Abstract
The majority of Afghan asylum seekers and refugees come to Austria from Afghanistan, Iran and Pakistan. While those from Afghanistan faced predominantly war-related traumatic events, those from Iran and Pakistan encountered discriminatory experiences related to the host countries. This vulnerable population’s mental health is further strained by different post-migration stressors in Austria. The purpose of the present study was to explore pre-migration environmental differences and association of different sociodemographic and forced-migration related risk factors to mental health outcomes, and the mediation and moderation effects of post-migration stressors. Data were collected from 305 Afghan participants (155 asylum seekers and 150 refugees) that came from Afghanistan, Iran or Pakistan through nonrandom sampling in Austria. Of the 305 participants, 161 (52.8%) had anxiety, 176 (57.7%) depression, 32 (10.5%) ICD-11 PTSD, and 63 (20.7%) ICD-11 CPTSD. In bivariate analyses, being asylum seeker, being divorced, being Pashtun, and higher number of traumata and stressors in pre-migration and post-migration environments were associated with higher prevalence of mental health problems. Pre-migration traumata and post-migration stressors significantly predicted all mental health outcomes in multiple linear regression analyses. Post-migration stressors significantly meditated and moderated the association between pre-migration traumata and mental health symptoms. The findings support pre-migration traumata’s effects and aggravating role of post-migration stressors in mental health of Afghan asylum seekers and refugees in Austria. Our findings imply the importance of implementing proactive and culturally relevant psychosocial interventions that emphasize prevention of post-migration stressors or mitigating their effects on the mental health.
By the end of 2022, 35.3 million refugees and 5.4 million asylum seekers were forcibly displaced worldwide as a result of persecution, conflict, violence or human rights violations (United Nations High Commissioner for Refugees [UNHCR], Citation2023). Among these, Afghans represent the third-largest refugee population globally, with 5.7 million hosted by 103 countries (UNHCR, Citation2023). The majority of Afghans come to European countries either directly from Afghanistan or from Iran and Pakistan, where they were born and raised or lived for a significant period (Schuster & Majidi, Citation2013). The current political situation in Afghanistan, coupled with restrictions in the first countries of asylum, namely Iran and Pakistan, have prompted new departures, primarily toward Europe (Crawley & Kaytaz, Citation2022).
Afghanistan, being a war-torn and conflict-ridden zone, exposes its people to war-related traumatic and stressful events and their psychological consequences on a daily basis, including terror attacks, armed insurgency, kidnapping, high rate of unemployment, drug issues, corrupt governance, gender violence, and shortages of public services. These factors create a pervasive sense of insecurity and pessimism about the country’s future (The Asia Foundation, Citation2019). On the other hand, more than five million Afghans reside in Iran and Pakistan as refugees or undocumented immigrants (UNHCR, Citation2022). In contrast to Afghans living in Afghanistan, those in Iran and Pakistan are less affected by war-related traumatic events. Rather, their mental health is primarily influenced by the traumatic and stressful experiences related to systematic discrimination in their host countries, such as forced mass deportation, illegal detainment, harassment, and restrictions on basic human rights: limitations in access to health care, education, freedom of movement, employment, and property ownership (Amnesty International, Citation2022; European Union Agency for Asylum, Citation2022; Human Rights Watch, Citation2015; LandInfo, Citation2011).
Both asylum seekers and refugees are people who fled their country or habitat to another country and seek protection from persecution and serious human rights violations. By law, refugees in Austria are entitled to asylum, and upon receiving it, they are granted permanent residence in the country. Asylum seekers, on the other hand, have not yet been legally recognized as refugees and await a decision on their asylum applications (Amnesty International, Citationn.d.). For the purpose of this study, both groups are collectively referred as refugee populations.
The mental health of Afghan asylum seekers as an already traumatized and vulnerable group is challenged in coping with various stressors in the host country: language barriers, social isolation, perceived discrimination, limited employment opportunities, family separation, fear of asylum application rejection, prolonged asylum procedure, mandatory detention, and uncertainty about their future (Li et al., Citation2016). Although some post-migration stressors, such as fear of deportation and employment and traveling restrictions, may be alleviated for Afghan asylum seekers after obtaining refugee status, the other remaining stressors continue to impact their mental health years after resettlement (Bogic et al., Citation2015).
An umbrella review by Turrini et al. (Citation2017) highlighted that depression, anxiety, and post-traumatic stress disorder (PTSD) symptoms are prevalent among asylum seekers and refugees, accounting for up to 40% within these populations. A systematic review focusing on the mental health of Afghan refugee populations resettled in industrialized nations indicated a moderate to high prevalence of anxiety, depression, PTSD, and psychological distress symptoms (Alemi et al., Citation2014).
Research consistently shows that greater exposure to pre-migration traumata and post-migration stressors is associated with anxiety, depression, PTSD, and psychological distress symptoms among refugee populations (e.g., Bogic et al., Citation2015; Cantekin & Gençöz, Citation2017; Porter & Haslam, Citation2005; Schweitzer et al., Citation2011). Moreover, the negative effect of post-migration stressors has been found to be over and above the effect of pre-migration traumata (Porter & Haslam, Citation2005; Schweitzer et al., Citation2011). Post-migration stressors have also been shown to mediate and moderate the effect of pre-migration traumata on the mental health of refugee populations (Chen et al., Citation2017; Dangmann et al., Citation2021).
Existing studies on the mental health symptoms of Afghan refugee populations resettled in developed countries have primarily investigated symptom differences based on sociodemographic variations (e.g., Alemi et al., Citation2015) or compared with refugee populations from other nations (e.g., Gerritsen et al., Citation2006). While these comparisons have provided valuable insights into the mental health challenges faced by Afghan refugee populations, there remains a significant gap in the literature concerning symptom differences based on pre-migration environmental distinctions. Understanding these distinctions is crucial, as the unique trauma exposures and stressors can influence mental health outcomes during resettlement.
The classification and understanding of trauma-related disorders have evolved over time. In 2018, the World Health Organization introduced significant changes to the diagnosis of PTSD in its 11th version of the International Classification of Diseases (ICD-11) and introduced a new category called Complex PTSD (CPTSD; World Health Organization, Citation2018). Unlike PTSD, which is associated with symptoms arising from a single traumatic event, CPTSD acknowledges the cumulative impact of chronic and multiple traumatic experiences. It includes core PTSD symptoms and disturbances in self-organization (DSO) consisting of three symptom clusters: affective dysregulation, disturbed self-concept, and difficulties in interpersonal relationships. The addition of CPTSD as a diagnosis and the awareness of its prevalence among treatment-seeking refugee populations may facilitate recognition of this disorder and provides a more comprehensive diagnostic framework for tailored interventions and support (Silva et al., Citation2021).
The evidence for ICD-11 PTSD and CPTSD among refugee populations is growing and is supported by recent studies (e.g., Silva et al., Citation2021; Vallières et al., Citation2018). While previous research has extensively explored the effects of pre-migration traumata and post-migration stressors on anxiety, depression, PTSD, and psychological distress symptoms of refugee populations, there is a paucity of studies on the symptoms of ICD-11 PTSD and CPTSD. Investigating the interplay between pre-migration traumata and ongoing post-migration stressors experienced by refugee populations might add insights into the complex pathways leading to the development and exacerbation of ICD-11 PTSD and CPTSD symptoms.
Numerous studies have examined the direct effects of post-migration stressors on the mental health of refugee populations, as well as the combined effects of post-migration stressors with pre-migration traumata (e.g., Alemi et al., Citation2014; Cantekin & Gençöz, Citation2017; Gerritsen et al., Citation2006; Gleeson et al., Citation2020; Heeren et al., Citation2014; Silove et al., Citation1997). However, fewer studies have assessed the mediating and moderating effects of post-migration stressors on the association between pre-migration traumata and mental health in refugee populations (e.g., Chen et al., Citation2017; Dangmann et al., Citation2021). Moreover, there is a notable gap in research investigating the mediating and moderating effects of post-migration stressors on ICD-11 PTSD and CPTSD symptomology.
To address these issues, this study aimed (1) to examine forced migration related mental health symptoms among Afghan asylum seekers and refugees residing in Austria considering their differences in: (a) pre-migration environment—Afghanistan, Iran, or Pakistan, (b) residence status—asylum seeker or refugee, and (c) sociodemographics—gender, age, marital status, ethnicity, educational level, and length of residency in Austria; (2) to investigate the relative contributions of traumata and stressors in the pre-migration environment and post-migration settlement to mental health outcomes—anxiety, depression, ICD-11 PTSD and CPTSD, and psychological distress scores; and (3) to assess the mediation and moderation effects of post-migration stressors on the association between pre-migration traumata and mental health symptoms among refugee populations.
Methods
Participants
In this study, the inclusion criteria were set to include individuals who were either asylum seekers or refugees in Austria, identified as Afghan, aged 18 years or older, and came to Austria from Afghanistan, Iran, or Pakistan (with at least 7 years of residence in these countries). Additionally, participants needed to be willing to take part voluntarily in the study and able to communicate in Dari. Data were collected in Austria from Afghan asylum seekers between February 2019 and March 2020 and from Afghan refugees between November 2020 and March 2021.
A total of 305 participants, comprising 155 asylum seekers and 150 refugees, completed the questionnaires. Among them, 202 were male (66.2%) and 103 were female (33.8%). The participants’ age ranged from 18 to 72 years (M = 31.38, SD = 11.05). Asylum seekers had been residing in Austria for a mean duration of 3.88 years (SD = 1.08, range = 1 month–9 years), while refugees had a mean residence of 5.99 years (SD = 2.02, range = 6 months–10 years). Half of the participants came to Austria from Afghanistan (n = 153, 50.1%) and half of the participants came from Iran or Pakistan (n = 143, 46,9% and n = 9, 3.0%, respectively). The majority of participants were either married (n = 151, 49.5%) or never married (n = 133, 43.6%). Regarding education, less than 10 percent of participants (n = 29, 9.5%) had a university degree, 78 participants (25.6%) a high school diploma, while 187 participants (61.3%) did not complete school, never attended school, or received informal education. Eleven participants (3.6%) did not state their level of education. The ethnic distribution showed that the majority of participants were Hazara (n = 135, 43.9%), followed by Tajik (n = 66, 21.6%), Pashtun (n = 26, 8.5%), and Uzbek and other minority groups (n = 78, 23.1%).
Measures
The Hopkins Symptom Checklist-25 (HSCL-25; Mollica et al., Citation1987) is a commonly used symptom inventory to measure symptoms of anxiety and depression and is suited for the refugee populations. It consists of 25 items in two parts: part I has 10 items for anxiety symptoms and part II has 15 items for depression symptoms. A cutoff point of ≥1.75 indicates clinically significant distress and is widely accepted in refugee settings and in cross-cultural research (Mollica et al., Citation2004). The Dari version of HSCL-25 has been validated and widely used in studies of Afghan asylum seekers and refugees (e.g., Brea Larios et al., Citation2023; Gerritsen et al., Citation2006; Jakobsen et al., Citation2011). The internal consistencies of anxiety and depression subscales of the Dari version for this study were very good (α = .88 and α = .91, respectively).
The International Trauma Questionnaire (ITQ; Cloitre et al., Citation2018) is an 18 question self-report measure focusing on the core features of PTSD and CPTSD introduced in ICD-11. The ITQ is designed for screening and can discriminate PTSD from CPTSD by employing validated diagnostic rules. The scale has two major subscales with three symptom clusters and two items in each: PTSD and disturbances in self-organization (DSO). In addition, there are three functional impairment items (social, occupational, and other important areas of life) for each of the PTSD and the DSO clusters. PTSD requires the endorsement of at least one symptom in each PTSD cluster, plus endorsement of at least one indicator of functional impairment associated with these symptoms. CPTSD requires additionally endorsement of at least one symptom in each DSO cluster and at least one indicator of functional impairment associated with the DSO cluster. A Dari version of the ITQ used in this study, which its statistical validity has been shown in a recent study (Andisha et al., Citation2023). In the current study, the internal consistency of the PTSD and DSO items were good (α = .83 and α = .88, respectively), and for the total scale was excellent (α = .90).
The Afghan Symptom Checklist (ASCL) is a culturally grounded assessment measure of psychological distress symptoms developed by Miller et al. (Citation2006). The ASCL consists of 23 items, and contains indigenous items known to Afghans (e.g., asabi—a state of nervous agitation; jigar khun—a state of extreme and persistent dysphoria; and fishar-e-payin—a state of low energy and motivation) and items familiar to Western mental health professionals (e.g., crying, insomnia, social withdrawal, headache). Total scores range from 23 to 115, with higher scores indicative of higher distress levels. The ASCL demonstrated excellent internal consistency in this study (α = .93).
The Pre-and-post-migration traumatic and stressful events scale was specifically designed for this study to enlist and screen traumatic and stressful events experienced by Afghan participants in their lifetime. It consists of two sections: pre-migration and post-migration. The pre-migration section consists of 31 items: 21 traumatic events and 10 stressful events. The scoring consists the total number of events that happened to the participants in their lifetime before or in the way of migration to their current settlement. The scale covered war-related events relevant to Afghans who lived in Afghanistan, as well as discriminatory experiences faced by Afghans residing in Iran and Pakistan. The post-migration section consists of 15 items: two traumatic events and 13 stressful events. The participants in this section select the level that each item is currently a challenge for them with a five-point Likert scale, ranging from 0 (not at all) to 4 (extremely). Items with scores ≥2 (moderately) are considered as potential challenge.
The trauma events section of the Harvard Trauma Questionnaire (Mollica et al., Citation1992) and the Post-migration Living Difficulty Checklist (Steel et al., Citation1999) are widely used screening measures in refugee population studies. However, these measures did not encompass those traumatic and stressful experiences that were related to the sociocultural and environmental differences of this study population. Initially, a semi-structured interview was designed containing all items from the two above mentioned measures. Ten Afghan asylum seekers (five males and five females) and three experts were selected through non-probability sampling and interviewed in order to elicit a contextually relevant screening measure specifically for this population. They were asked if they have experienced any of the events in the list or have seen or heard that other Afghans have experienced. Furthermore, they were asked if they have experienced, witnessed or heard any other events that were traumatic or stressful and were not in the list.
Consequently, irrelevant items were removed or converted to more relevant form (e.g., “poor access to health care services” to “not knowing to use health services”) and more relevant items were added (e.g., forced marriage, family violence, and fear that calls are under surveillance).
Procedure
A pilot test was conducted with 30 Afghan asylum seekers in Vienna to assess feasibility and refine the measures prior to the launch of the main research study. For instance, during this stage, it was observed that participants were less suspicious and more cooperative in completing the interview when demographic information was asked at the end of questionnaire.
For the main study, a cross-sectional quantitative survey was conducted across Austria, targeting Afghan asylum seekers and refugees residing in asylum shelters or private residences. Due to strict data protection regulations for the refugee population, accessing databases to identify participants was not feasible. Instead, known providers of accommodation and assistance to asylum seekers were identified through online search, and their approval was sought for data collection from Afghan asylum seekers in their residences. Furthermore, an association providing integration, cultural, and sporting activities to Afghans in Austria, assisted the data collection from Afghan refugees. Afghan refugees interested in participating in the study were identified through social media advertisements, distribution of flyers, and by enlisting the help of influential informal leaders within the Afghan communities.
The interviews were exclusively administered by the first author, an Afghan refugee and a native Dari speaker, providing cultural and linguistic advantages that eliminated language barriers and fostered increased trust and cooperation of participants. Before the interviews, participants were informed about the nature and purpose of the study, their rights, anonymity, and confidentiality, and they were provided with a study participation information brochure. They voluntarily participated in the study and only after signing the informed consent form. No incentives were offered for participation. The participants could either self-administer the questionnaire or be interviewed if they preferred. Due to the coinciding COVID-19 pandemic restrictions, data from refugees were collected solely through self-administration. The Afghan association distributed the questionnaires to interested participants, and the first author collected them later to ensure the data protection and verify that the questionnaires were correctly and completely filled.
Ethical considerations also addressed participants’ distress during the interview. They were informed that some questions might evoke memories of stressful or traumatic events, and they were given the option to skip or reschedule those questions. If distress was reported, immediate support was provided, and participants were referred to mental health service providers, if necessary. Participants were also given a brochure in Dari containing essential information on coping with negative emotional states and seeking professional psychological help, including a list of organizations offering free mental health services to asylum seekers and refugees.
Analysis
All statistical analyses were carried out using the IBM SPSS statistics version 24.0. In the data collection process, only the completed questionnaires were included. Hence, there were very few missing data (0.0–3.6%) across variables and were managed using the default pairwise exclusion method in the analyses. Descriptive statistics were generated for all variables and mental health symptoms. Chi-square tests were used to compare different groups based on their experiences of pre-migration and post-migration risk factors and the prevalence of mental health problems.
Independent samples t-tests, analysis of variance, and Pearson correlations were applied to identify significant associations with the mean scores of mental health measurements at the bivariate level. Multiple linear regression analysis was subsequently conducted to examine the predictive relationship between the independent variables (significant at the bivariate level) and the mental health outcomes - anxiety, depression, ICD-11 PTSD and CPTSD, and psychological distress. The PROCESS macro for SPSS developed by Hayes (Citation2018) was utilized to test the potentially mediating and moderating effects of post-migration stressors on the association between pre-migration traumata and mental health symptoms.
To assure that the sample size was sufficiently large to detect statistical significance in the presence of actual differences, a post hoc power analysis was performed using G*Power software, version 3.1 (Faul et al., Citation2007). With a sample size of 305 participants, a moderate effect size, and type I error of α = .05, the power (1 − β err prob) in this study ranged from 0.952 to 0.999, indicating that the data had enough statistical power.
Results
Pre-migration traumata and stressors
Nearly all participants reported being exposed to one or more traumatic (95.1%) and stressful (94.8%) events in their pre-migration environments or during their journey to Austria. presents the percentages and the chi-square test results of reported pre-migration traumata and stressors. On average, participants experienced 8.47 traumatic events (SD = 4.72) and 5.36 stressful events (SD = 2.83). Afghans from Afghanistan reported a significantly higher number of traumatic events (M = 9.46, SD = 4.68), compared to Afghans from Iran or Pakistan (M = 7.47, SD = 4.56), t(303) = 3.76, p < .001. Afghans from Iran or Pakistan reported a significantly higher number of pre-migration stressful events (M = 5.86, SD = 2.84), compared to Afghans from Afghanistan (M = 4.88, SD = 2.74), t(303) = −3.07, p < .01. Moreover, a higher percentage of Afghans from Afghanistan reported a low sense of safety in their residence before coming to Austria compared to Afghans from Iran or Pakistan (70.6% vs. 52.6%). However, both groups had an equally low sense of certainty about their future (62.1% vs. 61.2%). Additionally, asylum seekers experienced a significantly higher number of pre-migration traumatic events (M = 9.42, SD = 4.14), compared to refugees (M = 7.49, SD = 5.08), t(287.16) = 3.62, p < .001.
Table 1. Frequencies of reported pre-migration traumata and stressors.
Post-migration traumata and stressors
Ninety-seven percent of the participants reported experiencing one or more stressful events in Austria. presents the percentages and the chi-square test results of reported post-migration traumata and stressors. On average, participants experienced 0.20 traumatic events (SD = 0.48) and 7.33 stressful events (SD = 3.51). There were no significant differences in the number of traumatic experiences between Afghans from Afghanistan (M = 0.18, SD = 0.43) and Afghans from Iran or Pakistan (M = 0.23, SD = 0.52), t(292.08) = −0.98, p = .33, while also observing no significant differences in the number of stressful experiences between Afghans from Afghanistan (M = 7.24, SD = 3.35) and Afghans from Iran or Pakistan (M = 7.42, SD = 3.67), t(303) = −0.45, p = .66. Asylum seekers experienced a significantly higher number of post-migration traumatic events (M = 0.26, SD = 0.54), compared to refugees (M = 0.14, SD = 0.40), t(285.47) = 2.30, p < .05. Similarly, asylum seekers experienced a significantly higher number of stressful events (M = 8.95, SD = 2.55), compared to refugees (M = 5.65, SD = 3.59), t(268.29) = 9.24, p < .001.
Table 2. Frequencies of reported post-migration traumata and stressors.
Descriptive analyses of mental health problems
presents the percentages and the chi-square test results of diagnostic estimates. Asylum seekers showed significantly higher diagnostic rates of anxiety, depression, and ICD-11 PTSD than refugees. There were no differences between Afghans from Afghanistan and Afghans from Iran or Pakistan in all diagnoses. The mean total score on the ASCL for asylum seekers (M = 49.43, SD = 17.84) was significantly higher than refugees (M = 43.87, SD = 16.25), t(303) = 2.84, p < .01, indicating a markedly higher level of self-reported distress. Mean total scores on the ASCL for Afghans from Afghanistan (M = 46.91, SD = 17.14) did not differ from Afghans from Iran or Pakistan (M = 46.49, SD = 17.46), t(303) = 0.21, p = .83.
Table 3. Prevalence rates of anxiety, depression, and ICD-11 related posttraumatic symptoms.
Prediction of mental health outcomes
Factors correlated to mental health problems
reports bivariate relationships between different sociodemographic and sociocultural characteristics (categorical variables) and the mean scores of anxiety, depression, ICD-11 PTSD and CPTSD, and psychological distress (dependent variables). Asylum seekers showed significantly higher levels of symptoms on all dependent variables at the p < .01 level—anxiety (t[297] = 3.479), depression (t[303] = 2.945), ICD-11 PTSD (t[303] = 4.316), ICD-11 CPTSD (t[303] = 2.910), and psychological distress (t[303] = 2.842). Participants who reported being divorced scored significantly higher than other marital groups for depression (F[4, 300] = 3.415, p < .01) and ICD-11 CPTSD (F[4, 300] = 2.415, p < .05). Participants who identified as Pashtun scored significantly higher than other ethnic groups for depression (F[3, 301] = 4.753, p < .01) and psychological distress (F[3, 301] = 2.826, p < .05).
Table 4. Categorical variables and dependent variables (mental health problems) measured at bivariate level using independent samples T-tests and analysis of variance.
reports bivariate relationships between pre-migration and post-migration traumata and stressors, age, and length of residency in Austria (continuous variables), and the mean scores of anxiety, depression, ICD-11 PTSD and CPTSD, and psychological distress (dependent variables). Pearson correlations revealed moderate to strong positive and significant relationships between the pre-migration traumata and post-migration stressors and all dependent variables, indicating higher mental health symptoms in individuals with a higher number of experienced traumatic events in their pre-migration environments and post-migration stressful events in their new settlements. Pre-migration stressors and post-migration traumata had significant but weak relationships with the dependent variables.
Table 5. Contiguous variables and dependent variables (mental health problems) measured at bivariate level using Pearson correlation coefficient.
Factors predicting mental health outcomes
To ensure meaningful interpretations, categorical variables were dummy-coded. The residence status (asylum seekers = 0), marital status (divorced = 0), and ethnicity (Pashtun = 0) variables were coded and compared with their reference groups (coded 1) that would serve as useful comparisons (Cohen et al., Citation2002). Separate sets of multiple linear regression analyses were conducted for each mental health outcomes to reveal the predictors. The variables that showed significant bivariate relationships at p < .05 level were entered into the regression models to assess if they significantly contributed to the overall models.
The summary of regression models for each of the mental health outcomes is given in . Being an asylum seeker did not predict any mental health outcomes in the regression models. However, being divorced was predictive of a higher level of depression, and identifying as Pashtun was predictive of a higher level of depression. Pre-migration traumata and post-migration stressors were highly and significantly predictive of the mental health outcomes in all models. Moreover, post-migration traumata were predictive of higher levels of depression and psychological distress at p < .05 level.
Table 6. Multiple linear regression analysis of variables predicting mental health outcomes.
Mediation and moderation effects of post-migration stressors
The potentially mediating and moderating effects of post-migration stressors on the association between pre-migration traumata and mental health symptoms were assessed using bootstrapping procedures with 5000 bootstrap samples.
The results revealed a significant indirect effect of pre-migration traumata on all studied mental health symptoms—anxiety (B = 0.206, t = 4.910), depression (B = 0.289, t = 4.757), ICD-11 PTSD (B = 0.240, t = 4.906), ICD-11 CPTSD (B = 0.500, t = 5.112), and psychological distress (B = 0.404, t = 4.288). Furthermore, the direct effect of pre-migration traumata on all mental health symptoms in the presence of the mediator was also found significant—anxiety (B = 0.360, p < .001), depression (B = 0.547, p < .001), ICD-11 PTSD (B = 0.573, p < .001), ICD-11 CPTSD (B = 1.007, p < .001), and psychological distress (B = 1.374, p < .001). The direction for direct and indirect effects was the same, suggesting that post-migration stressors complimentarily and partially mediated the relationship between pre-migration traumata and mental health symptoms. A summary of the mediation analysis is presented in .
Table 7. Mediation analysis summary.
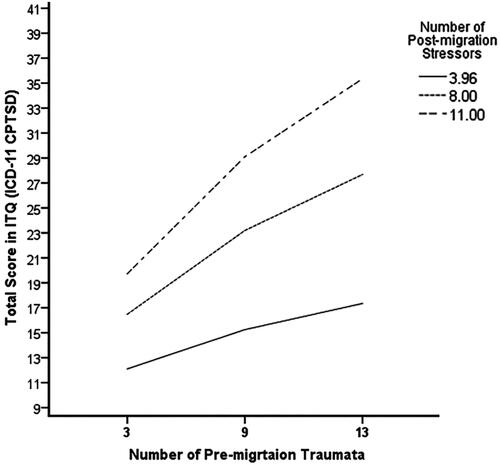
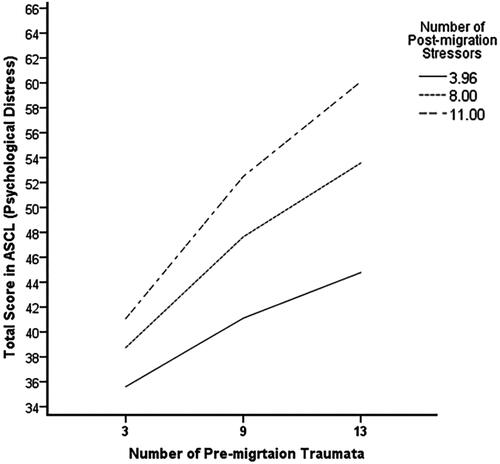
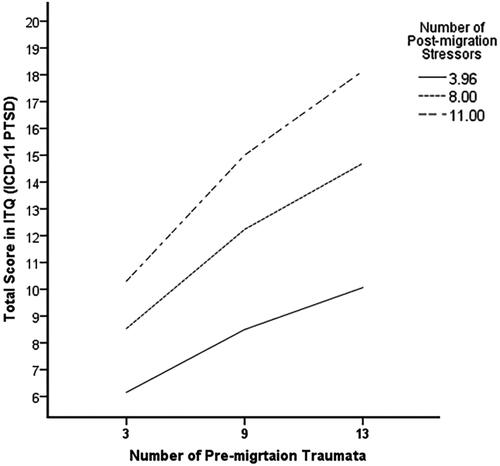
The interaction terms between post-migration stressors and pre-migration traumata showed significant moderating effects for all mental health symptoms. The results revealed a positive and significant moderating impact of post-migration stressors on the relationship between pre-migration traumata and all mental health symptoms—anxiety (B = 0.053, t = 2.547, p < .05), depression (B = 0.085, t = 2.886, p < .01), ICD-11 PTSD (B = 0.056, t = 2.181, p < .05), ICD-11 CPTSD (B = 0.147, t = 3.246, p < .01), and psychological distress (B = 0.140, t = 2.850, p < .01). present the results in slope graphs to provide a better visualization of the conditional effect of pre-migration stressors.
Figure 1. Moderation effect of post-migration stressors on the association between pre-migration traumata and anxiety symptoms. N = 305. Values for the post-migration stressors are the 16th, 50th, and 84th percentiles.
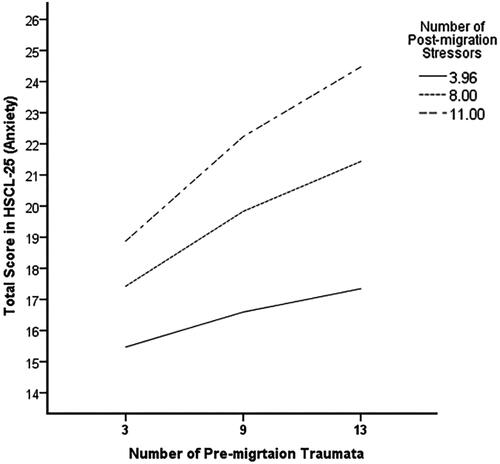
Figure 2. Moderation effect of post-migration stressors on the association between pre-migration traumata and depression symptoms. N = 305. Values for the post-migration stressors are the 16th, 50th, and 84th percentiles.
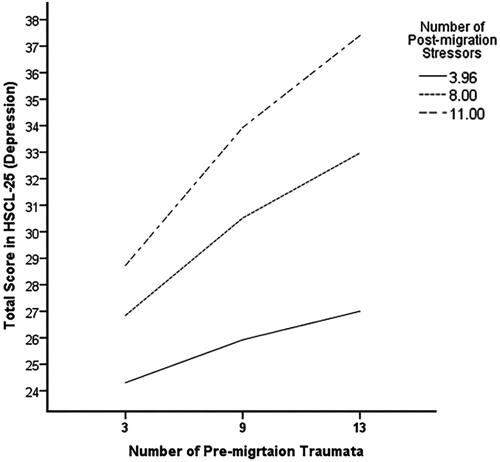
Figure 3. Moderation effect of post-migration stressors on the association between pre-migration traumata and ICD-11 PTSD symptoms. N = 305. Values for the post-migration stressors are the 16th, 50th, and 84th percentiles.
Discussion
This study aimed to investigate the mental health outcomes of Afghan asylum seekers and refugees residing in Austria, considering their differences in pre-migration environment, residence status, and various sociodemographic factors. Additionally, we explored the contributions of pre-migration traumata and post-migration settlement stressors to mental health outcomes and assessed the mediating and moderating effects of post-migration stressors.
The majority of participants experienced one or more stressful and traumatic events in their pre-migration environments and in Austria. Afghans from Afghanistan reported higher numbers of pre-migration traumatic experiences, mainly war-related, while Afghans from Iran or Pakistan reported higher numbers of pre-migration stressful experiences, mainly discriminatory experiences related to their host countries. However, both groups reported similar levels of traumatic and stressful experiences in Austria. Asylum seekers reported higher numbers of pre-migration traumatic experiences compared to refugees, and they also reported higher numbers of traumatic and stressful experiences in their post-migration settlement. This result aligns with our expectations and is consistent with previous studies (e.g., Gerritsen et al., Citation2006; Heeren et al., Citation2014).
We expected that variations in pre-migration traumatic and stressful experiences of Afghan refugee populations due to their differing pre-migration environments would influence their post-migration resettlement stressors and their mental health status. However, despite differing pre-migration experiences, we found no significant differences in post-migration stressors and mental health symptom levels between Afghan refugee populations coming from Afghanistan and those coming from Iran and Pakistan. The similar experiences of post-migration stressors could be partially explained by the fact that all Afghan refugee populations coming to Austria are identified by their nationality and are treated as a homogenous group. Consequently, they face common stressors related to resettlement, such as language barriers, cultural adjustments, economic challenges, and social isolation. These shared stressors may contribute to the converging levels of traumatic and stressful experiences in the host country, potentially leading to similar mental health outcomes across the groups.
The results of this study indicate alarmingly high level of mental health symptoms in Afghan asylum seekers and refugees, which appear to be more prevalent than in the general population. According to data from a systematic review of published evidence in Austria (Łaszewska et al., Citation2018), prevalence rates in the general population are 6.5% for anxiety disorders and 9–15% for depression. As ICD-11 PTSD and CPTSD are relatively new diagnostic categories of trauma-related disorders, studies are still emerging, and estimates vary based on diagnostic criteria and the studied population. A study by McGinty et al. (Citation2021) analyzing general population samples from four developed countries (United States of America, Israel, Republic of Ireland, and United Kingdom) estimated prevalence rates of ICD-11 PTSD at 3.4–6.7% and ICD-11 CPTSD at 3.9–12.9%. Despite the higher rates of ICD-11 PTSD (10.5%) and CPTSD (20.7%) in this study population, they are relatively lower than those reported in treatment-seeking Afghan asylum seekers and refugees in Austria (Schiess-Jokanovic et al., Citation2022: 17.78% for ICD-11 PTSD and 50% for ICD-11 CPTSD).
Compared to refugees, asylum seekers showed significantly higher prevalence rates of mental health symptoms with the exception of the ICD-11 CPTSD. This result is consistent with findings from previous studies comparing asylum seekers and refugees (e.g., Gerritsen et al., Citation2006; Heeren et al., Citation2014). Previous research comparing CPTSD symptomology between asylum seekers and refugees is lacking. A plausible explanation for the lack of difference could be the severity and persistence of traumata experienced by participants reporting CPTSD symptoms, which may contribute to its chronic nature. Mental health symptoms among refugee populations can endure for years, even in the absence of further trauma exposure (Bogic et al., Citation2015).
Treatment of CPTSD in refugee populations can be challenging due to its novelty as a diagnosis and limited research on its prevalence and treatment in this context. The absence of significant differences in this study does not diminish the significance of CPTSD as a mental health concern for both asylum seekers and refugees. Instead, it highlights the intricacy of CPTSD in these populations, calling for further research to explore the contributing factors leading to this symptomatology.
In bivariate analyses, gender, age, educational level, and length of residency in Austria were not associated with any of the studied mental health problems. This finding is consistent with a systematic literature review by Bogic et al. (Citation2015) that assessed different correlating factors with the long-term mental health of refugee populations. The majority of their reviewed studies reported no association between demographic factors and mental disorders. Similarly, their findings on the relationship between duration in exile and mental disorders suggested no significant association. Being an asylum seeker, being divorced, belonging to Pashtun ethnicity, and having a higher number of traumatic and stressful experiences in pre-migration and post-migration environments were associated with mental health problems.
Strong initial associations were found between residence status (being an asylum seeker) and mental health problems. However, after controlling for pre-migration and post-migration traumata and stressors, residence status was no longer associated with mental health issues, confirming patterns observed in a systematic review of previous relevant studies (Gleeson et al., Citation2020). Consistent with previous research in refugee populations, pre-migration traumata and post-migration stressors were consistently significant predictors for mental health outcomes, with the later demonstrating a greater adverse effect (e.g., Cantekin & Gençöz, Citation2017; Porter & Haslam, Citation2005; Schweitzer et al., Citation2011).
Furthermore, the findings showed significant mediation and moderation impacts of post-migration stressors on the relationship between pre-migration traumata and mental health symptoms. These stressors not only had stronger negative direct effects on the mental health of Afghan asylum seekers and refugees but also aggravated the negative effects of pre-migration traumata. This finding emphasizes the significant role of ongoing post-migration stressors on the mental health of refugee populations and is consistent with recent studies (Chen et al., Citation2017; Dangmann et al., Citation2021).
Several limitations to this study should be acknowledged. First, data collection was based on nonrandom sampling procedures, limiting generalizability. Second, the comprehension of questionnaire items between asylum seekers and refugees may have varied as due to COVID-19 pandemic regulations and restrictions—most refugees completed the questionnaires through self-administration, in contrast to asylum seekers of whom the majorities were interviewed. Additionally, some residences denied access to asylum seekers for interviews, leading to potential exclusion of participants and affecting the sample’s representativeness.
The developed pre-and-post-migration traumatic and stressful events scale in this study was an effort to improve upon existing checklists used in previous refugee population studies to quantify experienced traumata and stressors, and to elicit a contextually relevant screening for the Afghan refugee population. The scale was used to encompass the total number of lifetime events before and after migration. However, this approach may not fully capture the complexity and impact of events, potentially leading to overestimation, underestimation, or overlap of experiences reported by participants. For instance, witnessing a family member’s murder with a gun might be indicated as multiple traumatic events, resulting in overestimation. Conversely, some participants may have experienced one event multiple times, leading to underestimation. Additionally, the severity and nature of an experience can play a crucial role in determining its effect. Repeated instances of severe trauma, such as sexual violence or torture, can lead to more profound and enduring psychological consequences than less severe events, such as being robbed or witnessing single acts of violence.
Despite the aforementioned limitations, this study provides a valuable insight into the mental health challenges faced by Afghan refugee populations. It represents a pioneering effort in exploring the effects of the pre-migration environmental differences on the mental health of the Afghan refugee populations. Additionally, examining the manifestation of ICD-11 PTSD and CPTSD symptomology in Afghan asylum seekers and refugees adds to the growing body of evidence on these recently introduced trauma-related disorders, which is a relatively unexplored area in the context of forced migration. Moreover, the study investigated the mediation and moderation effects of post-migration stressors. The study used a comprehensive list of culturally grounded and validated measures and checklists, which were adapted to the refugee populations and were culturally sensitive in diagnosing the mental health symptoms of the Afghan population. Furthermore, interviews conducted by an Afghan refugee and native Dari speaker, helped to eliminate language barriers and increased trust and cooperation of participants. Consequently, it is plausible to suggest that these culturally sensitive approaches could have positively influenced the overall data collection quality, providing a robust foundation for assessing the unique mental health challenges experienced by Afghan refugee populations.
Future studies should refine previously used screening scales in refugee populations, specifically by focusing on identifying salient events with multiple ties to listed items and taking into account their independence and severity. A more focused approach is needed to differentiate the impact of pre-migration traumatic and stressful experiences specific to each group of Afghan refugee populations. One possible solution is to select participants who have lived exclusively in one of the pre-migration environments (Afghanistan, Iran, or Pakistan) to avoid potential overlap in experiences. Longitudinal studies initiated early in the migration process would be beneficial for differentiating the influential role of post-migration stressors on the mental health of asylum seekers and refugees. Additionally, investigating the effect of post-migration stressors on ICD-11 PTSD and CPTSD can provide deeper insights into these understudied mental health symptoms.
Although interventions to address pre-migration traumatic exposures of Afghan refugee populations are largely reactive and not easily amenable, proactive and culturally relevant interventions can be implemented upon resettlement to address post-migration stressors. Psychosocial interventions tailored to the living situations and specific sociocultural differences and needs of refugee populations might be particularly beneficial (Knefel et al., Citation2022). Additionally, interventions that promote social connectedness, such as community-based interventions, can contribute to improving the mental health of Afghan asylum seekers and refugees (Schiess-Jokanovic et al., Citation2022).
Conclusion
The findings of this study support the effects of pre-migration traumata and aggravating role of post-migration stressors affecting the mental health of Afghan asylum seekers and refugees in Austria. It is important to implement proactive and culturally relevant psychosocial interventions that emphasize prevention of post-migration stressors or mitigating their effects on the mental health.
Ethics approval
This study received ethics approval from the Ethics Committee of the University of Vienna (reference number: 00279, dated 29 November 2017).
Open Scholarship

This article has earned the Center for Open Science badges for Open Materials. The materials are openly accessible at https://osf.io/ach2x/?view_only=f8a3b54596b245d5abef57b81170f831.
Acknowledgments
The authors would like to thank all the participants for their participation and the association of Katib Kultur Sport Verein for their support in the data collection process.
Data availability statement
The data are not publicly available owing to the vulnerability of the participants and for their data protection to ensure public safety.
Additional information
Funding
Notes on contributors
Pouya Andisha
Pouya Andisha is a doctoral candidate in Department of Clinical and Health Psychology, Faculty of Psychology at University of Vienna. His research project is the contextual study of forced migration related mental health issues of Afghan refugee population in Austria. He is particularly interested in assessment of refugee population's trauma-related disorders and examining mental health risk and protective factors.
Brigitte Lueger-Schuster
Brigitte Lueger-Schuster is a Professor in Department of Clinical and Health Psychology, Faculty of Psychology at University of Vienna, and also leads the unit of Psychotraumatology. She is the Past President of the European Society for Traumatic Stress Studies (ESTSS). Her research interests focus on abuse in institutions, psychosocial consequences of traumatic stress, coping strategies, resilience, complex trauma, complex PTSD, assessment of trauma-related disorders, and human rights violations.
References
- Alemi, Q., James, S., Cruz, R., Zepeda, V., & Racadio, M. (2014). Psychological distress in Afghan refugees: A mixed-method systematic review. Journal of Immigrant and Minority Health, 16(6), 1247–1261. https://doi.org/10.1007/s10903-013-9861-1
- Alemi, Q., James, S., Siddiq, H., & Montgomery, S. (2015). Correlates and predictors of psychological distress among Afghan refugees in San Diego County. International Journal of Culture and Mental Health, 8(3), 274–288. https://doi.org/10.1080/17542863.2015.1006647
- Amnesty International. (n.d.). Refugees, asylum-seekers and migrants. https://www.amnesty.org/en/what-we-do/refugees-asylum-seekers-and-migrants/
- Amnesty International. (2022). End violence and serious human rights violations against Afghan refugees. https://www.amnesty.org/en/latest/news/2022/06/end-violence-and-serious-human-rights-violations-against-afghan-refugees/
- Andisha, P., Shahab, M. J., & Lueger-Schuster, B. (2023). Translation and validation of the Dari International Trauma Questionnaire (ITQ) in Afghan asylum seekers and refugees. European Journal of Psychotraumatology, 14(1), 2158428. https://doi.org/10.1080/20008066.2022.2158428
- Bogic, M., Njoku, A., & Priebe, S. (2015). Long-term mental health of war-refugees: A systematic literature review. BMC International Health and Human Rights, 15(1), 29. https://doi.org/10.1186/s12914-015-0064-9
- Brea Larios, D., Sam, D. L., & Sandal, G. M. (2023). Psychological distress among Afghan refugees in Norway as a function of their integration. Frontiers in Psychology, 14, 1143681. https://doi.org/10.3389/fpsyg.2023.1143681
- Cantekin, D., & Gençöz, T. (2017). Mental health of Syrian asylum seekers in Turkey: The role of pre-migration and post-migration risk factors. Journal of Social and Clinical Psychology, 36(10), 835–859. https://doi.org/10.1521/jscp.2017.36.10.835
- Chen, W., Hall, B. J., Ling, L., & Renzaho, A. M. N. (2017). Pre-migration and post-migration factors associated with mental health in humanitarian migrants in Australia and the moderation effect of post-migration stressors: Findings from the first wave data of the BNLA cohort study. The Lancet. Psychiatry, 4(3), 218–229. https://doi.org/10.1016/S2215-0366(17)30032-9
- Cloitre, M., Shevlin, M., Brewin, C. R., Bisson, J. I., Roberts, N. P., Maercker, A., Karatzias, T., & Hyland, P. (2018). The International Trauma Questionnaire: Development of a self-report measure of ICD-11 PTSD and complex PTSD. Acta Psychiatrica Scandinavica, 138(6), 536–546. https://doi.org/10.1111/acps.12956
- Cohen, J., Cohen, P., West, S. G., & Aiken, L. S. (2002). Applied multiple regression/correlation analysis for the behavioral sciences (3rd ed.). Routledge. https://doi.org/10.4324/9780203774441
- Crawley, H., & Kaytaz, E. S. (2022). Between a rock and a hard place: Afghan migration to Europe from Iran. Social Inclusion, 10(3), 4–14. https://doi.org/10.17645/si.v10i3.5234
- Dangmann, C., Solberg, Ø., & Andersen, P. N. (2021). Health-related quality of life in refugee youth and the mediating role of mental distress and post-migration stressors. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 30(8), 2287–2297. https://doi.org/10.1007/s11136-021-02811-7
- European Union Agency for Asylum. (2022). Iran - situation of Afghan refugees. https://doi.org/10.2847/181551
- Faul, F., Erdfelder, E., Lang, A., & Buchner, A. (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39(2), 175–191. https://doi.org/10.3758/BF03193146
- Gerritsen, A. A. M., Bramsen, I., Devillé, W., van Willigen, L. H. M., Hovens, J. E., & van der Ploeg, H. M. (2006). Physical and mental health of Afghan, Iranian and Somali asylum seekers and refugees living in the Netherlands. Social Psychiatry and Psychiatric Epidemiology, 41(1), 18–26. https://doi.org/10.1007/s00127-005-0003-5
- Gleeson, C., Frost, R., Sherwood, L., Shevlin, M., Hyland, P., Halpin, R., Murphy, J., & Silove, D. (2020). Post-migration factors and mental health outcomes in asylum-seeking and refugee populations: A systematic review. European Journal of Psychotraumatology, 11(1), 1793567. https://doi.org/10.1080/20008198.2020.1793567
- Hayes, A. F. (2018). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach (2nd ed.). The Guilford Press. https://www.guilford.com/books/Introduction-to-Mediation-Moderation-and-Conditional-Process-Analysis/Andrew-Hayes/9781462549030
- Heeren, M., Wittmann, L., Ehlert, U., Schnyder, U., Maier, T., & Müller, J. (2014). Psychopathology and resident status - Comparing asylum seekers, refugees, illegal migrants, labor migrants, and residents. Comprehensive Psychiatry, 55(4), 818–825. https://doi.org/10.1016/j.comppsych.2014.02.003
- Human Rights Watch. (2015). “What are you doing here?”: Police abuses against Afghans in Pakistan. https://www.hrw.org/report/2015/11/18/what-are-you-doing-here/police-abuses-against-afghans-pakistan
- Jakobsen, M., Thoresen, S., & Johansen, L. E. E. (2011). The validity of screening for post-traumatic stress disorder and other mental health problems among asylum seekers from different countries. Journal of Refugee Studies, 24(1), 171–186. https://doi.org/10.1093/jrs/feq053
- Knefel, M., Kantor, V., Weindl, D., Schiess-Jokanovic, J., Nicholson, A. A., Verginer, L., Schäfer, I., & Lueger-Schuster, B. (2022). Mental health professionals’ perspective on a brief transdiagnostic psychological intervention for Afghan asylum seekers and refugees. European Journal of Psychotraumatology, 13(1), 2068913. https://doi.org/10.1080/20008198.2022.2068913
- LandInfo. (2011). Afghan citizens in Iran. Oslo. https://landinfo.no/asset/2063/1/2063_1.pdf
- Łaszewska, A., Österle, A., Wancata, J., & Simon, J. (2018). Prevalence of mental diseases in Austria: Systematic review of the published evidence. Wiener Klinische Wochenschrift, 130(3-4), 141–150. https://doi.org/10.1007/s00508-018-1316-1
- Li, S. S. Y., Liddell, B. J., & Nickerson, A. (2016). The relationship between post-migration stress and psychological disorders in refugees and asylum seekers. Current Psychiatry Reports, 18(9), 82. https://doi.org/10.1007/s11920-016-0723-0
- McGinty, G., Fox, R., Ben-Ezra, M., Cloitre, M., Karatzias, T., Shevlin, M., & Hyland, P. (2021). Sex and age differences in ICD-11 PTSD and complex PTSD: An analysis of four general population samples. European Psychiatry: The Journal of the Association of European Psychiatrists, 64(1), e66. https://doi.org/10.1192/j.eurpsy.2021.2239
- Miller, K. E., Omidian, P., Quraishy, A. S., Quraishy, N., Nasiry, M. N., Nasiry, S., Karyar, N. M., & Yaqubi, A. A. (2006). The Afghan Symptom Checklist: A culturally grounded approach to mental health assessment in a conflict zone. The American Journal of Orthopsychiatry, 76(4), 423–433. https://doi.org/10.1037/0002-9432.76.4.423
- Mollica, R. F., Cardozo, B. L., Osofsky, H. J., Raphael, B., Ager, A., & Salama, P. (2004). Mental health in complex emergencies. Lancet, 364(9450), 2058–2067. https://doi.org/10.1016/S0140-6736(04)17519-3
- Mollica, R. F., Caspi-Yavin, Y., Bollini, P., Truong, T., Tor, S., & Lavelle, J. (1992). The Harvard Trauma Questionnaire: Validating a cross-cultural instrument for measuring torture, trauma, and posttraumatic stress disorder in Indochinese refugees. The Journal of Nervous and Mental Disease, 180(2), 111–116. https://doi.org/10.1097/00005053-199202000-00008
- Mollica, R. F., Wyshak, G., Marneffe, D. d., Khuon, F., & Lavelle, J. (1987). Indochinese versions of the Hopkins Symptom Checklist-25: A screening instrument for the psychiatric care of refugees. The American Journal of Psychiatry, 144(4), 497–500. https://doi.org/10.1176/ajp.144.4.497
- Porter, M., & Haslam, N. (2005). Predisplacement and postdisplacement factors associated with mental health of refugees and internally displaced persons: A meta-analysis. JAMA, 294(5), 602–612. https://doi.org/10.1001/jama.294.5.602
- Schiess-Jokanovic, J., Knefel, M., Kantor, V., Weindl, D., Schäfer, I., & Lueger-Schuster, B. (2022). The boundaries between complex posttraumatic stress disorder symptom clusters and post-migration living difficulties in traumatised Afghan refugees: A network analysis. Conflict and Health, 16(1), 19. https://doi.org/10.1186/s13031-022-00455-z
- Schuster, L., & Majidi, N. (2013). What happens post-deportation? The experience of deported Afghans. Migration Studies, 1(2), 221–240. https://doi.org/10.1093/migration/mns011
- Schweitzer, R. D., Brough, M., Vromans, L., & Asic-Kobe, M. (2011). Mental health of newly arrived Burmese refugees in Australia: Contributions of pre-migration and post-migration experience. The Australian and New Zealand Journal of Psychiatry, 45(4), 299–307. https://doi.org/10.3109/00048674.2010.543412
- Silove, D., Sinnerbrink, I., Field, A., Manicavasagar, V., & Steel, Z. (1997). Anxiety, depression and PTSD in asylum-seekers: Associations with pre-migration trauma and post-migration stressors. The British Journal of Psychiatry: The Journal of Mental Science, 170(4), 351–357. https://doi.org/10.1192/bjp.170.4.351
- Silva, U. d., Glover, N., & Katona, C. (2021). Prevalence of complex post-traumatic stress disorder in refugees and asylum seekers: Systematic review. BJPsych Open, 7(6), e194. https://doi.org/10.1192/bjo.2021.1013
- Steel, Z., Silove, D., Bird, K., McGorry, P., & Mohan, P. (1999). Pathways from war trauma to posttraumatic stress symptoms among Tamil asylum seekers, refugees, and immigrants. Journal of Traumatic Stress, 12(3), 421–435. https://doi.org/10.1023/A:1024710902534
- The Asia Foundation. (2019). Afghanistan in 2019: A survey of the Afghan people. https://reliefweb.int/sites/reliefweb.int/files/resources/2019_Afghan_Survey_Full-Report.pdf
- Turrini, G., Purgato, M., Ballette, F., Nosè, M., Ostuzzi, G., & Barbui, C. (2017). Common mental disorders in asylum seekers and refugees: Umbrella review of prevalence and intervention studies. International Journal of Mental Health Systems, 11(1), 51. https://doi.org/10.1186/s13033-017-0156-0
- United Nations High Commissioner for Refugees. (2022). Afghanistan situation regional response plan (RRP) January - December 2022. https://reporting.unhcr.org/afghansituation
- United Nations High Commissioner for Refugees. (2023). Global trends: Forced displacement in 2022. https://www.unhcr.org/global-trends-report-2022
- Vallières, F., Ceannt, R., Daccache, F., Abou Daher, R., Sleiman, J., Gilmore, B., Byrne, S., Shevlin, M., Murphy, J., & Hyland, P. (2018). ICD-11 PTSD and complex PTSD amongst Syrian refugees in Lebanon: The factor structure and the clinical utility of the International Trauma Questionnaire. Acta Psychiatrica Scandinavica, 138(6), 547–557. https://doi.org/10.1111/acps.12973
- World Health Organization. (2018). International Classification of Diseases for mortality and morbidity statistics (11th ed.). https://icd.who.int/browse11/l-m/en