 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
Background
College students are one of the susceptible population of Hepatitis B virus (HBV) infection. We aim to delineate HBV infection seromarkers among college freshmen and to evaluate immunological response of vaccination immunization for hepatitis B vaccine (HepB).
Methods
A simple random sampling method was adopted to select subjects and who met the ”inclusion and exclusion criteria” and who with history of vaccination were selected as the observation objects. HBsAg and anti-HBs levels were detected before revaccination. Subjects with negative anti-HBs before immunization were inoculated with 20 ug HepB according to the 0-1-6 procedure and those with weak positive anti-HBs before immunization were inoculated with 1-dose 20 ug HepB. Anti-HBs levels were detected after HepB booster. Combined with the results of anti-HBs, their immune response to HepB and influencing factors in freshmen were investigated. Anti-HBs before immunization was negative and ≥10 m IU/ml after immunization was considered positive conversion; anti-HBs before immunization was weak positive and anti-HBs≥100 m IU/ml after immunization was also considered positive conversion.
Results
A total of 10645 freshmen were included. The total rate of HBsAg carriers was 0.6% (63/10645), and the strong positive rate of anti-HBs was 16.1% (1706/10645), the weak positive rate was 14.4% (1526/10645).1286 freshmen were vaccinated with HepB and completed the questionnaire survey. About 79.0% (154/195) of freshmen’s anti-HBs turned strong positive after receiving 1-dose HepB and 100.0% (1091/1091) turned positive after receiving 3-doses HepB. The Geometrical Mean Titer (GMT) of anti-HBs was significantly influenced by gender, registration and the immunization doses of HepB.
Conclusion
The HBsAg carrying rate and anti-HBs positive rate of college freshmen were low, and the HepB has a good effect on the immunity of college freshmen. Increasing the immunization rate of HepB is very important for the prevention and control of hepatitis B.
1. Introduction
Hepatitis B virus (HBV) can cause hepatitis B, cirrhosis of the liver and even liver cancer, it is a serious global public health problem.Citation1 According to the World Health Organization, globally, in 2015, an estimated 257 million people were living with chronic HBV infection. Viral hepatitis caused 1.34 million deaths in 2015, a number comparable to deaths caused by tuberculosis and higher than those caused by HIV. Most viral hepatitis deaths in 2015 were due to chronic liver disease (720 000 deaths due to cirrhosis) and primary liver cancer (470 000 deaths due to hepatocellular carcinoma).Citation2 HBV is the most common carcinogenic agent of infection, and 30% of HBV infection-related liver cancer results from HBV infections acquired vertically in the neonatal period.Citation3 Currently, there is treatment for HBV infection, but the most effective and cost-beneficial way to prevent disease is vaccination. Since the implementation of hepatitis B vaccine (HepB) immunization strategy in China in 1992 for nearly 30 years, the epidemiological effect has been confirmed,Citation4 the prevalence of HBV surface antigen (HBsAg) in children under 5 years of age decreased from 9.7% in 1992 to 0.3% in 2014.Citation5,Citation6 However, in 2014, the national hepatitis B seroepidemiological survey of 1–29 years old showed that the HBsAg detection rate of 5–14 years old and 15–29 years old was 0.9% and 4.4%, respectively,Citation7 suggesting that college students may be at the risk of acquiring HBV. Another reason is that in order to avoid discrimination and cancel the hepatitis B related test for enrollment, the chances of college students being infected with HBV are relatively increased. HBV infection seriously harms the physical and mental health of college students and to a certain extent affects the interpersonal relationship, social adaptability and employment of college students.
In fact, the majority of freshmen had been vaccinated with HepB before entering the university, and the seroepidemiological characteristics of HepB were of concern. In this regard, very much prospective and cross-sectional studies from high- and low-endemic areas of HBV infection were conducted. The results of these studies showed that neonatal HepB vaccination was highly efficacious in preventing vertical transmission and provides long-term immunological memory even with loss of protective antibody titers.Citation8,Citation9 Therefore, periodic serological testing or booster injection among general population and low-risk subjects were not recommended. However, several studies have shown that the prevalence of HBsAg in people aged 1–29 years increases with ageCitation10 and a significant proportion of complete vaccines may have lost their immunological memories against HBsAg.Citation11 With age, risk factors such as sexual transmission, and intravenous drug use increase. Relevant studies at home and abroad have shown that with the increase of age, the positive rate of anti-HBs gradually decreases,Citation12,Citation13 and the antibody titer gradually decreases,Citation14 which also suggests that we cannot protect the recipients from HBV permanently by relying solely on the inoculation of HepB at birth. Booster doses are recommended for those without seroconversion, especially children who live in school with other students or have family members with positive HBsAg.Citation15 The peak of vaccine-induced anti-HBs titers appeared 1 month after the initial inoculation of HepB, and decreased rapidly in the following time.Citation16 Adult HepB vaccination has a good immune effect, economic benefits and social benefits,Citation17,Citation18 and it is very important to reduce the incidence and mortality of hepatitis B in the whole population in China.Citation19 The United States Advisory Committee on Immunization Practices, the Canadian National Advisory Committee on Immunization, and the European Consultative Group all recommend that adults do not need routine booster immunization for HepB. However, people at high risk of exposure need to be treated with caution, such as medical surgeons, kidney dialysis workers, homosexuals, people with hepatitis B in their families, and so on. Antibody levels need to be checked regularly and enhanced immunization should be implemented. In the face of the changing global hepatitis B epidemic, long-term follow-up studies are needed if new hepatitis B guidance strategies are to be proposed.
The objectives of this present study were to delineate seroepidemiology of HBV in college freshmen in Hangzhou, China, and to evaluate immunological response of booster immunization for HepB, for improving immunization strategy of HepB and providing a scientific basis for the prevention and control of hepatitis B among college students.
2. Materials and methods
2.1. Setting
In this study, a simple random sampling method was adopted to select healthy freshmen enrolled in 2019 from three universities in Hangzhou. Serum was collected to detect anti-HBs baseline level before HepB immunization during the entrance physical examination of freshmen, and whose basic demographic data, including age, gender and region, were derived from the physical examination system.
According to the results of anti-HBs before immunization, the subjects were divided into three groups: anti-HBs strong positive, anti-HBs weak positive and anti-HBs negative. The ‘strong positive’ is anti-HBs ≥100 mIU/mL, ‘weak positive’ is anti-HBs ≥10 mIU/mL and anti-HBs <100 mIU/mL, ‘negative’ is anti-HBs <10 mIU/mL. Subjects who met the “inclusion and exclusion criteria” were selected as the observation objects. The subjects with negative anti-HBs before immunization were inoculated with 20 μg HepB according to the 0-1-6 procedure and those with weak positive anti-HBs before immunization were inoculated with one dose. All the blood samples were extracted one month after completion of 1-dose vaccination for weak positive subjects and 3-doses vaccination for negative subjects to detect the positive conversion of anti-HBs and the levels of the Geometrical Mean Titer (GMT) after immunization with HepB. Meanwhile, a questionnaire survey was conducted to obtain the basic information of the subjects who were boosted, their previous history of HepB vaccination, infectious history, allergy history and other information including gender, age, height, weight, BMI and so on. Finally, combined with the results of serum anti-HBs detection in the laboratory, the immune responses of different booster policies for HepB and influencing factors in college freshmen were investigated.
In particular, the whole process of quality control was carried out to ensure the work quality of this study.
2.2. Target population and data collection
2.2.1. Status of HBV infection and seromarkers among college freshmen
This study was based on the current situation of HBsAg carrying rate in people over 15 years old. A sample size at least 9225 was included for cross-sectional investigation based on the formula: (α = 0.05, Z = 1.96, δ = 0.1P, P: the positive rate of HBsAg in the 15–29 year old group was 4.4%, the positive rate of anti-HBs in the 15–29 year old group was 56.9%,Citation10 and the pre-survey anti-HBs weak positive rate of the 2019 freshmen in Hangzhou was 16.5% (990/6000)).
Firstly, three comprehensive universities were randomly selected in Hangzhou City. Secondly, all freshmen who participated in the entrance physical examination in the three universities were collected for blood samples and isolated serums for antibody detection. Then, some freshmen were randomly selected for questionnaire survey to obtain basic information, previous vaccination history, infectious history, allergy history and other information of college students. In all, 10645 college freshmen were included in this study for seroepidemiological survey.
2.2.2. Immune effectiveness evaluation of different vaccination strategies for HepB in college freshmen
Inclusion criteria: (1) According to the results of anti-HBs and HBsAg before immunization, HBsAg-negative, anti-HBs<100 mIU/ml; (2) Normal liver function; (3) no previous history of hepatitis B infection; (4) No history of other prophylactic biological products and immunoglobulin inoculation during the study period or within 14 days before the study; (5) Who voluntarily received HepB inoculation.
Exclusion criteria: (1) Patients with severe allergic reactions in the past; (2) Allergic to any component in the vaccine; (3) Known immune function impairment or low; (4) Already suffering from hepatitis B disease; (5) Acute febrile diseases and infectious diseases; (6) Any situation that may affect the observation assessment.
The withdrawal and termination criteria of the subjects are as follows: (1) The subjects can withdraw from the study at any time according to their own will; (2) Severe reaction occurs after the first or second dose of vaccination; (3) Patients receiving immunosuppressant therapy should terminate the study in time; (4) Serious adverse events occurred during the study period, especially those requiring hospitalization, prolonged hospitalization, trauma, disability, damage to work ability, life-threatening events or death.
A sample size included for cross-sectional investigation is based on the formula: (α = 0.05, Z = 1.96, δ = 0.1, P = 90.2%, P: the positive conversion rate after a single dose of 20 ug HepB in 15–29 years old population with weak positive anti-HBs;Citation17 P = 98.7%, P: the positive conversion rate after three doses of 20 ug HepB in 15–29 years old population with negative anti-HBsCitation20). In all, 1286 college freshmen were vaccinated with HepB, and their blood samples were collected to detect anti-HBs levels and completed the questionnaire survey. All the participants were given the details of the aims of the present study and signed informed consent.
2.3. HepB vaccination
The HepB inoculated was recombinant hepatitis B vaccine (CHO cell), North China Pharmaceutical Co., Ltd. For those with weak positive anti-HBs before vaccination inoculate 1 dose 20 μg HepB, while for those with negative anti-HBs before vaccination inoculate according to the 0-1-6 months 3 doses 20 μg HepB immune procedure, injected on the lateral upper arm deltoid muscle. Before the first inoculation, the inoculated subjects were informed of the variety, effect, contraindication, adverse reactions and matters needing attention, asked about their health status and signed “informed consent for HepB inoculation” for those who met the requirements.
2.4. Experimental approach and results calculation
Physical examination will be arranged uniformly within 2 weeks after freshmen enter the school. With informed consent, blood of all subjects will be collected and separated, which will be cryopreservation at −20°C, ready for inspection. Fill in the Serum Sampling Registration Form at the same time. The bottom level of serum adopts Abon pharmaceutical (Hangzhou) co., LTD. Production of HBsAg detection kit (colloidal gold) qualitative detection HBsAg levels, using Abon pharmaceutical (Hangzhou) co., LTD. Production of anti-HBs detection kit (emulsion) qualitative detection anti-HBs level, operating procedure and result determination, in strict accordance with the manual for use in the period of validity. Two red bands appear, one in the test area (T) and the other in the quality control area (C), indicating positive. The two red bands are of the same shade as strong positive, means anti-HBs ≥100 mIU/mL, and one deep and one shallow represents weak positive, means anti-HBs ≥10 mIU/mL and anti-HBs <100 mIU/mL. Only one red band appears in the quality control area (C), while no red band appears in the test area (T), indicating negative means anti-HBs <10 mIU/mL. If there is no red band in the quality control area (C), it indicates that the operation process is incorrect or the reagent bar has deteriorated and damaged. Use a new reagent to re-test.
One month after immunization against HepB, samples were collected and cryopreserved at −20°C for examination. Anti-HBs detection kit (chemiluminescence) produced by Antu Biological Engineering Co., Ltd. was used to quantitatively detect anti-HBs in serum samples after immunization. Anti-HBs of the subjects was determined according to the test instructions as follows: (1) anti-HBs before immunization was negative and ≥10 m IU/ml after immunization was considered positive conversion; (2) anti-HBs before immunization was weak positive and anti-HBs≥100 m IU/ml after immunization was also considered positive conversion.
2.5. Statistical analysis
Quantitative variables with normal distributions were present using means± standard deviations (SD), and qualitative variables were present using frequencies (percentages). Statistical significance between groups was examined by two independent variables t-test and Pearson’s chi-square test or Fisher’s exact test. Logistic regression was used to analyze the associations between the rates of anti-HBs seroconversion and the related factors. Linear regression was used to analyze the associations between the GMT levels of anti-HBs and the related factors. Data were collected using Microsoft Office Excel (version 2010), and all statistical analyses and graphs were created by SPSS statistical software for Windows 19.0 (SPSS Inc., Chicago, IL, USA). A value of P < .05 (2-sided) was considered statistically significant.
3. Results
3.1. Status of HBV infection and seromarkers among college freshmen
A total of 10645 college freshmen were included in this study. About 56.9% (6059/10645) were male and 43.1% (4586/10645) were female. The average age was 19.24 ± 0.74 years old, the youngest was 16 years old and the oldest was 25 years old. There were 54.5% (5796/10645) local students and 45.6% (4849/10645) freshmen from other provinces.
The total rate of HBsAg carriers in freshmen was 0.6% (63/10645), which in college freshmen younger than 18 years old, 19 years old and older than 20 years old were 0.6% (5/798), 0.5% (33/7181), 0.9% (25/2666) (χ2 = 7.574, P = .023); and 0.7% (42/6059) and 0.5% (21/4586) in male and female freshmen (χ2 = 2.456, P = .117); 0.4% (23/5796) and 0.8% (40/4849) (χ2 = 8.224, P = .004) in local freshmen and who from other provinces, respectively.
The total strong positive rate of anti-HBs in freshmen was 16.1% (1706/10645), the weak positive rate was 14.4% (1526/10645). In college freshmen younger than 18 years old, 19 years old and older than 20 years old, the strong positive rate of anti-HBs was 21.8% (173/793), 15.9% (1136/7148), 15.0% (397/2641), the weak positive rate of anti-HBs was 15.5% (123/793), 14.0% (1001/7148), 15.2% (402/2641), respectively (χ2 = 26.531, P < .001), while strong positive rates of anti-HBs were 17.7% (1064/6017) and 14.1% (642/4565) in male and female freshmen, 14.2% (819/5773) and 18.4% (887/4809) in local freshmen and who from other provinces, respectively. And the weak positive rate of anti-HBs was 14.3% (861/6017) and 14.6% (665/4565) in male and female freshmen, 14.1% (813/5773) and 14.8% (713/489) in local freshmen and who from other provinces, respectively (all P value <.001). ()
Table 1. Distribution of HBsAg and anti-HBs positive rate among college freshmen
3.2. Immune responses evaluation of different vaccination policies for HepB in college freshmen
A total of 1286 college freshmen were vaccinated with HepB and completed the questionnaire survey. After then, their blood samples were collected to detect anti-HBs levels. About 44.1% (567/1286) were male and 55.9% (689/1286) were female. The average age was 19.01 ± 0.84 years old, the youngest was 17 years old and the oldest was 24 years old. The average height of college freshmen was 167.63 ± 8.50 cm, and the average body weight was 58.84 ± 10.66 kg, the average BMI of college freshmen was 20.83 ± 2.74 kg/m2. About 1.9% (25/1286) college freshmen have a history of smoking. About 34.1% (439/1286) freshmen had been vaccinated HepB, 9.8% (126/1286) freshmen had not been vaccinated and the status of HepB inoculation in 56.1% (721/1286) freshmen was unknown ().
Table 2. Rates of anti-HBs seroconversion and GMT levels of anti-HBs after HepB vaccination in college freshmen among various groups via univariate analysis
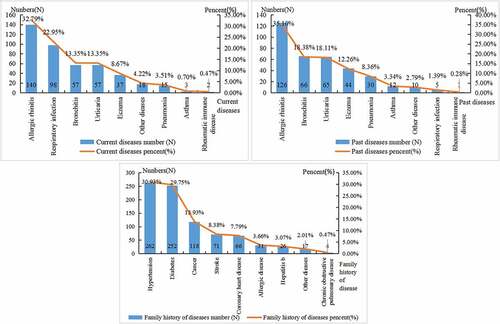
According the questionnaire survey, 33.2% (427/1286) college freshmen have a history of current disease, allergic rhinitis was the highest (140,32.8%), and rheumatic immune disease was the lowest (2, 0.5%). About 17.0% (218/1286) college freshmen have a history of allergy. About 27.9% (359/1286) college freshmen have a history of past disease, with allergic rhinitis was the highest (126,35.1%), and rheumatic immune disease was the lowest (1, 0.3%). About 65.9% (847/1286) college freshmen have a family history of disease, with Hypertension was the highest (262, 30.9%), and chronic obstructive pulmonary disease was the lowest (4, 0.5%). ()
Figure 1. Current diseases of college freshmen (a), past diseases of college freshmen (b), and family history of diseases of college freshmen (c).
Male and female freshmen with weak positive anti-HBs accounted for 42.1% (82/195) and 58.0% (113/195), respectively. Among them, 79.0% (154/195) of freshmen’s anti-HBs turned positive after receiving one dose HepB, with the GMT level of anti-HBs being 502.44 mIU/mL. Meanwhile, male and female freshmen with negative anti-HBs accounted for 44.5% (485/1091) and 55.6% (606/1091), respectively. Among them, 100% (1091/1091) of freshmen’s anti-HBs turned positive after receiving three doses of HepB, with the GMT level of anti-HBs being 876.43 mIU/mL. In multivariate analysis, overall, significantly lower GMT for anti-HBs were found in females compared with males (OR = 0.94, 95% CI: 0.89–0.99, P < .05); lower in subjects from other cities in Zhejiang Province and other provinces compared with subjects from Hangzhou City (OR = 0.94, 95% CI: 0.90–0.99; OR = 0.93, 95% CI: 0.88–0.98, all P-values<0.05); higher GMT for anti-HBswere found in subjects who were injected three doses of HepB compared with who were injected one dose (OR = 1.58, 95% CI: 1.51–1.65; P-value < 0.05) ().
Table 3. Association of Seroepidemiology of anti-HBs and related variables via multivariate analysis
In short, the GMT for anti-HBs was significantly influenced by gender, registration and the immunization doses of HepB, and no significant factors were discovered for the rates of anti-HBs seroconversion.
4. Discussion
Since 2002, HepB has been included in the immunization program, and free immunization of HepB has been provided to newborns. In recent years, the HepB inoculation rate of newborns in Hangzhou has maintained at a high level, with the HepB inoculation rate over 99.0%. Data show that the reported incidence of hepatitis B in Hangzhou has been decreasing for 10 consecutive years, and the reported incidence of hepatitis B in 2019 is 3.38/100,000. Since the implementation of neonatal HepB immunization strategy, hepatitis B prevention and control has achieved remarkable results,Citation10 but the situation is still grim.Citation1The results of this survey showed that the total HBsAg carrying rate of freshmen in Hangzhou was 0.6%, which was lower than the HBsAg prevalence rate of 1–29 years old in Zhejiang Province in 2014 (1.1%) and the national level of 1–29 years old in 2014 (2.6%).Citation10 This indicates that the HepB vaccination in China is effective in recent years, and the HepB immunization status of the population is good. However, this survey also found that the total anti-HBs positive rate of freshmen was 30.5%, which was lower than the national level of 15–29 years old (56.9%) in 2014 and the anti-HBs positive rate of 1–29 years old in Zhejiang Province (52.5%) in 2014, while the anti-HBs positive rate of other provinces was basically maintained between 54.0% and 72.0%Citation12,Citation21–23. A survey of permanent residents aged 25 to 45 in Beijing, Shanghai, Guangzhou, Chengdu and Wuhan found that only 12.5% had received HepB vaccination. However, the rate of HBsAg carriers among people aged 20 to 25 in China is as high as 12.0%,Citation24 and Tan Xiaohong et al. found that the positive rate of HBsAg among college students is about 10.0–12.8%.Citation25 Therefore, even with the introduction of HepB vaccination, there will still be a large number of chronic hepatitis B patients.Citation26 It is suggested that freshmen are one of the high-risk groups of hepatitis B, which may be related to collective life, active social activities and poor awareness of hepatitis B prevention. Some college students with HBV affect their study, abroad, employment, and even marriage. In order to effectively control the spread of HBV in the university campus, we should strengthen the knowledge of hepatitis B publicity and education of college students, so that they are aware of the importance of hepatitis B prevention and control and establish a healthy concept, in order to effectively control the spread of HBV in the campus, and then reduce the positive rate of HBsAg in college students.
In this survey, the HBsAg-carrying rate and anti-HBs positive rate of college freshmen from other provinces (0.6%–1.0%) were higher than those from our provinces (0.2%–0.6%). Studies on spatial epidemiology indicated that HBsAg carrying rates were significantly different among provinces (0.8%–27.1%).Citation27 The areas with high HBsAg carrying rates were mainly distributed in the coastal areas of central and southeast China and the Tibetan pastoral areas, and Guangdong,Citation28 Guangxi, Jiangxi and other provinces had the highest carrying rates.Citation27 According to the national seroepidemiological survey of people aged 1–29 in 2014,Citation10 the prevalence of HBsAg in the population aged 15–29 years in the south of the Yangtze River was higher than that in the north of the Yangtze River, which in the countryside was higher than that in the city. This suggests that the positive rate of anti-HBs is different in different regions. Immune planning, vaccine management and vaccination publicity may affect the immunization status of the population.Citation29,Citation30 Therefore, the publicity and education of HepB related knowledge should be strengthened to improve the correct understanding of vaccination and increase the vaccination rate of adult HepB.
The age distribution analysis of this survey showed that the HBsAg carrying rate of college freshmen was the highest (0.9%) in the age group over 20 years old, which was consistent with the results of the national seroepidemiological survey of 1–29 years old in 2014. The HBsAg prevalence rate of 1–29 years old population increased with age. The prevalence rate of HBsAg in 15–29 year olds was 4.4%, the highest in 20–24 year olds (5.0%), followed by 25–29 year olds (5.0%).Citation10 This may be due to the effective blocking of mother-to-child transmission of HBV by the extensive immunization of neonates and children with the HepB program.Citation31,Citation32 However, with the increase of age, such as sexual transmission, intravenous drug injection and other risk factors, resulting in the high level of HBV infection in the older group of people over 15 years old. This survey found that the anti-HBs positive rate in freshmen was the highest (37.3%) in the age group under 18 years old. With the increase of age, the anti-HBs positive rate gradually decreased, which was similar to the results of relevant studies at home and abroad.Citation12,Citation13 It is suggested that the antibody titer decreases gradually with the increase of age, that is, the increase of immune years.Citation14 It also suggests that neonatal HepB inoculation alone does not provide permanent protection against HBV. The peak of vaccine-induced anti-HBs titers appeared 1 month after the initial inoculation of HepB, and decreased rapidly in the following year. Shen Lingzhi et al. observed 7454 children 5–16 years after basic immunization and found that the positive rates of anti-HBs and HBsAg were 43.9% and 1.2%, respectively.Citation16 Adult HepB inoculation has a good immune effect, economic and social benefits.Citation17 The positive rates of HBsAg in adults with and without HepB inoculation history were 1.8% and 12.0%, respectively, HBV infection rate was 17.3% and 76.9%, respectively. This indicates that adult inoculation with HepB is an effective measure to control HBV infection.Citation18 The study of Zhang Wei et al.Citation33 confirmed that the infection rate of adult HBV was still at a high level, and it would still take a long time to control hepatitis B only by carrying out HepB vaccination in neonates. Wang’sCitation34 study compared immunogenicity of different HepB schedule, data suggested that the standard 20 μg (0-1-6 month) regimen of HepB should be recommended as a priority on the premise of complete compliance in adults. It is very important to carry out HepB vaccination in adults to reduce the incidence and mortality of hepatitis B in China.Citation19,Citation35
In this survey, 34.1% freshmen had been vaccinated HepB, 9.8% freshmen had not been vaccinated, and the status of HepB inoculation in others was unknown. The college freshmen not vaccinated against hepatitis B may be associated with a history of present disease, past medical history, past allergies, and past family history. Accordingly, the questionnaire survey found that 33.2% college freshmen had a history of current disease, with allergic rhinitis was the highest (32.8%), and rheumatic immune disease was the lowest (0.5%); 17.0% college freshmen had a history of allergy; 27.9% college freshmen had a history of past disease, with allergic rhinitis was the highest (35.1%), and rheumatic immune disease was the lowest (0.3%); 65.9% college freshmen had a family history of disease, hypertension was the highest (30.9%), and chronic obstructive pulmonary disease was the lowest (0.5%). In this survey, a total of 1286 college freshmen were vaccinated with HepB, and their blood samples were collected to detect serum anti-HBs antibody levels. Among them, 79.0% of freshmen’s anti-HBs turned positive after receiving one dose HepB, with the GMT level of anti-HBs being 502.44 mIU/mL. Meanwhile, male and female freshmen with negative anti-HBs accounted for 44.2% and 55.9%, respectively. Among them, 100.0% of freshmen’s anti-HBs turned positive after receiving three doses of HepB, with the GMT level of anti-HBs being 876.43 mIU/mL. The positive rate of anti-HBs was higher than the 77.5% reported by similar domestic studiesCitation36 and was close to 92.0%–97.8% reported by similar studies abroad.Citation37 The positive conversion rate of anti-HBS was not related to age and sex, indicating that the HepB had good immunogenicity. The school should not only strengthen supervision but also combine with the monitoring of anti-HBs to understand the immune status of HepB. Regarding the positive conversion rate of anti-HBs after HepB vaccination, due to the differences in the vaccines, methods, inoculated objects, samples and other factors, the good positive conversion rate in this study may be related to the following factors: (1) The survey method adopted in this study is different. Pei’sCitation36 study obtained inoculation information through retrospective questionnaire survey, which resulted in a large recall bias and affected inoculation. However, this study adopted a prospective survey method with strong reliability of the results. (2) The sample size of the inoculated subjects was 1289, which was highly representative, while William’s studyCitation37 had a small sample size. HepB inoculation is the most effective way to prevent HBV infection in college students. Therefore, in order to speed up the pace of hepatitis B control, HepB vaccination should be gradually carried out in people other than newborns according to the local situation, especially for high-risk groups such as university students.Citation38
In fact, there are also shortcomings in this study: (1) In this study, we only measured the levels of HBsAg and anti-HBs, but did not measure the levels of anti-HBc. Therefore, it is impossible to distinguish the past resolution of HBV infection from the anti-HBs-positive college students. We used the positive conversion rate of anti-HBs and GMT value to reflect the effectiveness of HepB vaccination; (2) The design of this study was indeed deficient in the absence of antibody levels after one dose of ‘negative’ anti-HBs immunization and antibody levels after three doses of antibody ‘weak positive’ anti-HBs immunization.
In conclusion, investigation of hepatitis B seroepidemiology in college students can help to understand the carrying status of HBsAg and its immunity to hepatitis B, and evaluate the immune effect of HepB, so as to provide a scientific basis for the development of hepatitis B control strategy and the application of HepB. The HBsAg carrying rate and anti-HBs positive rate of college freshmen were low, and the HepB has a good effect on the immunity of college freshmen. Thus, increasing the immunization rate of HepB is very important for the prevention and control of hepatitis B. While continuing to strengthen the vaccination of HepB in children, it is necessary to strengthen the promotion and use of HepB for high-risk groups such as university freshmen.
Author contributions
Formal analysis, Yuyang Xu; Investigation, Jun Wang, Xinren Che, Xuechao Zhang, Wei Jiang; Methodology, Yan Liu and Yuyang Xu; Project administration, Yan Liu; Software, Yuyang Xu; Validation, Jian Du, Xiaoping Zhang and Wenwen Gu; Writing – original draft, Yuyang Xu; Writing – review & editing, Yan Liu.
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
Ethical considerations
This program was approved by the ethics committee of Hangzhou Center for Disease Control and Prevention.
Additional information
Funding
References
- Sha HY, Du L, Wen L, Li SL. Epidemic dynamics and research progress of hepatitis B. J Prev Med Chin People Liberation Army. 2017;35(9):1149–53.
- World Health Organization. Global hepatitis report 2017. Geneva, Switzerland: WHO; 2017. p. 83.
- Qiao YL. Strategies and prospects of cancer population prevention and control in China. Chin J Oncol. 2012;34:483–85.
- Cui F, Shen L, Li L, Wang H, Wang F, Bi S, Liu J, Zhang G, Wang F, Zheng H, et al. Prevention of chronic hepatitis B after 3 decades of escalating vaccination policy, China. Emerg Infect Dis. 2017;23(5):765–72. doi:10.3201/eid2305.161477.
- Chen HY, Li X, Peng SX. Impact of chronic hepatitis B and HBeAg status on maternal and infant outcomes. Chin J Dis Control Prev. 2018;22(6):617–20.
- Cui FQ, Gong XH, Chen YS, Wang F, Zheng W, Wu Z. Vaccination progress of hepatitis b vaccine and epidemiology changes of carrying rate of hepatitis B surface antigen by province in China, 1992–2006. Chin J Vaccines Immunization. 2012;18(1):6–13.
- Wang GQ, Wang FS, Chen J, Ren H, Zhuang H, Sun J, Li LJ, Li J, Meng QH, Zhao JM, et al. The guideline of prevention and treatment for chronic hepatitis B: a 2015 update. J Clin Hepatol. 2015;31(12):1941–60.
- Zhao YL, Han BH, Zhang XJ, Pan -L-L, Zhou H-S, Gao Z, Hao Z-Y, Wu Z-W, Ma T-L, Wang F, et al. Immune persistence 17 to 20 years after primary vaccination with recombination hepatitis B vaccine (CHO) and the effect of booster dose vaccination. BMC Infect Dis. 2019;19(1):482. doi:10.1186/s12879-019-4134-9.
- Shen L, Wang F, Wang F, Cui F, Zhang S, Zheng H, Zhang Y, Liang X, Bi S. Efficacy of yeast-derived recombinant hepatitis B vaccine after being used for 12 years in highly endemic areas in China. Vaccine. 2012;30(47):6623–27. doi:10.1016/j.vaccine.2012.08.067.
- Cui FQ, Zhuang H. Epidemics and control of hepatitis B in China . Chin J Viral Dis. 2018;8:257–64.
- Wu TW, Lin HH, Wang LY. Chronic hepatitis B infection in adolescents who received primary infantile vaccination. Hepatology. 2013;57(1):37–45. doi:10.1002/hep.25988.
- Wang ZY, Dai DF, Xiao JH. Monitoring study of hepatitis B antibodies in healthy population and immune successful rate of hepatitis B vaccine in infants in Hunan . Pract Prev Med. 2010;17(5):888–89.
- Ni YH, Chang MH, Wu JF, Hsu H-Y, Chen H-L, Chen D-S. Minimization of hepatitis B infection by a 25-year universal vaccination program. J Hepatol. 2012;57(4):730–50. doi:10.1016/j.jhep.2012.05.021.
- Luo JS, Wang F, Liu J, Shan ZZ, Pan H. Analysis of the monitoring results of HBsAb among healthy population in Qiandongnan prefecture of Guizhou in 2013–2016. Stud Trace Elem Health. 2019;36(1):51–52+55.
- Yue X, Ge C, Zhuge S, He H, Yang H, Xu H, Huang A, Zhao Y. Changes and analysis of anti-HBs titres after primary immunization in 1- to 16-year-old Chinese children: a hospital-based study. J Viral Hepat. 2018;25(4):373–80. doi:10.1111/jvh.12818.
- Shen LZ. Study on enhancing immunity of hepatitis B vaccine in children aged 5–16 years. Ningbo, China: Ningbo University; 2012. p. 1–69.
- Qian YH, Lin YD, Shen HB, Dong MH, Deng Y, Wang XW, Yang YQ, Gu J, Yu RB. Effects of vaccination on hepatitis B virus infection in adults. Chin J Prev Med. 2008;42(12):930–31.
- Lin B, Zeng KF, Xue L. Survey on adult HBV infection rate and influence factor in Karamay City. Pract Prev Med. 2006;13(5):1195–97.
- Peng SH, Liao Z, Xiong CH, Wen HR, Zhang YX, Zhao HB. Epidemic trend and clustering analysis of hepatitis B incidence rate in Nanchang City, 2004–2010. Chin J Dis Control Prev. 2012;16(1):43–45.
- Tang Y. Evaluation and study on the effect of 20μg hepatitis B vaccine inoculation strategy in the army. Academy of Military Sciences; 2018.
- Yang Q, Chen XC, Tong WB, Liu Y, Bao Y, Qi Q. Hepatitis B surface antibody levels among healthy people in Sichuan province, 2018. Chin J Vaccines Immunization. 2019;25(5):524–27.
- Wang JH, Wang W, Sun L, Liang Y, Liu Y, Du H, Zhang ZG, Guo Y. Analysis of the antibody level for the hepatitis B surface antigen of the healthy population in Hebei province from 2008 to 2010. Chin J Health Lab Technol. 2011;21(9):2275–76.
- Deng QY, Zhong G, Wei JH, Yang RC, Du ZQ, Dong AH. Serological survey of hepatitis B and coverage of hepatitis B vaccine among people aged 1–29 years in Guangxi Zhuang Autonomous Region, 2014. Chin J Vaccines Immunization. 2017;23(4):406–10.
- He XT, Ma SH, Fan CX, Dong DW, Bao M. Investigation of hepatitis B KAP among 4 college students in Guangzhou. Chin J School Health. 2010;31(3):276–78.
- Tan XH. Investigation and analysis of hepatitis B infection among college students and countermeasures of health education. Chin Foreign Med Treat. 2010;1:149–50.
- Zhang SX, Sun PP, Xia Y. Evaluation and forecast for economic outcomes of hepatitis B immunoprophylaxis strategies in China from 2006 to 2030. Chin J Dis Control Prev. 2018;22:741–46.
- Li Y. Distribution characteristics of HBS Ag in high and low incidence areas of hepatitis B in China. Henan J Prev Med. 1983;3:1–5+26.
- Sha QH. Epidemiological investigation of viral hepatitis in Guangdong province. Vol. 2. Guangzhou,China: Epidemic Control Data of Guangdong; 1981. p. 32–39.
- Chung PW, Suen SH, Chan OK, Lao TH, Leung TY. Awareness and knowledge of hepatitis B infection and prevention and the use of hepatitis B vaccination in the Hong Kong adult Chinese population. Chin Med J (Engl). 2012;125:422–27.
- Polaris Observatory Collaborators. Global prevalence, treatment, and prevention of hepatitis B virus infection in 2016: a modelling study. Lancet Gastroenterol Hepatol. 2018;3(6):383–403. doi:10.1016/S2468-1253(18)30056-6.
- Liu MH, Sheng YJ, Liu JY, Hu H-D, Zhang Q-F, Ren H. Efficacy of telbivudine on interruption of hepatitis B virus vertical transmission: a meta-analysis. Ann Saudi Med. 2013;33(2):169–76. doi:10.5144/0256-4947.2013.169.
- Lao TT, Sahota DS, Chan PKS. Three decades of neonatal vaccination has greatly reduced antenatal prevalence of hepatitis B virus infection among gravidae covered by the program. J Infect. 2018;76(6):543–49. doi:10.1016/j.jinf.2018.04.003.
- Zhang W, Lin CY, Han LL, Li LQ, Gao P, Lin H, Gong XH, Huang F, Tang YQ, Ma JX, et al. Study on immune effects and influencing factors of different doses of domestic recombinant yeast hepatitis B vaccine in adults. Chin J Epidemiol. 2010;31(7):767–70.
- Wang ZZ, Gao YH, Wang P, Wei L, Xie C-P, Yang Z-X, Lan J, Fang Z-L, Zeng Y, Yan L, et al. Comparison of immunogenicity between hepatitis B vaccines with different dosages and schedules among healthy young adults in China: a 2-year follow-up study. Hum Vaccin Immunother. 2018;14(6):1475–82. doi:10.1080/21645515.2018.1438090.
- Pei G, Xu JM, Zhang B, Gui XF. Analysis on the epidemiology of hepatitis B in Shishou City, 2004–2010. Chin J Dis Control Prev. 2012;16(3):226–29.
- Ye LX, Zhou DJ, Yang JJ, Tang SW, Li XT, Yi YC. Immune effect of recombinant yeast hepatitis B vaccine in adults. Chin J Epidemiol. 2003;24(10):953–54.
- Cassidy WM, Watson B, Ioli VA, Williams K, Bird S, West DJ. A randomized trial of alternative two-and three-dose hepatitis B vaccination regimens in adolescents: antibody responses, safety, and immunologic memory. Pediatrics. 2001;107:626–31. doi:10.1542/peds.107.4.626.
- National Health and Family Planning Commission; National Development and Reform Commission; Ministry of Education; Ministry of Science and Technology; Ministry of Industry and Information Technology; The Ministry of Oublic Securuty; The Ministry of Finance; Ministry of Human Resourcs and Social Security; Ministry of Housing ang Urban-Rural Development; China Food and Drug Administration; National Administration of Traditional Chinese Medicine(NATCM). Action plan for the prevention and treatment of viral hepatitis in China (2017–2020). Chin J Viral Dis. 2018;8(1):1–5.

