Abstract
Introduction
In the past decade, the number of deliberate self-poisonings involving young people has increased strongly worldwide. This study aimed to gain insight into risk factors associated with deliberate self-poisonings among children and adolescents reported to the Dutch Poisons Information Center.
Methods
A study was performed between 1 February 2022 and 31 January 2023 involving those aged 8–17 years of age with deliberate self-poisoning. Data were collected on patient characteristics (age, gender, body mass index and living situation) and exposure characteristics (type of toxicant, way of acquiring toxicant and day of exposure).
Results
The Dutch Poisons Information Center was consulted about 1,424 deliberate self-poisonings among children and adolescents (10–17 years old). A high percentage of patients were female (85 percent), had a body mass index classified as overweight/obese (27 percent) and lived in a mental healthcare facility (13 percent). Patients mainly exposed themselves to pharmaceuticals, especially over-the-counter medications such as paracetamol (46 percent) and ibuprofen (15 percent). Young people living with parents/caregivers had higher odds of ingesting prescription pharmaceuticals or over-the-counter medication, while those living in a mental healthcare facility were more likely to ingest household products, personal care products or foreign bodies (predominantly batteries).
Discussion
This study sheds light on the pervasive issue of deliberate self-poisoning among children and adolescents, advocating for poisoning prevention strategies and promoting mental health of youth. Limitations include reliance on self-reported data from patients and the absence of clinical outcome data.
Conclusions
Female gender, a high body mass index and living in a mental healthcare facility are associated with in increased risk of deliberate self-poisonings in children and adolescents (10-17 years old). Prevention of deliberate self-poisonings among youth could focus on restricting access to medication and other potentially hazardous non-pharmaceuticals, such as household products and batteries, as well as limiting the sales of over-the-counter medication, especially paracetamol, to this young population.
Introduction
Self-harm rates among adolescents increased significantly all over the world in recent years [Citation1]. Worldwide, approximately one in six adolescents participate in self-harm behavior [Citation1], and suicide was the fourth leading cause of death among 15- to 19-year-olds from 2000 to 2019 [Citation2]. Approximately, 20% of all adolescent self-harm episodes involved deliberate self-poisonings [Citation1], and these often lead to emergency department presentations and hospital admissions [Citation3,Citation4].
In the past decade, countries such as the United States (US), the United Kingdom, Australia and Canada reported substantial increases in deliberate self-poisonings among children and adolescents [Citation5–8]. For example, in the US, self-poisoning suicide attempts among 10- to 18-year-old children and adolescents increased by 94% from 2010 to 2018. For females, 10–15 years of age, this increase was even higher at 151% [Citation5].
The COVID-19 pandemic has had a considerable impact on the mental health of children and adolescents. We recently showed that the number of deliberate self-poisonings among 13- to 17-year-old adolescents reported to the Dutch Poisons Information Center significantly increased by 45% from 2020 to 2021 (i.e., the second year of the COVID-19 pandemic). This increase was most prominent among 13- to 15-year-old girls [Citation9]. In France, they observed a similar increase in the number of deliberate self-poisonings among 12- to 24-year-olds starting in the second half of 2020, especially among females [Citation10]. Similarly, in the US, the number of deliberate self-poisonings among children and adolescents of 10–19 years of age increased by 30% in 2021 compared to pre-pandemic rates in 2019. This increase was greatest among females and adolescents of 10–15 years of age [Citation11]. Additionally, US poison center data showed that exposures with suicidal intent among adolescents during the first 1.5 years of the COVID-19 pandemic caused moderate/major health effects more frequently and had a higher mortality compared to pre-pandemic years [Citation12].
Patient-specific risk factors for deliberate self-poisonings in childhood and adolescence have not been studied extensively. Nonetheless, several potential risk factors for deliberate self-poisoning in adolescence have been proposed, including female gender [Citation5,Citation13–16], pre-existing psychiatric disorders [Citation17–19], school days [Citation9,Citation13,Citation20], school calendar [Citation13,Citation14,Citation20], poor school performance, stress, not living with both parents (for males), recurring drunkenness, daily smoking [Citation21] and the urbanization level of the patient’s residence [Citation14].
To further understand the phenomenon of deliberate self-poisoning among young people, we characterized deliberate self-poisonings among children and adolescents from 1 February 2022 up to and including 31 January 2023 on the following aspects: age, gender, body mass index, involved toxicant(s) (and method of acquisition), living situation and day of exposure. The aim of the study was to identify risk factors for deliberate self-poisonings in this age group in order to suggest preventive strategies to protect this young population.
Materials and methods
Study design and patient population
The current study was an observational study analyzing inquiries to the Dutch Poisons Information Center about deliberate self-poisonings among children and adolescents from 1 February 2022 to 31 January 2023. Inquiries involving children and adolescents (from 8 to 17 years of age inclusive) who exposed themselves to substances with the (suspected) intent of self-harm were included. Criteria for exclusion were age <8 years, unintentional exposures (e.g., medication errors) and intentional non-deliberate self-poisonings (i.e., recreational use of illicit drugs or alcohol, nonmedical use of medication (outside the realm of deliberate self-poisoning, e.g., performance enhancement) and as a consequence of peer pressure). Cases were assessed against the inclusion and exclusion criteria by three authors, and any disagreements were resolved through consensus.
For the purpose of this study, specialists in poison information recorded additional information during telephone inquiries to the Dutch Poisons Information Center that met the aforementioned inclusion criteria. This information concerned the patient’s height, living situation and additional information about the exposure. The living situation was either classified as living at home with parents or caregivers, or a living situation with additional mental healthcare (e.g., psychiatric facility, assisted living, and group home) or other (e.g., foster care, family replacement home, refugee center, juvenile detention center, care farm or other). In the case of ingestion of medication, enquiries were made as to whether the medication was prescribed to the patient. For non-prescribed medicines, it was asked how the patient obtained this medication (e.g., freely available at home, someone else’s medication or purchased at a drug store). Multiple inquiries to the Dutch Poisons Information Center regarding the same patient and same exposure(s) were analyzed as a single case. Additional relevant information, such as gender identity, was also noted.
The Dutch Medical Research Involving Human Subjects Act did not apply to this study. Therefore, no explicit consent from the patients was required.
Statistical analysis
Descriptive statistics were used to summarize patient demographics (e.g., age, gender, body mass index, and living situation), exposure characteristics (e.g., type of toxicant, way of acquiring toxicant and day of exposure) and treatment advice. All categorical data were first assessed using frequencies and percentages. Subsequently, Chi-square (χ2) tests were performed, followed by the determination of odds ratios to assess the presence and strength of any associations.
The median number of deliberate self-poisonings per weekday (Monday to Friday) and during the weekend (Saturday and Sunday) was calculated, after which a Mann–Whitney U-test was performed to compare both types of days. Similarly, the median ingested doses of paracetamol (acetaminophen) and ibuprofen were calculated for children and adolescents living at home with parents/caregivers and those living in a mental healthcare facility, after which a Mann–Whitney U-test was performed to compare both types of living conditions.
Statistical analyses were conducted using R (version 4.0.3) (R Foundation for Statistical Computing, Vienna, Austria) and IBM SPSS Statistics (Version 26; IBM, Armonk, NY).
Dutch Poisons Information Center procedures and definitions
The Dutch Poisons Information Center provides a 24/7 information service, which can be consulted by healthcare professionals for information on the diagnosis and management of acute poisonings, serving the entire Dutch population of 17.6 million. During an inquiry, data are collected in a standardized manner about patient and exposure characteristics, intention, clinical symptoms at the time of the inquiry, and treatment advice. The clinical outcome of the poisoning is unknown in most cases since follow-up of cases is not a standard procedure.
For every patient with known weight and height, the body mass index was calculated by dividing weight (kg) by the square of height (m2). Using the gender- and age-specific cut-off points for body mass index in childhood developed by the International Obesity Task Force, body mass index was subdivided into three groups: (1) underweight (thinness grade 2), (2) normal weight and (3) overweight and obesity [Citation22,Citation23]. For each age, the mean reference of that age was used as a cut-off point.
Pharmaceutical exposures were subdivided into different pharmaceutical classes based on their Anatomical Therapeutic Chemical code. Non-pharmaceutical products were subdivided into categories based on the Dutch Poisons Information Center classification system (household products, personal care products, drugs and legal stimulants (such as alcohol and tobacco), plants, foods and herbs, foreign bodies, disinfectants and other products) (Supplementary Table 1).
The Dutch Poisons Information Center performs a risk assessment based on the reported exposure dose (mg/kg body weight), the time passed since exposure and current symptoms. This results in one of the following treatment advice options (based on a pure medical toxicological point of view): (a) observation at home/mental healthcare facility (when estimated to be no or a mild intoxication) or (b) further medical examination by a physician, followed by hospital observation if necessary (when estimated to be a potentially moderate/severe intoxication). In case of unreliable or unclear history with respect to the ingested dose, the diagnostic and treatment approach defaults to the worst-case scenario for managing the patient. Observation in a hospital or a psychiatric facility could also be warranted because of psychiatric reasons. However, in the Netherlands, that decision is up to the patient’s physician (e.g., general practitioner or emergency physician) and not the Dutch Poisons Information Center.
Results
Patient characteristics
In total, the Dutch Poisons Information Center received 32,415 inquiries on acute human intoxications between 1 February 2022 and 31 January 2023. Of these, 3,029 involved children and adolescents from 8 to 17 years of age, of which 1,424 were included as child and adolescent deliberate self-poisoning (). No patients under the age of ten were included since none of these exposures were identified as deliberate self-poisoning. The median age was 15 (interquartile range: 14–16) years. Of all unintentional exposures among children and adolescents of 8 through 17 years of age from 2016 up until 2022, the average percentage of calls about males was 47%, for females 43%, and for the remaining cases, the gender was unknown. Of all deliberate self-poisoning cases in this age group, the majority of patients were female (85%, n = 1206) (). Our study population consisted of a relatively high percentage of children and adolescents who identify as transgender (2%, n = 23).
Figure 1. Patient selection flow-chart, covering all inclusions from 1 February 2022 until 31 January 2023.
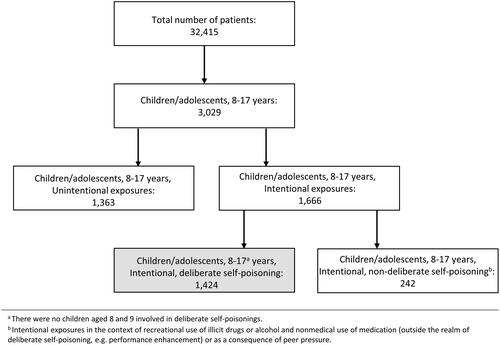
Table 1. Patient characteristics of deliberate self-poisonings among children and adolescents reported to the Dutch Poisons Information Center.
Body mass index could be calculated for 54% of patients (n = 776). The median body mass index was 21.0 (interquartile range: 18.9–24.2). Body mass index was classified as underweight in 2% (n = 15), healthy weight in 71% (n = 552) and overweight or obese in 27% (n = 209) of patients. In 2022, the percentage of overweight or obese children and adolescents (12- up to and including 17-year-olds) in the general Dutch population was 14.6% [Citation24], indicating that our study population contained a numerically higher percentage of overweight or obese young people.
Of all children and adolescents of 10–17 years of age, 64% were living with parents or caregivers (n = 913), 13% lived in a mental healthcare facility (n = 187), and 5% lived in a group home or assisted living facility (n = 72). For 3%, the living situation was categorized as "other" (n = 45), including foster care, refugee center, juvenile detention center, etc. For 15%, the living situation was unknown (n = 207) (). For comparison, the percentage of children and adolescents (12- up to and including 17-year-olds) in the general Dutch population living in a mental healthcare facility or group home/assisted living facility in 2022 was 0.1% and 1%, respectively [Citation25,Citation26], showing that children living in a mental healthcare facility or group home/assisted living facility were numerically over-represented in our study.
Exposure characteristics
During deliberate self-poisonings, children and adolescents more frequently exposed themselves to a single substance (72%, n = 1,028) than to multiple substances (28%, n = 396). Patients ingested over-the-counter medicines/freely available supplements in 61% of the cases (n = 867) and prescription pharmaceuticals in 38% (n = 540).
For those exposed to prescription pharmaceuticals (n = 540), this was prescribed to the patient in 63% of cases (n = 338), while in 22% someone else’s medication was used (n = 119) and in 18% of cases the source of the medicine was unknown (n = 99). Note that the total percentage exceeds 100 because a single patient might ingest more than one type of medicine. Over-the-counter medicines and freely available supplements (n = 867) were often present at home or a mental healthcare residence (26%, n = 227) or were bought by the patient (10%, n = 84). However, in the majority of cases, it was unknown how the patient acquired the medication (64%, n = 557).
A smaller percentage of patients was exposed to non-pharmaceutical products, including household products (5%, n = 65) such as bleach or detergents, personal care products (2%, n = 28), nail polish remover or shampoo, disinfectants (1%, n = 12) or foreign bodies (1%, n = 12), predominantly batteries (n = 10) (Supplementary Table 1).
Exposure type related to living situation
Children and adolescents living in a mental healthcare facility had higher odds of using household products (χ2, P < 0.001; odds ratio = 4.151, 95% confidence interval [2.292, 7.518]) or personal care products (χ2, P < 0.001; odds ratio = 6.747; 95% confidence interval [2.912, 15.631]) in deliberate self-poisonings than children and adolescents living at home with parents or caregivers. Those living in a mental healthcare facility were more likely to ingest foreign bodies (n = 8), as no cases were reported for children and adolescents living at home with parents or caregivers. In contrast, children and adolescents living with parents or caregivers had higher odds of using prescription medications (χ2, P < 0.001; odds ratio = 2.165; 95% confidence interval [1.506, 3.112]) and over-the-counter medication (χ2, P = 0.012; odds ratio = 1.436; 95% confidence interval [1.047, 1.970]) in deliberate self-poisonings compared to children and adolescents living in a mental healthcare facility ().
Table 2. Top 10 substances used in deliberate self-poisoning among children and adolescents living at home with parents/caregivers and children and adolescents living in a mental healthcare facility.
Treatment advice
Observation at home (n = 647) and medical evaluation by a physician/hospital observation (n = 777) were recommended for 45% and 55% of the patients, respectively. There was no significant difference in the treatment advice given to children and adolescents living in a mental healthcare facility and those living with parents or caregivers (χ2, P = 0.133).
For the three most frequently used pharmaceuticals, i.e., paracetamol, ibuprofen and methylphenidate, the body weight-corrected doses in mg/kg were determined if body weight and reported ingested dose were known. The median dose for paracetamol, ibuprofen and methylphenidate was 140.0 mg/kg (interquartile range: 87.8–200.0; n = 602), 70.2 mg/kg (interquartile range: 43.6–123.1; n = 196) and 2.9 mg/kg (interquartile range: 1.6–4.8; n = 73), respectively. Dose threshold values used by our poison center to determine whether an intake requires further medical assessment or observation are 150 mg/kg for paracetamol, 200 mg/kg for ibuprofen and 3 mg/kg for methylphenidate. Therefore, based on the self-reported ingested dose and patients’ weight, a substantial number of patients who ingested paracetamol or methylphenidate were advised to be referred to a hospital for treatment (Supplementary Figure 1).
Regarding paracetamol exposures, children and adolescents living in a mental healthcare facility ingested a significantly higher dose (median = 175.8 mg/kg; interquartile range: 124.0–260.6; n = 56) compared to those living at home with parents/caregivers (median = 136.7 mg/kg; interquartile range: 86.3–191.9; n = 434, P = 0.002). For ibuprofen, the difference in dose ingested was not significantly different for the two living conditions (P = 0.209).
Weekdays versus weekend
The exact day of exposure was known for 88.2% of deliberate self-poisonings (n = 1,256). The average number of deliberate self-poisonings per day was significantly higher from Monday to Friday (median = 3; interquartile range: 2–5) compared to the weekend (median = 2; interquartile range: 1–4; P < 0.001).
Discussion
Our study showed that in children and adolescents aged between 10 and 17 years, female gender, a high body mass index and living in a mental healthcare facility are associated with an increased risk of deliberate self-poisoning. The high prevalence of female deliberate self-poisonings is in accordance with studies from other Western countries [Citation5–8]. In contrast, unintentional exposures in this age group affected males more than females by a ratio of 1.11:1. The disproportionate representation of females in deliberate self-poisonings may be associated with the severe mental health deterioration that has been reported especially among females of 11- to 16-years-old in the Netherlands between 2017 and 2021 [Citation27]. Another remarkable finding was that a considerable percentage of our study population identified as transgender (2%). This overrepresentation might be explained by the increased risk of adolescent suicide attempts and self-harm among sexual minorities [Citation28,Citation29]. Children and adolescents who are overweight/obese were also overrepresented in this study in comparison to the general population. This may be related to the association found between obesity and depression [Citation30], as depression is a risk factor for self-poisoning behavior [Citation17–19].
Multiple studies have suggested that deliberate self-poisonings correlate with schooldays, with fewer self-poisoning attempts during the weekend compared to the weekdays [Citation9,Citation13,Citation20,Citation31]. This study shows a similar trend. School-related factors, such as bullying or pressure to perform, could possibly explain this finding, as the risk of self-harm is considerably higher when an adolescent is a victim or a perpetrator of bullying [Citation32,Citation33].
In our study, children and adolescents mainly exposed themselves to pharmaceuticals, with over-the-counter medication most commonly involved. Paracetamol and ibuprofen were involved in more than half of the cases. Nearly half of the patients who ingested paracetamol took a dose that could potentially cause severe liver damage. This shows the relatively high doses that are often ingested by children and adolescents and the potential severity of these deliberate self-poisonings. Future studies could consider looking into the health consequences of these deliberate self-poisonings, as in this study outcome data were not available.
Living in a mental healthcare facility was linked to a higher risk of deliberate self-poisoning compared to the general Dutch population in our study. This can be explained by the fact that young people living in mental healthcare facilities often exhibit psychiatric or behavioral problems. Furthermore, children living in a mental healthcare facility had higher odds of being exposed to household products, personal care products and foreign bodies (mostly batteries) compared to children and adolescents living at home with parents/caregivers. In contrast, children and adolescents who lived with parents/caregivers had higher odds of exposure to pharmaceuticals and over-the-counter medication compared to children and adolescents living in a mental healthcare facility. This may be related to greater awareness of the safe storage of medicines in mental healthcare facilities compared to private households, and, as a consequence, a shift towards household products involved in deliberate self-poisonings. Therefore, safe storage of pharmaceuticals, but also of household and personal care products, should be promoted, which could be achieved by educating parents and healthcare workers about the potential danger of certain substances.
Due to the high number of paracetamol poisonings in Western society, multiple European countries such as France, the United Kingdom and Switzerland, have prohibited the sales of paracetamol and/or restricted the packaging size of paracetamol at pharmacy and non-pharmacy outlets. An international survey across European poison centers revealed that packaging size restrictions were not effective in lowering the number of paracetamol-related inquiries [Citation34]. In contrast, countries that limited the sales of paracetamol at non-pharmacy outlets did report a lower number of inquiries about paracetamol poisonings [Citation34]. Additionally, prohibiting the sales of paracetamol to children and adolescents below 18 years of age resulted in a 17% reduction in admissions of young people (10–17 years) with paracetamol poisoning in Denmark [Citation35]. Therefore, limiting the sales of paracetamol at non-pharmacy outlets and restricting the sales of paracetamol to children and adolescents up to the age of 18 may be effective preventive measures to reduce the number of deliberate self-poisonings with paracetamol in children and adolescents in the Netherlands.
Lastly, easy access to mental healthcare and early identification, assessment and treatment of children and adolescents with mental health problems is of utmost importance to prevent deliberate self-poisonings. Educating parents/caregivers, teachers and medical professionals to detect warning signals of suicidal behavior could be of great value.
This study has some important limitations. Consultation of the Dutch Poisons Information Center for acute intoxications is not mandatory, so not every deliberate self-poisoning is reported to the Dutch Poisons Information Center. It is likely that the Dutch Poisons Information Center is more likely to be consulted about more severe or rare exposures, and less severe poisonings or those with a well-known treatment protocol (such as paracetamol) may be underreported. Additionally, all inquiries are based on self-reporting by patients to medical responders and are therefore prone to bias and error. There may also be a reporting bias, with certain institutions more likely to make enquiries, or with certain patient information more available for specific patient groups. Exposures are generally not analytically confirmed. Due to anonymous data collection, one individual may have been included several times in case of repeated self-poisonings. The Dutch Poisons Information Center does not routinely perform follow-up; therefore, no outcome data are available for these poisonings. Finally, for a small subset of exposures (approximately 3%), the true intent of the patient was not clearly stated. In these cases, inclusion was based on the dose ingested and exposure scenario.
Conclusions
In this study female gender, a high body mass index and living in a mental healthcare facility are all associated with an increased risk of deliberate self-poisoning among children and adolescents. Measures to prevent future deliberate self-poisoning among children and adolescents should include educating parents and healthcare workers, restricting access to medication and potentially harmful non-pharmaceuticals and limiting the sales of over-the-counter medication.
Supplemental Material
Download Zip (518.7 KB)Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Gillies D, Christou MA, Dixon AC, et al. Prevalence and characteristics of self-harm in adolescents: meta-analyses of community-based studies 1990–2015. J Am Acad Child Adolesc Psychiatry. 2018;57(10):733–741. doi: 10.1016/j.jaac.2018.06.018.
- World Health Organization. Suicide worldwide in 2019: global health estimates. Geneva: World Health Organization; 2021.
- Okumura Y, Shimizu S, Ishikawa KB, et al. Comparison of emergency hospital admissions for drug poisoning and major diseases: a retrospective observational study using a nationwide administrative discharge database. BMJ Open. 2012;2(6):e001857. doi: 10.1136/bmjopen-2012-001857.
- Diggins E, Kelley R, Cottrell D, et al. Age-related differences in self-harm presentations and subsequent management of adolescents and young adults at the emergency department. J Affect Disord. 2017;208:399–405. doi: 10.1016/j.jad.2016.10.014.
- Spiller HA, Ackerman JP, Spiller NE, et al. Sex- and age-specific increases in suicide attempts by self-poisoning in the United States among youth and young adults from 2000 to 2018. J Pediatr. 2019;210:201–208. doi: 10.1016/j.jpeds.2019.02.045.
- Cairns R, Karanges EA, Wong A, et al. Trends in self-poisoning and psychotropic drug use in people aged 5–19 years: a population-based retrospective cohort study in Australia. BMJ Open. 2019;9(2):e026001. doi: 10.1136/bmjopen-2018-026001.
- Gilley M, Sivilotti MLA, Juurlink DN, et al. Trends of intentional drug overdose among youth: a population-based cohort study. Clin Toxicol. 2020;58(7):711–715. doi: 10.1080/15563650.2019.1687900.
- Thomas E, Cooper GA, Vale JA. Intentional overdoses and self-harm enquiries in adolescents aged 8–16 years: a retrospective review of enquiries to the national poisons information service in the UK. XXXV International Congress of the European Association of Poisons Centres and Clinical Toxicologists (EAPCCT) 26–29 May 2015, St Julian’s, Malta. Clin Toxicol. 2015;53:244–245.
- Koppen A, Thoonen IMJ, Hunault CC, et al. Significant increase in deliberate self-poisonings among adolescents during the second year of the COVID-19 pandemic. J Adolesc Health. 2023;73(2):319–324. doi: 10.1016/j.jadohealth.2023.02.041.
- Jollant F, Blanc-Brisset I, Cellier M, et al. Temporal trends in calls for suicide attempts to poison control centers in France during the COVID-19 pandemic: a nationwide study. Eur J Epidemiol. 2022;37(9):901–913. doi: 10.1007/s10654-022-00907-z.
- Farah R, Rege SV, Cole RJ, et al. Suspected suicide attempts by self-poisoning among persons aged 10–19 years during the COVID-19 pandemic – United States, 2020–2022. MMWR Morb Mortal Wkly Rep. 2023;72(16):426–430. doi: 10.15585/mmwr.mm7216a3.
- Wang GS, Leonard J, Cornell A, et al. Adolescent US Poison Center exposure calls during the COVID-19 pandemic. J Adolesc Health. 2022;71(6):764–767. doi: 10.1016/j.jadohealth.2022.07.014.
- Froberg BA, Morton SJ, Mowry JB, et al. Temporal and geospatial trends of adolescent intentional overdoses with suspected suicidal intent reported to a state poison control center. Clin Toxicol. 2019;57(9):798–805. doi: 10.1080/15563650.2018.1554186.
- Spiller HA, Ackerman JP, Smith GA, et al. Suicide attempts by self-poisoning in the United States among 10–25 year olds from 2000 to 2018: substances used, temporal changes and demographics. Clin Toxicol. 2020;58(7):676–687. doi: 10.1080/15563650.2019.1665182.
- Overall B, Hon SL, Jones A, et al. Intentional suspected suicide exposures by poisoning among adolescents from 2009 to 2018 reported to the Georgia Poison Center and compared nationally. Basic Clin Pharmacol Toxicol. 2021;128(5):699–708. doi: 10.1111/bcpt.13563.
- Daly C, Griffin E, McMahon E, et al. Paracetamol-related intentional drug overdose among young people: a national registry study of characteristics, incidence and trends, 2007–2018. Soc Psychiatry Psychiatr Epidemiol. 2021;56(5):773–781. doi: 10.1007/s00127-020-01981-y.
- Lifshitz M, Gavrilov V. Deliberate self-poisoning in adolescents. Isr Med Assoc J. 2002;4(4):252–254.
- Fadum EA, Stanley B, Qin P, et al. Self-poisoning with medications in adolescents: a national register study of hospital admissions and readmissions. Gen Hosp Psychiatry. 2014;36(6):709–715. doi: 10.1016/j.genhosppsych.2014.09.004.
- Tay EY, Tan GF, Yeo AWC, et al. Intentional poisoning in pediatric patients: examining the risk factors. Pediatr Emerg Care. 2021;37(12):e1510–e1514. doi: 10.1097/PEC.0000000000002101.
- Chitty KM, Raubenheimer J, Cairns R, et al. Deliberate self-poisoning in Australian adolescents is increased on school days. J Psychiatr Res. 2022;148:103–109. doi: 10.1016/j.jpsychires.2022.01.045.
- Kivistö JE, Rimpelä A, Mattila VM. Adolescent risk factors for poisonings – a prospective cohort study. Acta Paediatr. 2011;100(12):1596–1602. doi: 10.1111/j.1651-2227.2011.02387.x.
- Cole TJ, Bellizzi MC, Flegal KM, et al. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320(7244):1240–1243. doi: 10.1136/bmj.320.7244.1240.
- Cole TJ, Flegal KM, Nicholls D, et al. Body mass index cut offs to define thinness in children and adolescents: international survey. BMJ. 2007;335(7612):194. doi: 10.1136/bmj.39238.399444.55.
- CBS. Leefstijl; persoonskenmerken. Netherlands: The Central Bureau of Statistics; 2023 [cited 2023 Jun 22]. Available from: https://www.vzinfo.nl/overgewicht/leeftijd-en-geslacht-jongeren
- CBS. Jongeren. Netherlands: The Central Bureau of Statistics; 2023 [cited 2023 Jun 22]. Available from: https://www.cbs.nl/nl-nl/visualisaties/dashboard-bevolking/leeftijd/jongeren
- CBS. Jongeren met jeugdzorg; persoonskenmerken. Netherlands: The Central Bureau of Statistics; 2023 [cited 2023 Jun 22]. Available from: https://opendata.cbs.nl/#/CBS/nl/dataset/85100NED/table
- Stevens GWJM, Van Dorsselaer S, Boer M, et al. HBSC 2017. Gezondheid en welzijn van jongeren in Nederland. Utrecht (Netherlands): Utrecht University; 2018.
- O'Reilly LM, Pettersson E, Donahue K, et al. Sexual orientation and adolescent suicide attempt and self-harm: a co-twin control study. J Child Psychol Psychiatry. 2021;62(7):834–841. doi: 10.1111/jcpp.13325.
- James SE, Herman J, Keisling M, et al. 2015 U.S. Transgender Survey (USTS). Inter-University Consortium for Political and Social Research [distributor]. Ann Arbor (MI): University of Michigan; 2019.
- Mannan M, Mamun A, Doi S, et al. Prospective associations between depression and obesity for adolescent males and females – a systematic review and meta-analysis of longitudinal studies. PLOS One. 2016;11(6):e0157240. doi: 10.1371/journal.pone.0157240.
- Beauchamp GA, Ho ML, Yin S. Variation in suicide occurrence by day and during major American holidays. J Emerg Med. 2014;46(6):776–781. doi: 10.1016/j.jemermed.2013.09.023.
- Heerde JA, Hemphill SA. Are bullying perpetration and victimization associated with adolescent deliberate self-harm? A meta-analysis. Arch Suicide Res. 2019;23(3):353–381. doi: 10.1080/13811118.2018.1472690.
- Myklestad I, Straiton M. The relationship between self-harm and bullying behaviour: results from a population based study of adolescents. BMC Public Health. 2021;21(1):524. doi: 10.1186/s12889-021-10555-9.
- Morthorst BR, Erlangsen A, Nordentoft M, et al. Availability of paracetamol sold over the counter in Europe: a descriptive cross-sectional international survey of pack size restriction. Basic Clin Pharmacol Toxicol. 2018;122(6):643–649. doi: 10.1111/bcpt.12959.
- Morthorst BR, Erlangsen A, Chaine M, et al. Restriction of non-opioid analgesics sold over-the-counter in Denmark: a national study of impact on poisonings. J Affect Disord. 2020;268:61–68. doi: 10.1016/j.jad.2020.02.043.

