ABSTRACT
Background: The COVID-19 pandemic caused multiple stressors that may lead to symptoms of adjustment disorder.
Objective: We longitudinally examined relationships between risk and protective factors, pandemic-related stressors and symptoms of adjustment disorder during the COVID-19 pandemic, as well as whether these relationships differed by the time of assessment.
Method: The European Society for Traumatic Stress Studies (ESTSS) ADJUST Study included N = 15,169 participants aged 18 years and above. Participants from 11 European countries were recruited and screened three times at 6-month intervals from June 2020 to January 2022. Associations between risk and protective factors (e.g. gender), stressors (e.g. fear of infection), and symptoms of adjustment disorder (AjD, ADNM-8) and their interaction with time of assessment were examined using mixed linear regression.
Results: The following predictors were significantly associated with higher AjD symptom levels: female or diverse gender; older age; pandemic-related news consumption >30 min a day; a current or previous mental health disorder; trauma exposure before or during the pandemic; a good, satisfactory or poor health status (vs. very good); burden related to governmental crisis management and communication; fear of infection; restricted social contact; work-related problems; restricted activity; and difficult housing conditions. The following predictors were associated with lower AjD levels: self-employment or retirement; working in healthcare; and face-to-face contact ≥ once a week with loved ones or friends. The effects of the following predictors on AjD symptoms differed by the time of assessment in the course of the pandemic: a current or previous mental disorder; burden related to governmental crisis management; income reduction; and a current trauma exposure.
Conclusions: We identified risk factors and stressors predicting AjD symptom levels at different stages of the pandemic. For some predictors, the effects on mental health may change at different stages of a pandemic.
HIGHLIGHTS
We longitudinally examined predictors of symptoms of adjustment disorder in 15,563 adults during the COVID-19 pandemic.
We found stressors, risk, and protective factors predicting adjustment disorder symptom levels at different stages of the pandemic.
For some predictors, the effects appear to change in different phases of a pandemic.
Antecedentes: La pandemia por COVID-19 fue causa de múltiples factores estresantes que puedan haber condicionado un trastorno de adaptación.
Objetivo: Se evaluó de forma longitudinal la relación entre factores protectores y factores de riesgo, factores estresantes asociados a la pandemia y síntomas del trastorno de adaptación durante la pandemia por COVID-19. Además, se evaluó si estas relaciones variaban según la temporalidad de la evaluación.
Métodos: El estudio ADJUST de la Sociedad Europea para el Estudio de Estrés Traumático incluyó a N = 15.169 participantes de 18 años o más. Se reclutó a participantes de 11 países europeos y fueron evaluados tres veces en intervalos de 6 meses desde junio del 2020 hasta enero del 2022. Las asociaciones entre los factores protectores (e. g. género) y de riesgo, los factores estresantes (e. g. miedo a contagiarse), los síntomas del trastorno de adaptación (AjD por sus siglas en inglés; empleando el Cuestionario para el Trastorno de Adaptación – Nuevo Módulo 8 o ADNM-8 por sus siglas en inglés) y sus interacciones según la temporalidad de la evaluación fueron analizados mediante una regresión linear mixta.
Resultados: Se asociaron con niveles significativamente mayores de síntomas del AjD los siguientes: género femenino o diverso; edad avanzada; consumo de noticias relacionadas con la pandemia mayor a 30 minutos al día; trastorno mental actual o previo; exposición a trauma antes o durante la pandemia; estado de salud bueno, satisfactorio o pobre (en comparación con uno muy bueno); carga asociada al manejo y comunicación gubernamentales de la crisis; miedo a infectarse; contacto social restringido; problemas laborales; actividad restringida; y dificultades asociadas a la vivienda. Se asociaron con menores niveles de síntomas del AjD los predictores siguientes: trabajo autónomo o condición de jubilado; trabajo en el sector salud; contacto en persona más de una vez por semana con amigos o seres queridos. Los efectos sobre los niveles de los síntomas del AjD que cambiaron según la temporalidad de la evaluación durante la pandemia fueron los siguientes: Trastorno mental actual o previo; carga relacionada con el manejo gubernamental de la crisis; reducción de ingresos; exposición actual al trauma.
Conclusiones: Se identificaron factores protectores y de riesgo predictores de niveles de síntomas del AjD en diferentes momentos de la pandemia. Para algunos predictores, los efectos sobre la salud mental impresionan cambiar en diferentes etapas de una pandemia.
1. Introduction
The COVID-19 pandemic resulted in profound psychological, societal, and economic disruptions (Dubey et al., Citation2020). It has caused illness, deaths, and strain on healthcare and economic systems. Entire populations have experienced multiple pandemic-specific stressors, such as fear of contracting or suffering from COVID-19, quarantine and physical distancing, home schooling and remote work. Some individuals faced income or work loss, which can additionally strain mental health and wellbeing (Thomson et al., Citation2022).
In view of the cumulative stress factors specific to the pandemic, those affected could be at increased risk of adjustment disorders (AjD). According to the eleventh version of the International Classification of Diseases (ICD-11; WHO, Citation2021), AjD is defined as a failure to adapt to stressors, such as illness or disability, socio-economic problems, and conflicts at home (WHO, Citation2021). The main features of AjD include preoccupation with the stressor or its consequences, recurrent and distressing thoughts about the stressor, or constant rumination about its consequences. Symptoms of AjD cause significant impairment in personal, family, social, educational, occupational functioning (WHO, Citation2021). During a pandemic, where multiple stressors may overtax coping abilities, development of AjD is plausible.
While many studies looked at the relationships between pandemic-related stressors and depressive or anxiety symptoms during the COVID-19 pandemic (Daniali et al., Citation2023), few studies examined the relationships with AjD symptom levels (e.g. Ben-Ezra et al., Citation2021; Dragan et al., Citation2021; Rossi et al., Citation2020). The studies on AjD syptoms reported cross-sectional associations between higher AjD symptom levels and younger age (Rossi et al., Citation2020), female gender (Ben-Ezra et al., Citation2021; Dragan et al., Citation2021; Rossi et al., Citation2020), general health problems, social isolation, and caregiving problems (Ben-Ezra et al., Citation2021). Relationships with AjD symptom levels were also found for unemployment (Dragan et al., Citation2021) and job loss (Zelviene et al., Citation2020), which are important risk factors for AjD (Lorenz et al., Citation2018).
A crosssectional analysis of the first wave of The European Society for Traumatic Stress Studies (ESTSS) ADJUST study reported associations between higher AjD symptom levels and a number of risk fators, including older age, female gender, fear of infection, trauma exposure, a previous mental health disorder, exposure to COVID-19 related news, and restricted social contact (Lotzin et al., Citation2021). While these findings provide insights into cross-sectional associations between risk factors and AjD symptom levels during the early phase of the pandemic, it is still unclear whether these relationships remain stable or may change over the different phases of the pandemic. Some of the pandemic-related stressors were completely new in the initial phase of the pandemic, but people may have learned to deal with them adaptively after an initial adjustment.
We are only aware of one previous study that examined longitudinal associations between pandemic-related risk factors and AjD symptoms at different time points of the COVID-19 pandemic among the general population. The study examined associations between female gender and health-related stressors (deterioration in health, diagnosis of an illness, and physical injury or disability) and AjD symptoms before and after the second lockdown during the pandemic in the Israeli population (Hamama-Raz et al., Citation2021). Significant relationships between these variables were found at both timepoints.
Addional research on predictors of AjD symptoms during the COVID-19 pandemic was conducted among patient samples. German patients with different mental health disorders were cross-sectionally assessed during the first year of the pandemic (Belz et al., Citation2022). AjD symptoms were evaluated retrospectively before the pandemic, during the most strict lockdown conditions, and after the most strict lockdown conditions (Belz et al., Citation2022). Psychosocial problems and media consumption were related to higher AjD symptom levels (Belz et al., Citation2022). Whether these relationships varied at different time points over the course of the pandemic was not assessed.
In sum, a few cross-sectional studies (Belz et al., Citation2022; Ben-Ezra et al., Citation2021; Dragan et al., Citation2021; Rossi et al., Citation2020) and one longitudinal study (Hamama-Raz et al., Citation2021) reported significant relationships between risk factors and pandemic-related stressors and AjD symptom levels, including both younger and older age, a COVID-19 infection, health-related stressors, female gender, psychosocial stressors, social isolation, caregiving problems, unemployment, and media consumption. We are unaware of research examining whether the relationships between these risk factors orstressors and AjD symptom levels change over time. Given the high and prolonged psychological burden of the COVID-19 pandemic, it seems essential to better understand the relationships between these factors and and symptoms of AjD over different phases of the COVID-19 pandemic to be able to design adequate intervention strategies for future pandemics.
Based on an adapted COVID-19 framework of determinants of health (Lotzin et al., Citation2020), this research examined the relationships between risk and protective factors (e.g. age, gender, income), pandemic-specific stressors (e.g. fear of infection, restricted social contact), and symptoms of AjD at three different time points over 18 months of the COVID-19 pandemic in a large sample of more than 15,000 participants from the general populations of eleven European countries. The very few studies conducted on AjD symptoms during the pandemic did not include such a large sample and only assessed one specific country. The knowledge gained from this study may help identify potential risk and protective factors for AjD symptoms at different time points of the pandemic.
2. Methods
2.1. Study design and setting
The ADJUST study was initiated by the ESTSS. The study investigated longitudinal associations between risk and protective factors, stressors, and symptoms of AjD during the COVID-19 pandemic in the general populations of eleven European countries (Austria, Croatia, Georgia, Germany, Greece, Italy, Lithuania, the Netherlands, Poland, Portugal, and Sweden). Participants who consented to study participation and to multiple data collections were assessed at three timepoints, with 6-months intervals from June 2020 to January 2022. A 6-months interval was chosen as COVID-infection rates and the corresponding lockdown measures were expected to change between different seasons (e.g. from summer to winter). The study was pre-registered in a study registry (OSF registry, https://osf.io/8xhyg).
2.2. Participants
We recruited participants from the general populations of the above mentioned eleven countries. Inclusion criteria were (1) at least 18 years of age, (2) ability to read and write in the respective language, and (3) willingness to participate in the study.
2.3. Measures
2.3.1. Symptoms of adjustment disorder
We assessed symptoms of AjD with the Adjustment Disorder – New Module 8 scale (ADNM-8; Kazlauskas et al., Citation2018), a self-report measure of AjD according to the eleventh version of the International Classification of Diseases (ICD-11; WHO, Citation2021). The participants were asked to ‘indicate what was the most straining event(s) during the Coronavirus-pandemic’, and to evaluate for the most stressful event how often the respective statement applied to them. AjD symptoms are assessed by eight items (1 = never, 2 = rarely, 3 = sometimes, 4 = often). A total score, ranging from 8 to 32, is calculated by summing the item scores. A cut-off score of >22 indicates probable AjD. The ADNM-8 is the short form of the ADNM-20; both measures have been widely used in ICD-11 AjD research (Kazlauskas et al., Citation2017). The ADNM-8 has proven structural and convergent validity (Ben-Ezra et al., Citation2018; Kazlauskas et al., Citation2017) and excellent accuracy of diagnosing AjD according to ICD-11 (Ben-Ezra et al., Citation2018).
2.3.2. Risk and protective factors
We used the WHO framework for social determinants of health (Solar & Irwin, Citation2010) for selecting risk and protective factors, which we adapted to the specific circumstances of the COVID-19 pandemic (Lotzin et al., Citation2020). Risk and protective factors included sociodemographic (e.g. age, gender), pandemic-related (, e.g. reduced income due to pandemic), and health-related characteristics (, e.g. current health condition). Items were self-constructed except for trauma exposure, as validated measured were unavailable at the time of survey development. For the self-constructed items, the core item set was developed in English language. The standard procedure for translation was as follows: A native speaker of the respective study site translated the self-constructed variables. A second native speaker backtranslated the translation and checked the correctness of the translation. Any discrepancies were discussed within the team and a final decision on the correct translation was made upon consensus.
Table 1. Pandemic-related and clinical characteristics (N = 15,169).
Table 2. Health-related characteristics (N = 15,169).
Trauma exposure was measured using the Criterion A section of the PTSD Checklist for DSM-5 (PCL-5; Weathers et al., Citation2013). Participants were asked whether they experienced stressful event(s) involving actual or threatened death, serious injury, or sexual violence before or during the COVID-19 pandemic.
2.3.2.1. Pandemic-related stressors
We assessed the burden of pandemic-related stressors within the last month by a self-constructed 30-item questionnaire named Pandemic Stressor Scale (PaSS). The measure, item construction and psychometric properties are described elsewhere (Lotzin et al., Citation2022). Participants indicate on 5-point scales (0 = ‘Not at all burdened’; 1 = ‘Somewhat burdened’; 2 = ‘Moderately burdened’; 3 = ‘Strongly burdened, 4 = ‘Does not apply to me’) how much different stressors have burdened them due to the pandemic. The PaSS measures pandemic-related stressors in nine domains: Crisis management and communication (e.g. poor information from the government); Fear of infection (e.g. fear of getting infected with the coronavirus); Burden of infection (e.g. own infection with the coronavirus); Restricted Face-to-face contact (e.g. restricted face-to-face contact with loved ones); Restricted activity (e.g. restricted everyday activity such as shopping); Restricted leisure activity (e.g. restaurant visit); Work-related problems (e.g. not being able to work); Difficult housing conditions, (e.g. restricted housing conditions such as little space); Restricted access to resources (e.g. restricted access to goods, e.g. food, water, clothing). Subscale scores for the different domains were calculated by the average of the scores of the respective items. Before calculating subscores, we recoded the ‘Does not apply to me’ category to ‘Not at all burdened’. The nine-factor structure yielded in the German sample of the ADJUST study could be replicated in a confirmatory factor analysis using the data of the Austrian sample (Lotzin et al., Citation2022).
2.3.3. Lockdown stringency
To adjust for possible differences in the strictness of lockdown measures during the COVID-19 pandemic, the Oxford stringency index (https://ourworldindata.org/covid-stringency-index) was included in the analysis on the person-level. We included the stringency value at the time of the data assessment for each participant separately, except for Croatia, where we used the start date of the assessment, as individual dates were unavailable. To adjust for between-country differences, a variable indicating the different countries was constructed.
2.3.4. Procedure
Data were collected between June 2020 and January 2022 at three time intervals (T1 June 2020 to December 2020; T2 December 2020 to June 2021; T3 June 2021 to January 2022). Symptoms of adjustment disorder as well as the measured risk and protective factors were collected repeatedly at T1, T2 and T3. Due to the lockdown situation, recruitment was predominantly conducted online. We applied different recruitment strategies to increase sample variability in terms of gender, age, and education. We promoted the study via social platforms, leisure and interest groups, newsletters, and advertisements in newspapers and magazines. We also disseminated the study information through universities, stakeholders, and professional organizations. The study site in Poland recruited participants via a professional panel service. A more detailed description of the recruitment strategy can be found elsewhere (Lotzin et al., Citation2021). Interested individuals received a study invitation by a website link to the survey. After providing consent, they could complete an online survey on web-based platforms following the EU data protection regulations.
2.3.5. Data analysis
The data analysis set of N = 15,196 included all cases that had at least one value in the dependent variable at either T1, T2 or T3. Individuals with missing values in the dependent variable at all three timepoints (7.6%) were excluded, as the imputation of missing values in the dependent variable is not recommended. We imputed missing values of all independent variables using multiple imputation following the guidelines by White and colleagues (Citation2011). We generated 50 imputed datasets by using the mice (multivariate imputations by chained equations) package in R (van Buuren & Groothuis-Oudshoorn, Citation2011) and the predictive mean matching option as imputation method. All independent and dependent variables of this data analysis were included in the imputation model. Additional variables were selected for the imputation model based on their correlation with the incomplete variables.
A linear mixed regression model with the AjD symptom score as dependent variable (ADNM-8) was performed. As fixed effects, risk and protective factors (see methods section), the nine PaSS subscales, and the timpoint of assessment were included in the model. The stringency index was included as fixed effect to adjust for possible differences in stringency of the applied lockdown measures. The participant identificator and the country of the data assessment were included as random effects. Descriptive statistics were computed for all variables included in the model. Mean and standard deviation were calculated, as appropriate, for the continuous variables; absolute and relative frequencies were computed for categorical variables. As a sensitivity analysis, the same analysis was performed using the dataset with all imputed values including the dependen variable, which relevealed comparable results. All analyses were conducted with R-4.2.2 for Windows.
2.3.6. Results
Out of the N = 15,169 participants, n = 6006 (36.6%) completed all three waves of the survey whereas n = 8389 (51.12%) and n = 2016 (12.28%) dropped out at T2 and T3, respectively. Cases were complete (i.e. no missing values in the variables used in analysis) in n = 1680 (10.2%) participants. Missing values ranged from 0.01% (gender at T1) to 69.31% (burden related to reduced social contact at T2) in the independent variables.
Table 3. Pandemic-related stressors (N = 15,169).
2.3.7. Sample characteristics
Two third of the sample were female (n = 10,402, 68.6% female; n = 4712, 31.1% male; n = 54, 0.4% diverse). Age (M = 42.7, SD = 15.3, range 18–96 years) and income (n = 1209, 8.5% very low income; n = 2709, 19.1% low income; n = 5105, 36.0% medium income; n = 5162, 36.4% high income) varied. The sample was predominantly high-educated (n = 368, 2.5% less than 10 years of schooling; n = 3466, 23.3% ≥ 10 years of schooling; n = 2143, 14.4% vocational studies, n = 8886, 59.8% completed studies). About half of the sample (n = 7578, 50.1%) was employed full time, 15.8% (n = 2381) was employed part-time, 15.6% (n = 2359) seeked work, and 10.6% (n = 1605) were retired. The remaining participants were self-employed (n = 876, 5.8%), freelancer (n = 553, 4.2%), in training or study (n = 874, 5.8%) or had another occupation (n = 817, 7.2%). Work areas varied across the sample (n = 1913, 14.6% healthcare; n = 1796, 13.7% education; n = 856, 6.6% retail or services; n = 749, 5.7% public security; n = 420, 3.2% maintenance, repair, or construction; n = 4790, 36.7% other work area; n = 2539, 19.4% not working). Lockdown stringency was lower at T1 and T3 compared to T2 (). The percentage of individuals with a COVID-19 infection, verified by a test, increased over time (; T1 n = 296; 2.0%; T2, n = 632, 9.1%, T3 n = 752, 12.9%).
The AjD symptom level was moderate at all three measurement points: T1 (M = 16.03, SD = 6.45), T2 (M = 16.51, SD = 6.65), and T3 (M = 15.41, SD = 6.47), on average. The prevalence of probable AjD was 18.7%, 21.5%, and 17.1% at T1, T2 and T3, respectively (). At all time points, the highest burden was related to the pandemic stressors 'Fear of infection', 'Restricted activity' and 'Restricted social contact' ().
2.3.8. Predictors of AjD symptoms
2.3.8.1. Risk factors
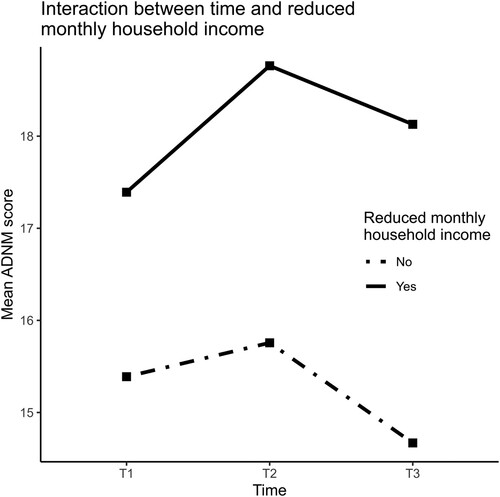
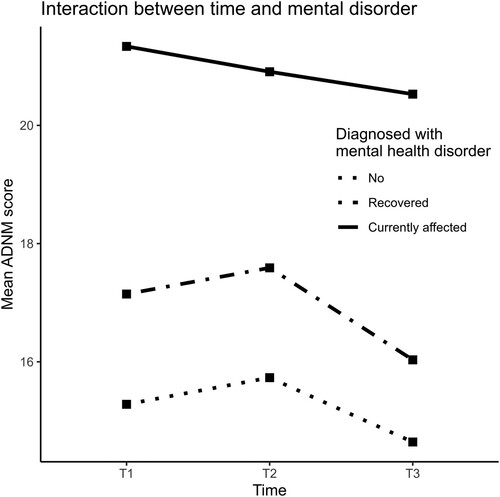
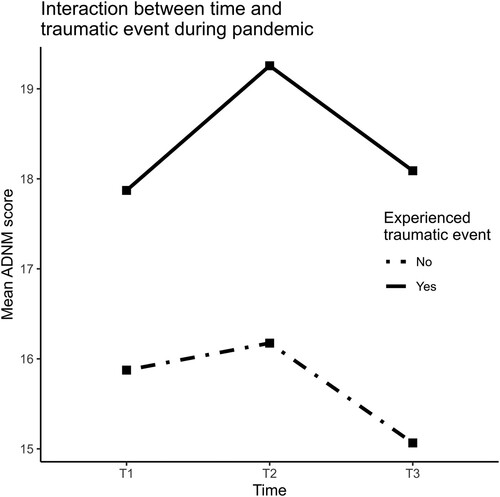
The following sociodemographic, pandemic- or health-related variables were significantly associated with higher AjD symptom levels (, for effect estimates and p-values see ): female or diverse gender (vs. male gender), older age (vs. younger age), pandemic-related news consumption of more than 30 min a day (vs. no news consumption); diagnosis of a current mental health disorder; diagnosis of a previous mental health disorder; trauma exposure during the pandemic (vs. no trauma exposure); trauma exposure before the pandemic (vs. no trauma exposure); ‘good’, ‘satisfactory’ or ‘poor’ health status (vs. ‘very good’ health status). The following of the above reported effects did not differ by time of assessment: female or diverse gender (vs. male gender), older age (vs. younger age), pandemic-related news consumption of more than 30 min a day (vs. no news consumption); trauma exposure before the pandemic (vs. no trauma exposure); ‘good’, ‘satisfactory’ or ‘poor’ health status (vs. ‘very good’ health status). In contrast, a significant interaction effect with time was found for the following variables: The effect of income reduction on AjD symptom levels was significantly greater at T2 vs. T1 (). The effect of a current mental health disorder on AjD symptom levels was significantly greater at T1 vs. T2 and T3. The effect of a previous mental health disorder was significantly greater at T1 vs. T3. In contrast, the effect of trauma exposure during the pandemic on AjD symptoms was significantly greater at T2 and T3 vs. T1.
Figure 1. Effect estimates of the linear mixed regression analysis.
Notes. ≥10 years = 10 or more years of schooling. Reduced income = Reduced monthly household income due to the coronavirus. Financial support = Receiving financial support from the government. Maintenance/repair/etc. = Maintenance, repair, construction. More at home = Spent more time at home due to the coronavirus pandemic. Social dist. = Spent more time at home as a precautionary measure (social distancing). Self-isolation = Stayed at home in self-isolation because of self-infection. Quarantine = Stayed at home due to contact with infected people or being in risk areas. Face contact = Face-to-face contact with loved ones or friends. Face contact at work = Work involves (almost) daily face-to-face contact with other people. Digital contact = Digital contact with loved ones or friends, e.g. by phone, Skype, or Zoom. News = Hours a day watching, reading, or listening to the news or other information about the coronavirus pandemic. COVID-19 inf. = Infected (i.e. tested positive) with the coronavirus.
Reference categories: aMale. bLess than 10 years of schooling. cVery low. dNo. eOther. fNo. gI have no personal contact with other people. hI have no contact by phone, skype, etc. iI do not watch, read or listen to news about the coronavirus pandemic. jVery good. kNo.
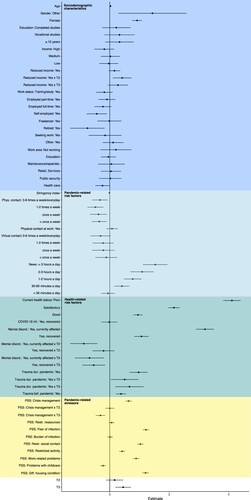
Table 4. Effect estimates of risk factors and stressors on symptoms of adjustment disorder (N = 15,169).
2.3.8.2. Protective factors
The following variables were significantly related to lower AjD symptom levels: self-employment or retirement (vs. having no work); working in healthcare (vs. other work area); and a higher face-to-face contact of more than once a week (vs. no face-to-face contact; , for effect estimates and p-values see ). The reported significant effects did not differ by time of assessment.
2.3.8.3. Pandemic stressors
Six out of nine pandemic stressor domains were positively related to AjD symptom levels (all p < .001, , ). These included ‘Fear of infection,’ ‘Governmental crisis communication and management’, ‘Restricted face-to-face contact’, ‘Work-related problems’, ‘Restricted (leisure and everyday) activity’, and ‘Difficult housing conditions’. ‘Problems with childcare’ was negatively associated with AjD symptom levels. The analysis was controlled for lockdown stringency, which was related to AjD symptom levels. Significant interaction effects with time were found for the effect of ‘Governmental crisis communication/management’, which was higher at T1 vs. T3. For the remaining variables, effects did not differ by the time of assessment.
3. Discussion
This study examined predictors of AjD symptoms, including risk and protective factors and pandemic-related stressors, in the general populations of eleven countries over 18 months of the COVID-19 pandemic. The prevalence rate of self-reported probable AjD was 18.7% at the first assessment (June 2020 to December 2020), 21.5% at the second assessment (December 2020 to June 2021), and 17.1% at the third assessment (June 2021 to January 2022). The higher lockdown stringency at the second assessment might have contributed to an increased pandemic-related burden and a higher risk of AjD.
3.1. Sociodemographic factors
A number of sociodemographic factors, including female or diverse gender and age, were significantly related to AjD symptom levels. Female gender was associated with higher AjD symptom levels at all three assessments. Meta-analytic evidence indicates that women showed greater depressive and anxiety symptoms during the pandemic compared to men (Robinson et al., Citation2022). Women may have experienced more pandemic-related stressors, as they are more often responsible for childcare than men (Petts et al., Citation2021). They also might have been more affected by domestic violence and job loss (Flor et al., Citation2022), thereby aggravating existing pre-pandemic mental health gender inequalities. On the other hand, gender differences in AjD symptoms could reflect higher biological stress vulnerability. There are gender-specific differences in the hypothalamic-pituitary-adrenal (HPA) stress system and its responses, which could explain gender-specific differences in AjD between women and men. For example, stressors activate the HPA axis more quickly and releases a greater amount of stress hormones in women compared to men (Goel et al., Citation2014).
Diverse gender (vs. male) was related to higher AjD symptom levels in our study, although the sample size of this subgroup was small. Associations between divere gender and higher distress during the pandemic were reported in earlier studies (Hunt et al., Citation2021). Gender diverse individuals may receive less social support and gender-affirming interventions (Jones et al., Citation2021), which may contribute to higher AjD levels.
Older age (vs. younger age) was associated with higher AjD symptom levels, consistent with earlier research during the COVID-19 pandemic (Dworakowski et al., Citation2022). Older age might be related to poorer health, a higher risk for a severe or life-threatening COVID-19 infection, and reduced face-to-face contact compared to younger age, which may be factors related to AjD. While earlier research reported relationships between younger age and increased psychological distress (Breslau et al., Citation2023), we did not find this relationship with regard to AjD symptoms over the three assessed timepoints.
In contrast to our expectations, working in healthcare (vs. other work area) was related to lower AjD symptoms. However, the chosen category ‘working in healthcare’ might have been too broad to identify high-risk individuals, such as healthcareworkers who cared for COVID-19 infected patients. Future studies should examine different types of healthcare professions more in depth to differentiate between high- and low-risk groups.
The effects of the sociodemographic variables female and diverse gender, age, work area and work status did not differ by the time of assessment, indicating that the relationships with AjD symptom levels remained stable over the pandemic.
3.1.1. Income reduction
While the main effect of income reduction (vs. no income reduction) on AjD symptom levels did not reach significance, time of assessment moderated the relationship between income reduction and AjD symptom levels. Income reduction was related to a greater increase in AjD symptoms at the second assessment compared to the first assessment. Income reduction could be particularly burdensome if it lasts for a longer period of time (Gupta et al., Citation2020; Midões & Seré, Citation2022), which could have been the case for our study participants at the second compared to the first assessment. Another factor that differed at the second assessment was the degree of lockdown stringency, which was highest at this time period. Consistent with our findings, earlier research found that income was more greatly reduced during phases of high lockdown stringency (Midões & Seré, Citation2022). In these phases, the reduction in income could have reduced the financial resources for the necessary food and housing expenses (Midões & Seré, Citation2022), which might have increased distress. Earlier pre-pandemic research found that low income was associated with higher distress (Breslau et al., Citation2023), depression and anxiety symptoms (Blasco-Belled et al., Citation2022).
3.2. Pandemic-related factors
The frequency of face-to-face contact with loved ones or friends was related to lower AjD symptom levels over the three assessments, while the frequency of digital social contact with loved ones or friends was unrelated to AjD symptom levels. These findings are in line with earlier research reporting that face-to-face contact had a stronger positive affect on mental health and wellbeing than digital contact during the pandemic (Newson et al., Citation2021; Stieger et al., Citation2023). Research has indicated that communication perceived as more natural was related to lower levels of loneliness and sadness and higher levels of happiness compared to less natural communication (Petrova & Schulz, Citation2022). Face-to-face communication may help to reduce distress and may increase positive emotions that may buffer against the stressors of the pandemic.
Consumption of news related to COVID-19 of at least 30 min per day (vs. no news consumption) was associated with higher AjD symptom levels, while news consumption of less than 30 min a day was unrelated to AjD symptom levels. There was a dose-response relationship between the variables, i.e. the longer the duration of news consumption, the higher were the reported AjD symptom levels. Pandemic-related news consumption may not be harmful at a lower dosis, but may lead to AjD symptoms at a higher dosis.
3.3. Health-related factors
A current health status perceived as less than very good (i.e. good, satisfactory, or poor) was related to higher AjD symptom levels. The worse the health status, the higher were the AjD symptom levels. Individuals with a poor health condition reported the highest levels of AjD symptoms. Previous studies reported associations between medical problems or physical diseases and higher levels of distress, anxiety, and depression during the COVID-19 pandemic (Mazza et al., Citation2020; Özdin & Bayrak Özdin, Citation2020). Poor health can lead to a variety of stressors, such as worrying about caring for the health condition and accessing needed treatment or medication (Boyle et al., Citation2020). These additional stressors may overwhelm the capacity to cope with the numerous other stressors during a pandemic.
A current or previous diagnosis of a mental health disorder (vs. no mental health disorder) was related to higher AjD symptom levels, in line with an earlier cross-sectional study reporting associations between a previous mental health diagnosis and higher levels of AjD symptoms (Rossi et al., Citation2020). Previous research found strong associations between pre-existing mental health disorders and higher levels of anxiety or depressive symptom during the pandemic (Neelam et al., Citation2021). Pre-existing mental health disorders might lead to additional burden and lower abilities to cope with the stressors during a pandemic.
The effects of a current or previous mental health disorder on AjD symptoms were significantly greater at the first assessment compared to the following assessments. A mental health disorder might reduce the capacities to cope with the multiple novel stressors during the early phase of a pandemic. In addition, many health support facilities were closed in the earlier phase of the pandemic which reduced mental health support (Duden et al., Citation2022).
Trauma exposure before the pandemic and trauma exposure during the pandemic (vs. no trauma exposure) were related to higher AjD symptom levels. People with trauma exposure during the pandemic showed the highest AjD symptom levels at all timepoints. It is well documented that trauma exposure is a transdiagnostic risk factor for mental health disorders (Hogg et al., Citation2023).
The effect of trauma exposure during the pandemic on AjD symptom levels – but not trauma exposure before the pandemic – was greater at the second and third assessment compared to the first assessment. At the third assessment, AjD symptom levels were lower in both the trauma and non-trauma group compared to the second assessment, but the AjD symptom levels stayed relatively high in the trauma-exposure group. These findings may indicate that the effect of trauma exposure on AjD symptom levels is more pronounced when lockdown stringency is high.
3.3.1. Work status
Self-employment and retirement were associated with lower AjD symptom levels compared to having no work. Retirement might be related to fewer work-related stressors, such as risk of COVID-19 infection in the workplace. Self-employment, i.e. income from an independent pursuit of economic activity, might be related to a lower risk of income loss, and a higher level of control of one’s own financial situation. Employment and freelancing were unrelated to AjD symptoms compared to having no work, which may indicate similar levels of distress during the pandemic.
3.4. Pandemic-related stressors
Out of the nine assessed stressor domains, six domains were significantly associated with AjD symptoms. Burden due to inefficient Crisis management and communication of the government was related to higher AjD symptom levels, pointing to the importance of efficient and clear governmental communication and management for the mental health of the general population. In times of a global pandemic, crisis communication is essential to reduce fear and uncertainty and motivate individuals to act together against health threats (Su et al., Citation2021). Inadequate crisis communication, such as ongoing news about COVID-19 infection and death rates is associated with fear and uncertainty (Li et al., Citation2021; Su et al., Citation2021). Due to the increased anxiety, individuals could experience the pandemic as less manageable and therefore may have an increased risk of developing AjD. Adequate governmental management and communication seems to be particularly important at the beginning of a pandemic, as we found that the effect of this factor was lower at the last assessment (vs. the first).
Distress due to Fear of infection was associated with higher AjD symptom levels. COVID-19 related fear could be addressed by preventive interventions to reduce distress and AjD symptoms. The perceived Burden of infection was unrelated to AjD symptom levels, which might be since a low proportion of participants (i.e. 13% at the last assessment) contracted COVID-19 in our study. Individuals severely affected by a COVID-19 infection might have not been able to participate in the survey. Distress related to Restricted face-to-face contact was associated with higher AjD symptom levels. Earlier research found associations between social support and lower levels of depression and anxiety symptoms during the COVID-19 pandemic (Li et al., Citation2021). Social support can mitigate distress (Cohen & Hoberman, Citation1983) and is associated with better mental health during the COVID-19 pandemic (Li et al., Citation2021).
Restricted activity including restricted shopping, restaurant visits, and private travelling, was related to higher AjD symptom levels. Leisure activities significantly reduced distress during the first lockdown of the COVID-19 pandemic (Takiguchi et al., Citation2023). Engaging in activities may be helpful to reduce AjD symptoms, as they may promote functional coping, social support and opportunities for positive environmental reinforcement (Arends et al., Citation2012). Preventive interventions in pandemic contexts may therefore include the planning and implementation of safe and permitted activities in public and private spaces.
Distress related to Difficult housing conditions, such as restricted room space and conflicts at home, was associated with higher AjD symptom levels. Previous studies reported associations between poorer housing conditions and increased levels of depressive symptoms during the COVID-19 pandemic (Amerio et al., Citation2020). No access to outdoor space and household crowding were associated with higher levels of anxiety symptoms (Keller et al., Citation2022). Hence, difficult housing conditions seem to contribute to poor mental health during a pandemic.
Contrary to our expectations, distress due to Problems with childcare (i.e. loss of childcare, difficulties with combining work with childcare) was negatively related to AjD symptoms, although an earlier study found associations between difficulties obtaining childcare and depression and anxiety symptoms during the pandemic (Racine et al., Citation2021). Parents who use childcare (and have problems with it) may be more priviledged in terms of financial ressources compared to parents not using childcare, which might reduce burden during a pandemic. Moreover, spending time with children might foster family bonding, which might in turn buffer the effects of other pandemic-related stressors.
Overall, we identified significant predictors of AjD symptoms among the general populations of eleven countries that included risk and protective factors, as well as pandemic-related stressors over a period of 18 months of the COVID-19 pandemic. The effect sizes were in the small to moderate range, with a current poor or satisfactory health condition (vs. very good health condition) and a current diagnosis of a mental health disorder (vs. no mental health disorder) showing greater effect sizes, followed by news consumption more than 3 h a day (vs. no news consumption), diverse gender, fear of infection, restricted face-to-face contact, and a difficult housing situation. Due to their comparatively greater impact, these factors should be prioritized in prevention and intervention efforts.
The effects of the predictors were mostly additive, i.e. the size of the effect on AjD symptom levels did not differ by the time of assessment, relative to the respective comparison group. According to our results, most of the predictors of AjD symptoms remained stable over time, independently from different levels of lockdown stringency and the chronicity of the pandemic.
Nevertheless, we did find specific predictors for which the size of the effect on AjD symptoms depended on the time of assessment. While the effects of a previous mental health disorder and governmental communication and management were more pronounced at the earlier phase of the pandemic, the effects of income reduction and trauma exposure during the pandemic were more pronounced at later phases of the pandemic. Addressing the identified predictors of AjD symptoms at an optimal time window, i.e. when they have stronger effects, may help to reduce AjD symptoms and may improve preparedness for future pandemics.
3.5. Strengths and limitations
The longitudinal study design, the large sample size and the use of a well-established measure as the dependent variable are strengths of this study. The use of a non-probabilistic sample is a weakness of this study, as it overrepresents individuals with higher education and women, and underrepresents individuals with no or poor internet accessibility and those severely affected by a COVID-19 infection. Moreover, the study might have overrepresented individuals with higher psychological distress as they might be more inclined to participate in surveys on mental health problems (Groves et al., Citation2004). On the other hand, individuals with a severe mental health disorder might be underrepresented as they might be more hesitant to participate in a survey (Pierce et al., Citation2020). Furthermore, the use of self-report measures could have introduced systematic bias.
4. Conclusions
We found several risk factors and stressors longitudinally associated with AjD symptom levels over the COVID-19 pandemic. The risk factors and stressors may help identify individuals with high-risk profiles. These may include individuals with a less than very good health status, fear of COVID-19 infection, a mental health disorder, trauma exposure, lack of social support, work-related problems, and restricted housing conditions.
Most of the effects of the risk factors and stressors were relatively stable over the first two years of the pandemic, i.e. independent from lockdown stringency and duration of the pandemic. Few risk factors and stressors showed differential effects depending on the time of assessment during the pandemic. These risk factors and stressors should be particularly addressed at the time windows in which they might have stronger effects. The identified predictors may be targeted by psychosocial interventions to reduce AjD symptoms and to prevent more severe mental health disorders in future pandemics.
Author contributions
AL designed the study in cooperation with all members of the ADJUST consortium formed by the representatives of the ESTSS countries. All authors recruited study participants and contributed to the data management of the respective site. KS conducted the data analysis. AL drafted the first version of the manuscript. All authors revised sections of the manuscript and approved the final version of the manuscript.
Data protection and quality assurance
The dataset for the data analysis was stored on a server of the coordinating site (Centre for Interdisciplinary Addiction Research, CIAR, University of Hamburg). Data handling followed the EU General Data Protection Regulation (DSGVO); data will be stored for at least 10 years.
Ethics, consent, and permissions
Each country obtained ethical approval of the study: Ethics Committee of the University of Vienna, 00554. Ethics Committee of the University of Urbino ‘Carlo Bo’, 34, 22 July 2020. Ethics Committee of the Department of Psychology, Faculty of Humanities and Social Sciences, University of Zagreb, 21 May 2020. Ethics Review Board of the Faculty of Social and Behavioural Sciences, Utrecht University, 20-360. Ilia State University Faculty of Arts and Science Research Ethics Committee, 12 June 2020. Local Psychological Ethics Committee at the Centre for Psychosocial Medicine, LPEK-0149. Social Sciences Ethics Review Board (SSERB), University of Nicosia, SSERB 00109. The Swedish Ethical Review Authority, 2020-03217. Vilnius University Ethics Committee of Research in Psychology, 44. Ethics Committee of the Faculty of Psychology, University of Warsaw, 6 July 2020. Ethics Committee of the Medical Faculty, University of Porto and Centro Hospitalar São João, Porto, CE 201-20. The National Ethical Review Board in Sweden, 2020-03217. All participants provided informed consent before taking part in the study. Participants were informed that they were under no obligation to participate and that they could withdraw at any time from the study without consequences.
Acknowledgments
The authors thank the collaborators for their support and contribution to the present paper: Ozan Demirok (team Austria); Marina Ajdukovic, Helena Bakic, Ines Rezo Bagaric, Tanja Franciskovic (team Croatia); Nino Makhashvili and Sophio Vibliani (team Georgia); Eleftheria Eugeniou, George Fevgas, Kostas Messas, Marianna Philippidou, Eleni Papathanasiou, Anastasia Selidou (team Cyprus/Greece); Ilaria Cinieri, Alessandra Gallo and Chiara Marangio (team Italia); Monika Kvedaraite and Auguste Nomeikaite (team Lithuania); Joanne Mouthaan, Suzan Soydas, Marloes Eidhof, Marie José van Hoof and Simon Groen (team the Netherlands); Magdalena Skrodzka and Monika Folkierska-Żukowska (team Poland); Aida Dias, Camila Borges, Diana Andringa, Guida Manuel, Joana Beker and João Veloso, Francisco Freitas (team Portugal); Kristina Bondjers, Josefin Sveen, Rakel Eklund, Kerstin Bergh Johannesson and Ida Hensler (team Sweden). We greatly thank the study team of the coordinating site at University Medical Center Hamburg-Eppendorf (team Germany) that conducted the overall data management: Laura Kenntemich, Leonie von Huelsen, Sven Buth, Eike Neumann-Runde, Ronja Ketelsen, Lennart Schwierzke, Julia Groß, Laura Gutewort, and Emily Price.
Data availability
The detailed sociodemographic information of the dataset does not fully protect the anonymity of the respondents. For this reason, the entire dataset cannot be made publicly available. However, excerpts of the data on a higher aggregation level can be provided upon justified request by the first author.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Amerio, A., Brambilla, A., Morganti, A., Aguglia, A., Bianchi, D., Santi, F., Costantini, L., Odone, A., Costanza, A., Signorelli, C., Serafini, G., Amore, M., & Capolongo, S. (2020). COVID-19 lockdown: Housing built environment’s effects on mental health. International Journal of Environmental Research and Public Health, 17(16), 5973. https://doi.org/10.3390/ijerph17165973
- Arends, I., Bruinvels, D. J., Rebergen, D. S., Nieuwenhuijsen, K., Madan, I., Neumeyer-Gromen, A., Bultmann, U., & Verbeek, J. H. (2012). Interventions to facilitate return to work in adults with adjustment disorders. Cochrane Database of Systematic Reviews, 12(12), Art. No CD006389. https://doi.org/10.1002/14651858.CD006389.pub2
- Belz, M., Hessmann, P., Vogelgsang, J., Schmidt, U., Ruhleder, M., Signerski-Krieger, J., Radenbach, K., Trost, S., Schott, B. H., Wiltfang, J., Wolff-Menzler, C., & Bartels, C. (2022). Evolution of psychosocial burden and psychiatric symptoms in patients with psychiatric disorders during the Covid-19 pandemic. European Archives of Psychiatry and Clinical Neuroscience, 272(1), 29–40. https://doi.org/10.1007/s00406-021-01268-6
- Ben-Ezra, M., Hou, W. K., & Goodwin, R. (2021). Investigating the relationship between COVID-19-related and distress and ICD-11 adjustment disorder: Two cross-sectional studies. BJPsych Open, 7(1), e21. https://doi.org/10.1192/bjo.2020.158
- Ben-Ezra, M., Mahat-Shamir, M., Lorenz, L., Lavenda, O., & Maercker, A. (2018). Screening of adjustment disorder: Scale based on the ICD-11 and the Adjustment Disorder New Module. Journal of Psychiatric Research, 103, 91–96. https://doi.org/10.1016/j.jpsychires.2018.05.011
- Blasco-Belled, A., Tejada-Gallardo, C., Fatsini-Prats, M., & Alsinet, C. (2022). Mental health among the general population and healthcare workers during the COVID-19 pandemic: A meta-analysis of well-being and psychological distress prevalence. Current Psychology, 1, 1–12. https://doi.org/10.1007/s12144-022-02913-6
- Boyle, C. A., Fox, M. H., Havercamp, S. M., & Zubler, J. (2020). The public health response to the COVID-19 pandemic for people with disabilities. Disability and Health Journal, 13(3), 100943. https://doi.org/10.1016/j.dhjo.2020.100943
- Breslau, J., Roth, E. A., Baird, M. D., Carman, K. G., & Collins, R. L. (2023). A longitudinal study of predictors of serious psychological distress during COVID-19 pandemic. Psychological Medicine, 53(6), 2418–2426. https://doi.org/10.1017/S0033291721004293
- Cohen, S., & Hoberman, H. M. (1983). Positive events and cocial supports as buffers of life change stress. Journal of Applied Social Psychology, 13(2), 99–125. https://doi.org/10.1111/j.1559-1816.1983.tb02325.x
- Daniali, H., Martinussen, M., & Flaten, M. A. (2023). A global meta-analysis of depression, anxiety, and stress before and during COVID-19. Health Psychology, 42(2), 124–138. https://doi.org/10.1037/hea0001259
- Dragan, M., Grajewski, P., & Shevlin, M. (2021). Adjustment disorder, traumatic stress, depression and anxiety in Poland during an early phase of the COVID-19 pandemic. European Journal of Psychotraumatology, 12(1), 1860356. https://doi.org/10.1080/20008198.2020.1860356
- Dubey, S., Biswas, P., Ghosh, R., Chatterjee, S., Dubey, M. J., Chatterjee, S., Lahiri, D., & Lavie, C. J. (2020). Psychosocial impact of COVID-19. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 14(5), 779–788. https://doi.org/10.1016/j.dsx.2020.05.035
- Duden, G. S., Gersdorf, S., & Stengler, K. (2022). Global impact of the COVID-19 pandemic on mental health services: A systematic review. Journal of Psychiatric Research, 154, 354–377. https://doi.org/10.1016/j.jpsychires.2022.08.013
- Dworakowski, O., Huber, Z. M., Meier, T., Boyd, R. L., & Horn, A. B. (2022). Emotion regulation across the lifespan: Age differences in intrapersonal and interpersonal strategies for the adjustment to the COVID-19 pandemic in four countries. Aging & Mental Health, 26(10), 2048–2053. https://doi.org/10.1080/13607863.2021.1972933
- Flor, L. S., Friedman, J., Spencer, C. N., Cagney, J., Arrieta, A., Herbert, M. E., Stein, C., Mullany, E. C., Hon, J., Patwardhan, V., Barber, R. M., Collins, J. K., Hay, S. I., Lim, S. S., Lozano, R., Mokdad, A. H., Murray, C. J. L., Reiner, R. C., Sorensen, R. J. D., … Gakidou, E. (2022). Quantifying the effects of the COVID-19 pandemic on gender equality on health, social, and economic indicators: A comprehensive review of data from March, 2020, to September, 2021. The Lancet, 399(10344), 2381–2397. https://doi.org/10.1016/S0140-6736(22)00008-3
- Goel, N., Workman, J. L., Lee, T. T., Innala, L., & Viau, V. (2014). Sex differences in the HPA axis. Comprehensive Physiology, 4(3), 1121–1155. https://doi.org/10.1002/cphy.c130054
- Groves, R. M., Presser, S., & Dipko, S. (2004). The role of topic interest in survey participation decisions. Public Opinion Quarterly, 68(1), 2–31. https://doi.org/10.1093/poq/nfh002
- Gupta, A., Zhu, H., Doan, M. K., Michuda, A., & Majumder, B. (2020). Economic burden of COVID-19 lockdown on the poor. SSRN Electronic Journal. https://doi.org/10.2139/ssrn.3642987
- Hamama-Raz, Y., Goodwin, R., Leshem, E., & Ben-Ezra, M. (2021). The toll of a second lockdown: A longitudinal study. Journal of Affective Disorders, 294, 60–62. https://doi.org/10.1016/j.jad.2021.06.080
- Hogg, B., Gardoki-Souto, I., Valiente-Gómez, A., Rosa, A. R., Fortea, L., Radua, J., Amann, B. L., & Moreno-Alcázar, A. (2023). Psychological trauma as a transdiagnostic risk factor for mental disorder: An umbrella meta-analysis. European Archives of Psychiatry and Clinical Neuroscience, 273(2), 397–410. https://doi.org/10.1007/s00406-022-01495-5
- Hunt, C., Gibson, G. C., Vander Horst, A., Cleveland, K. A., Wawrosch, C., Granot, M., Kuhn, T., Woolverton, C. J., & Hughes, J. W. (2021). Gender diverse college students exhibit higher psychological distress than male and female peers during the novel coronavirus (COVID-19) pandemic. Psychology of Sexual Orientation and Gender Diversity, 8(2), 238–244. https://doi.org/10.1037/sgd0000461
- Jones, B. A., Bowe, M., McNamara, N., Guerin, E., & Carter, T. (2021). Exploring the mental health experiences of young trans and gender diverse people during the Covid-19 pandemic. International Journal of Transgender Health, 24, 292–304. https://doi.org/10.1080/26895269.2021.1890301
- Kazlauskas, E., Gegieckaite, G., Eimontas, J., Zelviene, P., & Maercker, A. (2018). A brief measure of the International Classification of Diseases-11 adjustment disorder: Investigation of psychometric properties in an adult help-seeking sample. Psychopathology, 51(1), 10–15. https://doi.org/10.1159/000484415
- Kazlauskas, E., Zelviene, P., Lorenz, L., Quero, S., & Maercker, A. (2017). A scoping review of ICD-11 adjustment disorder research. European Journal of Psychotraumatology, 8(sup7), 1421819. https://doi.org/10.1080/20008198.2017.1421819
- Keller, A., Groot, J., Matta, J., Bu, F., El Aarbaoui, T., Melchior, M., Fancourt, D., Zins, M., Goldberg, M., & Nybo Andersen, A.-M. (2022). Housing environment and mental health of Europeans during the COVID-19 pandemic: A cross-country comparison. Scientific Reports, 12(1), 5612. https://doi.org/10.1038/s41598-022-09316-4
- Li, F., Luo, S., Mu, W., Li, Y., Ye, L., Zheng, X., Xu, B., Ding, Y., Ling, P., Zhou, M., & Chen, X. (2021). Effects of sources of social support and resilience on the mental health of different age groups during the COVID-19 pandemic. BMC Psychiatry, 21(1), 16. https://doi.org/10.1186/s12888-020-03012-1
- Lorenz, L., Perkonigg, A., & Maercker, A. (2018). A socio-interpersonal approach to adjustment disorder: The example of involuntary job loss. European Journal of Psychotraumatology, 9(1), 1425576. https://doi.org/10.1080/20008198.2018.1425576
- Lotzin, A., Aakvaag, H., Acquarini, E., Ajdukovic, D., Ardino, V., Böttche, M., Bondjers, K., Bragesjö, M., Dragan, M., Figueiredo-Braga, M., Gelezelyte, O., Grajewski, P., Javakhishvili, D., Kazlauskas, E., Knefel, M., Lueger-Schuster, B., Makhashvili, N., Mooren, T., Sales, L., … Schäfer, I. (2020). Stressors, coping and symptoms of adjustment disorder in the course of the COVID-19 pandemic – Study protocol of the European Society for Traumatic Stress Studies (ESTSS) pan-European study. European Journal of Psychotraumatology, 11(1), 1780832. https://doi.org/10.1080/20008198.2020.1780832
- Lotzin, A., Ketelsen, R., Zrnic, I., Lueger-Schuster, B., Böttche, M., & Schäfer, I. (2022). The Pandemic Stressor Scale: Factorial validity and reliability of a measure of stressors during a pandemic. BMC Psychology, 10(1), 92. https://doi.org/10.1186/s40359-022-00790-z
- Lotzin, A., Krause, L., Acquarini, E., Ajdukovic, D., Ardino, V., Arnberg, F., Böttche, M., Bragesjö, M., Dragan, M., & Figueiredo-Braga, M. (2021). Risk and protective factors, stressors, and symptoms of adjustment disorder during the COVID-19 pandemic – First results of the ESTSS COVID-19 pan-European ADJUST study. European Journal of Psychotraumatology, 12(1), 1964197. https://doi.org/10.1080/20008198.2021.1964197
- Mazza, C., Ricci, E., Biondi, S., Colasanti, M., Ferracuti, S., Napoli, C., & Roma, P. (2020). A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: Immediate psychological responses and associated factors. International Journal of Environmental Research and Public Health, 17(9), 3165. https://doi.org/10.3390/ijerph17093165
- Midões, C., & Seré, M. (2022). Living with reduced income: An analysis of household financial vulnerability under COVID-19. Social Indicators Research, 161(1), 125–149. https://doi.org/10.1007/s11205-021-02811-7
- Neelam, K., Duddu, V., Anyim, N., Neelam, J., & Lewis, S. (2021). Pandemics and pre-existing mental illness: A systematic review and meta-analysis. Brain, Behavior, & Immunity – Health, 10, 100177. https://doi.org/10.1016/j.bbih.2020.100177
- Newson, M., Zhao, Y., Zein, M. E., Sulik, J., Dezecache, G., Deroy, O., & Tunçgenç, B. (2021). Digital contact does not promote wellbeing, but face-to-face contact does: A cross-national survey during the COVID-19 pandemic. New Media & Society, 26, 426–449. https://doi.org/10.1177/14614448211062164
- Özdin, S., & Bayrak Özdin, Ş. (2020). Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. International Journal of Social Psychiatry, 66(5), 504–511. https://doi.org/10.1177/0020764020927051
- Petrova, K., & Schulz, M. (2022). Emotional experiences in technology-mediated and in-person interactions: An experience-sampling study. Cognition and Emotion, 36(4), 750–757. https://doi.org/10.1080/02699931.2022.2043244
- Petts, R. J., Carlson, D. L., & Pepin, J. R. (2021). A gendered pandemic: Childcare, homeschooling, and parents’ employment during COVID-19. Gender, Work & Organization, 28(S2), 515–534. https://doi.org/10.1111/gwao.12614
- Pierce, M., McManus, S., Jessop, C., John, A., Hotopf, M., Ford, T., Hatch, S., Wessely, S., & Abel, K. M. (2020). Says who? The significance of sampling in mental health surveys during COVID-19. The Lancet Psychiatry, 7(7), 567–568. https://doi.org/10.1016/S2215-0366(20)30237-6
- Racine, N., Hetherington, E., McArthur, B. A., McDonald, S., Edwards, S., Tough, S., & Madigan, S. (2021). Maternal depressive and anxiety symptoms before and during the COVID-19 pandemic in Canada: A longitudinal analysis. The Lancet Psychiatry, 8(5), 405–415. https://doi.org/10.1016/S2215-0366(21)00074-2
- Robinson, E., Sutin, A. R., Daly, M., & Jones, A. (2022). A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. Journal of Affective Disorders, 296, 567–576. https://doi.org/10.1016/j.jad.2021.09.098
- Rossi, R., Socci, V., Talevi, D., Mensi, S., Niolu, C., Pacitti, F., Di Marco, A., Rossi, A., Siracusano, A., & Di Lorenzo, G. (2020). COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Frontiers in Psychiatry, 11, 790. https://doi.org/10.3389/fpsyt.2020.00790
- Sevilla, A., & Smith, S. (2020). Baby steps: The gender division of childcare during the COVID-19 pandemic. Oxford Review of Economic Policy, 36(Supplement_1), S169–S186. https://doi.org/10.1093/oxrep/graa027
- Solar, O., & Irwin, A. (2010). A conceptual framework for action on the social determinants of health. World Health Organization. https://www.who.int/publications/i/item/9789241500852.
- Stieger, S., Lewetz, D., & Willinger, D. (2023). Face-to-face more important than digital communication for mental health during the pandemic. Scientific Reports, 13(1), 1. https://doi.org/10.1038/s41598-023-34957-4
- Su, Z., McDonnell, D., Wen, J., Kozak, M., Abbas, J., Šegalo, S., Li, X., Ahmad, J., Cheshmehzangi, A., Cai, Y., Yang, L., & Xiang, Y.-T. (2021). Mental health consequences of COVID-19 media coverage: The need for effective crisis communication practices. Globalization and Health, 17(1), 4. https://doi.org/10.1186/s12992-020-00654-4
- Takiguchi, Y., Matsui, M., Kikutani, M., & Ebina, K. (2023). The relationship between leisure activities and mental health: The impact of resilience and COVID-19. Applied Psychology: Health and Well-Being, 15(1), 133–151. https://doi.org/10.1111/aphw.12394
- Thomson, R. M., Igelström, E., Purba, A. K., Shimonovich, M., Thomson, H., McCartney, G., Reeves, A., Leyland, A., Pearce, A., & Katikireddi, S. V. (2022). How do income changes impact on mental health and wellbeing for working-age adults? A systematic review and meta-analysis. The Lancet Public Health, 7(6), e515–e528. https://doi.org/10.1016/S2468-2667(22)00058-5
- van Buuren, S., & Groothuis-Oudshoorn, K. (2011). Mice: Multivariate imputation by chained equations in R. Journal of Statistical Software, 45, 1–67. https://doi.org/10.18637/jss.v045.i03
- Weathers, F. W., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schnurr, P. P. (2013). PTSD Checklist for DSM-5 (PCL-5) with Criterion A. https://www.ptsd.va.gov/professional/assess-ment/adult-sr/ptsd-checklist.asp
- White, I. R., Royston, P., & Wood, A. M. (2011). Multiple imputation using chained equations: Issues and guidance for practice. Statistics in Medicine, 30(4), 377–399. https://doi.org/10.1002/sim.4067
- WHO. (2021). ICD-11 – Mortality and Morbidity Statistics (Version: 01/2023). https://icd.who.int/browse11/l-m/en
- Zelviene, P., Kazlauskas, E., & Maercker, A. (2020). Risk factors of ICD-11 adjustment disorder in the Lithuanian general population exposed to life stressors. European Journal of Psychotraumatology, 11(1), 1708617. https://doi.org/10.1080/20008198.2019.1708617