ABSTRACT
Despite the introduction of the trivalent vaccine (measles, mumps, rubella) more than 20 years ago, measles outbreaks have occurred in Europe, including Italy, due to its underutilization. In Italy mandatory vaccination was established in 2017 (Decree Law 119/2017). This study aimed at evaluating the impact of mandatory vaccination and determining the trend in vaccination coverage for measles and rubella in Italy. We retrieved data from the Annual Status Update, a form sent annually by the Italian National Verification Committee to the Regional Verification Committee for Europe, from 1st January 2013 to 31st December 2019. Since the beginning of 2013, 14,788 cases of measles have been reported, ranging from 256 (3.9 x 1,000,000) to 5,397 (88.4 x 1,000,000) compared to 259 rubella cases for the same period. From 2013 to 2015, vaccination coverage decreased for the first dose of measles (90.4% to 85.3%) and rubella vaccine (90.3% to 85.2%), but then it increased significantly, reinforced by the Italian Decree Law, reaching 94.4% in 2019. The trend for the second dose showed a decrease from 2013 to 2016 (84.1% to 82.2% for measles and 83.7% to 82.0% for rubella), but then increased significantly and reached 90.2% in 2019 for measles and 90.0% for rubella. The mandatory vaccination law has resulted in a significant increase in vaccination coverage for measles and rubella in Italy, and demonstrates encouraging progress toward the 95% target and the restriction of measles transmission. Special attention should be paid to maintaining and further improving vaccination coverage.
Introduction
Two doses of measles and rubella vaccine is the standard for all National Immunization Programs.Citation1 Achieving and maintaining high rates of vaccination coverage are key public health strategies aimed at reducing measles incidence and reaching the elimination target established by the World Health Organization (WHO) Regional Committee for Europe.Citation2–4 Specifically, the WHO has recommended two doses and a minimum 95% coverage to reach herd immunity, which also confers indirect protection on unvaccinated individuals, and prevents outbreaks.Citation5
Despite the introduction of the trivalent measles, mumps and rubella (MMR) vaccine in national vaccination schedules more than 20 years ago, its underutilization has meant that measles outbreaks have still occurred throughout Europe.Citation6 Indeed, anti-vaccination movements have become more prominent, fueled by the fear and mistrust resulting from the vaccine hesitancy phenomenon, which is defined as a delay in acceptance or refusal of vaccines despite the availability of vaccination services.Citation7–10 During the first three months of 2014, 1,197 cases of measles were notified in Europe, with 795 suspected cases reported in Italy, the country with the highest incidence (60.1% of all cases).Citation6 In 2017, a large epidemic measles outbreak occurred in Italy, mostly attributable to the decreasing uptake of measles vaccination, which caused large pockets of measles-susceptible individuals. As a result, in line with France and Germany, a mandatory vaccination strategy was considered, and a new National Vaccine Plan for the years 2017–2019 was approved.Citation11 This was followed by the National Law 119/2017, which expanded the number of mandatory vaccinations from four to ten (against polio, tetanus, diphtheria, pertussis, measles, mumps, rubella, chickenpox, hepatitis B and Haemophilus influenzae type b) and introduced administrative penalties for those parents or individuals who were hesitant about or refused vaccination.Citation12,Citation13 According to this Law, all children under 16 years are required to exhibit proof of mandatory vaccinations including measles and rubella, prior to be admitted to state schools.
Three years after the introduction of mandatory vaccination law (MLV), official data show an increase in vaccination coverage both at national and regional level, but there are conflicting issues arising from the legislation. On the one hand, maintaining an optimal level of vaccine coverage is necessary to avoid a resurgence of the related infectious diseases. On the other hand, the maintenance of mandatory MMR vaccination is debatable for ethical and/or political reasons. Within this context, quantifying the impact of the mandatory vaccination law could provide timely evidence to inform the ongoing political debate. Hence, since a comprehensive assessment of its effects is still lacking, the aim of this study was to evaluate the impact of mandatory vaccination three years after its introduction and to determine the trend of MMR vaccinations in Italy by: i) describing the epidemiological trends in measles and rubella in Italy between 2013 and 2019; ii) analyzing the coverage rates for the MMR vaccine at 24 months (first dose) and at 6 years (full vaccination cycle) of age in Italy from 2013 to 2019; iii) evaluating changes in the trends in coverage rates, particularly after the introduction of the aforementioned MVL.
Materials and methods
This observational study describes and analyses vaccination coverage for measles and rubella in Italy from 1st January 2013 to 31st December 2019, also taking into account the epidemiological features of measles and rubella cases diagnosed in the same period. Data were collected from the Annual Status Update (ASU), a form sent annually by the Italian National Verification Committee (NVC) to the Regional Verification Committee for Europe, within the project “Actions to support the National Plan for the Elimination of Measles and Congenital Rubella.” The form is divided in four sections (section 1: country measles and rubella profile; section 2: update of general programme activities by components; section 3: activities of the National verification Committee and its Secretariat; section 4: additional data on measles, rubella and congenital rubella syndrome) plus annexes and includes five core components: epidemiology, molecular data, performance of the surveillance system, immunity data and sustainability of the National Immunization Programme.Citation3,Citation14 Immunity data are collected by the Ministry of Health from the Regions with the respective administrative territories, whereas data on the incidence rates of measles and rubella are provided by the Italian Institute of Health, through the electronic platform used by the Regions in the National Integrated Surveillance System for Measles and Rubella. Measles surveillance is integrated with rubella surveillance, as both measles and rubella affect the same age groups, have similar symptoms and can be difficult to distinguish on a clinical basis. Integrated surveillance requires that cases of suspected measles that test negative to confirmatory tests are evaluated for rubella and, oppositely, cases of suspected rubella that test negative to confirmatory tests are checked for measles.Citation15
Measles and rubella case definition
Suspected measles cases were considered those with signs and symptoms consistent with measles clinical criteria [fever and maculopapular rash and cough or coryza (runny nose) or conjunctivitis (red eyes)]. Laboratory-confirmed measles cases were considered those that met the laboratory criteria for measles case confirmation. Epidemiologically linked measles cases were those that had not had adequate laboratory testing and that had been in contact with a laboratory-confirmed measles case 7–18 days before rash onset.
Suspected rubella cases were considered those with signs and symptoms consistent with rubella clinical criteria, i.e. maculopapular rash and cervical, sub-occipital or post-auricular adenopathy, or arthralgia/arthritis. Laboratory-confirmed rubella cases were those that met the laboratory criteria for rubella surveillance case confirmation. Epidemiologically linked rubella cases were defined as suspected cases that had not had adequate laboratory testing and that had been in contact with a laboratory-confirmed rubella case 12–23 days prior to disease onset.
According to WHO guidelines and European Decision 2002/253/EC23, measles and rubella cases were classified as “possible” if the case met only the clinical criteria, “probable” if the case met the clinical criteria plus an epidemiological link or “confirmed” if the case met both clinical and laboratory criteria.Citation16 The notification of measles and rubella cases is mandatory in Italy, since they are considered relevant diseases and were included in the second class of diseases subject to notification obligation by the Decree of the Ministry of Health of the 15th of December 1990.Citation17
Statistical analysis
Italy is divided into 19 administrative Regions and two autonomous provinces (APs). For the purposes of this study, Italy was divided into three territorial macro-areas containing the following Regions:Citation18
Northern Italy: Piemonte, Valle d’Aosta, Lombardia, AP of Bolzano, AP of Trento, Veneto, Friuli-Venezia Giulia, Liguria, Emilia-Romagna;
Central Italy: Toscana, Umbria, Marche, Lazio;
Southern Italy and Islands: Abruzzo, Molise, Campania, Puglia, Basilicata, Calabria, Sicilia, Sardegna.
Epidemiological data on measles and rubella are presented descriptively. Comparisons of the incidence of measles cases over time were performed by the χ2 test. Immunization coverage was detailed in percentages; its trends over time were displayed using the rates of vaccine coverage over the study years. The χ2 test was used to analyze differences in vaccine coverage between 2016 (the last year before the introduction of the MVL) and the following calendar years. The significance level was set to p < .05. Analyses were performed with STATA 13 (StataCorp LLC, 4905 Lakeway Drive College Station, Texas, USA).
Moreover, joinpoint regression models were used to identify statistically significant changes in trends (increasing/decreasing) in measles and rubella vaccination coverage during the period 2013–2019 in Italy. With vaccination coverage rates as inputs, this model is able to identify the year(s) after which a significant trend change occurs.Citation19 Joinpoint Regression Programme version 4.8.0.1 was used to perform the analysis [Joinpoint Regression Program, Version 4.8.0.1 – April 2020; Statistical Methodology and Applications Branch, Surveillance Research Program, National Cancer Institute].
Results
Incidence of measles and rubella in Italy from 2013 to 2019
Measles: national level
Since the beginning of 2013, 14,788 cases of measles have been reported in Italy, ranging from 256 to 5,397 (data not shown). The age groups most affected were in the range 15–39 years old. Overall, in the period January 2013 to December 2019, 73.8% of reported cases were laboratory confirmed, 13.0% were classified as probable cases and 13.2% as possible ones (data not shown). Transmission occurred in families, nosocomial settings, schools and nomadic settlements.
Compared to 2017, which represented the year with the highest epidemic peak (88.4 cases per 1,000,000 inhabitants), the frequency of measles cases among Italian Regions/APs was significantly lower in 2018 (p < .001) and 2019 (p < .001) (data not shown).
Measles: regional level
In 2013, the highest level of incidence was observed in the AP of Bolzano (208.7 per 1,000,000 inhabitants), followed by Liguria and Piemonte Regions (). Liguria showed the highest level of incidence in 2014 with 123.7 cases per 1,000,000 inhabitants, followed by Piemonte, Sardegna and Emilia-Romagna. The incidence rate decreased in 2015 across all regions, with the highest level in the AP of Bolzano with 44.4 cases per 1,000,000 inhabitants, and then in 2016 the number of cases began to rise again with the highest incidence rate reported for Calabria (61.9 cases/1,000,000 inhabitants), followed by Campania, Umbria, and the AP of Trento. The Region of Lazio reported the highest incidence rate (333.3 cases/1,000,000) in 2017, followed by Abruzzo and Piemonte. In 2018, about 44% of cases were reported in Sicilia, which also reported the highest incidence (238.9 cases per 1,000,000 inhabitants), while in 2019 the incidence rates decreased dramatically with the highest incidence (87.9 cases per 1,000,000 inhabitants) reported for Lazio ().
Table 1. Measles incidence (x 1,000,000) in Italy, by Regions
Rubella: national and regional level
Since the beginning of 2013, 259 cases of rubella have been reported: 65 in 2013, 26 in 2014, 27 in 2015, 30 in 2016, 68 in 2017, 21 in 2018 and 22 in 2019 (data not shown). Overall, 41% of cases were laboratory confirmed. Incidence rates for each Region are detailed in .
Table 2. Rubella incidence (x 1,000,000) in Italy, by Regions
Measles vaccination coverage
National level
Coverage for the first dose of measles vaccine in Italy decreased from 2013 (90.4%) to 2015 (85.3%) – a remarkable 5.1% difference – after which it increased consistently, in particular after introduction of the MVL, reaching 94.4% in 2019. From 2016, increases in annual percentages reached statistical significance (). Considering the second dose, the trend decreased from 2013 (84.1%) to 2016 (82.2%), after which it reversed from 2017 and reached 90.2% in 2019: again, increases in annual percentages were statistically significant ().
Table 3. Percentage of vaccinated children against measles in Italy in 2016 and comparison with the following calendar years after the introduction of the Decree Law 119/2017
The joinpoint model confirmed that the trend in vaccination coverage for the first dose of measles-containing vaccine from 2013 to 2019 had one break point in 2015 (which was the year in the study period showing the lowest coverage): from 2013 to 2015 there was a non-significant reduction in vaccination coverage with an average annual 2.31% decrease; from 2015 to 2019 there was a significant 2.51% increase per year ().
Figure 1. Joinpoint analysis of the trend in vaccination rates for measles and rubella between 2013 and 2019 in Italy. a, trend in vaccination coverage for first dose of measles vaccine; b, trend in vaccination coverage for second dose of measles vaccine; c, trend in vaccination coverage for first dose of rubella vaccine; d, trend in vaccination coverage for second dose of rubella vaccine. The use of asterisks (*) indicates that the Slope is significantly different from zero at the alpha = 0.05 level. Final Selected Model: 1 Joinpoint.
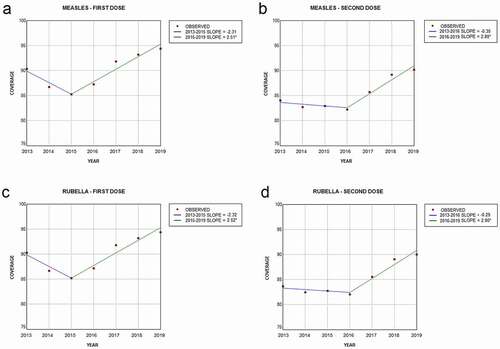
The trend in vaccination coverage for the second dose of measles-containing vaccine from 2013 to 2019 showed only one break point, in 2016 (). From 2013 to 2016, there was a non-significant reduction in vaccination coverage with an average annual 0.35% decrease, whereas from 2016 to 2019 there was a significant 2.80% increase per year.
Regional level
Regarding the single Regions/APs in Northern Italy, almost all of them showed similar trends in vaccination coverage (), with the exception of the AP of Bolzano where percentages for both doses were lower and far from the target established by the WHO (first dose, increasing from 68.9% in 2013 to 75.5% in 2019; second dose, dropping from 73.2% in 2013 to 59.8% in 2015 and then increasing to 78.2% in 2019). Additionally, the region of Valle d’Aosta experienced the lowest percentage for the first dose in 2014 (77.6%) and the highest in 2019 (91.5%).
Figure 2. Trends in coverage for first (a) and second (b) dose of measles vaccine (2013–2019) by Region. Each concentric circle represents one year, starting with 2013 in the center.
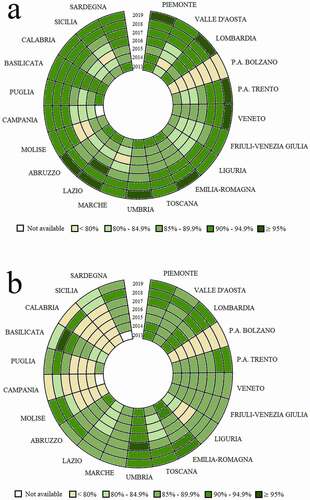
In central Italy, the Region of Lazio experienced several reductions in coverage rate between the first and second doses in any given year (first dose, from 90.9% in 2013 to 84.5 in 2015 and 95.7% in 2019; second dose, from 81.9% in 2013 to 81.0% in 2014 and 85.4% in 2019). Conversely, Umbria and Marche reported some years with the opposite and greater shortfalls, where vaccination coverage percentages for the first dose were lower than those of the second.
The pattern of vaccination coverage appeared heterogeneous in Southern Italy and Islands, since several regions showed percentages that differed from the overall trend in Italy: in this context, large differences between the first and second dose were registered by Molise (first dose, from 87.6% in 2013 to 73.5 in 2016 and 93.4% in 2019; second dose, from 77.1% in 2013 to 59.8% in 2016 and 92.6% in 2019), Campania (first dose, from 83.7% in 2014 to 80.8 in 2015 and 94.7% in 2019; second dose, from 73.9% in 2014 to 79.0% in 2019), Calabria (first dose, from 87.6% in 2013 to 83.2 in 2014 and 93.1% in 2019; second dose, from 64.9% in 2013 to 91.2% in 2018 and 78.6% in 2019) and Sicilia (first dose, from 89.0% in 2013 to 79.2 in 2015 and 92.2% in 2019; second dose, from 54.6% in 2013 to 81.4% in 2019).
In 2019, eight regions exceeded the 95% target for the first dose.
Rubella vaccination coverage
National level
Coverage for the first dose of rubella vaccine in Italy underwent a 5.1% decrease from 2013 (90.3%) to 2015 (85.2%), while from 2016 the trend reversed, increasing to 94.4% in 2019. Indeed, from 2016 to 2019, vaccination coverage increased significantly year-on-year (). For the second dose, the trend showed a decrease from 2013 (83.7%) to 2016 (82.0%), but then reversed from 2017 and reached 90.0% in 2019. Again, the annual increases in coverage from 2016 were statistically significant ().
Table 4. Percentage of vaccinated children against rubella in Italy in 2016 and comparison with the following calendar years after the introduction of the Decree Law 119/2017
The joinpoint model confirmed one break point in 2015 for the trend in vaccination coverage for the first dose of rubella vaccine from 2013 to 2019 (). From 2013 to 2015 there was a non-significant reduction in vaccination coverage with an average annual 2.32% decrease, whereas from 2015 to 2019 there was a significant 2.52% increase per year. Conversely, the trend in vaccination coverage for the second dose of rubella-containing vaccine from 2013 to 2019 showed one break point in 2016 (). From 2013 to 2016 there was a non-significant reduction in vaccination coverage with an average annual 0.29% decrease, whereas from 2016 to 2019 there was a significant 2.80% increase per year.
Regional level
At the regional level, almost all Regions/APs in the Northern area showed similar trends in vaccination coverage, again with the exception of the AP of Bolzano, whose percentages for both doses were lower and far short of the WHO target (first dose, decreasing from 68.9% in 2013 to 75.5% in 2019; second dose, decreasing from 72.5% in 2013 to 59.8% in 2015 and then increasing to 77.9% in 2019) (). Also, Valle d’Aosta experienced its lowest percentage coverage for the first dose in 2014 (77.1%) and its highest in 2019 (91.5%).
Figure 3. Trends in vaccination coverage for first (a) and second (b) dose of rubella vaccine (2013–2019) by Region. Each concentric circle represents one year, starting with 2013 in the center.
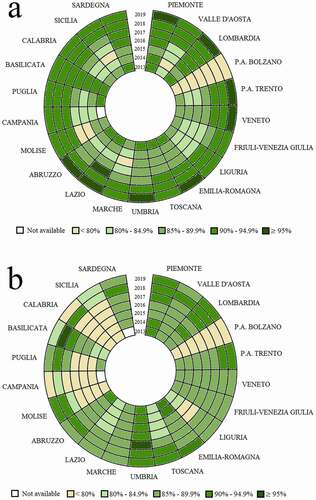
In central Italy, Lazio experienced a number of shortfalls between the first and second doses (first dose, decreasing coverage from 90.9% in 2013 to 84.5% in 2015, then markedly higher at 95.7% in 2019; second dose, decreasing from 81.9% in 2013 to 81.0% in 2014 and then 85.2% in 2019), whereas Umbria and Marche have reported for some years with the opposite and greater differences, since vaccination coverage percentages for the first dose were lower than those for the second.
The pattern of vaccination coverage appeared to be heterogeneous in Southern Italy and Islands, since more regions have shown levels of vaccination coverage that differ from the overall trend in Italy. In this context, wider differences between the first and second dose were seen in Molise (first dose, coverage decreasing from 87.6% in 2013 to 73.5% in 2016, but 93.4% in 2019; second dose, decreasing from 77.1% in 2013 to 50.8% in 2016, and increasing to 92.6% in 2019), Campania (first dose, decreasing from 83.7% in 2014 to 80.8% in 2015, then 94.7% in 2019; second dose, increasing from 73.9% in 2014 to 78.9% in 2019), Calabria (first dose, down from 87.6% in 2013 to 83.2% in 2014, then 93.1% in 2019; second dose, ranging from 64.9% in 2013 to 91.2% in 2018 and 78.6% in 2019) and Sicilia (first dose, decreasing from 89.0% in 2013 to 79.2% in 2015, but 92.2% in 2019; second dose, ranging from 54.6% in 2013 to 81.4% in 2019).
Discussion
This study describes the epidemiological trends of measles and rubella cases in Italy from 2013 to 2019 and analyses the coverage rate for the MMR vaccine over this period, with a specific focus on any changes in the trend after the introduction of the Decree Law for mandatory vaccination in 2017.
Measles cases in Italy, during the period 2013–2019, showed a cyclical trend with epidemic peaks in 2013 and 2014, a decrease in the number of cases reported in 2015, a slight recovery in 2016, and a new high peak of cases in 2017. In particular, the prevalence of cases among young adults, including healthcare workers,Citation20 shows that vaccination coverage in this age category was insufficient. A similar trend was observed for rubella, but with a substantially lower incidence. At the regional level, the incidence of measles cases was heterogeneous. In 2013, three Regions reported about 70% of cases. In 2014, the largest number of cases occurred in six Regions, together comprising 81% of cases. In 2015, approximately 75% of the cases were reported by five Regions whereas in 2016, 80% of reported cases occurred in six Regions and, in 2017, 90% of reported cases were reported by eight Regions. After introduction of the mandatory vaccination law, the distribution pattern of cases throughout the country changed, such that most outbreaks occurred in just a few Regions. Indeed, in 2018, Sicily reported 44.2% of cases and in 2019, two Regions (Lazio and Lombardia) reported over half of cases.
It has been estimated that vaccination against measles has prevented 21.1 million deaths worldwide from 2000 to 2017.Citation21 The positive effects of vaccination are so well recognized that measles was planned for elimination in the Global Vaccine Action Plan 2015–2020.Citation22 Nevertheless, population vaccination uptake rates declined throughout Europe so that some countries were forced to make some vaccinations mandatory. Using data from the European Center for Disease Prevention and Control and the World Health Organization, Vaz et al.Citation23 found that mandatory vaccination was associated with a 3.7 (95% confidence interval [CI]: 1.7 to 5.7) percentage point higher prevalence of measles vaccination when compared with countries that did not have mandatory vaccination. Additionally, mandatory vaccination was associated with decreased measles incidence only for countries without nonmedical exemptions.Citation23 In the Italian context, there are four main possible reasons for the decrease in vaccination coverage: i) the austerity measures introduced across Italy from 2010, causing a special suffering of prevention activities.Citation24 In fact, the Italian regions/APs experiencing the largest drop in MMR coverage were those where the largest financial cuts occurred;Citation25 ii) some questionable Court sentences, such as that which awarded vaccine-injury compensation for a case of autism;Citation26 iii) the growth of no-vax movements; iv) some decisions of the “Agenzia Italiana del Farmaco,” the Italian Medicines Agency: for example, that to withdraw some batches of adjuvanted trivalent influenza vaccine in November 2014, because of two deaths within 48 hours of vaccine administration.Citation27 Other reasons that might reinforce vaccine hesitancy include unsubstantiated opinions about the safety and side-effects of the MMR vaccine,Citation28,Citation29 or difficulties complying with vaccine delivery schedules (i.e., providing multiple vaccines to young recipients simultaneously and within a tight time frame).
Two considerations about vaccination coverage, the first at the national level and the second at the regional level, can be drawn from our analysis: i) at the national level, for the first dose of measles or rubella vaccine, the MVL seems to have reinforced a trend that was already in progress, probably as a result of the greater attention devoted to the problem and to the vaccination campaigns after the decrease in coverage recorded in 2015; for the second dose of measles or rubella vaccine the National Law seems to have been critical in reversing the trend from decreasing to significantly increasing vaccine uptake; ii) at the regional level, prior to the introduction of the Law, coverage for measles and rubella vaccines was heterogeneous. After its implementation, differences in measles vaccination coverage among Regions/APs were attenuated: although a range still persists (from 75.5% in the AP of Bolzano to 96.1% in Tuscany), in 2019 almost no region had coverage less than 91% and eight regions had a coverage greater than 95%, as recommended by the WHO.Citation30
Recently, whether mandatory vaccination for measles, mumps, rubella and chicken pox should be continued has been the subject of political debate. An opportunity to withdraw the requirement for mandatory vaccination was contained within Law 119/2017 itself, with a deadline of three years (i.e. August 2020) after its implementation. However, according to an ad hoc recommendation edited by the NITAG (National Immunization Technical Advisory Group), full implementation of the Law, although advanced and implemented in all Regions, appears still not to be complete; moreover, the NITAG has suggested that, in the absence of more accurate information, any consideration is likely also to be incomplete, exposing policy makers to the risk of making imperfect or untimely decisions.Citation31 For these reasons, the law has not been abrogated, but it is worth mentioning that this decision was taken during the coronavirus disease 2019 (COVID-19) pandemic. Public health measures to control this emergency, based on social distancing and quarantine rules, could cause decreased access to immunization services. In the United States, for example, vaccination coverage has decreased for most vaccinations except for those administered in the hospital setting.Citation32 In England, MMR vaccination coverage in 2020 was 19.8% lower than in the same period in 2019.Citation33 Restrictive measures against SARS-CoV-2 also resulted in decreased vaccination coverage in Italy.Citation34 In a recent survey, almost all participating Local Health Authorities claimed to have witnessed a decrease in vaccinations during the COVID-19 emergency, largely because vaccination activities were suspended to restrict the transmission of SARS-CoV-2 virus in vaccination centers and because health personnel were reallocated to combat the pandemic.Citation34 Hence, although only 103 measles cases occurred from 1 January to 31 December 2020 across the whole of ItalyCitation35 probably due also to social distancing and any other community control measures adopted to control COVID-19,Citation36 but under-diagnoses and under-reporting during the pandemic should be excluded: continuous monitoring will help to identify the causes of this phenomenon, mainly when containment measures are lifted. Moreover, reinstating vaccination programs will be essential to avoid a resurgence in measles over the next few years: the main strategies for achieving this naturally include restoring the vaccination services themselves, but also strengthening communication programmes to address vaccine misinformation, and expanding routine vaccination services to reach unvaccinated people.Citation34 Additional strategies could include: i) expansion of time slots and opening days of vaccination clinics to increase coverage in all age groups; ii) activation of mobile teams to support the local offer (especially for areas with lower population density or disadvantaged areas); iii) organization of vaccination sessions in schools, using spaces that comply with anti-COVID measures; iv) organization of vaccination sessions for adults in outdoor spaces with a “drive-through” system, already used for SARS-CoV-2 swabs with good results; v) supporting the vaccination of healthcare workers; vi) supporting vaccinations in women before and after pregnancy.
This paper has some strengths and limitations. To the best of our knowledge, this is the first attempt to assess trends and changes in measles and rubella vaccination coverage at the national and subnational levels in Italy, with the aim of assessing the impact of the Law on mandatory vaccination. Indeed, we provided a comprehensive description of the incidence and the vaccination coverage rates for measles and rubella in Italy over the years 2013–2019. Also, we used regional and national data collected through the ASUs and Synthetic Regional Reports, which are part of the official material annually requested by the WHO to support the epidemiological analysis and the identification of weaknesses and strengths in regional elimination plans.Citation37 Conversely, the main limitation of this study is represented by the heterogeneity of data between regions. Differences between regions might relate to disparities in the timing of compliance with mandatory vaccination requirements due to differences in the organization of the respective services, or be due to socioeconomic inequalities and different educational approaches. Decentralization is another factor that could impact prevention activities leading to significant differences among regional health services.Citation14 Even though these differences are not strictly a limitation of our approach, but are a consequence of the peculiarities of the Italian National Health Service, they may have affected our analysis.
To conclude, this study has shown that the application of the MVL has resulted in a significant increase in vaccination coverage for measles and rubella in Italy, with important consequences for the 95% target, and has resulted in the restriction of measles transmission. Nevertheless, to avoid indirect negative consequences of the COVID-19 pandemic, special attention should be paid to the further maintenance and improvement of MMR vaccination coverage.
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
Acknowledgments
Joinpoint Regression Programme version 4.8.0.1 was provided by the National Cancer Institute and was downloaded from https://surveillance.cancer.gov/joinpoint/download.
Additional information
Funding
References
- Adamo G, Sturabotti G, D’Andrea E, Baccolini V, Romano F, Iannazzo S, Marzuillo C, Villari P. The end of measles and congenital rubella: an achievable dream? Ann Ig. 2017;29(1):1–10. doi:10.7416/ai.2017.2128.
- World Health Organization. Framework for verifying elimination of measles and rubella. Weekly Epidemiological Record. 2013;88:89–100. [accessed 2020 Oct 12]. https://apps.who.int/iris/rest/bitstreams/959204/retrieve .
- Adamo G, Baccolini V, Massimi A, Barbato D, Cocchiara R, Di Paolo C, Mele A, Cianfanelli S, Angelozzi A, Castellani F, et al. Towards elimination of measles and rubella in Italy: progress and challenges. PLoS One. 2019;14(12):e0226513. doi:10.1371/journal.pone.0226513.
- Adamo G, Baccolini V, Marzuillo C, Sturabotti G, Villari P. Slow progress in measles and rubella elimination in Italy. Epidemiol Biostat Public Health. 2016;13:2015–16. doi:10.2427/12075.
- World Health Organization. Measles vaccines: WHO position paper. Weekly Epidemiological Record. 2009;35:349–60. [accessed 2020 Oct 12]. http://www.who.int/wer/2009/wer8435.pdf .
- Amendola A, Bubba L, Piralla A, Binda S, Zanetti A, Pariani E, Ranghiero A, Premoli M, Pellegrinelli L, Coppola L, et al. Surveillance and vaccination coverage of measles and rubella in Northern Italy. Hum Vaccin Immunother. 2015;11(1):206–13. doi:10.4161/hv.35865.
- MacDonald NE. SAGE working group on vaccine hesitancy. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–64. doi:10.1016/j.vaccine.2015.04.036.
- Rosso A, Massimi A, De Vito C, Adamo G, Baccolini V, Marzuillo C, Vacchio MR, Villari P. Knowledge and attitudes on pediatric vaccinations and intention to vaccinate in a sample of pregnant women from the City of Rome. Vaccine. 2019;37(14):1954–63. doi:10.1016/j.vaccine.2019.02.049.
- Rosso A, Massimi A, Pitini E, Nardi A, Baccolini V, Marzuillo C, De Vito C, Villari P. Factors affecting the vaccination choices of pregnant women for their children: a systematic review of the literature. Hum Vaccin Immunother. 2020;16(8):1969–80. doi:10.1080/21645515.2019.1698901.
- Ministero della Salute. Piano Nazionale di Prevenzione Vaccinale 2012-2014. [accessed 2020 Oct 12]. https://www.salute.gov.it/imgs/C_17_pubblicazioni_1721_allegato.pdf .
- Ministero della Salute. Piano Nazionale di Prevenzione Vaccinale 2017-2019. [accessed 2020 Oct 12]. http://www.salute.gov.it/imgs/C_17_pubblicazioni_2571_allegato.pdf .
- Legge 31 Luglio. N. 119; 2017 [accessed 2020 Oct 12]. https://www.trovanorme.salute.gov.it/norme/dettaglioAtto?id=60201 .
- Signorelli C, Guerra R, Siliquini R, Ricciardi W. Italy’s response to vaccine hesitancy: an innovative and cost effective National Immunization Plan based on scientific evidence. Vaccine. 2017;35(33):4057–59. doi:10.1016/j.vaccine.2017.06.011.
- Adamo G, Sturabotti G, Baccolini V, De Soccio P, Prencipe GP, Bella A, Magurano F, Iannazzo S, Villari P, Marzuillo C. Regional reports for the subnational monitoring of measles elimination in Italy and the identification of local barriers to the attainment of the elimination goal. PLoS One. 2018;13(10):e0205147. doi:10.1371/journal.pone.0205147.
- Italian ministry of health - national integrated surveillance system for measles and rubella. [Ministero della Salute – sorveglianza integrata morbillo e rosolia]. 2019 Dec [accessed 2021 June 1]. https://www.salute.gov.it/portale/malattieInfettive/dettaglioContenutiMalattieInfettive.jsp?lingua=italiano&id=4776&area=Malattie%20infettive&menu=sorveglianza#:~:text=La%20sorveglianza%20integrata%20prevede%20che,conferma%20vengano%20testati%20per%20morbillo.
- World Health Organization. Manual for the laboratory diagnosis of measles and rubella virus infection. [accessed 2020 Oct 12]. http://www.who.int/ihr/elibrary/manual_diagn_lab_mea_rub_en.pdf .
- Decree of the Ministry of Health of the 15th December 1990. [accessed 2021 Mar 25]. https://www.epicentro.iss.it/infettive/pdf/DM_151290.pdf .
- National Institute for Statistics (ISTAT). Geographical divisions. [Istituto nazionale di statistica (ISTAT). Documenti con Tag: ripartizioni geografiche]. [accessed 2021 Jun 1]. https://www.istat.it/it/archivio/ripartizioni+geografiche .
- Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med 2000;19(3):335–51. Erratum in: Stat Med 2001;20(4):655. doi:10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z.
- Baccolini V, Sindoni A, Adamo G, Rosso A, Massimi A, Bella A, Filia A, Magurano F, Marzuillo C, Villari P, et al. Measles among healthcare workers in Italy: is it time to act? Hum Vaccin Immunother. 2020;16(11):2618–27. doi:10.1080/21645515.2020.1737458.
- World Health Organization (WHO). Measles. [accessed 2020 Oct 12]. http://www.who.int/mediacentre/factsheets/fs286/en/ .
- World helath organization – global vaccine action plan. [accessed 2021 May 27]. https://www.who.int/teams/immunization-vaccines-and-biologicals/strategies/global-vaccine-action-plan .
- Vaz OM, Ellingson MK, Weiss P, Jenness SM, Bardají A, Bednarczyk RA, Omer SB. Mandatory vaccination in Europe. Pediatrics. 2020;145(2):e20190620. doi:10.1542/peds.2019-0620.
- Rosso A, De Vito C, Marzuillo C, Massimi A, D’Andrea E, Villari P. The negative effect of financial constraints on planning prevention activities: some evidence from the Italian experience. Eur J Public Health. 2015;25(6):1117–19. doi:10.1093/eurpub/ckv087.
- Toffolutti V, McKee M, Melegaro A, Ricciardi W, Stuckler D. Austerity, measles and mandatory vaccination: cross-regional analysis of vaccination in Italy 2000-14. Eur J Public Health. 2019;29(1):123–27. doi:10.1093/eurpub/cky178.
- Court of Rimini, decision n. 148/2010, Role 0474/2010; Cron. 886/2012. [accessed 2020 Oct 12]. http://www.quotidianosanita.it/allegati/allegato8730279.pdf .
- Levi M, Sinisgalli E, Lorini C, Santomauro F, Chellini M, The BP. “Fluad Case” in Italy: could it have been dealt differently? Hum Vaccin Immunother. 2017;13(2):379–84. doi:10.1080/21645515.2017.1264738.
- Gowda C, Schaffer SE, Kopec K, Markel A, Dempsey AF. Does the relative importance of MMR vaccine concerns differ by degree of parental vaccine hesitancy?: an exploratory study. Hum Vaccin Immunother. 2013;9(2):430–36. doi:10.4161/hv.22065.
- Luthy KE, Beckstrand RL, Callister LC. Parental hesitation in immunizing children in Utah. Public Health Nurs. 2010;27(1):25–31. doi:10.1111/j.1525-1446.2009.00823.x.
- quotidianosanita.it. Vaccini. Crescono le coperture nel. 2019. [accessed 2020 Oct 12]. http://www.quotidianosanita.it/studi-e-analisi/articolo.php?articolo_id=87721&fr=n .
- quotidianosanità.it. Governo e Parlamento. [accessed 2020 Oct 12]. http://www.quotidianosanita.it/governo-eparlamento/articolo.php?articolo_id=87178&fr=n .
- Bramer CA, Kimmins LM, Swanson R, Kuo J, Vranesich P, Jacques-Carroll LA, Shen AK. Decline in child vaccination coverage during the COVID-19 pandemic - michigan care improvement registry, May 2016-May 2020. MMWR Morb Mortal Wkly Rep 2020;69(20):630–31. PMID: 32437340. doi:10.15585/mmwr.mm6920e1.
- McDonald HI, Tessier E, White JM, Woodruff M, Knowles C, Bates C, Parry J, Walker JL, Scott JA, Smeeth L, et al. Early impact of the coronavirus disease (COVID-19) pandemic and physical distancing measures on routine childhood vaccinations in England, January to April 2020. Euro Surveill. 2020;25(19):2000848. doi:10.2807/1560-7917.ES.2020.25.19.2000848.
- Ministero della Salute – vaccinazioni. [accessed 2020 Oct 12]. http://www.normativasanitaria.it/jsp/dettaglio.jsp?id=75346.
- Morbillo and Rosolia News – aggiornamento mensile. [accessed 2021 Apr 12]. https://www.epicentro.iss.it/morbillo/bollettino/RM_News_2020_63.pdf .
- Nicolay N, Mirinaviciute G, Mollet T, Celentano LP, Bacci S. Epidemiology of measles during the COVID-19 pandemic, a description of the surveillance data, 29 EU/EEA countries and the United Kingdom, January to May 2020. Euro Surveill. 2020;25(31):2001390. doi:10.2807/1560-7917.ES.2020.25.31.2001390.
- World Health Organization (WHO) Regional Office for Europe. A report on the epidemiology of selected vaccine-preventable diseases in the European Region. WHO EpiBrief. 2018;1:1–16. [accessed 2021 Apr 12]. http://www.euro.who.int/__data/assets/pdf_file/0009/370656/epibrief-1-2018-eng.pdf.

