aid support labelled by importance rating.
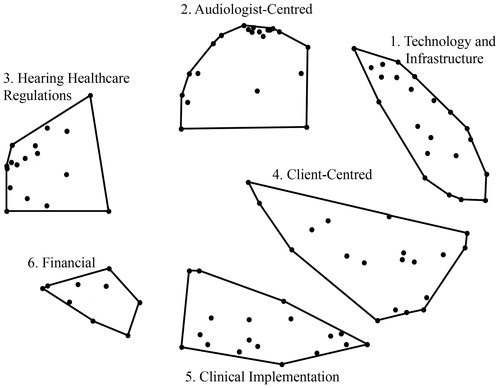
Hierarchical cluster analyses, using input from multidimensional scaling, mathematically grouped each statement into adjustable cluster solutions, based on how participants rated and sorted the data. Each cluster represents a unique theme on the resulting map, as seen in . All possible cluster solutions between 4 and 12 were examined by the research team and a final solution of 6 clusters was selected; this was analysed using guidance from the Global Max software (e.g. bridging and anchoring values) and was chosen to yield an interpretable and parsimonious cluster solution (Wutzke et al. Citation2017). Final cluster labels reflect the general theme for each cluster of statements. Using single cluster go-zone plots, allowing for visualisation of the relationship between participant ratings by subgroup and with respect to the concept map, a list of the main themes, subthemes and example statements was reported (). A go-zone, calculated per cluster, is a bivariate plot of the data that compares statements across two variables of interest. For this project, the subgroups of interest were used to define the X and Y variables on the go-zone plot, resulting in a representation of the statements in quadrants and according to the mean value for the cluster and for each subgroup (Kane and Trochim Citation2007). This information was used to inform the themes (i.e. statements that were rated to reside above the mean for both subgroups) as well as the subthemes presented in . Subthemes that applied to the overall group were first identified by the research team, followed-by separate subthemes specific to either the paediatric- or adult-audiologist subgroups (i.e. statements that resided above the mean for each subgroup separately). The three example statements presented by theme included those that received high overall average ratings of importance. The total number of statements sorted into each cluster is reported in M = 17.67); a total list of statements is available upon request.
Table 2. Concept mapping clusters, subthemes and example statements created using the prompt: one thing that may influence my use of tele-audiology for remote follow up hearing aid support is….
Table 3. Clusters and corresponding total statement numbers arranged by importance level, along with the overall and subgroup mean importance values.
The reliability of the sorting and rating data was analysed according to methods presented by Rosas and Kane (Citation2012). For the sorting data, split-half reliability analyses were completed by dividing the total group into two randomly assigned groups. A correlation analysis using the Spearman-Brown correction was then completed for both sort matrices (from each split-half group) to obtain the split-half reliability of the sorts. This resulted in a high average split-half total matrix reliability of .89, which is slightly higher than the average reported split-half reliability from a meta-analysis conducted on 69 concept mapping studies. The internal consistency of the rating data was assessed by computing the average correlation among items using Cronbach’s alpha. This resulted in a reliability score of .95, suggesting high internal consistency and intercorrelation (Rosas and Kane Citation2012).
presents the mean importance values for each cluster, according to the overall group and by subgroup. Mean cluster values are presented in order of most important to least important and correspond to responses collected using the five-point scale of importance. To further illustrate the similarities/differences in importance ratings across subgroups, an absolute pattern match diagram is provided in .
Figure 3. Absolute pattern match diagram comparing relative importance levels between adult- and paediatric-audiologists, overall and at the single cluster level. Statistically different ratings by subgroups and cluster are denoted with an asterisk (*).
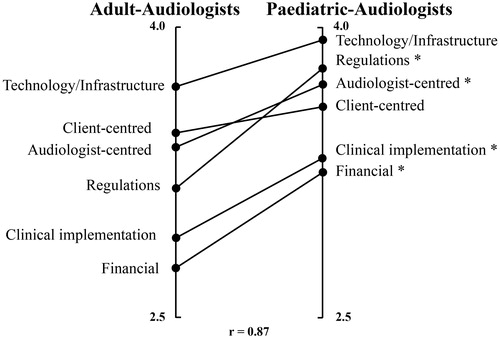
shows a strong overall correlation between the relative average cluster importance ratings for audiologists (r = .87), with some discrepancies noted when comparing relative averages at the single cluster level and across audiology subgroups. Paired-sample t-tests were conducted to compare importance level for each cluster by subgroup. There was a significant difference in relative importance ratings by subgroup for 4/6 of the clusters: audiologist-centred considerations [t (40) = 2.33, p < 0.05]; hearing healthcare regulations [t (32) = 4.37, p < 0.001]; clinical implementation considerations [t (34) = 2.39, p < 0.05]; and financial considerations [t (16) = 2.83, p < 0.02]. These results suggest that the paediatric-audiologists placed a significantly higher level of importance on all four of these themes, when compared to the adult-audiologists.
Interpretation
The results of this study were provided to all participating audiologists in the form of a concept map (with included importance levels), underlying statements, and an explanation written in understandable language. Using email correspondence, participants were asked to interpret the results and indicate their level of agreement. In the case where a participant did not agree with a label(s) and/or the cluster solution, they were encouraged to suggest an alternate one. Six of the 42 audiologists chose to participate in the interpretation step of the study, with all but one indicating total agreement with the presented results. The remaining audiologist indicated feeling unsure about labelling but did not offer alternate options.
Discussion
The primary objective of this study was to develop a conceptual framework related to factors, perceived by audiologists, to affect the clinical adoption of remote follow-up HA support services. A total of 42 audiologists practicing in Ontario, Canada, were recruited to participate in this study. The secondary objective was to explore whether the main age group of the audiologists’ clients (paediatric versus adult) influenced their perceived importance of the CM themes identified.
The resulting framework consisted of six main themes thought to influence audiologists’ uptake of remote follow-up HA support services (in order of most to least importance to the overall group): (1) technology and infrastructure; (2) audiologist centred considerations; (3) hearing healthcare regulations; (4) client-centred considerations; (5) clinical implications; and (6) financial considerations. Technology and infrastructure were rated to be of greatest importance by both adult- and paediatric-audiologists. This finding is consistent with the literature, with technology-specific barriers being cited at the top of the list of barriers to adopting telemedicine worldwide (Kruse et al. Citation2018). For the audiologists included in this study, the subthemes identified in the technology and infrastructure theme can be best described by the acronym “TECH” (accessible Technology, Easy to use, robust Connection, and Help available). Top rated overall statements defining TECH related to:
T: Accessibility of required technology to perform remote HA support, considering the audiologist in their clinic and the client in their home environment, including the internet, a computer, software, a smartphone/tablet, HA devices, and/or access to funds to purchase items not currently available.
E: Whether the technology was “easy to use”, guidance tools (e.g. demonstration tools) were available during applications, and the client possessed a positive or “open” feeling towards technology in general.
C: The robustness of the available internet connection for all users (e.g. reliability and efficiency) and the ability of tele-audiology technologies to connect to a wide range of smartphones/tablets.
H: Availability of support to help with the set-up, maintenance, and ongoing support “at time of need” for all users, including workplace support as well as support from caregivers and/or other professionals.
The findings from this study also suggest a relationship between the perceived importance of the themes and the subgroups of interest. Overall, paediatric-audiologists placed a higher importance level on all themes (refer to ), and rated four of the six themes as being significantly more important, when compared to adult-audiologists (refer to ). Of these four themes, the hearing healthcare regulations theme presented the greatest discrepancy in importance level by subgroup. The paediatric-audiologists placed markedly higher importance on the need for regulations to define standards around tele-audiology practices (e.g. client/patient consent, privacy, and security) and the opportunity to follow best-practice protocols. This may be explained by the fact that all paediatric-audiologists in this study were part of the province-wide early hearing detection and intervention programme (The Ontario Infant Hearing Program; IHP). In brief, the IHP provides hearing screening to all newborns, coordinates services to support language development until school-age, and trains all support personnel in the provision of a wide-range of audiological services, each with specific protocols developed within the programme (Ontario Ministry of Children and Youth Services Citation2017). The noted subthemes of importance to paediatric-audiologists, therefore, align with the specialised training and protocol requirements that are part of this programme. Furthermore, close to half of the paediatric-audiologists included in this study reported their main place of practice to be hospital-based, a highly regulated healthcare environment, whereas almost all adult-audiologists were practising out of private-practise settings in the community. These findings are likely to generalise to most of the Canadian healthcare context, considering provinces that offer IHPs, and to other countries in the cases where training in a paediatric-audiology specialisation and regulated services are governed at the state or provincial level. Current literature on the use of telehealth services to facilitate audiological management for children echoes this need for protocols and procedures in order to ensure that tele-audiology services are provided in a standardised manner (Blaiser et al. Citation2013; Govender and Mars Citation2017).
The adult-audiologists in this study also valued the opportunity to practice in a regulated manner and placed a greater importance around knowledge related to the validity of remote HA service delivery and the impact of this service delivery model on adoption and return rates. These adult-focussed subthemes speak to the need for more research around remote HA support services and studies that directly compare to a face-to-face service model. The majority of studies evaluating remote audiological management, including remote HA support, have focussed on the feasibility of the service delivery model and/or the perceived benefit/satisfaction of the end-user (Angley, Schnittker, and Tharpe Citation2017; Brännström et al. Citation2016; Gladden, Beck, and Chandler Citation2015; Govender and Mars Citation2017; Penteado et al. Citation2014). Studies related to the verification and validation of remote follow-up HA support services are also warranted. The few publications found in the literature have included HA usage and applications involving a facilitator and videoconferencing to evaluate remote probe microphone measurement (Campos and Ferrari Citation2012; Ferrari and Bernardez-Braga Citation2009).
At the time of this study, remote verification of HA fittings was not possible without the use of a facilitator and specialised equipment positioned in the remote location. Although not a focus of this study, recent research outlines how a trained facilitator can be used to verify an initial remote fitting and/or of the effects of adjustments made in a follow-up remote fitting (Campos and Ferrari Citation2012; Novak et al. Citation2016). In the current study, HA support topics were discussed in the context of a follow-up appointment, not an initial fitting. The topic of verification was highlighted in the audiologist-centred theme in relation to perceived comfort around and accuracy with which the audiologists felt they could perform remote HA support services. Other specific applications that were rated as important to the overall group included using remote services to make gain adjustments, programme/fine-tune devices, manage feedback, pair wireless accessories, and monitor overall usage. The audiologists’ overall technological knowledge level and access to related training were factors that emerged as important to all audiologists. The adult-audiologists placed greater importance on the time and motivation needed to keep up with the required technologies. This theme raises the need for clinical guidance documents to support audiologists’ in the clinical implementation of specific applications related to remote HA support services. Methods for evaluating the technical competencies required of audiologists when providing remote services are also needed.
When considering client-centred factors that emerged from this study, an overall high importance level was placed on improving access to services using remote delivery, and on their client’s ability to communicate effectively and/or benefit from an appointment outside of the clinic (e.g. in a real-world school or home context). Access-related statements included mention of “travel-related constraints”, “difficult to reach clients/caregivers”, and enabling the inclusion of people within the client’s circle of care in appointments. Paediatric-audiologists placed a high importance level on multi-lingual service delivery, while adult-audiologists were highly interested in gaining knowledge of the client’s preference for remote versus face-to-face services and their perceived value of remote services. This suggests the need to develop and validate tools that will assist the audiologist in evaluating client/family candidacy for remote service delivery. Candidacy evaluation tools have started to emerge as a topic of interest in the literature (Muñoz et al. Citation2017); however, further research is warranted to be able to offer standardised clinical tools that are appropriate across populations (adult compared with paediatric populations).
Considering the group of audiologists’ in this study, very few currently provide any type of tele-audiology service (12%). This finding is consistent with those reported in a large-scale survey on audiologists’ attitudes towards telehealth, which concludes that despite the fact that most have a positive attitude, international implementation rates of telehealth are reported to be less than 25% (Eikelboom and Swanepoel Citation2016). In this CM study, perceived clinical implementation factors were focussed on the timeliness and ease of remote service delivery and related scheduling factors, including access to an optimal practice environment and the management of patient expectations around the “24/7” trend in service provision. Paediatric-audiologists valued the idea of providing more frequent follow-up appointments to families and in experiencing fewer missed appointments as a result of remote delivery; these subthemes align with the current literature around timeliness of service delivery for children with hearing impairment, indicating audiological follow-up to be one of the key factors in reducing the adverse effects of hearing loss on developmental outcomes (Walker et al. Citation2014).
Of the six themes that emerged from this study, the financial considerations theme was rated to have the lowest importance. The overall subthemes of knowledge of reimbursement models and their clinical application emerged as being important to all audiologists, aligning with the general need for best practice guidelines to support clinical uptake. Paediatric-audiologists indicated the importance of general financial constraints in their practice context, while adult-audiologists placed more value on being able to cover specific costs related to licencing and training of staff. Overall, tele-audiology is often reported in the literature to be a cost-effective supplement to face-to-face service provision (Ravi et al. Citation2018), which may have contributed to audiologists’ perceived low importance level with regards to financial considerations in this study.
Utilisation
Trochim and McLinden discuss the utilisation step in CM research as an ongoing process related to the study objective(s) and resulting conceptual framework (Trochim and McLinden Citation2017). Findings from this study, which focussed on the factors influencing audiologists’ clinical uptake of remote follow-up HA services, included six main themes and related subthemes. The themes and subthemes suggest the need for improved organisational/stakeholder buy-in to support and improve on TECH factors, the provision of knowledge (e.g. through literature and practice guidelines) to support positive attitudes; the provision of best-practice protocols and related training to support aptitudes; and overall implementation of remote services into varying clinical contexts/workflows. Our implementation plans will also include best-practice recommendations for connected hearing healthcare services such as the use of client-site facilitators for remote paediatric audiology practice. The findings from this study can be used to tailor planning and implementation efforts according to a client/family-focus, with an emphasis on the provision of best-practice protocol documents around remote HA support services in the context of specialised paediatric care.
Limitations and future research
Although participating audiologists were recruited from a range of practice contexts/locations, providing services to both adult and paediatric clients, the geographical reach of their services was not explored in this study. Given the practice locations of the participating audiologists, being mainly based in medium-to-large urban population centres in Ontario, Canada, service provision was likely focussed on urban-based clientele. Future research incorporating audiologists that routinely provide services to clients residing in rural centres is warranted to explore whether the perceived factors and/or the importance level of the main themes would differ from those reported in this study. In addition, research investigating the factors that influence audiologists’ use of remote hearing aid fitting support when incorporating a facilitator to operate specialised equipment would be of value to the field.
As discussed in previous CM studies related to hearing aids, the personal attributes of the included participants likely shaped the results of this study (Bennett Citation2019). When considering the variable experiences and perceptions brought forth by this group of audiologists, several factors related to the participants’ “attitudes” towards the topic of remote HA support likely influenced the results. A robust sample of 42 audiologists was included in this study; however, it is possible that the results may have differed according to the group of participants included and their relation to each other. Although, each brainstorming session was carefully and consistently moderated by the research team, participation may have been influenced by the presence of colleagues and/or employers. For some participants, the group session was held in the same building as their place of practice and/or was attended by colleagues; these factors may have influenced the discussion that took place. Furthermore, motivation to pursue professional development, willingness to engage in an alternate service delivery model, and attitudes around organisational buy-in likely shaped the way in which each audiologist contributed to the study. Future research carried out in a country-wide survey, for example, could help inform the themes and underlaying subthemes that significantly contribute to audiologists’ “readiness” to uptake of remote service delivery for urban versus remote population centres.
| Abbreviations | ||
| CM | = | Concept mapping |
| HA | = | Hearing aid |
| IHP | = | Infant Hearing Program |
| M | = | Mean |
| Max | = | Maximum |
| Min | = | Minimum |
| TECH | = | Accessible Technology, Easy to use, robust Connection, and Help available |
Acknowledgements
Special thanks to Dr. Laya Poost-Foroosh, Dr. Mary-Beth Jennings and Dr. Gurjit Singh for their valuable guidance in the planning phase of the study, to Keshinisuthan Kirubalingam for his contributions to the project and to Dr. Scott Rosas for statistical guidance. Finally, the authors are thankful to the participants of this study for their time and efforts.
Disclosure statement
Danielle Glista is a member of the following advisory boards: Phonak expert circle on eAudiology and the College of Audiologists and Speech-Language Pathologists of Ontario Telepractice Advisory Working Group.
Additional information
Funding
References
- American Speech-Language-Hearing Association. 2002. Survey Report on Telepractice Use among Audiologists and Speech-Language Pathologists, 1–12. Rockville, MD: American Speech-Language-Hearing Association. https://www.asha.org/uploadedFiles/practice/telepractice/SurveyofTelepractice.pdf.
- American Speech-Language-Hearing Association. 2016. 2016 SIG 18 Telepractice Survey Results. Rockville, MD: American Speech-Language-Hearing Association. https://www.asha.org/uploadedFiles/ASHA/Practice_Portal/Professional_Issues/Telepractice/2016-Telepractice-Survey.pdf.
- Angley, G. P., J. A. Schnittker, and A. M. Tharpe. 2017. “Remote Hearing Aid Support: The Next Frontier.” Journal of the American Academy of Audiology 28 (10): 893–900. doi:10.3766/jaaa.16093.
- Bennett, R. J. 2019. “Improve Your Patients’ Hearing Aid Management Skills.” The Hearing Journal 72 (4): 20–21. doi:10.1097/01.HJ.0000557746.12905.5a.
- Bennett, R. J., C. J. Meyer, R. H. Eikelboom, and M. D. Atlas. 2018. “Investigating the Knowledge, Skills, and Tasks Required for Hearing Aid Management: Perspectives of Clinicians and Hearing Aid Owners.” American Journal of Audiology 27 (1): 67–84. doi:10.1044/2017_AJA-17-0059.
- Blaiser, K. M., D. Behl, C. Callow-Heusser, and K. R. White. 2013. “Measuring Costs and Outcomes of Tele-Intervention When Serving Families of Children Who Are Deaf/Hard-of-Hearing.” International Journal of Telerehabilitation 5 (2): 3–10. doi:10.5195/ijt.2013.6129.
- Brännström, K. J., M. Öberg, E. Ingo, K. N. T. Månsson, G. Andersson, T. Lunner, and A. Laplante-Lévesque. 2016. “The Initial Evaluation of an Internet-Based Support System for Audiologists and First-Time Hearing Aid Clients.” Internet Interventions 4: 82–91. doi:10.1016/j.invent.2016.01.002.
- Campos, P. D., and D. V. Ferrari. 2012. “Teleaudiology: Evaluation of Teleconsultation Efficacy for Hearing Aid Fitting.” Jornal da Sociedade Brasileira de Fonoaudiologia 24 (4): 301–308. doi:10.1590/s2179-64912012000400003.
- Caulfield, B. M., and S. C. Donnelly. 2013. “What is Connected Health and Why Will It Change Your Practice?” QJM: Monthly Journal of the Association of Physicians 106 (8): 703–707. doi:10.1093/qjmed/hct114.
- Davies-Venn, E., and D. Glista. 2019. “Connected Hearing Healthcare: The Realisation of Benefit Relies on Successful Clinical Implementation.” ENT & Audiology News 28 (5): 59–60.
- Edwards, B. 2007. “The Future of Hearing Aid Technology.” Trends in Amplification 11 (1): 31–45. doi:10.1177/1084713806298004.
- Eikelboom, R. H., and D. Swanepoel. 2016. “International Survey of Audiologists' Attitudes Toward Telehealth.” American Journal of Audiology 25 (3S): 295–298. doi:10.1044/2016_AJA-16-0004.
- Ferrari, D. V., and G. R. A. Bernardez-Braga. 2009. “Remote Probe Microphone Measurement to Verify Hearing Aid Performance.” Journal of Telemedicine and Telecare 15 (3): 122–124. doi:10.1258/jtt.2009.003005.
- Gladden, C., L. Beck, and D. Chandler. 2015. “Tele-Audiology: Expanding Access to Hearing Care and Enhancing Patient Connectivity.” Journal of the American Academy of Audiology 26 (9): 792–799. doi:10.3766/jaaa.14107.
- Govender, S., and M. Mars. 2017. “The Use of Telehealth Services to Facilitate Audiological Management for Children: A Scoping Review and Content Analysis.” Journal of Telemedicine and Telecare 23 (3): 392–401. doi:10.1177/1357633X16645728.
- Joukes, E., R. Cornet, M. C. de Bruijne, and N. F. de Keizer. 2016. “Eliciting End-User Expectations to Guide the Implementation Process of a New Electronic Health Record: A Case Study Using Concept Mapping.” International Journal of Medical Informatics 87: 111–117. doi:10.1016/j.ijmedinf.2015.12.014.
- Kane, M., and W. Trochim. 2007. Concept Mapping for Planning and Evaluation: Vol. 50 (L. Bickman & D. J. Rog, Eds.). Thousand Oaks, CA: Sage Publications.
- Kaplan, D. M., M. deBlois, V. Dominguez, and M. E. Walsh. 2016. “Studying the Teaching of Kindness: A Conceptual Model for Evaluating Kindness Education Programs in Schools.” Evaluation and Program Planning 58: 160–170. doi:10.1016/j.evalprogplan.2016.06.001.
- Kruse, C. S., P. Karem, K. Shifflett, L. Vegi, K. Ravi, and M. Brooks. 2018. “Evaluating Barriers to Adopting Telemedicine Worldwide: A Systematic Review.” Journal of Telemedicine and Telecare 24 (1): 4–12. doi:10.1177/1357633X16674087.
- Meyer, C., M. Waite, J. Atkins, N. Scarinci, R. Cowan, and L. Hickson. 2019. “Promoting Patient-Centered Hearing Care through the Use of eHealth: Current Status and Future Possibilities.” Perspectives of the ASHA Special Interest Groups 4 (2): 331–344. doi:10.1044/2018_PERS-SIG7-2018-0003.
- Muñoz, K., K. Kibbe, E. Preston, A. Caballero, L. Nelson, K. White, and M. Twohig. 2017. “Paediatric Hearing Aid Management: A Demonstration Project for Using Virtual Visits to Enhance Parent Support.” International Journal of Audiology 56 (2): 77–84. doi:10.1080/14992027.2016.1226521.
- Ng, S. L., S. Phelan, M. Leonard, and J. Galster. 2017. “A Qualitative Case Study of Smartphone-Connected Hearing Aids: Influences on Patients, Clinicians, and Patient-Clinician Interactions.” Journal of the American Academy of Audiology 28 (6): 506–521. doi:10.3766/jaaa.15153.
- Novak, R. E., A. Gonzales Cantu, A. Zappler, L. Coco, C. A. Champlin, and J. C. Novak. 2016. “The Future of Healthcare Delivery: IPE/IPP Audiology and Nursing Student/Faculty Collaboration to Deliver Hearing Aids to Vulnerable Adults via Telehealth.” Journal of Nursing & Interprofessional Leadership in Quality & Safety 1 (1): 1–11.
- Ontario Ministry of Children and Youth Services. 2017. “Ontario Infant Hearing Program: A Guidance Document.” 1–34. https://www.uwo.ca/nca/pdfs/clinical_protocols/IHP%20Guidance%20Document_2017.01.pdf
- Penteado, S., R. F. Bento, L. R. Battistella, S. M. Silva, and P. Sooful. 2014. “Use of the Satisfaction with Amplification in Daily Life Questionnaire to Assess Patient Satisfaction following Remote Hearing Aid Adjustments (Telefitting).” JMIR Medical Informatics 2 (2): e18. doi:10.2196/medinform.2769.
- Perez, L., S. D. Scollie, S. T. Moodie, D. Walton, and D. Glista. 2020. “An Exploration of Audiologists’ Readiness to Adopt Connected Hearing Healthcare for Remote Hearing Aid Fitting.” Paper presented at 2020 HRS Graduate Research Conference, February 4.
- Ravi, R.,. D. R. Gunjawate, K. Yerraguntla, and C. Driscoll. 2018. “Knowledge and Perceptions of Teleaudiology among Audiologists: A Systematic Review.” Journal of Audiology & Otology 22 (3): 120–127. doi:10.7874/jao.2017.00353.
- Rosas, S. R., and M. Kane. 2012. “Quality and Rigor of the Concept Mapping Methodology: A Pooled Study Analysis.” Evaluation and Program Planning 35 (2): 236–245. doi:10.1016/j.evalprogplan.2011.10.003.
- Singh, G., M. K. Pichora-Fuller, M. Malkowski, M. Boretzki, and S. Launer. 2014. “A Survey of the Attitudes of Practitioners toward Teleaudiology.” International Journal of Audiology 53 (12): 850–860. doi:10.3109/14992027.2014.921736.
- Speech-Language and Audiology Canada. 2019. “Speech-language Pathologists and Audiologists per 100,000 People in Canada.” Speech-Language & Audiology Canada, Orthophonie et Audiologie Canada. https://www.sac-oac.ca/sites/default/files/resources/SAC-OAC_Stats_Map_Canada_EN.pdf
- Swanepoel, D., and J. W. Hall. 2010. “A Systematic Review of Telehealth Applications in Audiology.” Telemedicine Journal and e-Health: The Official Journal of the American Telemedicine Association 16 (2): 181–200. doi:10.1089/tmj.2009.0111.
- Trochim, W. 1989. “An Introduction to Concept Mapping for Planning and Evaluation.” Evaluation and Program Planning 12 (1): 1–27. doi:10.1016/0149-7189(89)90016-5.
- Trochim, W., and D. McLinden. 2017. “Introduction to a Special Issue on Concept Mapping.” Evaluation and Program Planning 60: 166–175. doi:10.1016/j.evalprogplan.2016.10.006.
- Walker, E. A., L. Holte, M. Spratford, J. Oleson, A. Welhaven, and M. Harrison. 2014. “Timeliness of Service Delivery for Children with Later-Identified Mild-to-Severe Hearing Loss.” American Journal of Audiology 23 (1): 116–128. https://doi.org/10.1044/1059-0889(2013/13-0031). doi:10.1044/1059-0889(2013/13-0031).
- World Health Organization. 2019. “Deafness and Hearing Loss.” World Health Organization. https://www.who.int/news-room/fact-sheets/detail/deafness-and-hearing-loss
- Wutzke, S., N. Roberts, C. Willis, A. Best, A. Wilson, and W. Trochim. 2017. “Setting Strategy for System Change: Using Concept Mapping to Prioritise National Action for Chronic Disease Prevention.” Health Research Policy and Systems 15 (1): 69–13. doi:10.1186/s12961-017-0231-7.

